Panic Disorder
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
Panic Disorder DSM Criteria
You must have both:
(1) Recurrent unexpected panic attacks + at least 4 symptoms:
Palpitations, pounding heart
Sweating
Trembling or shaking
Shortness of breath or smothering
Choking feeling
Chest pain
Nausea
Dizziness
Derealization or depersonalization
Parathesis
Chills or hot flashes
Fear of losing control or going crazy
Fear of dying
(2) At least one of the attacks has been followed by at least 1 month by one or more of the following:
Persistent concern about having additional attacks
Worry about the implications of the attack or its consequences
A significant change in behaviour related to the attacks
Recurrent panic attacks
More than one panic attack
Attacks happen on a regular-ish basis
Unexpected panic attacks
Panic attacks occur out of the blue
Ex. if you have a panic attack every time you see dogs (expected stimuli) = you do not meet criteria for panic disorder
In panic disorder, what is the focus of the fear?
Panic, fear, internal bodily symptoms???
What is the prevalence of panic disorder (12 months & lifetime)?
12 months = 2.4% (1.6% in Canada)
Lifetime = 4.7% (3.7% in Canada)
T or F: panic disorder is 2x as common in women than men
TRUE
What is the age of onset for panic disorder?
Early 20s
What percentage of individuals with panic disorder have a commorbid disorder?
93.7%
They have an average of 4.5 additional disorder diagnoses (typically GAD, SAD, MDD)
Without treatment, what is the course of panic disorder?
Chronic course (stable over time)
Do HPA axis signs overlap with panic disorder symptoms?
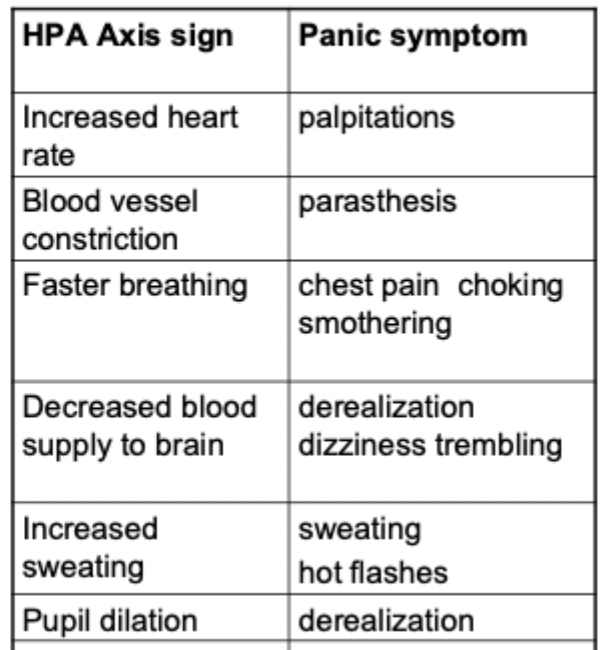
YES!
Almost a 1:1 mapping
What happens when the panic has a clearly threatening trigger?
We can correctly attribute the panic sensations to a legitimate fear
What happens when the panic has NO clearly threatening trigger?
Since we have no idea, we start to incorrectly attribute the panic sensations to a "going crazy", "having a heart attack", or "dying"
Cognitive-behavioural model of panic disorder
People with PD pay very close attention to their bodily sensations
They are quick to misinterpret these sensations as signs of imminent catastrophe
*Panic disorder is a fear of fear
Cognitive-behavioural model of panic disorder DIAGRAM!!!
MUST KNOW THIS FOR EXAM!!!
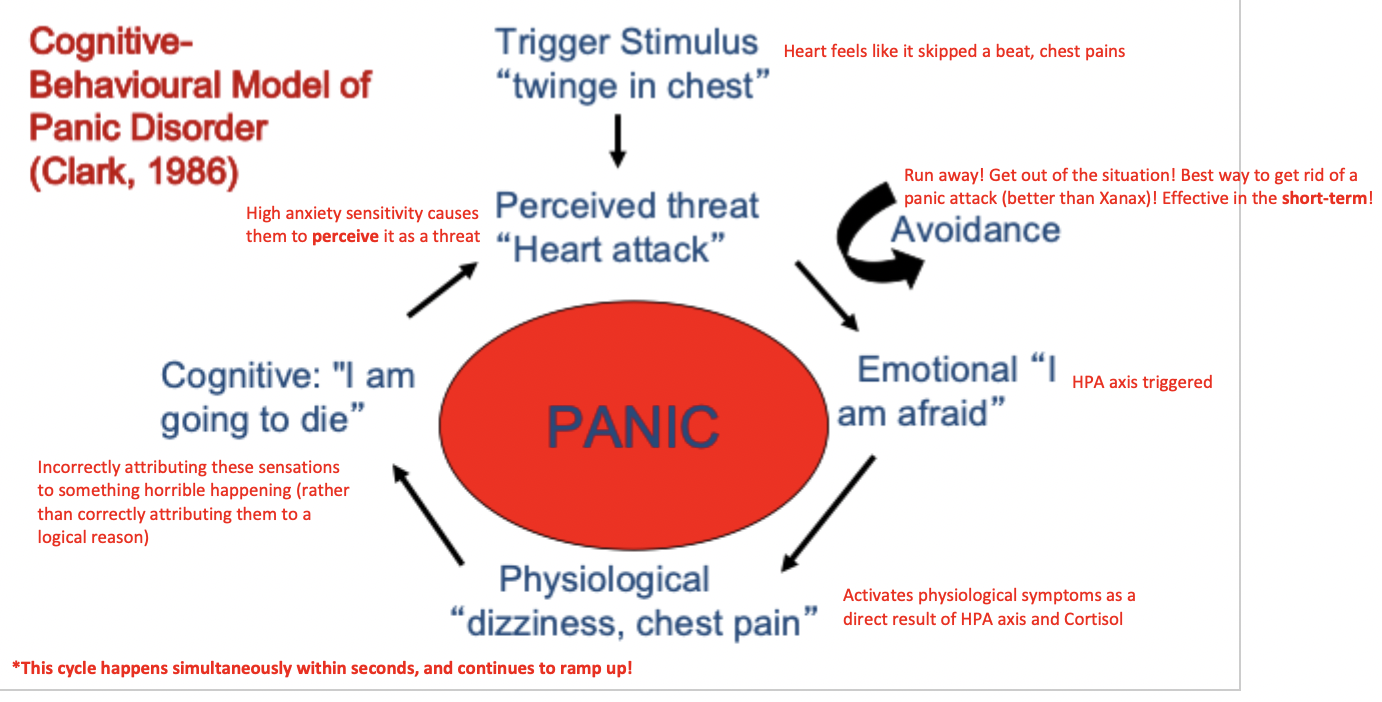
What are the specific cognitive and behavioural components of the cognitive-behavioural model of PD?
Cognitive: catastrophic thoughts intensify physiological bodily sensations and fear/panic
Behavioural:
Classical conditioning = previously neutral situations become associated with panic sensations -> drives the avoidance
Operant conditioning = avoidance is maintained by negative reinforcement (fleeing, short-term relief)
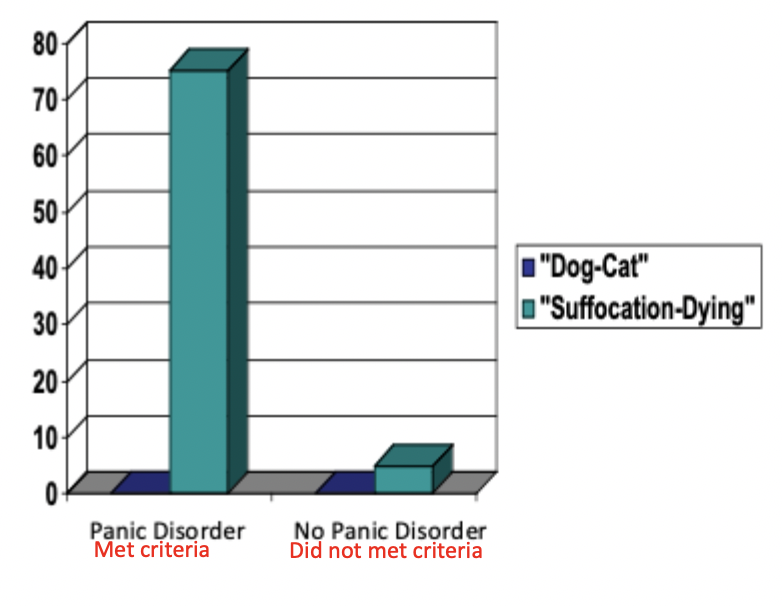
Study providing evidence for the cognitive-behavioural model of PD (Clark, 1988)
Study details:
Study measured how many participants had a panic attack in the lab
Participants shown neutral word pairs ("dog-cat") + panic-related word pairs ("suffocating-dying")
Findings:
Participants who never experienced a panic attack prior to this study very rarely had an attack in response to the word pairs (extremely low percentage)
BUT for participants with PD who had experienced a panic attack prior to this study, simply reading panic-related words activated catastrophizing thoughts + made them focus on their internal bodily sensations ("I am suddenly feeling short of breath…") -> thus activating the cycle of panic illustrated by the model
What is a key psychological vulnerability for PD?
High anxiety sensitivity (ASI) = more likely to interpret bodily sensations as signs of danger
Ex. "When I feel pain in my chest, I worry that I'm going to have a heart attack"
"When my stomach is upset, I worry that I might be seriously ill"
"When I feel 'spacey' or spaced out, I worry that I might be mentally ill"
Higher ASI scores significantly predict greater panic symptom response to CO2 challenge in individuals with PD
CO2 challenge = Participants inhale a gas mixture (35% CO₂ + CO₂) which mimics the physical sensations similar to those experienced during a panic attack (ex. Short breath, dizziness, heart racing)
T or F: Anxiety sensitivity has a genetic base
TRUE
What study provides evidence for familial transmission of anxiety sensitivity? (Mogg et al., 2012)
Study question:
Do children with parents who have PD already show a vulnerability (anxiety sensitivity) to PD this early in their lives?
Study details:
High-risk study design
Participants included girls of mothers with lifetime PD + girls with mother who did not have PD
NOTE: the girls themselves (9-14 yos) did not have PD (only some of their mothers)
Task:
Used a visual probe task to assess attentional bias to physical threat
Version 1 = Stimulus picture (ambulance) + neutral picture (U-haul van) flashed briefly on the screen at top and bottom the same time -> screen goes blank -> small cross appears either at the top or bottom of screen (where either picture was)
Version 2 = Same procedure as before, expect it was a stimulus word (injury) + neutral word (laundry)
Participants then asked "Did the cross appear on the top or bottom of the screen?"
Hypothesis:
If the girls attention was drawn to the ambulance (shown at the top of the screen), she will be quicker to respond if that’s also where the dot appeared (because her eyes were already there)
Findings:
Girls with mothers who had PD (meaning the girls had higher ASI scores) showed significantly greater attentional bias to the threatening stimulus (ambulance + "injury"), meaning they were able to respond faster when the cross appeared where the threat was
***Girls with a mothers who had a lifetime history of PD = more likely to meet criteria for PD + higher anxiety sensitivity index (ASI) scores + higher state and trait anxiety scores
What are some examples of in-vivo exposure targets for PD?
In vivo = gradual exposure to the fear
Driving
Public transportation
Bridges
Waiting in lines
Crowds
Stores/malls
Elevators/escalators
Closed spaces
Restaurants
What is the difference between in-vivo and interoceptive exposure?
In-vivo Exposure = Exposure to the situations
Interoceptive Exposure = Exposure to the symptoms themselves
What are some specific elements of CBT for PD?
Interoceptive exposure = exposure to the physiological symptoms of panic
Intended to help remove the conditioned response of panic caused by physical sensations
Removing the "fear of the fear"
*NOTE: symptoms must be fully induced in order to ensure that extinction takes place
How are symptom hierarchies used in CBT / interoceptive exposure for PD?
Allows client to practice invoking the feared symptoms + rank them according to intensity, fear, and similarity
Ex. "Okay [client], put your head down and shake it back and forth!"
Provokes feelings of dizziness, derealization, etc. (all of which are associated with panic attacks)
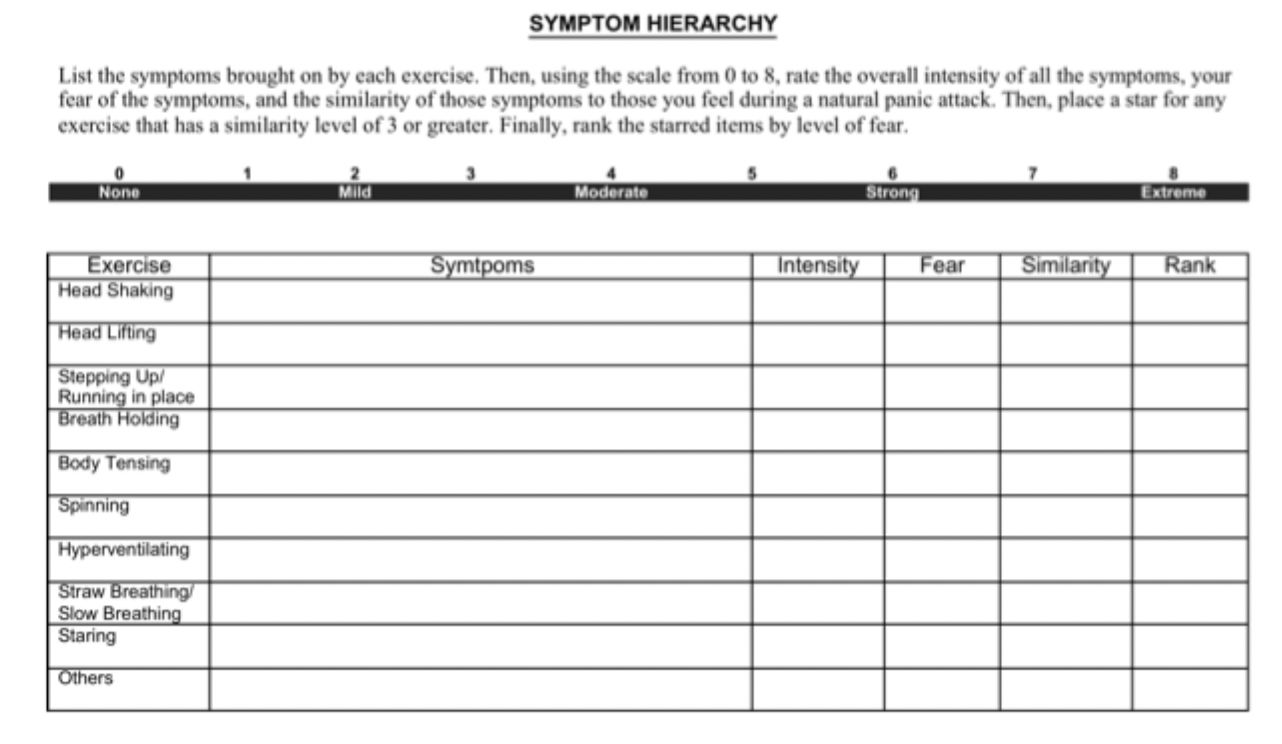
How are interoceptive exposure exercise records used in CBT / interoceptive exposure for PD?
Allows client to track multiple trials of invoking different symptoms through various exercises/movements, ultimately with the goal of seeing their anxiety decrease over time with multiple exposures