Introduction to Immunohematology
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
84 Terms
Encompasses activities, procedures, and testsdone to ensure that blood for transfusion is properly collected, preserved, stored, and dispensed for later use in blood transfusion
Blood Banking
is a multidisciplanary branch of medicine concerned with the transfusion of blood and blood components, including proper selection and utilization of blood components as well as removal of blood components in the treatment or prevention of disease
Transfusion Medicine
History of Transfusion Medicine
1492
First recorded unsuccessful blood transfusion
Donors were three young men in the hope of curing the stricken Pope Innocent VII
History of Transfusion Medicine
1628
William Harvey > English physician, discovered the circulation of blood
History of Transfusion Medicine
1665
The first recorded successful blood transfusion occurs in England
Physician Richard Lower > kept dogs alive by transfusion of blood from other dogs
History of Transfusion Medicine
1818
James Blundell > a british obstetrician performs the first successful transfusion of human blood to a patient for the treatment of postpartum hemorrhage
History of Transfusion Medicine
1840
Samuel Armstrong Lane> At St. George's School in London, aided by consultant Dr. Blundelll performs the first successful whole blood transfusion to treat hemophilia
History of Transfusion Medicine
1867
Joseph Lister > English surgeon, used antiseptics to control infection during transfusions
History of Transfusion Medicine
1869
Braxton Hicks > recommended sodium phosphate in an attempt to find a non-toxic anticoagulant as clotting was the principal obstacle to overcame
History of Transfusion Medicine
1873 to 1880
US physicians transfuse milk from cows, goats, and humans
History of Transfusion Medicine
1884
Saline infusion replaces milk as a blood substitute due to the increased frequency of adverse reactions to milk
History of Transfusion Medicine
1901
Karl Landsteiner > an Austrian physician, discovered the ABO blood groups
He received the Nobel Prize for Medicine for this discovery in 1930
History of Transfusion Medicine
1902
Alfred Decastello and Adriano Sturli, Landsteiner's colleagues, add AB blood group
History of Transfusion Medicine
1907 - Hektoen
suggests that the safety of transfusion might be improved by crossmatching blood between donors and patients to exclude incompatible mixtures
History of Transfusion Medicine
1907 - Reuben Ottenberg
performs the first blood transfusion with performed blood typing and crossmatching in Newyork
also observed the mendelian inheritance of blood groups and recognized the universal utility of group ) donors
History of Transfusion Medicine
1908 - Alexis Carrel
Alexid Carrel > French surgeon, devised a way to prevent clotting by sewing the vein of the recipient directly to the vein of the donot
This vein-to-vein or direct method known as ANASTOMOSIS was practiced by a number of physicians
Among them, J.B. Murphy in Chicago and George Crile in Clevelans
The procedure was proved unfeasible for blood transfusion but paved the way for successful organ transplantation for which Carrel received the Nobel Prize in 1912
History of Transfusion Medicine
1908 - Moreschi
Describes the antiglobulin reaction
The antiglobulin is a direct way of visualizing an antigen-antibody reaction that has taken place but is not directly visible
The antigen and antibody react with each other, them after washing to remove any unbound antibody, the antiglobulin reagent is added and binds between the antibody molecules that are stuck onto the antigen
This makes the complex big enough to see
History of Transfusion Medicine
1912
Roger Lee > a visiting physician at the Massachusetts General Hospital, along with Paul Dudley White develops the Lee-White clotting time
Lee demonstrates that is is safe to give group O blood to patients of any blood group and that blood from all groups can be given to group AB patients
The terms universal donor and universal recipient are coined
History of Transfusion Medicine
1913
Edward Lindemann > Vein-to-vein blood transfusion was carried out using multiple syringes and a special cannula for puncturing the vein through the skin
History of Transfusion Medicine
1914
Hustin > reported the use of sodium citrate as anticoagulant allowing longer preservation of blood
History of Transfusion Medicine
1915
Richard Lewisohn > used sodium citrate as an anticoagulant to transform the transfusion procedure from direct to indirect
Richard Weil > demonstrated the feasibility of refrigerated storage of such anticoagulated blood
History of Transfusion Medicine
1916
Francis Rous and J.R. Turner > introduced a citrate-glucose solution that permits storage of blood for several days after collection
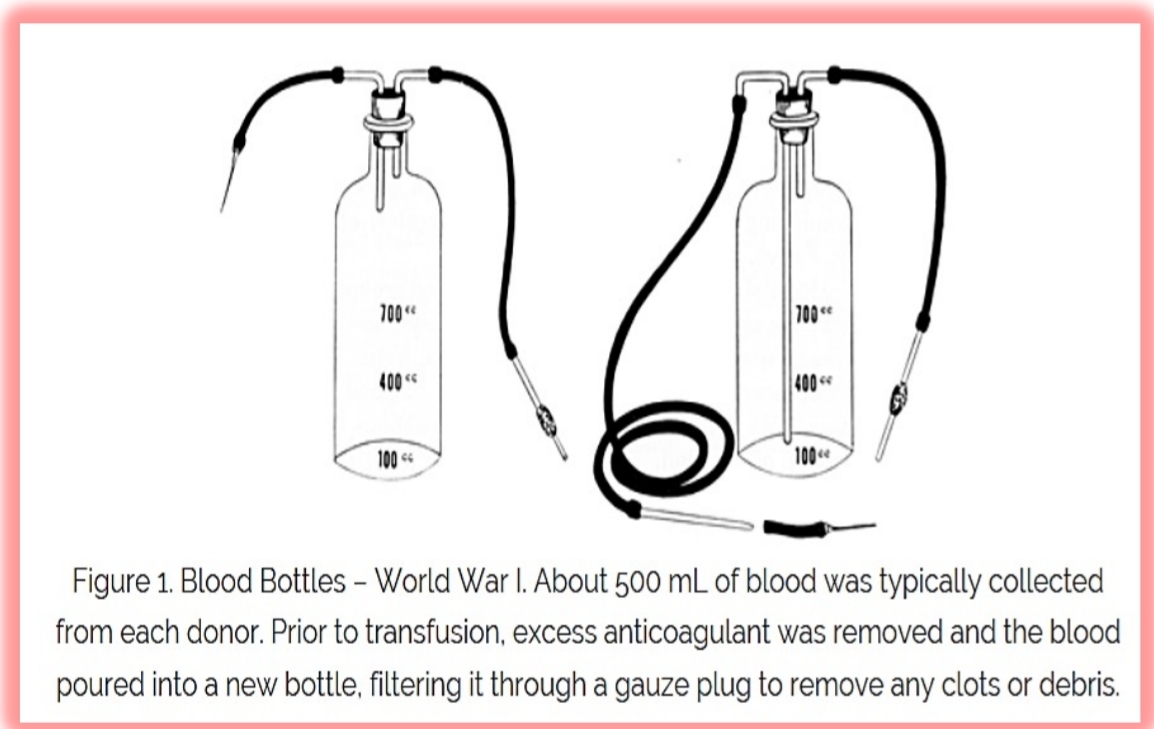
Oswald Robertson > an American Army Officer, was credited with creating the blood depots, he received the AABB LAndsteiner Award in 1958 as developer of the first blood bank
History of Transfusion Medicine
1927 to 1947
The MNSs and P systems are discovered
History of Transfusion Medicine
1939/1940
The Rh blood group system was discovered by Karl Landsteiner, Alex Wiener, Philip Levine, and R.E. Stetson and was soon recognized as the cause of majority of transfusion reactions
History of Transfusion Medicine
1940
The United States government established a nationwide program for the collection of blood
Charles R. Drew > developed the “Plasma for Britain” Program which is a pilot project to collect blood for shipment to the British Isles
The American Red Cross participated, collecting 13 million units of blood by the end of World War II
History of Transfusion Medicine
1941
Dr. Drew > appointed director of the first american Red Cross Blood Bank at Presbyterian Hospital
History of Transfusion Medicine
1943
J.F. Loutit and Patrick L. Mollison > introduce acid citrate dextrose (ACD) solution
P. Beeson > published the classic description of transfusion-transmitted hepatitis
History of Transfusion Medicine
1945
Coombs, Mourant, and Race > described the use of antihuman globulin (later known as Coombs Test) to identify “incomplete” antibodies
History of Transfusion Medicine
1947
The American Association of Blood Banks (AABB) was formed to promote common goals among blood banking practitioners and the blood donating public
History of Transfusion Medicine
1949 to 1950
The US blood collection system include 1,500 hospital blood banks, 46 community blood centers, and 31 American Red Cross regional blood centers
History of Transfusion Medicine
1950
Audrey Smith > reported the use of glycerol cryoprotectant for freezing red blood cells
Carl Walter and W.P. Murphy Jr. > introduced the plastic bag for blood collection
History of Transfusion Medicine
1953
Development of refrigerated centrifuge further expedited blood component therapy
History of Transfusion Medicine
1957
The AABB formed its committee on Inspection and Accreditation to monitor the implementation of standards for blood banking
History of Transfusion Medicine
1958
The AABB published its first edition of Standards for a Blood Transfusion Service (now titled as Standards for Blood Banks and Transfusion Services)
History of Transfusion Medicine
1960
The AABB begins publication of TRANSFUSION, the first American journal wholly devoted to the science of blood banking and transfusion technology
History of Transfusion Medicine
1957
Gibson > introduced an improved preservative solution called CPD (a less acidic anticoagulant)
History of Transfusion Medicine
1959
Max Perutz > from Cambridge University deciphered the molecular structure of hemoglobin, the molecule that transports oxygen and gives red blood cells their color
History of Transfusion Medicine
1960
A. Solomon and J.L. Fahey > reported the first therapeutic plasmapheresis procedure (a procedure that separates whole blood into plasma and red blood cells
History of Transfusion Medicine
1979
A new anticoagulant preservative, CPDA-1, extends the shelf life of whole blood and red blood cellls to 35 days, increasing the blood supply and facilitating resource sharing among blood banks
History of Transfusion Medicine
1983
Additive solutions extend the shelf life of red blood cells to 42 days
Traditionally, the amount of whole blood in a unit has been _ of blood
More recently, _ of blood are being collected
450 mL ± 10%
500 mL ± 10%
Units of whole blood collected can be separated into three components: (3)
packed RBCs, platelets, and plasma
In recent years, less whole blood has been used to prepare platelets with the increased utilization of _
apheresis platelets
Whole blood-prepared RBCs may be stored for _ to _ days
21 to 42 days
Donated blood is free but a fee is still charged for each unit to cover the cost associated with (4)
collection, storage, testing, and transfusion
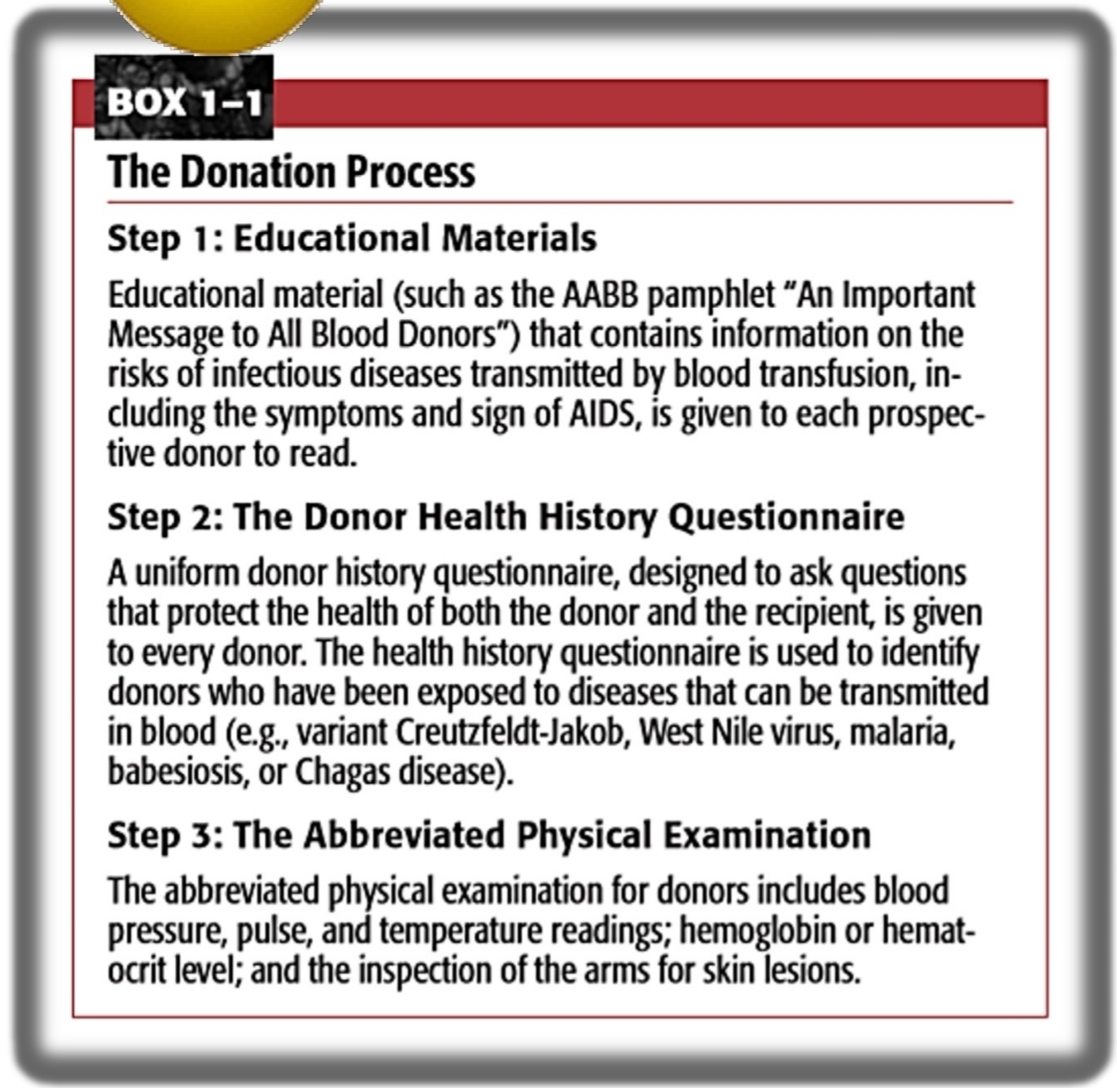
The Donation Process
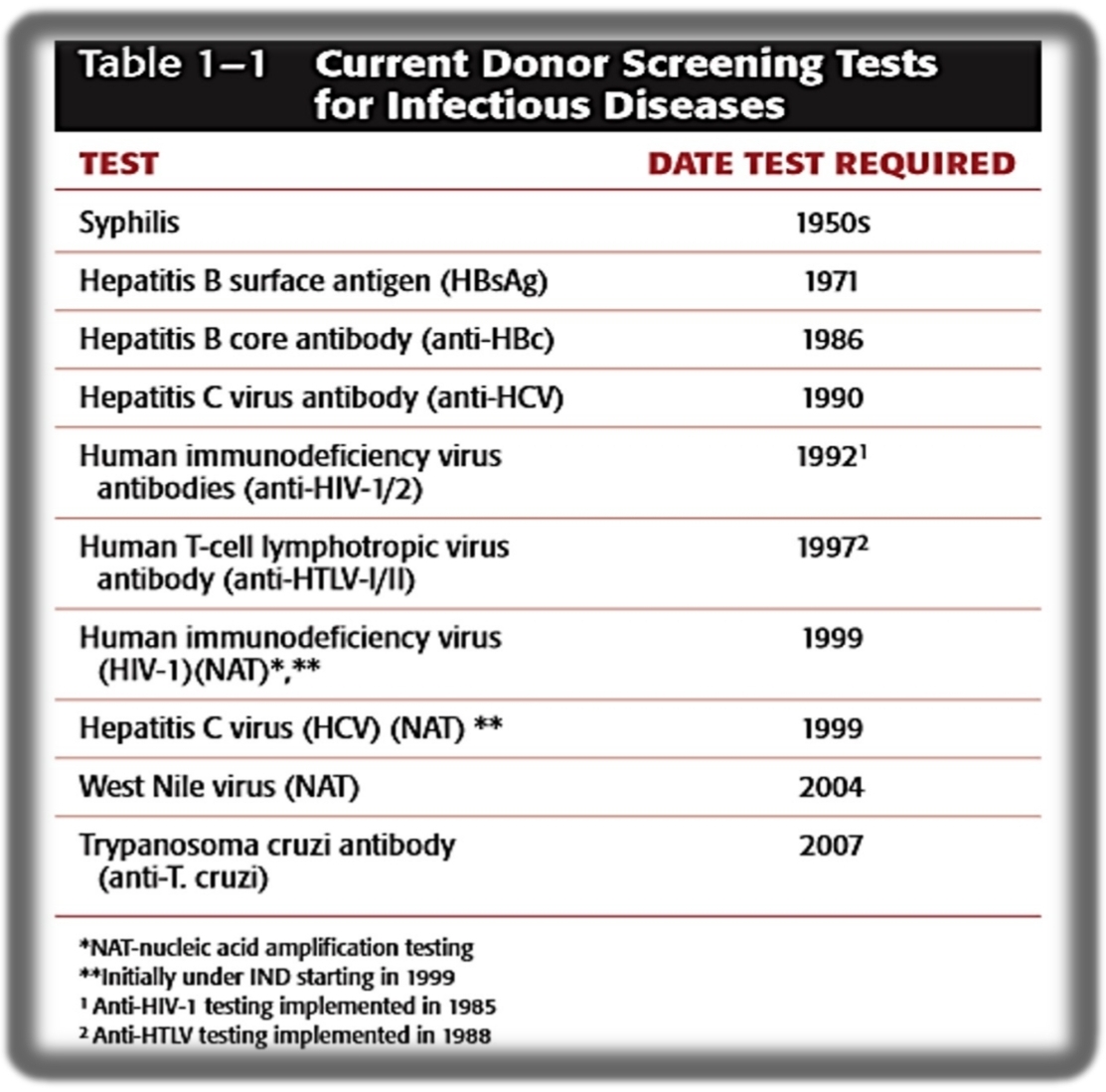
Current Donor Screening Test for Infectious Diseases
Three areas of RBC biology are crucial for normal erythrocyte survival and function:
Normal chemical composition and structure of the RBC membrane
Hemoglobin structure and function
RBC metabolism
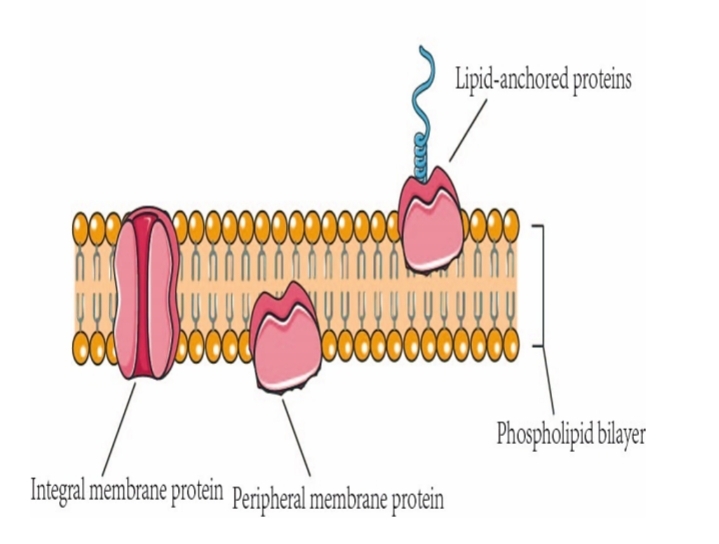
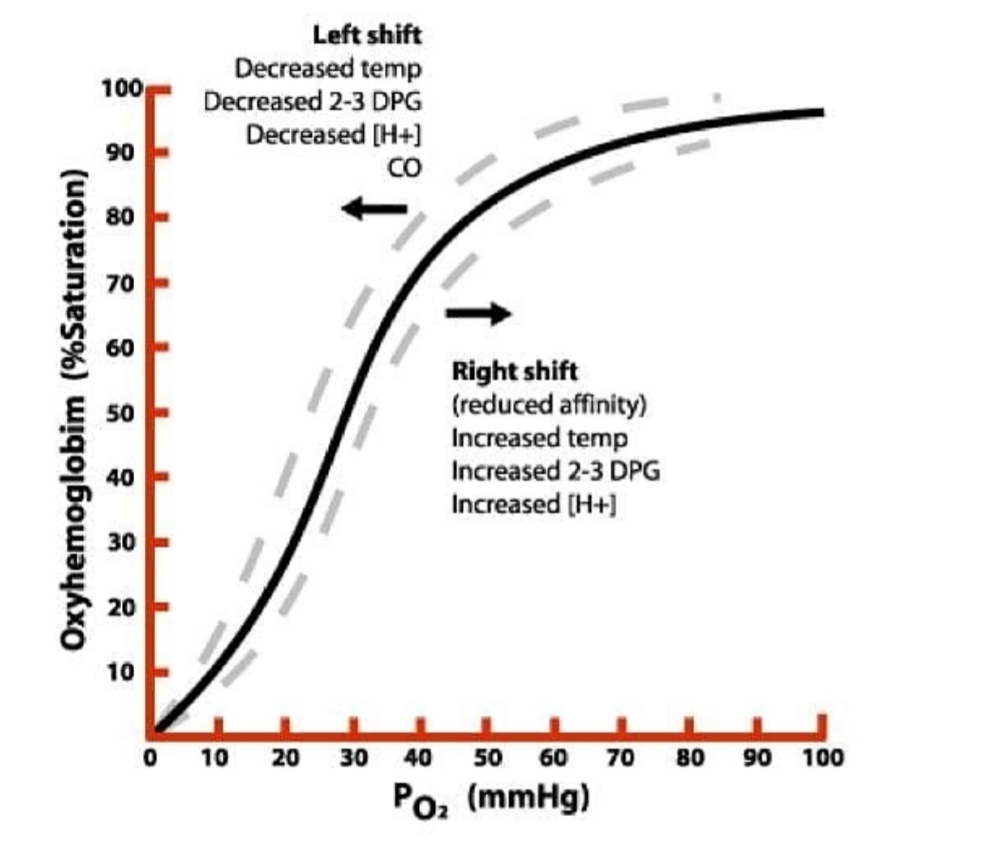
RBC membrane is a semi-permeable lipid bilayer supported by a mesh-like protein cytoskeleton structure
Biochemical composition:
52% protein
40% lipid
8% carbohydrates
RBC membrane
_ extend from the outer surface and span the entire membrane of the inner cytoplasmic side of RBC
Integral Membrane Proteins
RBC membrane
_ > located and limited to the cytoplasmic surface of the membrane; form the RBC cytoskeleton
Peripheral Proteins
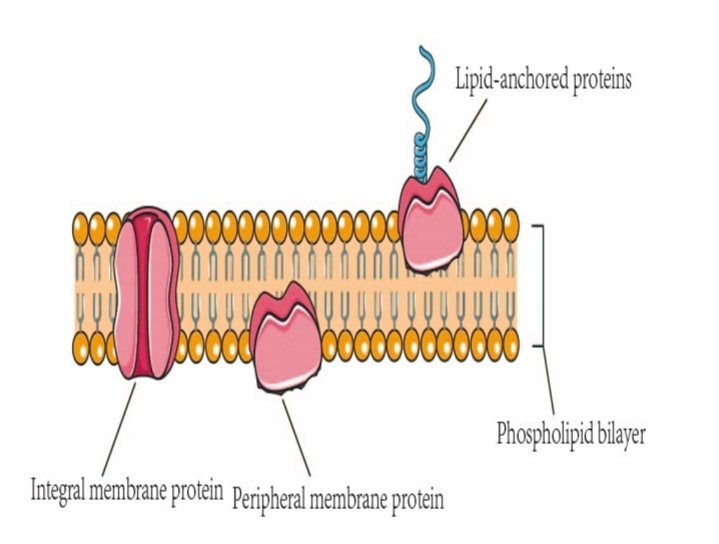
Integral and Peripheral Proteins
The normal chemical composition, structural arrangement and molecular interactions of the erythrocyte membrane are crucial to the normal length of RBC survival in the circulation and in RBC's two important characteristics:
Deformability
Permeability
DEFORMABILITY
To remain viable, nrmal RBCs must also remain flexible, deformable, and permeable
The loss of ATP levels leas to decrease in _ and in turn a loss of membrane deformability
An accumulation or increase in deposition of membrane _ also results, causing an increase in membrane rigidity and loss of pliability
phosporylation of spectrin
calcium
PERMEABILITY
The permeability properties of the RBC membrane and the active _ prevent colloid hemolysis and control the volume of RBC
RBC IC to EC ratios of Na+ and K+: _
When RBCs are ATP-depleted, Ca2+ and Na+ accumulate intracellularly and and are lost > dehydrated and rigid cell subsequently sequested by the spleen
RBC cation transport
1:12 (Na+) and 25:1 (K+)
K+ and H2O
Primary function is as transport: O2 delivery to tissues and CO2 excretion
Hemoglobin
Hemoglobin molecule is composed of four subunits, each containing heme and globin:
1 heme = 1 mole of O2
1 Hb molecule = 4 moles of O2
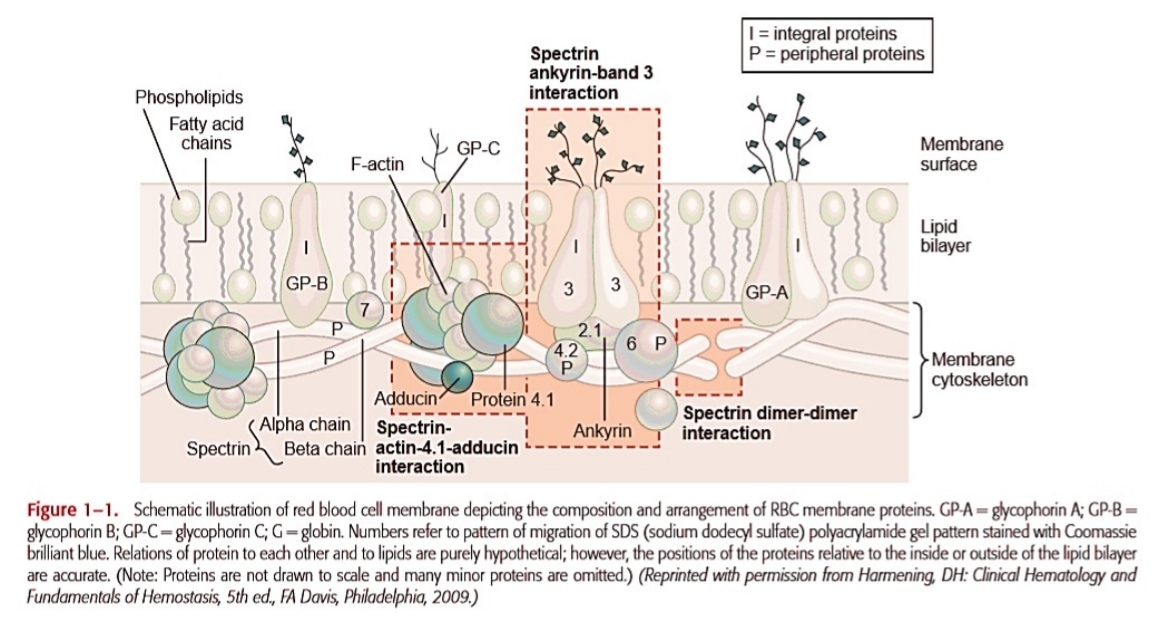
One of the most important controls of hemoglobin's affinity for oxygen is _
2,3-DPG (diphosphoglycerate or biphosphoglycerate)
Graphically describes the relationship between oxygen content of hemoglobin (% of saturation) and the partial pressure of O2 (PO2)
Oxygen Dissociation Curve - As 𝑃𝑂2 increases, hemoglobin's affinity for oxygen increases, causing a rapid rise in saturation, which then plateaus at higher pressures.
Normal shape of the curve is _
sigmoid
Oxygen Dissociation Curve
Shift to the LEFT
Increased Hb affinity for O2, decreased delivery of O2 to tissues
Increased pH
Decreased 2,3-DPG, CO2, and temperature
Oxygen Dissociation Curve
Shift to the RIGHT
Decreased Hb affinity for O2, increased delivery of O2 to tissues
Decreased pH
Increased 2,3-DPG, CO2, and temperature
RBC Metabolic Pathways
Anaerobic Glycolytic Pathway
→Embden-Meyerhof Pathway
Ancillary Pathways
→Pentose Phosphate Pathway / HMP - prevents denaturation of hemoglobin by oxidation
→Methemoglobin Reductase Pathway - Heme iron is constantly exposed to oxygen and peroxides. Peroxide oxidizes heme iron from the ferrous (2+) to the ferric (3+) state (methemoglobin); maintains iron in heme in its reduced form (Fe+2). This pathway Converts methemoglobin back to normal hemoglobin using the methemoglobin reductase enzyme which makes it a corrective mechanism
→Leubering-Rapoport Shunt - generates 2,3 - DPG
Blood collection is a _ system consisting of main bag with needle, tubing, and up to four satellite bags attached
The entire system is sterile
closed system
How many mL of blood is taken in blood collection
450 mL ± 45 mL (with 63 mL anticoagulant) or 500 mL ± 50 mL (with 70 mL anticoagulant)
Blood Preservation
Component of anticoagulant used in blood donation (4)
adenine - used in ATP synthesis
citrate - binds calcium to prevent coagulation
dextrose - food for cells
phosphate - source of 2,3-DPG which promotes oxygen release to tissues
4 anticoagulant sued in blood banking
ACD: Acid-Citrate-Dextrose (21 days)
CPD: Citrate-Phosphate-Dextrose (21 days)
CP2D: Citrate-Phosphate-Double Dextrose (21 days)
CPDA-1: Citrate-Phosphate-Dextrose-Adenine (35 days)
Biochemical changes in stored blood that can lead to decreased RBC viability
lesions of storage
Lesions of Storage
(5) decrease as RBCs are stored
After cells are transfused, (2) are restored in about 24 hours
Glucose, ATP, 2,3-DPG, pH, plasma sodium
ATP and 2,3-DPG
Lesions of Storage
Substances that increase during storage include (4)
plasma hemoglobin
plasma potassium
ammonium
lactic acid
These are added to RBCs after removal of plasma with or without platelets
Additive Solutions
Additive solutions contain _
MAGS
Mannitol
Adenine
Glucose
Saline
Additive solutions must be added within _
72 hours
Additives extend their shelf life to _ and reduce RBC viscosity during transfusion
42 days
Freezing of RBCs is primarily used for (2)
autologous units
storage of rare blood types
Freezing of RBCs
Cryoprotective agent is added to RBCs that are less than _ old
6 days
allows individual to donate blood for their own use in meeting their needs for blood transfusion
Autologous transfusion
auto meaning self
Advantages of Freezing RBCs (4)
Long term storage (10 years)
Maintenace of RBC viability and function
Low residual leukocytes and platelets
Removal of significant amounts of plasma proteins
Disadvantages of Freeezing RBCs
Time-consuming process
Higher cost of equipment and materials
Storage requirements (-65 °C)
Higher cost of product
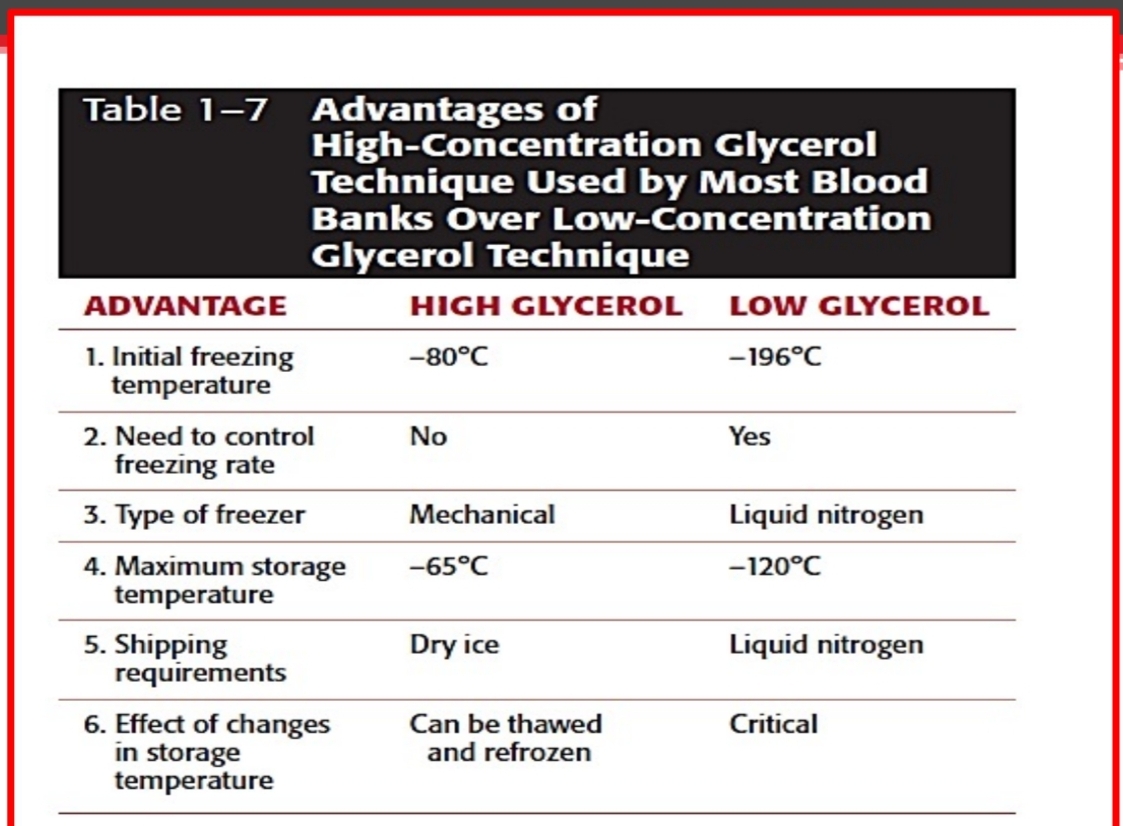
Advantages of HIgh-Concentration Glycerol Technique Used by Most Blood Banks Over Low-Concentration Glycerol Techniques
These are used to restore ATP and 2,3-DPG levels before freezing or transfusing a unit, and may be necessary for autologous or rare units
Rejuvenation Solutions
Rejuvenation Solutions contain _
PIGPA
Phosphate
Inosine
Glucose
Pyruvate
Adenine
Current Trends in RBC Preservation Research
Development of improved additive solutions
Development of procedures to reduce and inactivate the
level of pathogens that may be in RBC unitsDevelopment of procedures to convert A-, B-, and ABtype RBCs to O-type RBCs
Development of methods to produce RBCs through
bioengineering (blood pharming)Development of RBC substitutes
Current Trends in Platelet Preservation Research
Development of methods that would allow platelets to
be stored for 7 daysDevelopment of additive solutions, also termed synthetic
mediaDevelopment of procedures to reduce and inactivate the
level of pathogens that may be in platelet unitsDevelopment of platelet substitutes
New approaches for storage of platelets at 1°C to 6°C
The development of processes to cryopreserve platelets