From Skull Drill to Free Will - Test 3
1/41
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
What is the ‘DSM’?
DSM stands for Diagnostic and Statistical Manual of Mental Disorders
The current and latest edition is the DSM-5-TR, published in March 2022
It grew from a tradition filled with haphazard science and politically driven choices
Any steps forward in the reform of insane asylums were followed by steps backward.

What was ‘The Medical Superintendents of American Institutions (AMSAII)’?
Founded by Thomas Story Kirkbride; a physician and advocate for the mentally ill
It was commissioned to focus "primarily on the administration of hospitals and how that affected the care of patients“ - As opposed to conducting research or promoting the profession.
The 1840 census: mental health in the United States created the recording of the frequency of – “idiocy/insanity”
Their original goal was to:
Count the numbers of patients confined in mental hospitals, and
Create a uniform system of naming, classifying and recording the cases of mental illness.
By the 1880 Census - There were 7.
What were the seven types of mental illness as of the 1880 census?
Mania
Melancholia
Monomania
Paresis
Dementia
Dipsomania
Epilepsy
How did the AMSAII change over the decades?
In 1892:
It expanded its membership to include other mental health professionals
Changed its name to the American Medico-Psychological Association
In 1921
It became the American Psychiatric Association
What was the ‘National Commission on Mental Hygiene’?
Founded in 1909 by Clifford Beers
Later became Mental Health America
A US-based organization
A key figure in the early mental hygiene movement.
Its primary mission was to advocate for improved care and treatment of mental illness, research, and preventative services.
The committee played a crucial role in shaping public understanding and policy regarding mental health in the early 20th century.
How did the DSM come to be?
The DSM root’s go back to the 1840s – Before the first edition was conceived or published.
Throughout history there have been reform periods.
When it is possible to detect different motivations behind its implementation and when deliberate action was taken, and it started with:
The 1840 US census
Marked the first time the federal government collected data on “idiocy/insanity”
Canada's first census to collect data on individuals considered "lunatic" was in 1851.
This census, taken in New Brunswick, included a question asking about individuals who were sick, infirm, deaf and dumb, blind, lunatic, or idiot
The first four provinces that formed the Dominion of Canada in 1867 were Ontario, Quebec, Nova Scotia, and New Brunswick.
The first census of Canada was taken in 1871.
According to The Census Act of May 12, 1870, census-taking was to take place no later than May 1st.
Under Section 8 of the Constitution Act of 1867 (formerly the British North America Act)
1844
At a meeting took place in Philadelphia, 13 superintendents and organizers of insane asylums and hospitals gathered
This new foundation was The Medical Superintendents of American Institutions (AMSAII)
Together, the AMSAII and the National Commission on Mental Hygiene developed a guide for mental
hospitals called the "Statistical Manual for the Use of
Institutions for the Insane” in 1917
Over the years it would be revised several times by the APA
Who was Dorothea Dix?
April 4, 1802 – July 17, 1887
An American activist on behalf of the insane
She was a leading figure in those national and international movements that challenged the idea that people with mental disturbances could not be cured or helped.
Through a vigorous program of lobbying:
State legislatures and The United States Congress
Created the first generation of American mental asylums
Played an instrumental role in the founding or expansion of more than 30 hospitals for the treatment of the mentally ill.
Dorothea Dix convinced many state legislatures to pay for hospitals
By doing so, she bolstered the lives of countless people with mental illness from neglect and inhumane conditions
How did the World Wars affect recognition of mental disorders?
Similar to other significant moments of social change, world events and their consequences set in motion the need to transform thinking and action.
One key source that furthered the development and understanding of mental illness was the results of the World Wars
WWI from 1914 to 1918
WW2 from 1939 to 1945
During WWI and WW2, military psychiatrists who treated soldiers suffering from mental disorders believed their conditions resulted from their traumatic war experiences
They were specifically concerned with a reoccurring theme:
It consists of a lingering anxiety a tendency toward nightmares, ‘flashback memories’ of battle, and the avoidance of activities that might provoke a sensation of danger.
The war years witnessed large-scale involvement of American (The US) and British psychiatrists
During World War II British psychiatrists primarily used The International Classification of Diseases (ICD) for classifying and diagnosing mental disorders.
Following World War II, the 6th edition of the ICD (ICD-6) was published.
It was the first time, it included a section on mental disorders.
War time injuries introduced another new reality; it caused an examination of social norms values and beliefs.
Prior to war these men (for the most part), had been well functioning, even considered elite respected members of society
Shell shock
This involvement consequently redirected the psychiatric focus away from mental institutions, “the asylums” and what was then considered the traditional clinical perspective
What is ‘The International Classification of Diseases’?
The first ICD was adopted by the International Statistical Institute in 1893, based on the Bertillon Classification of Causes of Death.
Developed by Jacques Bertillon, it was originally intended for classifying causes of death and was later expanded to include morbidity
In 1948 The World Health Organization (WHO) took charge of the classification system.
Who was William C. Menninger?
Was a brigadier-general and the head of psychiatry in the Office of the Surgeon General during World War II
Advanced a classification scheme for the US army, later called Medical 203.
What is ‘Medical 203’?
Between the two wars, in 1943, a committee would develop the new classification scheme called Medical 203
It was used to help psychiatrists treat the soldiers whose mental health was harmed as a result of their war experiences
The military nosology appeared in October 1945 as the Technical Medical Bulletin.
Some stated it breathed the spirit of psychoanalysis, describing “psychoneurotic disorders” as “resulting from the exclusion from the consciousness (ie, repression) of powerful emotional charges, usually attached to certain infantile and childhood developmental experiences.”
Drawing from psychiatrist Adolf Meyer, as well as on Sigmund Freud, the disorders were referred to as “reactions” of “dissociative reaction”
How did Medical 203 impact the DSM?
“In acute cases, the personality (ego) disorganization appears to permit the anxiety to overwhelm, and momentarily govern the total individual. The repressed impulse, giving rise to the anxiety, may be either discharged or deflected into various symptomatic expressions such as fugue, amnesia, etc.”
This document became the basis of psychiatric classification in postwar America.
The conception of the DSM, one could say, came about due to these various changes.
By 1948, confusion soon existed because of the numerous classification systems being used.
Unhappy about the confusing diagnostic systems currently in play, the APA asked its Committee on Statistics to prepare an official nosology that would preclude all others.
In 1950 the APA decided to examine the various manuals
The ultimate goal was to create one system that could be used for diagnostic and statistical purposes, plus a glossary of definitions for the different illnesses.
Decisions were made, and one was to call the new document the DSM.
In 1952 the DSM-1 was published.
The DSM’s unfolding succession of publications was an American product – beginning with Medical 203 in 1945
Then it was guided by psychoanalytic insights through DSM-I in 1952 and DSM-II in 1968
In 1980, DSM-III represented a massive – “turning of the page” in nosology – the branch of medical science dealing with the classification of diseases.
What are the three purposes that the DSM V serves?
To provide “a helpful guide to clinical practice
To facilitate research and improve communication among clinicians and researchers
To serve as “an educational tool for teaching psychopathology
What is the history of the term ‘alcoholism’?
Was first called “An Odious Disease” by Dr. Benjamin Rush in 1784
The word “alcohol” didn’t come into use until the eighteenth century and was used to designate the intoxicating ingredient in liquor.
“Alcoholism” was first used in 1849 by Dr. Magnus Huss to describe chronic intoxication with physical and social pathology
A century later the word “alcoholic” was common in the United States
What has alcoholism looked like in the DSM, historically?
DSM (1952)
The history of diagnoses in the DSM reflects the evolving concept of addiction
In the DSM the diagnostic decision is binary, they either meet the specific criteria or they do not.
In reality, symptoms exist more as if on a continuum.
In the first edition of the DSM in the 1950’s, alcoholism and drug addiction were grouped with “sociopathic personality disturbances”
Signs and symptoms were not described, but instead the idea that addiction came from an “underlying brain or personality disorder”.
What changes were made to “alcoholism” in the DSM II (2)?
In DSM II (1968) added “subtypes” of alcoholism.
Episodic excessive drinking, habitual excessive drinking, and alcohol addiction.
In DSM II, drug dependence was expanded to include subcategories.
Specific drug classes and physiological signs of dependence (withdrawal and tolerance)
What changes were made to “alcoholism” in the DSM III (3)?
1970’s the Feighner criteria are adopted, constructed on research based decision rules
This was reflected in DSM III (1980), which also included:
The idea of abuse and dependence
The term “alcoholism” was eliminated
Substance use disorders got their own section and were no longer listed under personality disorders
The idea of a public health model was introduced to explain addiction.
The dependence category required either tolerance or withdrawal (or both) to be present.
Abuse was the presence of drug related problems in the absence of physiological symptoms
DSM III-R (1987)
Reflected a growing concept that addiction really involved a broader behavioural syndrome and was not only defined by physical symptomology.
“Abuse” remained as a category for people who never met the “dependence” diagnosis.
What changes were made to “alcoholism” in the DSM IV (4)?
DSM IV (1994)
Over 100 different substance related disorders for 12 different classes of drugs.
Dependence was now a “syndrome” involving compulsive use, tolerance or withdrawal.
DSM IV-R (2000)
Defined substance abuse as meeting any of the four criteria revolving around recurrent problems related to the substance.
Dependence has to meet three or more of seven physiological or behavioural criteria.
This left some diagnostic orphans, none of the criteria for abuse and only one or two in the dependence category.
What changes were made to “alcoholism” in the DSM V (5)?
DSM V (2013)
Factor analyses found that the abuse and dependence criteria actually loaded on a single factor and are interrelated with each other.
The term “addiction” is not applied as a diagnostic term, the more neutral term, “substance use disorder” is used to describe the wide range of the disorder.
How did the American Society of Addiction Medicine explain addiction as of 2011?
Addiction is a primary, chronic disease of brain reward, motivation, memory and related circuitry.
Dysfunction in these circuits leads to characteristic biological, psychological, social and spiritual manifestations.
This is reflected in an individual pathologically pursuing reward and/or relief by substance use and other behaviours.
What were some changes made to the description of substance – related and addictive disorders brought on by the American Society of Addiction Medicine?
Gambling disorder is added.
No longer separates the diagnoses of “abuse” and “dependence”.
Criteria are provided for a “substance use disorder” with severity judged on the number of criteria met.
Also included are criteria for intoxication, withdrawal, substance induced disorders, and unspecified substance related disorders.
The DSM IV “recurrent substance related legal problems” is switched out with “craving, or a strong desire or urge to use a substance”.
A new criteria threshold is in place to establish a substance use disorder…it is now “two or more” criteria. Past abuse was one or more or three or more for dependence.
Cannabis withdrawal and caffeine withdrawal are new disorders.
The DSM IV specifier for “physiological subtype” is eliminated.
The DSM IV diagnosis of “polysubstance dependence” is eliminated.
“Early remission” is defined as “at least three months but less than twelve months” without meeting substance use disorder criteria (except for craving).
“Sustained remission” is defined as at least “twelve months without meeting criteria” (except craving).
Additional Specifiers:
“in a controlled environment”, “on maintenance therapy”
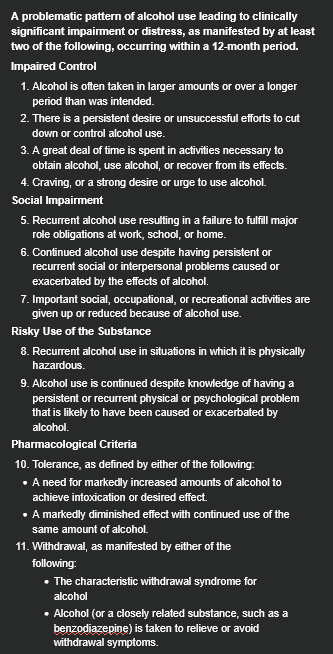
What is the DSM V criteria for a Substance Use Disorder?
A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period.
Impaired Control
Alcohol is often taken in larger amounts or over a longer period than was intended.
There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
Craving, or a strong desire or urge to use alcohol.
Social Impairment
Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school, or home.
Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol.
Important social, occupational, or recreational activities are given up or reduced because of alcohol use.
Risky Use of the Substance
Recurrent alcohol use in situations in which it is physically hazardous.
Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
Pharmacological Criteria
Tolerance, as defined by either of the following:
A need for markedly increased amounts of alcohol to achieve intoxication or desired effect.
A markedly diminished effect with continued use of the same amount of alcohol.
Withdrawal, as manifested by either of the
following:
The characteristic withdrawal syndrome for alcohol
Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
How is the severity of a Substance Use Disorder measured?
Severity is ranges from mild to severe based on the number of symptoms —
Mild: two to three symptoms
Moderate: four to five
Severe: six or more
What are some specifiers for where a person is at in recovery for their addiction?
“in early remission”
“in sustained remission”
“on maintenance therapy”
“in a controlled environment”
What is ‘social impairment’?
Fail to fulfill major roles (work, school, home)
Persistent social or interpersonal problems caused by substance use
Important social, occupational, recreational activities given up or reduced
How is ‘risky use of the substance’ defined?
Use in physically hazardous situations
Use despite physical or psychological problems caused by use
What is ‘substance- specific syndrome’?
Problematic behavioural change due to stopping or reducing prolonged use.
What are some physiological & cognitive components of withdrawal?
Significant distress in social, occupational or other important areas of functioning
Not due to another medical condition or mental disorder
No withdrawal: PCP; other hallucinogens; inhalants
What are ‘Gambling Disorders’?
Term used was “pathological gamblers”
Pathological gambling was added to the DSM in 1980
The criteria was based on clinical experience.
Pathological gambling was listed under “impulse control disorders”.
DSM-IV criteria was revised to reflect it’s similarity to substance dependence.
The National Comorbidity Study Replication verifies that 74% of persons with a gambling disorder meet criteria for another lifetime disorder.
What are some changes the DSM V made to Gambling Disorders?
Reclassifies gambling disorders from impulse control problems as “substance related and addictive disorders”.
Officially changes the name from “pathological gambling” to “gambling disorder”.
Eliminates the criteria: “has committed illegal acts such as forgery, fraud theft or embezzlement to finance gambling”.
Changes “Is preoccupied with gambling” to “Is often preoccupied with gambling”,
Changes “Gambles as a way to escape problems” to “Gambles when feeling distressed”.
Now states that to diagnose a gambling disorder, the criteria are met within a 12 month period. The DSM-IV did not specify a time period.
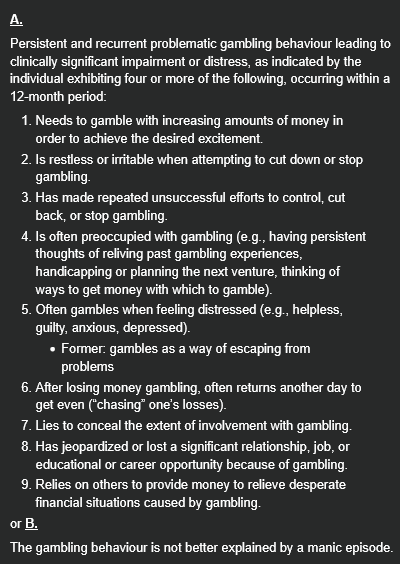
What is the DSM V criteria for a Gambling Disorder?
A.
Persistent and recurrent problematic gambling behaviour leading to clinically significant impairment or distress, as indicated by the individual exhibiting four or more of the following, occurring within a 12-month period:
Needs to gamble with increasing amounts of money in order to achieve the desired excitement.
Is restless or irritable when attempting to cut down or stop gambling.
Has made repeated unsuccessful efforts to control, cut back, or stop gambling.
Is often preoccupied with gambling (e.g., having persistent thoughts of reliving past gambling experiences, handicapping or planning the next venture, thinking of ways to get money with which to gamble).
Often gambles when feeling distressed (e.g., helpless, guilty, anxious, depressed).
Former: gambles as a way of escaping from problems
After losing money gambling, often returns another day to get even (“chasing” one’s losses).
Lies to conceal the extent of involvement with gambling.
Has jeopardized or lost a significant relationship, job, or educational or career opportunity because of gambling.
Relies on others to provide money to relieve desperate financial situations caused by gambling.
or B.
The gambling behaviour is not better explained by a manic episode.
What is the difference between episodic and persistent gambling disorders?
Episodic: Meeting diagnostic criteria at more than one time point, with symptoms subsiding between periods of gambling disorder for at least several months.
Persistent: Experiencing continuous symptoms, to meet diagnostic criteria for multiple years.
What is the criteria for being in early remission of a gambling disorder?
After full criteria for gambling disorder were previously met, none of the criteria for gambling disorder have been met for at least 3 months but for less than 12 months.
To simplify: a person exhibits none of the 9 points of criteria for a gambling disorder (ex: is restless or irritable when attempting to cut down or stop gambling.) for 3 months at minimum, but not more than 12 months.
What is the criteria for being in sustained remission of a gambling disorder?
After full criteria for gambling disorder were previously met, none of the criteria for gambling disorder have been met during a period of 12 months or longer.
To simplify: a person exhibits none of the 9 points of criteria for a gambling disorder (ex: is restless or irritable when attempting to cut down or stop gambling.) for 12 months at minimum, or more.
How is the severity of a Gambling Disorder measured?
Severity is ranges from mild to severe based on the number of symptoms —
Mild: 4–5 criteria met.
Moderate: 6–7 criteria met.
Severe: 8–9 criteria met.
What are some other explanations/diagnoses for gambling that aren’t a gambling disorder?
Non-Disordered Gambling
In professional gambling, risks are limited and discipline is central.
Social gambling typically occurs with friends or colleagues and lasts for a limited period of time, with acceptable losses.
Manic Episode
Loss of judgment and excessive gambling may occur during a manic episode.
In additional diagnosis of gambling disorder should be given only if the gambling behaviour is not better explained by manic episodes.
Personality Disorders
Problems with gambling may occur in individuals with antisocial personality disorder and other personality disorders.
If the criteria are met for both disorders, both can be diagnosed.
Other Medical Conditions
Some patients taking dopaminergic medications (e.g., Parkinson‘s disease) may experience urges to gamble.
If such symptoms dissipate when dopaminergic medications are reduced in dosage or ceased, then a diagnosis of gambling disorder would not be indicated.
What is ‘neuroadaptation’?
Refers to underlying CNS changes that occur following repeated use such that person develops tolerance and/or withdrawal
Pharmacokinetic: adaptation of metabolizing system
Pharmacodynamic: ability of CNS to function despite high blood levels
What is ‘tolerance’?
Need to use an increased amount of a substance in order to achieve the desired effect
OR
Markedly diminished effect with continued use of the same amount of the substance
What is ‘etiology’?
Multiple interacting factors influence using behaviour and loss of decisional flexibility
Not all who become dependent experience it same way or motivated by same factors
Different factors may be more or less important at different stages (drug availability, social acceptance, peer pressure VS personality and biology)
Where are substance use and gambling disorders treated?
Hospitalization
Due to drug OD, risk of severe withdrawal, medical comorbidities, requires restricted access to drugs, psychiatric illness with suicidal ideation
Residential Treatment Unit
No intensive medical/psychiatric monitoring needs
Require a restricted environment
Partial hospitalization
Outpatient Program
No risk of med/psych morbidity and highly motivated patient
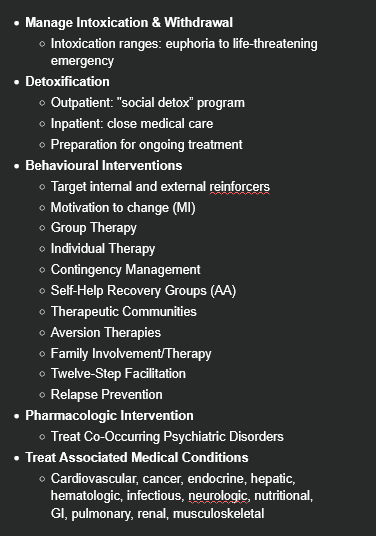
How are substance use and gambling disorders treated?
Manage Intoxication & Withdrawal
Intoxication ranges: euphoria to life-threatening emergency
Detoxification
Outpatient: "social detox” program
Inpatient: close medical care
Preparation for ongoing treatment
Behavioural Interventions
Target internal and external reinforcers
Motivation to change (MI)
Group Therapy
Individual Therapy
Contingency Management
Self-Help Recovery Groups (AA)
Therapeutic Communities
Aversion Therapies
Family Involvement/Therapy
Twelve-Step Facilitation
Relapse Prevention
Pharmacologic Intervention
Treat Co-Occurring Psychiatric Disorders
Treat Associated Medical Conditions
Cardiovascular, cancer, endocrine, hepatic, hematologic, infectious, neurologic, nutritional, GI, pulmonary, renal, musculoskeletal
True or False: 50% of patients with substance–related and addictive disorders will have another psychiatric disorder.
True.