Chapter 22: Mental Health Issues of Children and Adolescents
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
Chapter 22: Mental Health Issues of Children and Adolescents
Childhood and adolescent mental health & neurodevelopmental disorders are often difficult to identify and diagnose, leading to delayed treatment and interventions.
Children and adolescents may meet criteria for multiple mental health disorders and may have comorbid conditions.
Behaviors become problematic when they interfere with:
Home life
School performance
Peer interactions
Disorders That Can Appear During Childhood and Adolescence
Depressive Disorders – Major depressive disorder, persistent depressive disorder
Anxiety Disorders – Separation anxiety disorder, panic disorder
Trauma- & Stressor-Related Disorders – PTSD
Substance Use Disorders – Alcohol, tobacco, cannabis use disorder
Feeding & Eating Disorders – Anorexia nervosa, bulimia nervosa, binge eating disorder
Disruptive, Impulse Control, & Conduct Disorders – Oppositional defiant disorder, disruptive mood dysregulation disorder, conduct disorder
Neurodevelopmental Disorders – ADHD, autism spectrum disorder, intellectual developmental disorder, specific learning disorder
Bipolar & Related Disorders
Schizophrenia Spectrum & Other Psychotic Disorders
Nonsuicidal Self-Injury & Suicidal Behavior Disorder – Suicide is a leading cause of death ages 10–24
Impulse Control Disorders – Intermittent explosive disorder
Factors Impeding Diagnosis (3)
Limited language/cognitive/emotional skills to describe symptoms
Wide variation of “normal” behaviors by developmental stage
Difficulty distinguishing emotional problems from typical behavior delays diagnosis
Characteristics of Good Mental Health in Youth (6)
Accurately interpret reality; correct perception of environment
Positive self-concept
Cope with stress/anxiety in age-appropriate ways
Master developmental tasks
Express self spontaneously/creatively
Develop and maintain satisfying relationships
Etiology and General Risk Factors
Genetic Links / Chromosomal Abnormalities
Associated with: schizophrenia, bipolar disorder, autism spectrum disorder, ADHD, intellectual developmental disorder
Biochemical Factors
Neurotransmitter alterations (norepinephrine, serotonin, dopamine) contribute to some mental health disorders
Social & Environmental Factors
Risk factors: severe marital discord, low socioeconomic status, large families, overcrowding, parental criminality, substance use disorders, maternal psychiatric disorders, parental depression, foster care placement
Cultural & Ethnic Factors
Difficulty with assimilation, lack of cultural role models, lack of support from dominant culture
Resiliency
Ability to adapt to change, form nurturing relationships, use effective coping/problem-solving skills can protect against developing a mental disorder
Trauma Exposure
Witnessing or experiencing traumatic events (e.g., physical or sexual abuse) during formative years
Depressive Disorders in Children and Adolescents
Risk Factors
Family history of depression
Physical or sexual abuse, neglect
Homelessness
Parental disputes, family/peer conflict, rejection
Bullying (as aggressor or victim; includes cyberbullying)
High-risk behaviors
Learning disabilities
Chronic illness
Expected Findings
Sadness
Temper tantrums (verbal/behavioral outbursts)
Loss of appetite
Vague health complaints
Solitary play or work
Appetite changes → weight changes
Sleep pattern changes
Crying
Fatigue/low energy
Irritability
Aggression
High-risk behavior
Poor school performance / school dropout
Hopelessness about the future
Suicidal ideation or attempts
Anxiety Disorders & Trauma- and Stressor-Related Disorders
Expected Findings
Interferes with normal growth and development
Severe enough to impair normal functioning at home, school, and other areas
Separation Anxiety Disorder
Excessive, developmentally inappropriate anxiety when separated from home/parents
Can lead to school phobia or fear of being alone
Depression is common comorbidity
May occur after a specific stressor (death, illness, move, assault)
Can progress to panic disorder or other phobias
Interventions
Provide emotional support that accepts regression/defense mechanisms
Offer protection during panic-level anxiety by meeting needs
Use strategies to boost self-esteem and achievement
Posttraumatic Stress Disorder (PTSD)
Triggered by experiencing/witnessing/learning of a traumatic event
Signs in children/adolescents: anxiety, depression, phobia, conversion reactions
External signs: irritability, aggression, poor academic performance, somatic complaints, belief in shortened life expectancy, sleep disturbances
Small children may reduce play or engage in trauma-related play
Interventions
Assist in processing traumatic events or losses to reach acceptance
Encourage group therapy participation
Disruptive, Impulse Control, and Conduct Disorders
Expected Findings
Behavioral problems occur in school, home, and social settings
Common comorbidities: ADHD, depression, anxiety, substance use disorders
Symptoms often worsen in:
Situations requiring sustained attention (e.g., classroom)
Unstructured group situations (e.g., playground)
Interventions
Use calm, firm, respectful approach
Model acceptable behavior
Gain attention before giving instructions; keep directions short/clear
Set and consistently enforce behavior limits
Plan physical activities for energy release and success
Help parents develop reward systems (e.g., wall charts, tokens) with child involvement
Focus on strengths, not just problems
Support parental hopefulness
Maintain safe environment for all
Give positive feedback for meeting expectations
Identify causes of power struggles and address them
Teach effective coping skills
Promote group, individual, and family therapy participation
Administer and monitor medications (antipsychotics, mood stabilizers, anticonvulsants, antidepressants)
Oppositional Defiant Disorder (ODD)
Recurrent antisocial behaviors:
Negativity, disobedience, hostility
Defiant behavior (esp. toward authority)
Stubbornness, argumentativeness, limit testing
Unwillingness to compromise
Refusal to accept responsibility for misbehavior
Misbehavior directed at person best known; usually at home
Clients don’t see behavior as defiant, but as a response to perceived unreasonable demands
Associated with: low self-esteem, mood lability, low frustration tolerance
May progress to conduct disorder
Disruptive Mood Dysregulation Disorder (DMDD)
Severe, recurrent temper outbursts (verbal/physical) inappropriate for developmental level
Outbursts occur ≥3 times/week in at least two settings (home, school, with peers)
Mood between outbursts: irritable/angry
Onset between ages 6–18
Not due to another mental health disorder (e.g., bipolar disorder)
Intermittent Explosive Disorder (IED)
Recurrent, episodic violent/aggressive behavior (verbal or physical) with potential harm to people, property, or animals
Onset: as early as age 6; most common ages 13–21
More common in males
Triggered by minor events; followed by shame/regret
Can impair relationships/employment; linked to chronic diseases (e.g., hypertension, diabetes)
Conduct Disorder (Childhood or Adolescent Onset)
Persistent pattern violating rights of others or societal rules
Categories:
Aggression toward people/animals
Property destruction
Deceit/theft
Serious rule violations
Onset:
Childhood-onset: before age 10; males more prevalent
Adolescent-onset: after age 10; male-to-female ratio equal
Contributing Factors
Parental rejection/neglect
Difficult temperament
Harsh/inconsistent discipline
Abuse (physical/sexual)
Lack of supervision
Early institutionalization
Frequent caregiver changes
Large family size
Association with delinquent peers
Parent with psychological illness
Chaotic home life
Lack of male role model
Manifestations
Lack of remorse/empathy
Bullying/threats/intimidation
Justifies aggression
Low self-esteem, irritability, reckless behavior, temper outbursts
Possible suicidal ideation
Concurrent learning/cognitive impairments
Physical cruelty to people/animals
Weapon use causing serious harm
Property destruction
Theft, shoplifting, truancy
Running away from home
A nurse is performing an admission assessment on an adolescent client who has depression. Which of the following findings are expected for this disorder?
Select all that apply.
a
Fear of being alone
b
Substance use
c
Weight gain
d
Irritability
e
Aggressiveness
b Substance use
d Irritability
e Aggressiveness
Solitary play or work, rather than the fear of being alone, is an expected finding associated with depression.
Loss of appetite and weight loss, not weight gain, are expected findings associated with depression.
A nurse is teaching a group of guardians about manifestations of conduct disorder. Which of the following findings should the nurse include?
Select all that apply.
a
Bullying of others
b
Threats of suicide
c
Law-breaking activities
d
Narcissistic behavior
e
Flat affect
a Bullying of others
b Threats of suicide
c Law-breaking activities
Low self-esteem, rather than narcissism, is an expected finding of conduct disorder.
Irritability and temper outbursts, rather than a flat affect, are expected findings of conduct disorder.
Neurodevelopmental Disorders
Etiology & General Risk Factors
Prevalence increasing in the U.S. (current rate: 1 in 6 children)
Symptoms may change with maturation but can persist into adulthood
Often multifactorial: hereditary + environmental influences affect neurological development
Comorbidities
May occur alongside various medical conditions
Diagnosis challenging due to overlapping symptoms with other disorders
Attention Deficit Hyperactivity Disorder (ADHD)
Inability to control behaviors requiring sustained attention
Core Behaviors:
Inattention – Difficulty paying attention, listening, focusing
Hyperactivity – Fidgeting, inability to sit still, inappropriate running/climbing, difficulty playing quietly, excessive talking
Impulsivity – Difficulty waiting turns, frequent interruptions, acting without considering consequences
Risks & Requirements
Inattentive/impulsive behaviors increase risk of injury
Diagnosis: symptoms before age 12, present in more than one setting, and causing impairment
Associated behaviors differ from typical attention patterns in adults/peers
Types
Predominantly Inattentive – Main symptoms are inattention
Predominantly Hyperactive-Impulsive – Main symptoms are hyperactivity/impulsivity
Combined Type – Both inattentive and hyperactive-impulsive symptoms present
Interventions
Use calm, firm, respectful approach
Model acceptable behavior
Gain attention before giving instructions; keep directions short/clear
Set and consistently enforce behavior limits
Plan physical activities for energy release and success
Help parents develop reward systems (e.g., wall charts, tokens) with child involvement
Focus on strengths, not just problems
Support parental hopefulness
Maintain safe environment for all
Give positive feedback for meeting expectations
Identify causes of power struggles and address them
Teach effective coping skills
Promote group, individual, and family therapy participation
Administer and monitor medications (antipsychotics, mood stabilizers, anticonvulsants, antidepressants)
Autism Spectrum Disorder (ASD)
Genetic origin; affects communication and social interaction
Common signs: poor eye contact, repetitive actions, strict routines
Onset: early childhood; more common in boys
Possible physical issues: sensory integration dysfunction, sleep disorders, GI problems, seizures, allergies
Functioning ranges from severe impairment to near-normal abilities
Interventions
Refer for early interventions (physical, occupational, speech therapy)
Provide structured environment
Collaborate with parents for consistent, individualized care
Use short, concise, developmentally appropriate communication
Identify/reward desired behaviors
Model social skills and role-play conflict resolution
Encourage verbal communication
Replace self-stimulatory behaviors with alternative play
Identify emotional/situational triggers
Give advance notice of routine changes
Intellectual Developmental Disorder
Onset: infancy/childhood
Deficits in intellectual functions: reasoning, abstract thinking, learning
Impaired independence and social responsibility (daily living, social participation, school)
Severity: mild to severe
Specific Learning Disorder
Persistent difficulty in reading, writing, or math
Performance below expected level for age/intelligence/education
May require individualized education program (IEP)
Communication Disorders
Problems with language and speech skills
Speech issues: stuttering
Difficulty with conversational skills, worsened by age-related social pressures
Match the following manifestations with the appropriate mental health disorder for children or adolescents.
Conduct disorder
Attention deficit hyperactivity disorder
Disruptive mood dysregulation disorder
Depressive disorder
Oppositional defiant disorder
Recurrent temper outbursts that are severe and do not correlate with situation.
Feeling of sadness.
Limit testing.
Demonstrates lack of remorse.
Inability of a person to control behaviors requiring sustained attention.
Recurrent temper outbursts that are severe and do not correlate with situation.
Disruptive mood dysregulation disorder
Feeling of sadness.
Depressive disorder
Limit testing.
Oppositional defiant disorder
Demonstrates lack of remorse.
Conduct disorder
Inability of a person to control behaviors requiring sustained attention.
Attention deficit hyperactivity disorder
A nurse is assessing a 4-year-old child for indications of autism spectrum disorder. For which of the following manifestations should the nurse assess?
a
Impulsive behavior
b
Repetitive counting
c
Destructiveness
d
Somatic problems
b Repetitive counting
Impulsive behavior is an indication of ADHD rather than autism spectrum disorder.
Destructiveness is an indication of conduct disorder rather than autism spectrum disorder.
Somatic problems are an indication of posttraumatic stress disorder rather than autism spectrum disorder.
A nurse is assisting the guardians of a school-age child who has oppositional defiant disorder in identifying strategies to promote positive behavior. Which of the following strategies should the nurse recommend?
Select all that apply.
a
Allow the child to choose which behaviors are unacceptable.
b
Use role-playing to act out unacceptable behavior.
c
Develop a reward system for acceptable behavior.
d
Encourage the child to participate in school sports.
e
Be consistent when addressing unacceptable behavior.
c Develop a reward system for acceptable behavior.
d Encourage the child to participate in school sports.
e Be consistent when addressing unacceptable behavior.
CNS Stimulants Indications / Contraindications
Purpose
Expected Pharmacological Action: Increase norepinephrine and dopamine levels in the CNS
Therapeutic Uses
ADHD in children and adults
History of substance use disorder, cardiovascular disorders, severe anxiety, psychosis
Teratogenic — avoid during pregnancy
CNS Stimulants Admin / Meds
Administration Guidelines
Swallow sustained-release tablets whole; do not chew/crush
Stress regular, consistent dosing schedule (regular or extended-release available)
Give oral tablets 30–45 min before meals, last dose before 4 p.m.
Administer oral suspension regardless of meals; shake for 10 seconds before measuring
For transdermal use: apply patch to one hip daily in the morning, max 9 hours; alternate hips; flush patch after removal
Full therapeutic response may take up to 6 weeks
Avoid all OTC meds unless approved by provider
Avoid alcohol during therapy
Parent/Client Education
ADHD is not cured by medication; best outcomes occur with combined family and cognitive therapy
Medications have special handling rules; handwritten prescriptions often required for refills
Store medications safely to prevent misuse
Warn of high potential for substance use disorder, especially in adolescents
Nursing Evaluation of Effectiveness
Look for improved ADHD manifestations:
Increased ability to focus and complete tasks
Improved peer interactions
Decreased hyperactivity and impulsivity
Prototype Medication
Methylphenidate
Other Medications
Amphetamine mixture
Dextroamphetamine
Dexmethylphenidate
Lisdexamfetamine dimesylate
CNS Stimulants Complications / Interactions
CNS Stimulation (insomnia, restlessness)
Nursing Actions
Reduce dosage per provider’s order
Give last dose before 4 p.m.
Client Education
Avoid caffeine-containing items (coffee, tea, cola, chocolate)
Weight Loss / Appetite Suppression / Growth Suppression
Nursing Actions
Monitor height/weight vs. baseline
Consider medication “holidays” per provider
Give medication during or after meals
Client Education
Eat regular meals; avoid unhealthy food choices
Cardiovascular Effects (dysrhythmias, chest pain, hypertension)
May ↑ risk of sudden death in clients with heart abnormalities
Nursing Actions
Monitor vitals and ECG
Teach to report symptoms immediately
Psychotic Manifestations (hallucinations, paranoia)
Client Education
Report immediately; discontinue medication
Withdrawal Reaction (headache, nausea, vomiting, muscle weakness, depression)
Client Education
Avoid abrupt cessation
Hypersensitivity Skin Reaction to Transdermal Methylphenidate (hives, papules)
Client Education
Remove patch and notify provider
Toxicity (dizziness, palpitations, hypertension, hallucinations, seizures)
Nursing Actions
Treat hallucinations: chlorpromazine
Treat seizures: diazepam
Administer fluids
MAOIs
Concurrent use → hypertensive crisis
Nursing Action: Discontinue MAOIs; wait ≥14 days before starting amphetamines
Caffeine
Concurrent use → ↑ CNS stimulant effects
Nursing Action: Avoid caffeine-containing foods/beverages
Phenytoin, Warfarin, Phenobarbital
Methylphenidate inhibits metabolism → ↑ drug levels
Nursing Action: Monitor for CNS depression/bleeding; use with caution
OTC Cold & Decongestant Medications
Concurrent use → ↑ CNS stimulation
Client Education: Avoid these OTC products
A nurse is caring for a school age child who has conduct disorder and a new prescription for methylphenidate transdermal patches. Which of the following information should the nurse provide about the medication?
a
Apply the patch once daily at bedtime.
b
Place the patch carefully in a trash can after removal.
c
Apply the transdermal patch to the anterior waist area.
d
Remove the patch each day after 9 hr.
d Remove the patch each day after 9 hr.
The transdermal patch should be applied to a clean, dry area on the hip, and the waist area should be avoided.
For safety when discarding the transdermal preparation, the client should fold the patch and flush it down the toilet to prevent others from using it.
The transdermal patch is applied once daily in the morning.
Selective Norepinephrine Reuptake Inhibitor (SNRI) Indications / Contraindications
Purpose
Action: Blocks norepinephrine reuptake at CNS synapses (non-stimulant)
Use: ADHD in children and adults
Generally well tolerated with minimal side effects
Contraindications / Precautions — Atomoxetine
Use cautiously in cardiovascular disorders
Contraindicated in suicidal ideation
Contraindicated in angle-closure glaucoma or pheochromocytoma (adrenal tumor → epinephrine/norepinephrine overproduction)
Selective Norepinephrine Reuptake Inhibitor (SNRI) Complications / Interactions
Appetite/Growth Suppression, Weight Loss
Nursing Actions: Monitor height/weight; give with or after meals
Education: Encourage regular meals and healthy food choices
GI Effects (nausea, vomiting, abdominal pain)
Education: Take with food if GI upset occurs
Suicidal Ideation (children/adolescents)
Nursing Actions: Monitor for depression signs
Education: Report mood changes, excessive sleeping, agitation, irritability
Hepatotoxicity
Education: Report flu-like symptoms, jaundice, abdominal pain
CNS Effects (headache, insomnia, irritability)
Nursing Actions: Lower dose if prescribed; last dose before 4 p.m.
Education: Monitor for symptoms; avoid caffeine-containing products
MAOIs
Risk: hypertensive crisis
Education: Stop MAOIs ≥14 days before starting atomoxetine
Paroxetine (SSRI), Fluoxetine (SSRI), Quinidine Gluconate (Antiarythmatic)
Inhibit metabolism → ↑ atomoxetine levels
Nursing Action: May need to reduce atomoxetine dose
Education: Monitor/report increased adverse effects
Selective Norepinephrine Reuptake Inhibitor (SNRI) Admin / meds
Nursing Administration
Monitor for changes related to dose/timing
Administer once daily (morning) or split into two doses (morning + afternoon), with or without food
Client Education
Initial effects in days; full therapeutic effect in up to 6 weeks
Avoid alcohol
Avoid OTC meds unless approved
Prototype Medication
Atomoxetine
Other Medication
Bupropion
Tricyclic Antidepressants (TCAs) Indications / Contraindications
Purpose
Expected Pharmacological Action: Block reuptake of norepinephrine and serotonin in the synaptic space, increasing their effects
Therapeutic Uses in Children
Depression
Autism spectrum disorder
ADHD
Panic disorder, separation anxiety disorder
Social phobia
Obsessive-compulsive disorder (OCD)
Teratogenic
Contraindicated: recent MI, heart failure, prolonged QT
Use cautiously in seizure disorders, CAD, diabetes, liver/kidney/respiratory disease, urinary retention, angle-closure glaucoma, BPH, hyperthyroidism
↑ suicide risk; lethal in overdose
Tricyclic Antidepressants (TCAs) Complications / Interactions
Orthostatic Hypotension
Anticholinergic Effects (dry mouth, blurred vision, photophobia, urinary retention, constipation, tachycardia)
Client Education:
Chew sugarless gum
Sip water regularly
Wear sunglasses outdoors
Eat high-fiber foods
Increase fluid intake to 2–3 L/day
Void before taking medication
Report intolerable effects
Weight Gain (↑ appetite)
Nursing Action: Monitor weight
Sedation
Client Education:
Effects usually decrease over time
Avoid hazardous activities if excessive sedation occurs
Take at bedtime to reduce daytime drowsiness and improve sleep
Toxicity
Manifestations: Cholinergic blockade + cardiac toxicity (dysrhythmias, confusion, agitation → seizures, coma, death)
Nursing Actions:
Dispense only 1-week supply for acutely ill clients
Obtain baseline ECG
Monitor vitals and signs of toxicity; notify provider
Decreased Seizure Threshold
Excessive Sweating
Client Education: Monitor and perform frequent linen changes
MAOIs → severe hypertension; wait ≥14 days after stopping MAOIs before starting TCAs
Antihistamines / Other Anticholinergic Agents → additive effects; avoid concurrent use
Epinephrine / Dopamine → hypertensive crisis risk; avoid concurrent use
Alcohol, Benzodiazepines, Opioids, Antihistamines → additive CNS depression; avoid while on TCAs
Tricyclic Antidepressants (TCAs) Admin / Meds
Instruct parents to administer daily as prescribed to maintain therapeutic plasma levels
Emphasize adherence; initial effects in 1–3 weeks, full effects in ~6 weeks
Stress importance of continuing therapy after improvement to prevent relapse
Give at bedtime to reduce daytime drowsiness
Due to suicide risk: give only 1-week supply to acutely ill clients, then 1-month supply thereafter
Prototype Medication
Desipramine
Other Medications
Imipramine
Clomipramine
Nursing Evaluation of Effectiveness (TCAs)
For Depression
Reports improved mood
Better sleep and eating patterns
Increased peer interaction
For Autism Spectrum Disorder
Reduced anger
Less compulsive behavior
For ADHD
Reduced hyperactivity
Improved attention span
For OCD, Panic, Anxiety Disorders
Lower anxiety levels
Better recognition of symptoms/triggers
Improved management of episodes
Enhanced self-care ability
Increased peer interaction
Able to resume normal roles
Nursing Evaluation of Effectiveness (SSRIs)
For intermittent explosive disorder:
↓ Hyperactivity
Improved mood
For conduct disorder:
↓ Aggressiveness
Nursing Evaluation of Effectiveness (Atypical Antipsychotics)
Autism Spectrum Disorder
↓ Hyperactivity
Improved mood
Conduct Disorder
↓ Aggressiveness
OCD
↓ Anxiety
Better control of compulsive actions
Improved self-care
↑ Social interaction
Able to assume usual role
ADHD
↓ Hyperactivity & impulsivity
Alpha-Adrenergic Agonists Indications / Contraindications
Pharmacological Action: Activates presynaptic alpha₂-adrenergic receptors in the brain (exact mechanism not fully understood)
Therapeutic Uses: ADHD, tic disorders, conduct/oppositional defiant disorders
Not established for use in children < 6 years old
Use cautiously in clients with cardiac disease
Alpha-Adrenergic Agonists Complications / Interactions
CNS Effects (Sedation, Drowsiness, Fatigue)
Nursing: Monitor and report
Education: Avoid hazardous activities
Cardiovascular Effects (Hypotension, Bradycardia)
Nursing: Monitor BP and pulse, especially early in treatment
Education: Do not abruptly stop — may cause rebound hypertension
Weight Gain
Nursing: Monitor weight, encourage exercise and healthy diet
GI Effects (Nausea, Vomiting, Constipation, Dry Mouth)
Nursing: Monitor and report
Prevention Strategies:
Chew sugarless gum
Sip water
Eat high-fiber foods
Engage in regular exercise
Increase fluid intake to 2–3 L/day
CNS Depressants (Including Alcohol)
↑ CNS effects
Nursing: Avoid concurrent use
Antihypertensives
↑ Hypotension risk
Nursing: Avoid concurrent use
High-Fat Meals
↑ Guanfacine absorption
Nursing: Avoid taking with high-fat meals
Alpha-Adrenergic Agonists Administration / Meds
Assess alcohol and CNS depressant use (especially adolescents)
Monitor BP and pulse at baseline, initial treatment, and dosage changes
Avoid abrupt discontinuation → risk of rebound hypertension; taper per prescribed schedule
Do not chew, crush, or split extended-release tablets
Guanfacine, Clonidine
Atypical Antipsychotics Complications / Interactions
1. Diabetes Mellitus
Risk: New onset or loss of glucose control in clients with diabetes
Nursing actions:
Obtain baseline fasting blood glucose, monitor periodically
Instruct client to report signs (increased thirst, urination, appetite)
2. Weight Gain
Client education:
Follow healthy, low-calorie diet
Engage in regular exercise
Monitor weight
3. Hypercholesterolemia
Risk: Higher chance of hypertension & cardiovascular disease
Nursing actions: Monitor cholesterol, triglycerides, and blood glucose if weight gain > 14 kg (30 lb)
4. Orthostatic Hypotension
Nursing actions: Monitor BP with first dose; instruct slow position changes
5. Anticholinergic Effects (urinary retention/hesitancy, dry mouth)
Nursing actions: Monitor and report occurrence
Client education: Relieve dry mouth (sip fluids throughout the day)
6. Agitation, Dizziness, Sedation, Sleep Disruption
Nursing actions: Monitor; change medication if prescribed
7. Mild Extrapyramidal Symptoms (EPS) — tremor
Nursing actions: Monitor and teach clients to recognize EPS; usually dose-related
1. CNS Depressants (alcohol, opioids, antihistamines)
Effect: Additive CNS depression
Client education:
Avoid alcohol and other CNS depressants
Avoid hazardous activities (e.g., driving)
2. Levodopa
Effect: Activates dopamine receptors, counteracting antipsychotic effects
Nursing actions: Avoid concurrent use with levodopa or other dopamine receptor agonists
3. TCAs, Amiodarone, Clarithromycin
Effect: Prolong QT interval → ↑ risk of cardiac dysrhythmias
Nursing actions: Avoid concurrent use
4. Barbiturates & Phenytoin
Effect: Promote hepatic drug metabolism → ↓ drug levels of quetiapine
Nursing actions: Monitor for effectiveness
5. Fluconazole & other CYP3A4 inhibitors
Effect: Inhibit metabolism → ↑ drug levels of aripiprazole and quetiapine
Nursing actions: Monitor for adverse effects
Atypical Antipsychotics Administration / Meds
Administer orally or via IM route.
Risperidone: Oral solution & quick-dissolving tablets for easier administration.
Olanzapine: Orally disintegrating tablets.
Quetiapine: Immediate-release tablets for adolescents.
Aripiprazole: Tablets, orally disintegrating tablets, or oral solution for adolescents.
May be taken with or without food.
Client education:
Begin with low doses, gradually increasing.
Prototype Medication: Risperidone
Other Medications: Olanzapine, Aripiprazole, Quetiapine
Atypical Antipsychotics Indications/Contraindications
Expected Pharmacological Action
Primarily block serotonin receptors
To a lesser extent, block dopamine receptors
Also block receptors for norepinephrine, histamine, and acetylcholine
Therapeutic Uses
Autism spectrum disorder
Conduct disorder
Obsessive-compulsive disorder (OCD)
Relief of psychotic manifestations
Avoid alcohol use in adolescents
Use cautiously with cardiovascular disease, seizures, or diabetes
Clients with diabetes require baseline fasting glucose & ongoing monitoring
Selective Serotonin Reuptake Inhibitors (SSRIs) Indications/Contraindications
Expected Pharmacological Action
Blocks the synaptic reuptake of serotonin, increasing serotonin levels at the neuron junction.
Therapeutic Uses
Intermittent explosive disorder
Autism spectrum disorder
Obsessive-compulsive disorder (OCD)
Major depressive disorder
Bulimia nervosa
Generalized anxiety disorder (GAD)
May increase suicidal ideation in children/adolescents.
Abrupt withdrawal can cause discontinuation syndrome (dizziness, insomnia, nervousness, irritability, agitation). Must taper dose.
Selective Serotonin Reuptake Inhibitors (SSRIs) Complications / Interactions
Agitation, anxiety, sleep disturbance, tremors, tension headache
Nursing actions: Monitor for these adverse effects; agitation & hallucinations may indicate serotonin syndrome.
Weight changes
Client education:
Weigh weekly & report significant changes to provider.
Maintain a healthy diet.
GI effects (nausea, constipation, diarrhea, dry mouth)
Nursing actions: Monitor & report adverse effects.
Client education:
Relieve dry mouth with frequent sips of fluids or sugarless gum.
Take with food to reduce GI upset.
Concurrent use with MAOIs, SNRIs, buspirone, or St. John’s wort → Risk of serotonin syndrome.
Client education:
Avoid concurrent use.
Allow 2 weeks between fluoxetine and MAOI use.
Selective Serotonin Reuptake Inhibitors (SSRIs) Administration / Meds
Take sustained-release tablets whole, not chewed/crushed.
Explain that initial response occurs 1–3 weeks, maximum effect by 12 weeks.
Can be taken with or without food.
Morning administration minimizes sleep disturbances.
Take daily to maintain therapeutic plasma levels.
Do not abruptly discontinue.
Report suicidal thoughts immediately.
Select Prototype Medication
Fluoxetine
Sertraline
Fluvoxamine
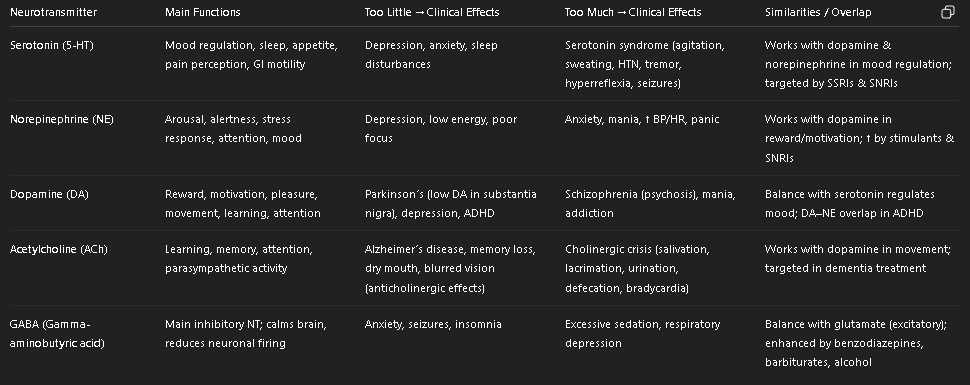
Major Neurotransmitters: Similarities & Differences (Table)
Key Similarities
Mood regulation: Serotonin, norepinephrine, dopamine all play roles in depression/anxiety.
Overlap in drug targets:
SSRIs → serotonin
SNRIs → serotonin + norepinephrine
Stimulants → dopamine + norepinephrine
Interconnected systems: Dopamine–serotonin balance influences mood/psychosis; dopamine–norepinephrine overlap affects attention/reward.
Key Differences
Serotonin → more about mood, sleep, appetite.
Norepinephrine → alertness, stress, “fight-or-flight.”
Dopamine → reward/pleasure, movement, psychosis.
Acetylcholine → memory, learning, parasympathetic.
GABA → inhibitory “brake” on the brain.
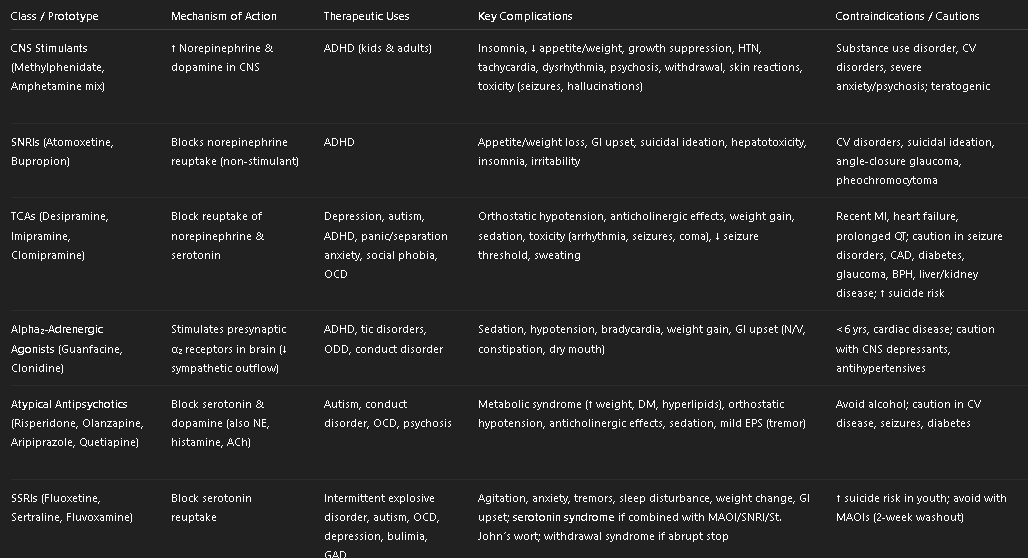
Child & Adolescent Psych Medications (Table)
CNS Stimulants (Methylphenidate, Amphetamines)
Gold standard for ADHD treatment (especially in children).
Hallmark adverse effect: appetite suppression → weight loss & growth suppression.
Buzzwords: “Give before meals, last dose before 4 PM, monitor height/weight.”
SNRIs (Atomoxetine, Bupropion)
Gold standard non-stimulant for ADHD (preferred if substance use disorder or stimulant intolerance).
No dopamine “rush” like in CNS stimulants
Hallmark risk: suicidal ideation in adolescents; hepatotoxicity.
Buzzwords: “Takes weeks for full effect, not a controlled substance.”
Tricyclic Antidepressants (Desipramine, Imipramine, Clomipramine)
Second-line/older agents used when SSRIs aren’t effective.
Hallmark toxicity: cardiac dysrhythmias & seizures in overdose → limit supply to 1 week.
Buzzwords: “Anticholinergic side effects + lethal overdose risk.”
Alpha₂-Adrenergic Agonists (Guanfacine, Clonidine)
Alternative for ADHD (esp. if insomnia, tics, or aggression are present).
Hallmark adverse effect: sedation & hypotension, rebound hypertension if abruptly stopped.
Buzzwords: “Taper slowly, monitor BP/HR, watch for drowsiness.”
Atypical Antipsychotics (Risperidone, Aripiprazole, Quetiapine, Olanzapine)
Gold standard for severe irritability & aggression in autism spectrum disorder.
Hallmark risk: metabolic syndrome (weight gain, diabetes, hyperlipidemia).
Buzzwords: “Monitor weight, glucose, cholesterol; risk of mild EPS (tremor).”
SSRIs (Fluoxetine, Sertraline, Fluvoxamine)
Gold standard for pediatric depression & anxiety disorders.
Hallmark adverse effect: serotonin syndrome (if combined with MAOI/SNRI/St. John’s wort) + suicidal ideation in youth.
Buzzwords: “Takes 1–3 weeks to start working, full effect at 12 weeks; taper slowly to avoid withdrawal.”
A nurse is providing teaching to an adolescent client who is to begin taking atomoxetine for ADHD. The nurse should instruct the client to monitor for which of the following adverse effects?
Select all that apply.
a
Somnolence
b
Yellowing skin
c
Increased appetite
d
Fever
e
Malaise
b Yellowing skin
d Fever
e Malaise
All are a potential indication of hepatotoxicity that the client should report to the provide
Insomnia, rather than somnolence, is an adverse effect that the client should report to the provider.
Insomnia vs Somnolence
Difficulty falling asleep, staying asleep, or experiencing non-restorative sleep
Excessive sleepiness during the day, even after adequate nighttime sleep.