clin med II exam 6
1/75
Earn XP
Description and Tags
becca_frizz
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
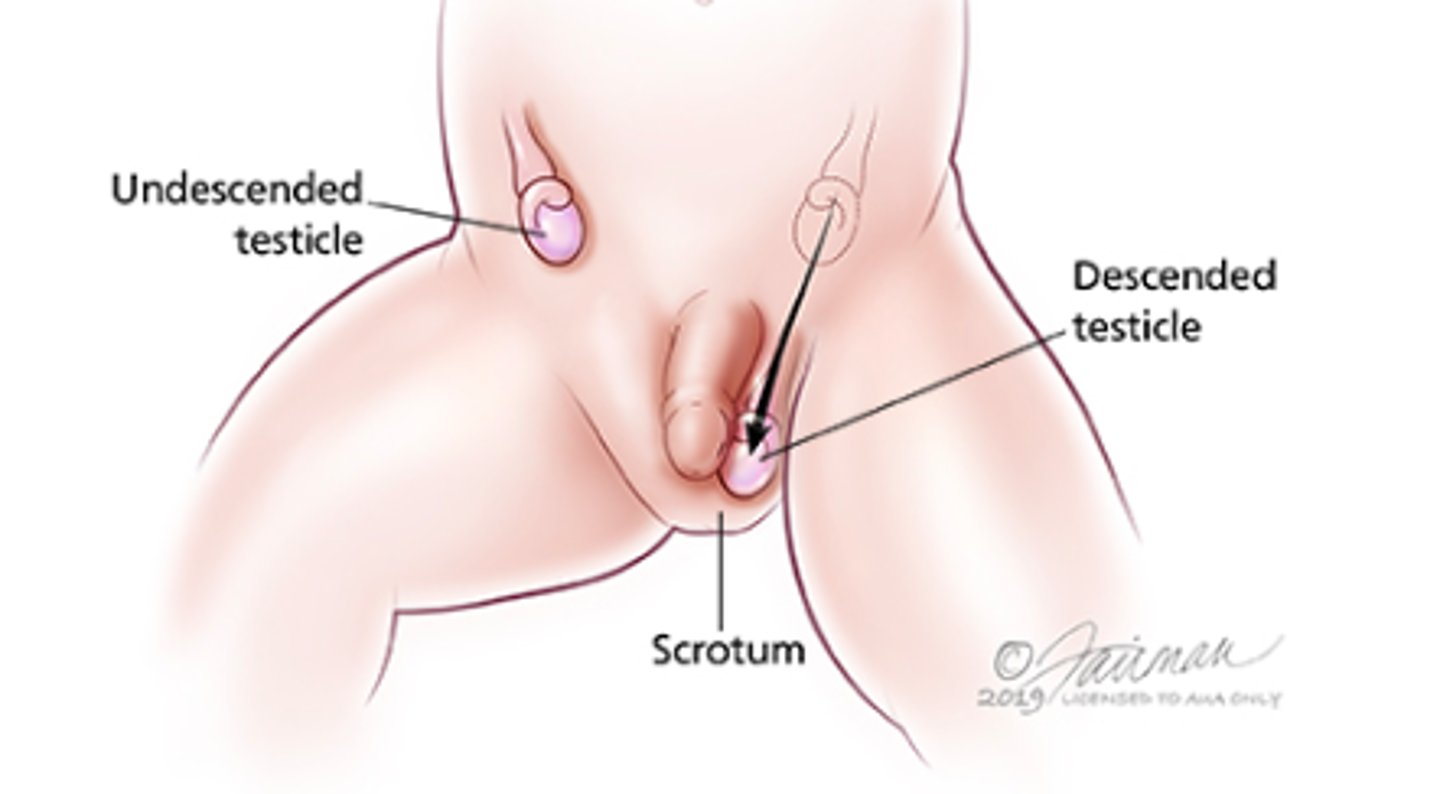
cryptorchidism patho
-undescended testis
-a testis that is not within the scrotum and does not descend spontaneously into the scrotum by 4 months of age
-may be absent or undescended
-etiology is multifaceted
Malpositioned along descent pathway
Genetic syndromes
Disorders of sexual development
-birth weight is the principal determining factor
-associated with infertility and a 10-20 fold increase in risk of testicular cancer
absent testis
may be due to agenesis or atrophy secondary to intrauterine vascular compromise
undescended testis
testes that have stopped short along their normal path of descent into the scrotum. They may remain in the abd cavity or they may be palpable in the inguinal canal or just outside the external ring
retractile testes
normal testes that have been pulled into a suprascrotal position by the cremasteric reflex
ascending testis
testis that are noted to be in a scrotal position in early childhood and then to ascend and become undescended
ectopic testis
testes that descend normally through the external ring but then are diverted to an aberrant position
cryptorchidism presentation
-typically asymptomatic and is noted incidentally
-complications of undescended testes:
Inguinal hernia
Testicular torsion
Testicular trauma
Subfertility
Malignant transformation
-testis may be impalpable or palpable in a location other than the scrotum, but usually along the path of normal descent
80% palpable
-palpable testes may be undescended, ectopic, or retractile
-nonpalpable testes may be intra-abdominal or absent
cryptorchidism diagnostics
-US or MRI to exclude genital ambiguity
-testing to rule out intersex condition
-17-hydroxylase progesterone
-testosterone (nml for unilateral, decreased for bilateral)
-LH (elevated)
-FSH (elevated)
cryptorchidism plan
-observation
-hormonal therapy
-surgical: orchiopexy
-refer and follow up
when should you treat cryptorchidism?
-In term boys, NET 4 month
-In premies, NET 6 months
-Should be corrected between age 9-15 mo to reduce risk of infertility
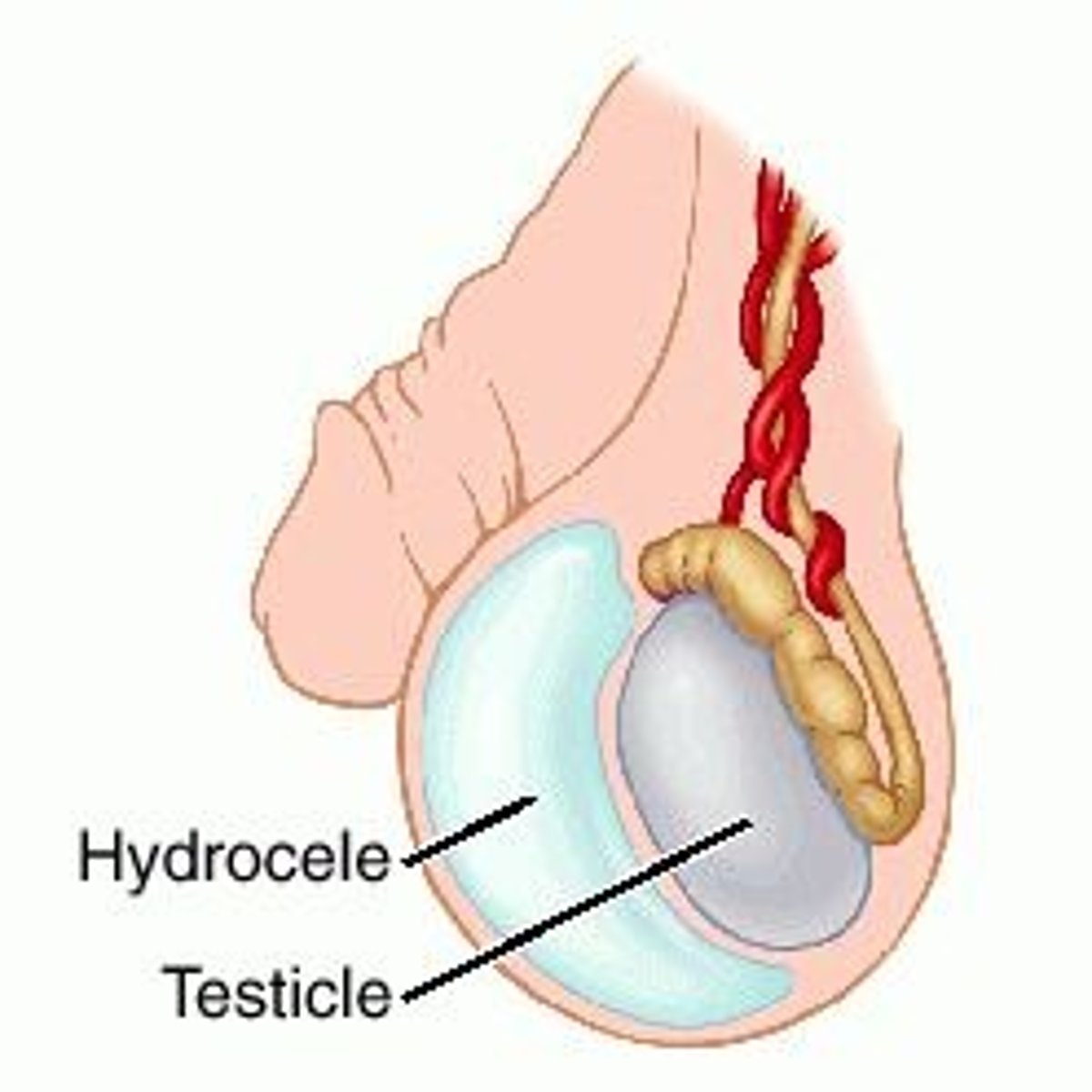
hydrocele patho
-fluid accumulation between the parietal and visceral layers of the tunica vaginalis
-abnormal fluid accumulation in the scrotum between the visceral and parietal layers of the tunica vaginalis
-more commonly on the right hemiscrotum
-In older boys and men, usually due to abnormal absorption or secretion secondary to another pathologic process
In infants, usually due to:
Incomplete closure of the processus vaginalis from the peritoneum
Residual peritoneal fluid that has yet to reabsorbed after processus closure
hydrocele presentation
-may be painful, with erythema and tenderness
-chronic hydroceles are typically painless
-sensation of heaviness
-transilluminates
-diffuse scrotal swelling
-not usually reducible
-may have generalized bluish discoloration
-preserved cremasteric reflex
hydrocele diagnostics
-scrotal US
-urinalysis and urine culture
For older adults:
Urethral swab
Nuclear scanning
hydrocele plan
For congenital noncommunicating:
-conservative management for the first 1-2 years of life b/c may close spontaneously
-beyond that time, surgical repair
For communicating hydrocele in infants:
-Elective hydrocelectomy with exploration of contralateral side
For adults:
-Surgery for secondary hydrocele
-Needle aspiration/decompression
-Sclerosis
-Supportive devices
varicocele patho
-dilated, tortuous veins of pampiniform plexus and the internal spermatic vein around the testicle
-most common cause of scrotal enlargement in young adults
->80% are on left
-There is an association with male infertility
Impaired venous drainage → increased venous pressure → vein dilation
varicocele presentation
-usually asymptomatic
-painless mass in the scrotum that feels like a bag of worms
-pain or a dragging, heavy feeling in the scrotum
-atrophy of the left testicle
-when the pt performs the Valsalva maneuver, the distention increases
-when supine, there is less distention of the mass than on standing
-usually unilateral and involving the left testicle, but can be bilateral

varicocele diagnostics
-clinical diagnosis
-baseline set of semen analyses if testicular atrophy is present
-in the eval of the infertile man with a varicocele: FSH level
Ancillary diagnostic tests:
Doppler stethoscope
Scrotal US
Spermatic venography
Scrotal thermography
Radionuclide scanning of the scrotum
varicocele plan
-First choice: no specific tx
-Second choice: open repair of the varicocele. Repair is either trans inguinal, retroperitoneal, of infrainguinal
-Third choice: varicocele repair through a laparoscope, sclerotherapy, or percutaneous embolization
-Tx should be considered when infertility is present
-Follow varicocelectomy pts with semen analyses every 3 months for the first yr or until pregnancy is achieved
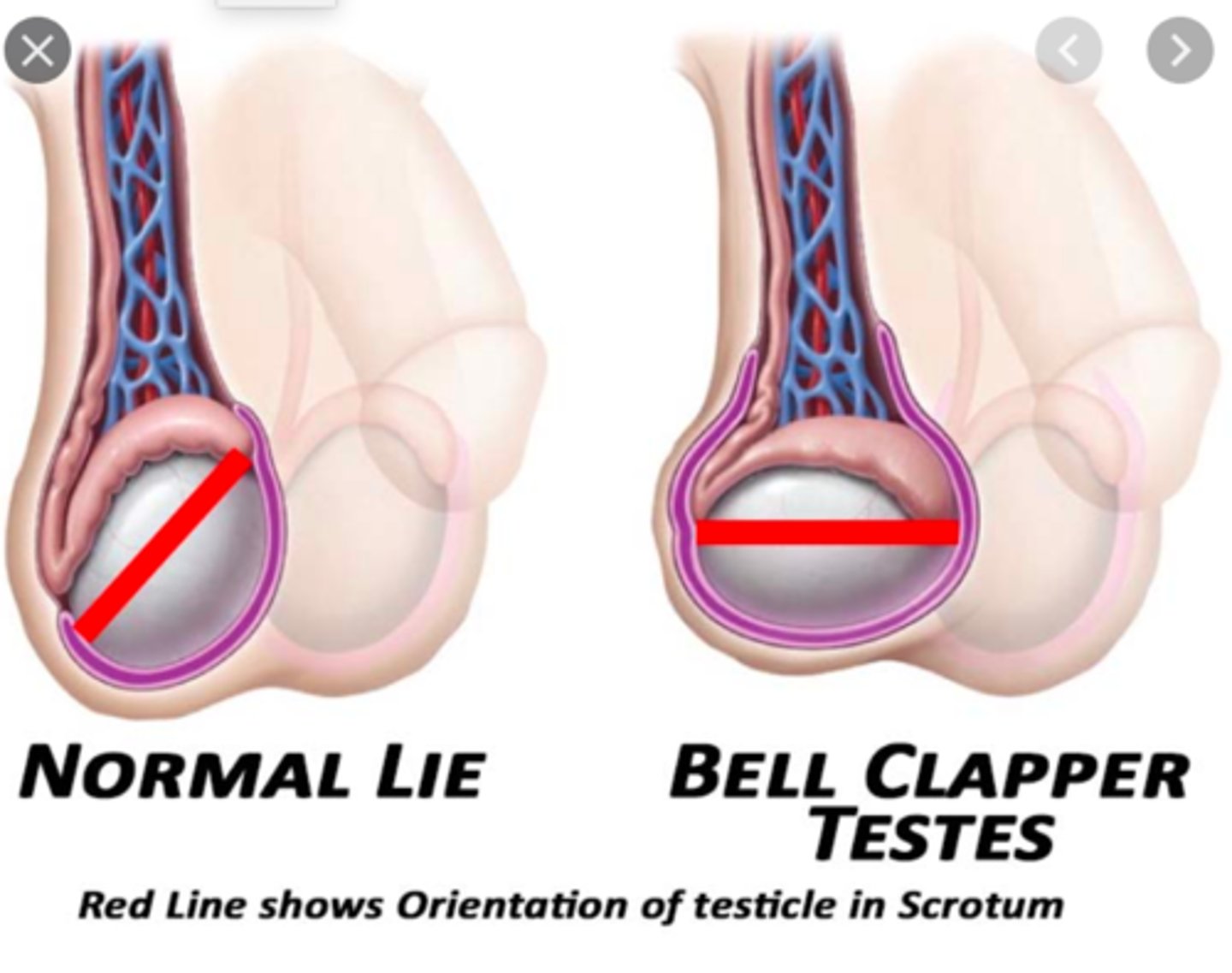
testicular torsion patho
-tunica vaginalis that is overly large and inserts high on the spermatic cord
-the cord is redundant and the testis can dangle and move within the scrotum
-2 types:
Extravaginal (infants)
Intravaginal (adolescents)
-torsion is 10 times as likely in an undescended testis
-results from inadequate fixation of the lower pole of the testis to the tunica vaginalis
-may occur after an inciting event or spontaneously
testicular torsion presentation
-early: profound testicular swelling
-12-24 hours: reactive hydrocele and overlying erythema of the scrotal wall
-often possible to detorse a testis during exam by gentle rotation away from the midline
-sudden onset of severe pain
usually starts in scrotum but can be localized to the central or lower abd or the inguinal area
-N/V
-most pts report no urinary symptoms
-affected hemiscrotum is swollen, tender, and firm
-scrotal skin becomes red and edematous
-testis is high-rising and in a horizontal lie (bell clapper deformity)
-testis may be drawn up into the neck of the scrotum, where the cord is palpably thickened
-cremasteric reflex absent on affected side
-20% of pts have mild fever
testicular torsion diagnostics
doppler US
testicular torsion plan
-surgical emergency
-immediate urology surgeon consult
-orchiectomy if non-viable testis
-orchiopexy as prophylaxis
-advice on avoiding contact sports that may jeopardize the remaining testicle
-attempt to detorse the testicle while you wait for the surgeon
Similar to opening a book, testicle is rotated out 1.5 rotations
testicular torsion risks
-testis sufferers irreversible damage after 12 hours of ischemia
-infertility may result
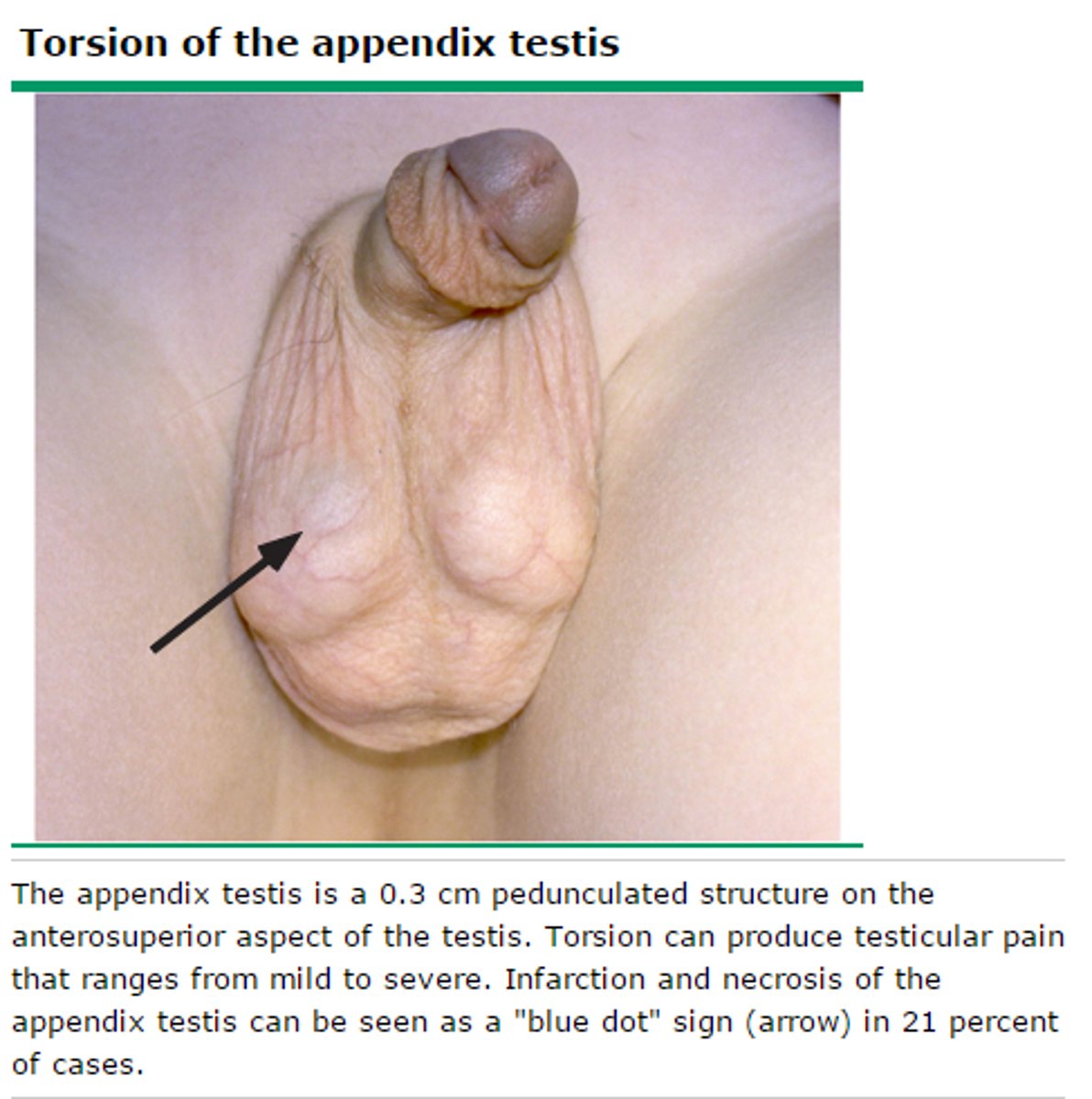
torsion of the appendix testis patho
-torsion of the appendage occurs when the tissue twists
-the appendix testis is a small appendage of normal tissue that is usually located on the upper portion of the testis
-one of the most frequent causes of acute scrotum
-the appendix epididymis is a small appendage on the top of the epididymis
-usually occurs pre-adolescent <11 YO
torsion of the appendix testis presentation
-cremasteric reflex is usually preserved
-blue dot sign
A hard, tender nodule may be palpable on the upper pole of the testicle, and a blue discoloration
torsion of the appendix testis diagnostics
US will usually show blood flow to the testis
phimosis patho
-tightness of penile foreskin that prevents it from being drawn back from over the glans
-Present as birth
-Caused by recurrent infection or irritation of the foreskin tissue
-Poor hygiene
-Diabetes
-Frequent diaper rash as infant
paraphimosis patho
-when the foreskin remains retracted proximal to the glans penis, causing constriction of glans penis
-Inexperienced healthcare provider or parent
phimosis presentation
-Usually not painful but may have pain on erection
-May produce urinary obstruction with ballooning of the foreskin and may lead to chronic inflammation and carcinoma
-Unretractable foreskin
-Superimposed balanitis
paraphimosis presentation
-Penile pain
-Drainage
-Ulceration
-swelling
phismosis/paraphimosis presentation
based on PE
phimosis plan
-Tx often no required for phimosis
-betamethasone cream 0.05% bid to tid applied to the top of the foreskin and the area touching the glans for 3 mo
-stretching the foreskin gently with 2 fingers or over an erect penis for 2-3 wk with care
-circumcision if conservative measures are ineffective
paraphimosis plan
-Should be regarded as an emergency
-Reduction of foreskin, usually while pt is sedated
hypospadias patho
-the urethral meatus opens on the ventral side of the penis proximal to the tip of the glans penis
-Results when fusion of the urethral folds is incomplete
epispadias patho
-urethra is displaced dorsally, and classification is based on its position in males
-Glandular: urethra opens on the dorsal aspect of the glans, which is broad and flattened
-Penile type: urethral meatus, often broad and gaping, is located between the pubic symphysis and the coronal sulcus
hypospadias presentation
-Difficulty directing the urinary stream and stream spraying
-Chordee causes ventral bending and bowing of the penile shaft, which can prevent sexual intercourse
epispadias presentation
-Urinary incontinence
-Dorsal curvature of the penis is bladder exstrophy
hypospadias diagnostics
-Buccal smear and karyotyping
-Ureteroscopy and cystoscopy
-Excretory urography to detect additional congenital anomalies of the kidneys and ureters
hypospadias plan
-Repair before the pt reaches school age (for psychological reasons)
-All types of repair involve straightening the penis by removal of the chordee
epispadias plan
Surgery required to correct the incontinence, remove the chordee to straighten the penis, and extend the urethra out onto the glans penis
urethral prolapse patho
-circumferential protrusion of the distal urethra through the external urethral meatus
-separation of the longitudinal and circular-oblique smooth muscle layers
urethral prolapse presentation
-doughnut shaped protrusion mucosa is observed obscuring urethral opening
Prepubertal:
-Usually asymptomatic
-MC: vaginal bleeding due to periurethral mass
-Pain of prolapse is large, thrombosed, or necrosis
-Acute urinary retention
-Hematuria and voiding disturbances are possible but not common
-Pinkish organ congested mass may be observed at the center of the urethral meatus
-May be painful and tender to palpation
-Mucosa is ulcerated in most cases and usually bleeds upon contact
Postmenopausal:
-Often symptomatic
-Vaginal bleeding and voiding symptoms
-Hematuria
-If large → strangulation → venous obstruction, thrombosis, necrosis
-UTI
-Erythematous inflamed mucosa protruding from the urethral meatus
-Congested mucosa may appear bright red or dark and cyanotic
-Depending on the evolution of the process, the prolapsed tissue may appear infected, ulcerated, or necrotic

urethral prolapse diagnostics
-diagnosed by verifying that a central opening is present within the prolapsed tissue and that this opening is the urethral meatus
-children: observation during voiding or catheterization of the central opening
-adults: urethral catheterization or cystourethroscopy
-if uncertain: surgical excision and pathologic exam
-MRI
urethral prolapse plan
-hygiene and local therapy with sitz baths
-topical hormones
-postmenopausal women with mild urethral prolapse: topical estrogen cream applied to the prolapsed urethra 2-3 x daily for 2 wk, in combo with sitz baths
-surgical excision for failed medical therapy, or strangulation
urethral stricture patho
-results from inflammatory, ischemic, or traumatic processes
-all lead to scar tissue formation → scar tissue contracts and reduces the caliber of the urethral lumen → resistance to the antegrade flow of urine
-occur after an injury to the urothelium or corpus spongiosum causes scar tissue to form
-a congenital stricture results from inadequate fusion of the anterior and posterior urethra, is short in length, and is not associated with an inflammatory process
urethral stricture presentation
-obstructive voiding symptoms
-urinary retention
-UTI
-decreased force of stream,
-incomplete emptying of the bladder
-urinary terminal dribbling
-urinary intermittency
urethral stricture diagnostics
-based on suggestive hx, PE findings, and radiographic or endoscopic techniques
-retrograde urethrogram or antegrade cystourethrogram
-US of male urethra
-flexible cystourethroscopy
urethral stricture plan
surgical
prostate cancer patho
-most common non dermatologic cancer
-most are slow growing and do not manifest during a pts lifetime
-95% are adenocarcinomas developing in the acini of prostatic ducts
-frequently multifocal within the prostate
-70% occur in peripheral zone
-genetic predisposition
-black men
prostate cancer presentation
-most often asymptomatic
-rarely systemic symptoms
-urinary outflow obstruction
-lower urinary tract symptoms
-bone pain
-reduced ejaculate volume
-hematospermia
-impotence
-may present with symptoms of spinal cord compression
-symptoms of hypercalcemia
-symptoms of renal failure
-prostatic induration (firm nodularity) on digital rectal exam or elevation or rapid PSA velocity
-pathologic fractures (related to metastasis)
-may present with unexplained DVT or recurrent thrombophlebitis (from mass effect)
-disease progression is by local extension via lymphatics or by hematologic spread to distant sites
prostate cancer diagnostics
-digital rectal exam
(Increased firmness
Loss of the median sulcus
Irregularly enlarged prostate
Nodules)
-PSA (elevated)
-BUN and Cr (elevated in urinary retention or obstruction)
-alkaline phosphatase (bony metastases)
-hypercalcemia (bony metastases)
-needle biopsy guided with TRUS
-MRI guided needle biopsy
-CT
-biopsy
prostate cancer plan
-tx depends on tumor grade
-radical prostatectomy
-radiation therapy
-active surveillance
-watchful waiting
-orchiectomy
-GnRH analogs
-chemotherapy
-ketoconazole
-medroxyprogesterone acetate
-consult
testicular cancer patho
-most common neoplasm in men aged 25-35
-slightly more common on the right than on the left
-primary germ cells tumors (GCTs) of the testis arising by the malignant transformation of primordial germ cells (more common)
-non-germ cell neoplasms include Leydig Cells, Sertoli cells, gonadoblastoma
-Seminomas: uniform type of cells and spread less aggressively
Approx 35%
-Nonseminomas: mixture of cell types, and are much more aggressive than seminomas
Approx 65%
Occurs earlier
testicular cancer presentation
-painless mass on a testes
-dull pain
-swelling
-heaviness in testis
-infertility
Signs of metastasis:
-Neck mass
-Neurologic findings consistent with spinal cord compression
-Unilateral or bilateral leg swelling secondary to inguinal node spread
-Abdominal mass
testicular cancer diagnostics
-orchiectomy for biopsy
-Alpha Fetoprotein (AFP): never elevated in seminoma
-beta-human chorionic gonadotropin (BhCG): greater elevation in non seminomas than seminomas
-lactate dehydrogenase (LDH): less-specific marker for GCTs, but levels can correlate with overall tumor burden
-13-hCG: elevated in nonseminomatous
-scrotal US
-CT of abd and pelvis with contrast
-chest xray
testicular cancer plan
-TNM staging system
-seminoma: radiotherapy
Stage 1 and many stage II, radiation is curative
Stage II and stage III: radiation with chemotherapy
-nonseminomatous: orchiectomy
-BEP is most common chemotherapy regimen for GCTs:
Bleomycin
Etoposide
Cisplatin
-refer
penile cancer patho
-majority arises on the glans, coronal sulcus, or on the prepuce as either a mass or ulceration
-squamous cell carcinomas accounts for 95%
-can also be melanoma, Kaposi sarcoma, Basal Cell Carcinoma, Lymphoma
-patterns of tumor infiltration:
-Pushing type: keep well-defined boundaries
-Reticular: smaller blocks infiltrate normal stroma
penile cancer presentation
-skin abnormality or palpable mass
-painless lump or ulcer
-rash
-bleeding
-balanitis
-early cases may exhibit a painless red, velvety lesions, but most often the lesion is an exophytic nodular or wart-like growth with secondary infection
-inguinal adenopathy
penile cancer diagnostics
biopsy
penile cancer plan
-if appears to be infected, 4-6 wk course of antifungal/antibiotic
-small, non infiltrating lesions:
-Fluorouracil cream
-External beam radiation
-Laser therapy
-larger lesions not involving deep structures that are limited to the distal penis:
Partial penile amputation at least 2 cm proximal to the lesion
-deeply infiltrating and proximal lesions:
Total penectomy, with formation of a perineal urethrostomy
-pts with high-risk features:
Prophylactic node dissection
Radiation
-pts with distant metastases:
Cisplatin and methotrexate
differential for penile cancer
soft chancre due to Haemophilus ducreyi infection
bladder cancer patho
-in industrialized countries >90% of cases start in the transitional epithelial cells
Called transitional cell carcinoma
-in developing countries, 75% if cases are SCC caused by Schistosoma haematobium infection
-occupational link
-can be latent period of up to 50 yrs
3 main histologic types:
-Transitional cell carcinoma (TCC)- most common
-Squamous carcinoma
-Adenocarcinoma
Oncogenes associated with bladder cancer:
-Ras gene family
-P21 ras oncogene
Tumor suppressor genes:
-P53 on chromosome 17p
-Retinoblastoma gene chromosome 13q
-Genes on chromosome 9: 9p21 and 9q32-33
bladder cancer presentation
-may initially be asymptomatic
-anorexia, weight loss in advanced disease
-irritative voiding symptoms
-pain is a late feature, indicating advanced disease
-85-90% of pts present with painless gross hematuria (classic presentation)
-abd mass
Bladder may be palpable if filled with blood clot or if a large tumor mass is present
-anemia
-cachexia in advanced disease
bladder cancer diagnostics
-UA with microscopy: hematuria
-urine culture (UTI may be associated with bladder cancer)
-voided urine cytology (positive)
-CT of abd and pelvis
-MRI
-IVP
-renal US
-cystoscopy is nearly 100% accurate
Definitive diagnostic procedure
Biopsy confirms the dx
-full blood count (anemia)
-serum BUN and Cr (renal failure)
-serum potassium
-liver function tests
-IV urogram
-retrograde pyelogram
-bone scan is metastatic disease suspected
-filling defect within bladder noted on x-ray imaging
bladder cancer treatment
TCC:
Superficial lesions are resected endoscopically
If multiple or recur frequently: intravesical mitomycin C, thiotepa, doxorubicin hydrochloride, epirubicin, Bacille Calmette- Guerin (BCG) may be used
BCG is TOC for recurrent superficial transitional cell carcinoma
Carcinoma in situ treated endoscopically, and requires tx with intravesical BCG
-multiple invasive disease is treated by radical cystectomy or TURBT
-metastatic disease may be treated with chemotherapy: M-VAC (methotrexate, vinblastine, doxorubicin, cisplatin), CMV (cisplatin, methotrexate, vinblastine), CISCA (cisplatin, cyclophosphamide, doxorubicin)
-SCC: radical cystectomy and sometimes radiotherapy
-adenocarcinoma: radical cystectomy
-surveillance for pts with superficial transitional cell cancer include cystoscopy and bladder wash cytologies every 3 months for 2 yrs, then every 6 months for 2 yrs, and then at least yearly
-referral
trichomoniasis presentation in women
-Symptoms range from none in women who are asymptomatic carriers to a severe pelvic inflammatory disease
-Yellow vaginal discharge
-Malodorous frothy, yellow-green
-Abnormal vaginal odor
-Dysparenuina
-Vulvar itching
-Dysuria
-Vulvar and vaginal erythema are common
-Pruritis
trichomoniasis diagnostics
-vaginal pH measured on Nitrazine paper is elevated: pH is >5.0 -6.0
-saline wet mount: ovoid shaped parasites
-C&S
-OSOM trichomonas rapid test
trichomoniasis plan
-Metronidazole is TOC 2 g PO x 1 dose
-tinidazole 2 g PO single dose
-metronidazole 500 mg PO bid f7
HPV screening
Initiating screening at age 21, regardless of the age of initiation of sexual activity
chlamydia screening
-Women >= 25 yrs if risk factors are present
-Sexually active women <25
-Repeat testing of all women 3-4 months after tx, esp adolescents or when they next present for care within 12 months
-Pregnant: first prenatal visit or increased risk
-Men: clinical settings with a high prevalence
gonorrhea screening
-Screening all sexually active women
Pregnancy:
-Should be performed at first prenatal visit for women at risk or those living in an area in which the prevalence is high
-Repeat test during the 3rd trimester for those at continued risk
At risk MSM:
-Annual screening for urethral and rectal gonorrhea and chlamydia, and for pharyngeal gonorrhea
urge incontinence
-the strong, sudden need to urinate due to bladder spasms or contractions
-most common in older women
stress incontinence
-an involuntary loss of urine that occurs during physical activity, such as coughing, sneezing, laughing, or exercise
-women <50
mixed incontinence
the combination of both urge and stress incontinence
urge incontinence treatments
-behavioral: diet, urge suppression, BioFB/PT
-medication
-tertiary: sacral neuromodulation, Botox, PTNS
stress incontinence treatments
-Kegels
-surgical treatment: sling vs UBA