Echo - Test 1
1/154
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
155 Terms
location of the heart
lies posterior to sternum within middle mediastinum
where does the heart lie?
45 degree angle, between third and fifth intercostal spaces
apex
constitutes the cone or bottom of the heart and rests on the diaphragm below the seventh rib
what does the apex consist of?
tip of the LV
position of the heart
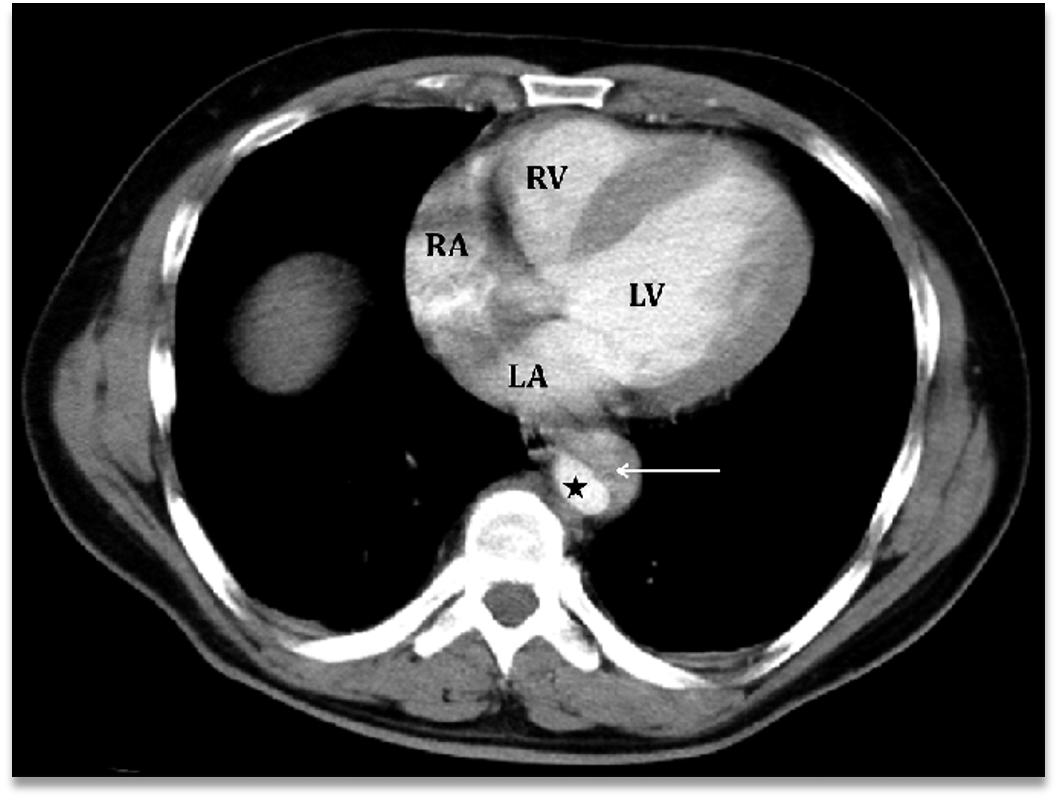
superior border of the heart
RA & LA
inferior (diaphragmatic) border of the heart
almost entirely RV and portion of the LV
right border of the heart
RA
left border of the heart
LV & small portion of LA
anterior border of the heart
almost entirely RV and small portions of RA & LV
posterior border of the heart
LA & LV
pericardium
thin sac that houses the heart and roots of the great vessels
what are the two layers of the pericardium?
parietal and visceral
pericardial cavity
space between the parietal and visceral layers of the pericardium
pericardium
contains serous fluid that lubricates the 2 layers as the heart beats
IV sulcus
separates RV from LV externally
AV sulcus
separates LA from LV externally
coronary sulcus
separates RA from RV externallys
sulcus terminalis
separates anterior and posterior portions of RA
crux
located at posterior portion of heart where all four chambers come together; determines dominance of heart by which coronary artery feeds this portion; Rt dominate is fed by RCA
epicardium
outermost layer of the heart
AKA the visceral layer of the pericardium
composed of epithelial cells
myocardium
middle layer
composed of involuntary muscle fibers and muscle cells
responsible for contraction
endocardium
innermost layer of the heart
lines the inside of the myocardium
covers the valves and tendons
composed of simple squamous epithelial cells
continuous with endothelial lining of the large blood vessels and vascular system
KNOW THIS
interatrial septum
located between LA and RA; prevents mixing of oxygenated and deoxygenated blood
interatrial septum can be divided into 3 regions where defects occur:
sinus venosus
septum secundum
septum primum
sinus venosus
located at the junction of the SVC & IVC with atrium
septum secundum
located at the mid portion
foramen ovale - prenatal opening to allow for fetal circulation
fossa ovalis - postnatally the foramen ovale closes and becomes the fossa ovalis
septum primum
located at the endocardial cushion level (AV valves)
interventricular septum
located between the RV and LV and prevents mixing of oxygenated and deoxygenated blood
what are the two portions of the IVS?
membranous portion & muscular portion
membranous IVS
located between outflow tracts; made up of a thin membrane
muscular IVS
from the membranous portion of the apex
coronary sinus
drains blood from the myocardium
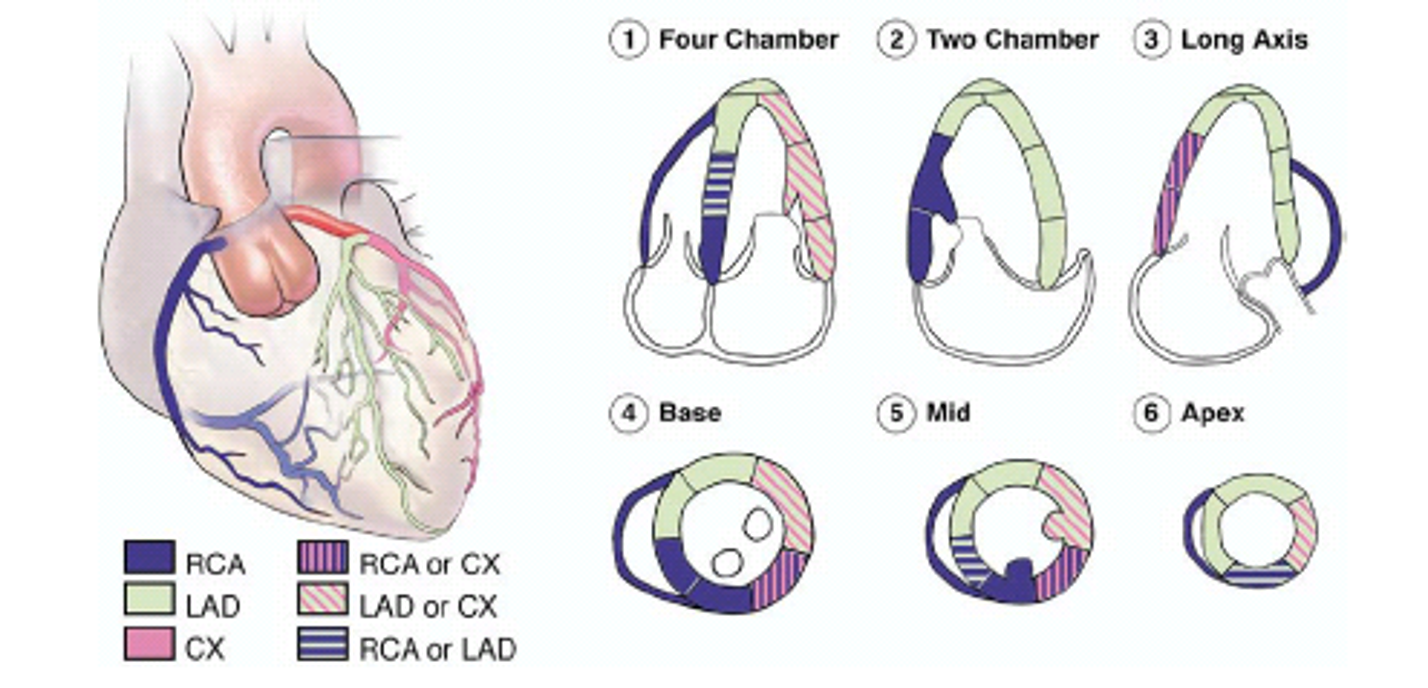
coronary artery system
supplies oxygenated blood to heart muscle
coronary artery system
located on external surface of the heart, between the epicardium and myocardium
sinuses of valsalva
RCA & LCA originate here just above the aortic valve; very common to have variations in branching
left coronary artery
begins with left main, arising from the left coronary cusp » branches into left anterior descending (LAD) and left circumflex (LCX)
left anterior descending artery
follows the AV sulcus and feeds the anterior wall of the LV, apex, and portions of the septum, as well as the right and left bundle branches of the conduction system
has septal perforators of the conduction system
left circumflex artery
follows the coronary sulcus to lateral and posterior portion of LV
feeds the SA node (45%), AV node (20%), and Bundle of HIS (10%)
has obtuse marginals
right coronary artery
arises from the RT coronary cusp at the sinuses of valsalva and runs through the coronary sulcus to the RV
RCA
feeds the RA, RV, inferior portion of the LV, and a portion of the ventricular septum
feeds the SA node (55%), AV node (80%), and Bundle of HIS (90%)
has acute marginal branches
RCA
distal portion gives rise to posterior descending artery which feeds crux and runs down posterior portion of the IV sulcus
coronary artery wall distribution
sinoatrial node (SA)
native pacemaker of the heart located within the sulcus terminalis at the confluence of the SVC, RA appendage and the lateral wall of the RA
SA node
initiates the cardiac cycle and has inter-nodal pathways and the Bachman’s bundle feeds the RA
responsible for initiating and stimulation atria (rate of 60-100 bpm)
atrioventricular (AV) node
located in the medial floor of the RA and delays impulse to allow for ventricular filling (40-60 times per minute)
transducer windows
suprasternal: suprasternal notch
subcostal: body midline beneath costal margin
apical: over cardiac apex
parasternal: over area bounded superiorly by left clavicle, medially by sternum, inferiorly by apical region
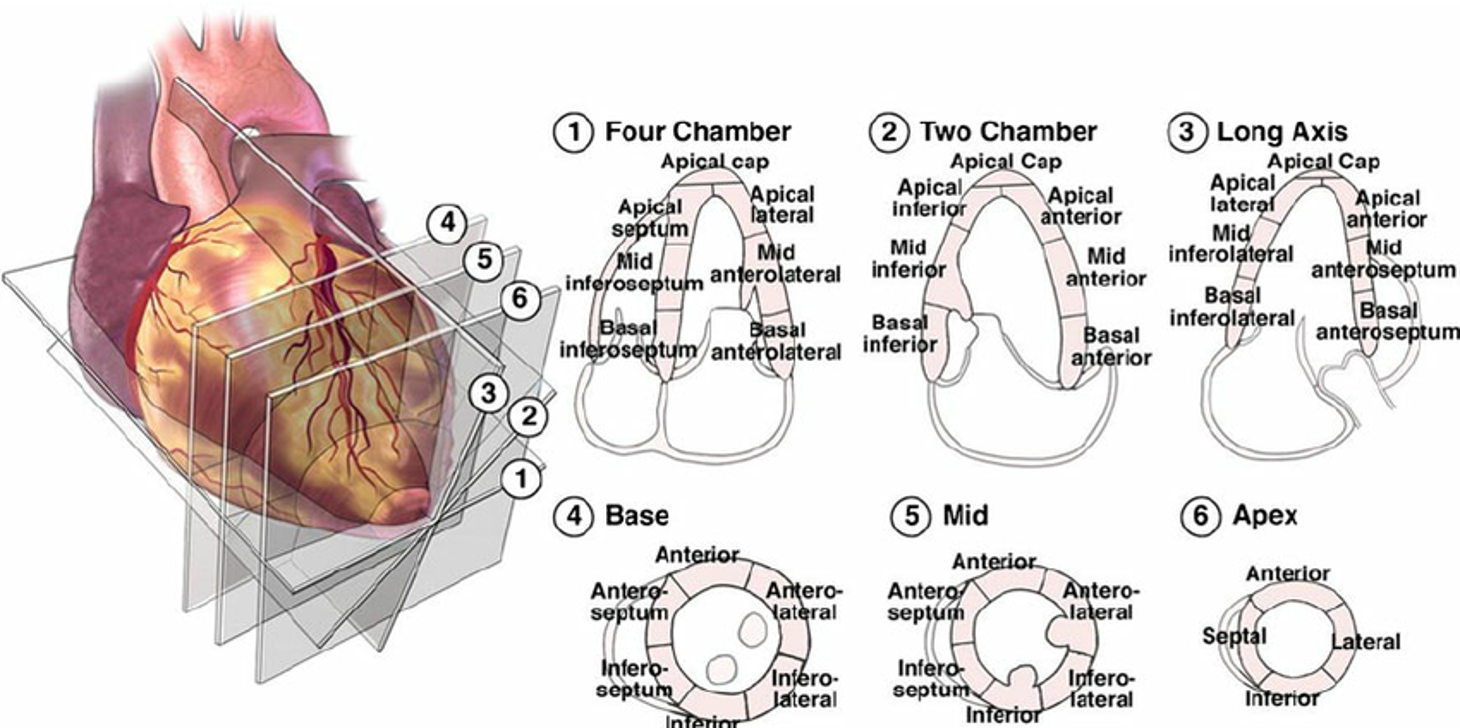
parasternal views
PLAX: LV in sag, RV inflow, LV outflow
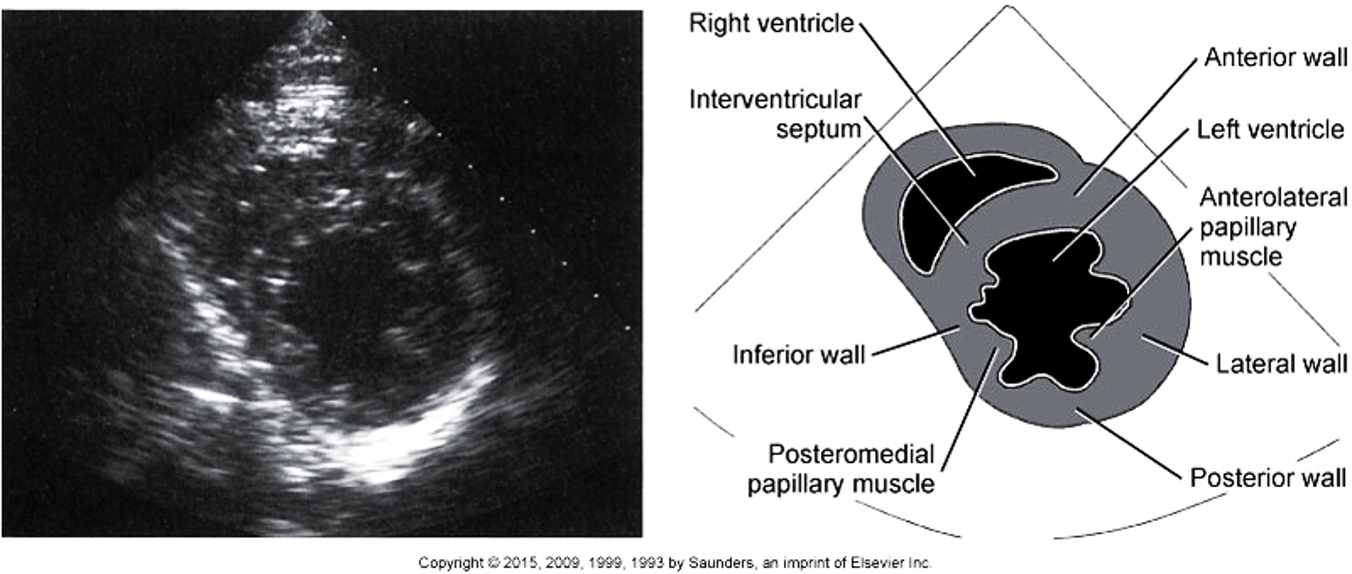
PSAX: LV apex, LV mid @ pap muscles, MV, AV/TV/RVOT/PV (basal view)
PLAX
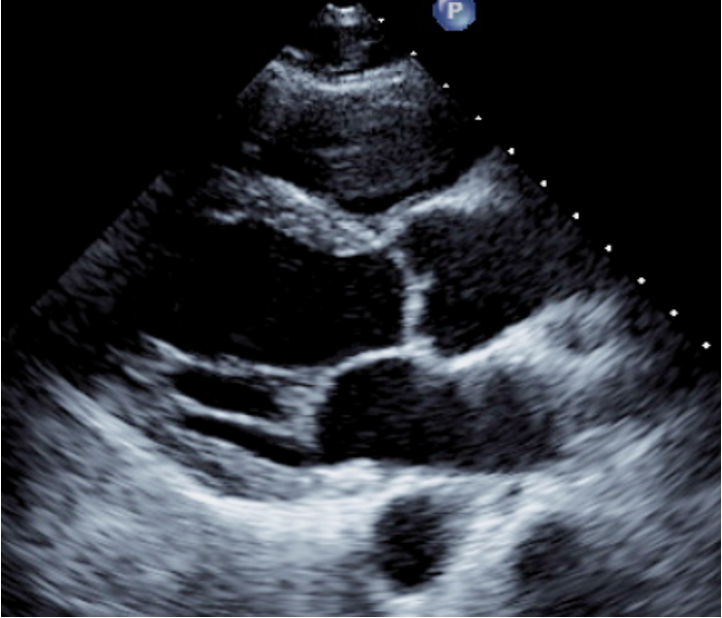
PSAX
apical views
4C
5C
2C
apical long (3C)
subcostal views
4C
IVC
PSAX LV
additional: PSAX MV & PSAX AV
suprasternal notch (SSN)
ascending aorta
descending aorta
right pulmonary artery
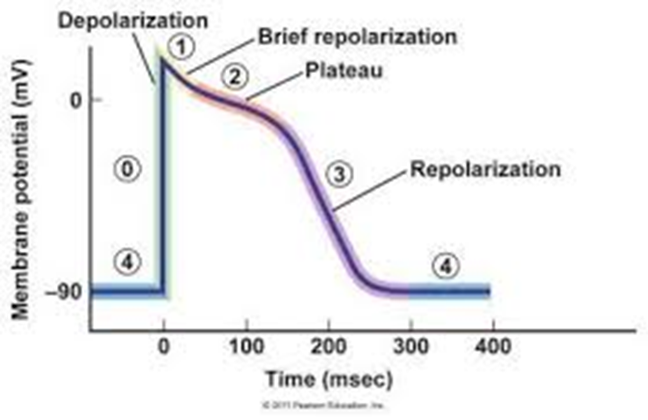
phase 0 (depolarization)
channels are opened with stimulation and a rapid influx of sodium enters the cell, making the cell more positive on the inside than on the outside
happens at the onset of the QRS interval on the EKG
phase 1
gating mechanisms close and the entry of sodium slows down, making the interior of the cell less positive
phase 2
sodium is no longer entering the cell through fast channels » calcium is entering through slow channels, determining the degree of contraction
phase 3 (repolarization)
potassium ions exit the cell making the inside more negative
phase 4 (refractory period)
sodium is transported from inside to outside of the cell and potassium is brought back inside the cell » the cells can be stimulated again once they reach the threshold potential
phases curve
p wave
atrial depolarization
hidden in the QRS complex
atrial repolarization
QRS
ventricular depolarization
t wave
ventricular repolarization
phases of the cardiac cycle
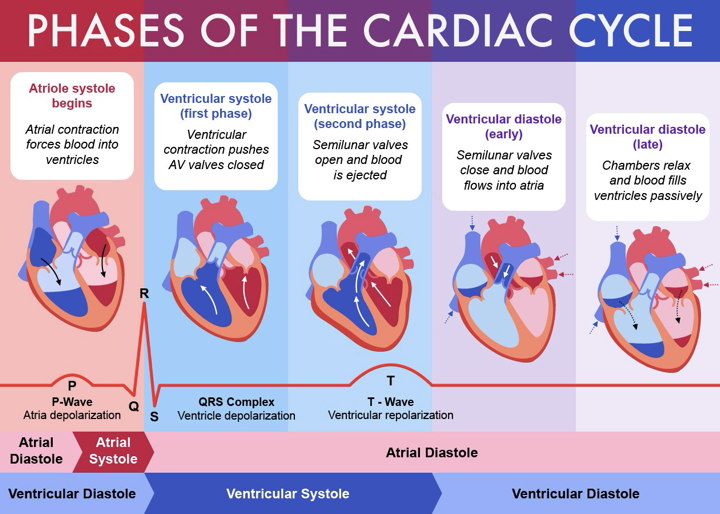
ventricular diastole » isovolumetric relaxation
after ejection of blood through the semilunar valves, they close; for a brief moment, all 4 valves are closed » repolarization of the ventricles initiates relaxation (t wave)
isovolumetric relaxation
ventricles continue to relax, volume is constant and pressure is decreasing
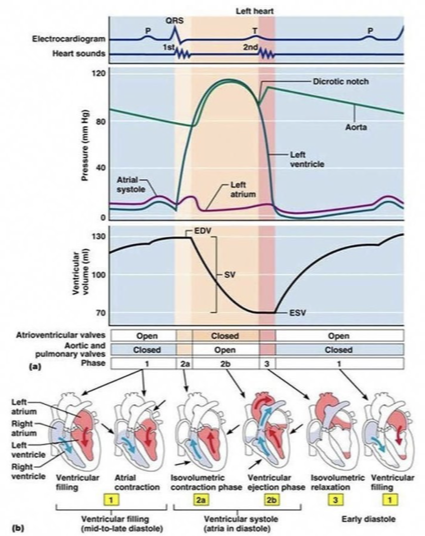
what does 3 on the diagram represent?
isovolumetric relaxation
ventricular diastole - ventricular filling
AV valves open and blood begins to move from LA to LV because ventricular pressure drops below the atrial pressure; semilunar valves are closed
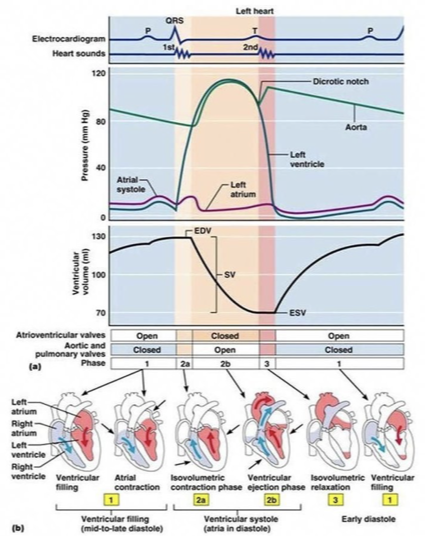
what is 1 on the diagram?
ventricular filling
three phases of ventricular filling
rapid ventricular filling (early diastole - MV E wave)
diastasis - flow slows because AV pressures have equalized
slow filling (atrial kick or contraction - MV A wave): SA node sends impulse and atria contract (P wave)
ventricular systole - isovolumetric contraction
near the end of atrial systole, the impulse from the SA node has passed through the AV node and into the ventricles causing them to depolarize (QRS complex) » contraction begins and blood is pushed up against the AV valves, forcing them to shut » for about 0.05 seconds all 4 valves are closed
isovolumetric contraction
as contraction continues, volume is constant and pressure is increasing
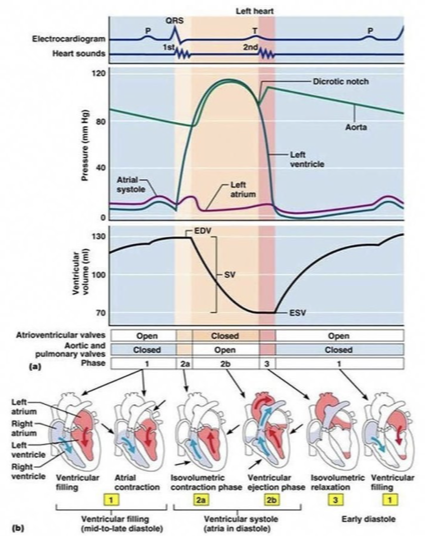
what is 2a on the diagram?
isovolumetric contraction
ventricular systole - ventricular ejection
when LV pressure surpasses the aortic pressure and the RV pressure surpasses the PA pressure, the semilunar valves open and blood is ejected from the heart » lasts about 0.25 seconds
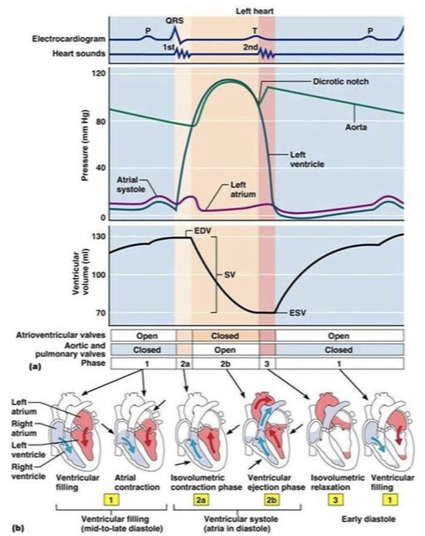
what is 2b on the diagram?
ventricular ejection
end systolic volume (ESV)
the volume of blood remaining in the ventricles after systole (about 50-60 mL)
stroke volume (SV)
the amount of blood ejected per beat » typically around 70 mL
SV
EDV - ESV
preload
the stretch of the heart before it contracts
the greater the preload…
the greater the force of contraction » the more the heart is filled during diastole, the greater the force of contraction during systole (Frank-Starling law of the heart)
contractility
the forcefulness of the contraction
afterload
the pressure that must be exceeded for LV contraction » ejection of blood begins when the pressure in the RV/LV exceeds the pressure of the aorta/PA; dependent on systemic and pulmonary vascular resistance
common indications for an echo - signs & symptoms
enlarged heart
murmur
chest pain
heart failure
fever or bacteremia
shortness of breath
palpations
syncope/presyncope
TIA, stroke or peripheral embolic event
arrhythmias: A-fib, SVT, VT, etc.
common indications for an echo - known cardiac diagnoses
valvular heart disease
hypertension
heart failure
cardiomyopathy
aortic disease
cardiac masses
pericardial disease
congenital heart disease
coronary artery disease (CAD)
pulmonary hypertension
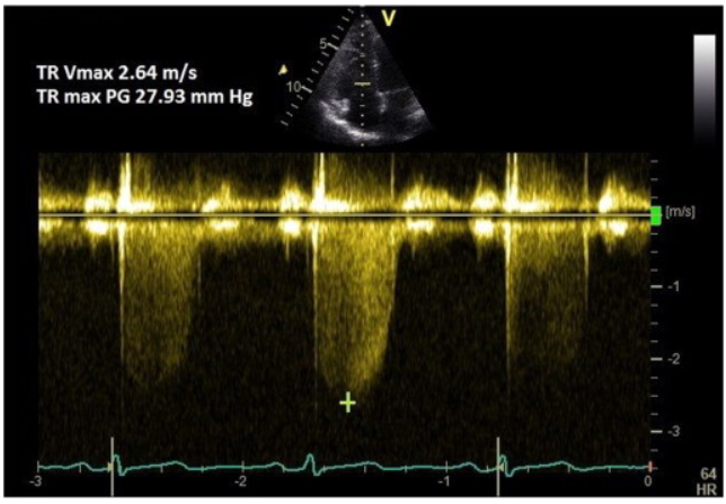
doppler equation (fd)
2/c x v x ft x cos angle
c
propagation speed of sound in the medium
v
speed of moving interface (blood)
ft
frequency of transmitted (original) sound wave
cos angle
cosine of the angle of incidence between transmitted sound wave and particle (RBCs or reflector) motion
bernoulli equation
∆p = 4v²
bernoulli equation
pressure gradient across a value is related to velocity
pressure drop across a stenotic valve, in echo, is calculated using this
color doppler
don’t invert color map
velocity scale
specifies range of velocities displayed
adjust to maximize waveform without aliasing
sweep speed
changes number of cardiac cycles shown
use 100 mm/sec
sample volume size
adjusts width of sample volume
adjust to receive adequate signal while reducing noise
wall filter
eliminate low-velocity signals near baseline
adjust to remove unwanted noise without erasing flow information
spectral doppler gain
amplifies doppler signals before display
optimize for ability to measure accurately
baseline
position to optimize the doppler signal as large as possible
use with doppler scale to eliminate aliasing
peak velocity and pressure gradient
caliper to measure PV
PP gradient is calculated based on PV using bernoulli