SLHS Unit 2: Cleft Lip/Palate
1/135
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
136 Terms
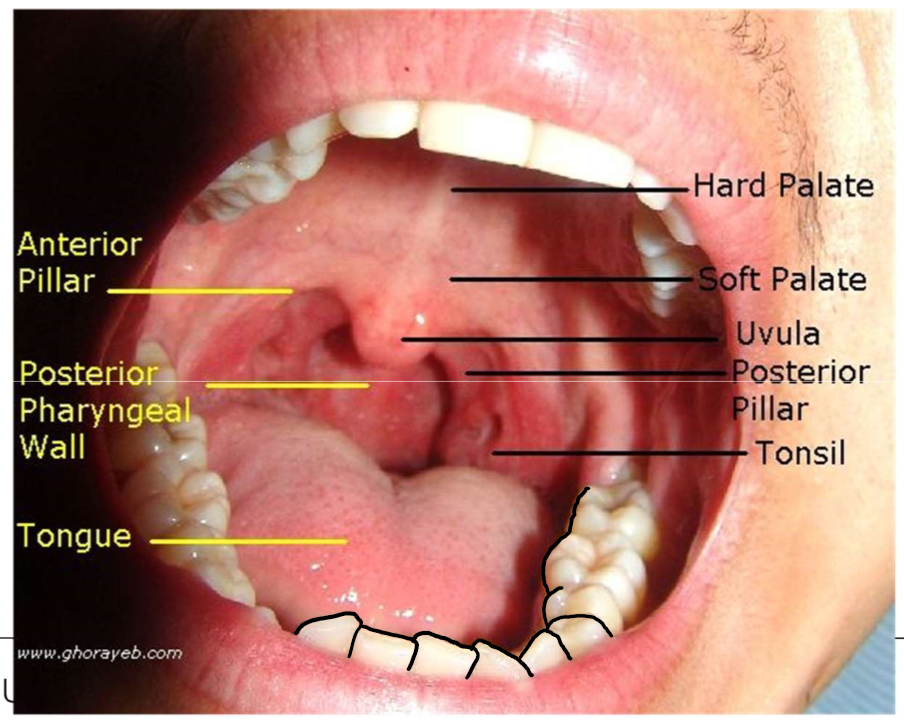
Know Anatomical Landmarks
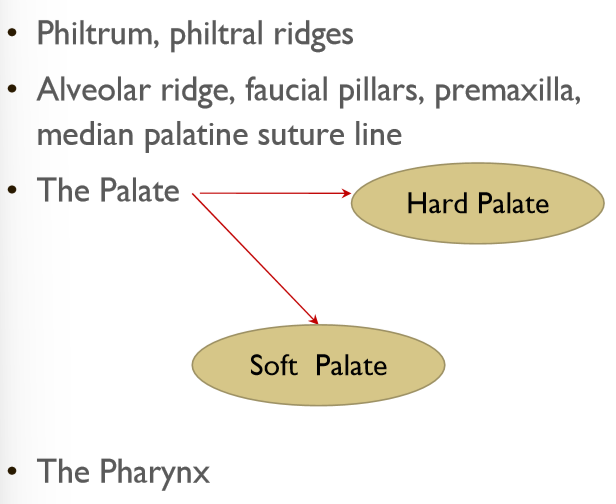
Know Oral Landmarks
Maxilla (Upper Jaw)
Fuses medially during embryogenesis
Anterior 2/3 of hard palate = palatine process of maxilla
Horizontal Plate of Palatine Bone
Posterior 1/3 of hard palate
Hard Palate:
Provides stable platform for mobile muscular valve located posteriorly
Facial & Palatal Development: 4 weeks gestation
Mandible fuses
Facial & Palatal Development: 7 weeks gestation
Lip fuses
Facial & Palatal Development: 9 weeks gestation
Hard palate fuses
Facial & Palatal Development: 12 weeks gestation
Soft palate fuses
Clefting caused by a…
Failure of the structures to fuse during early embryological development
4-7 weeks after conception
Face and anterior parts of mouth are formed
Normal development of face: result of complex fusion of 5 main embryonic processes
Mandibular processes (R and L)
Frontonasal process
Maxillary processes (R and L)
Fusion of R and L mandibular processes
Occurs 4-5 week of gestation
Fuse at the midline of the face
Frontonasal and Maxillary process
Frontonasal process grows downward
Lateral nasal and nasomedian processes fuse with maxillary process
Tissue from the nasomedian process will form the…
Anterior portion of the upper lip
Front of the alveolus
Front of the hard palate (premaxilla)
Week 7 gestation
8-12 weeks after conception
Hard and soft palates are formed
Fusion of palatal shelves
The palatal plates descend from…
…the inner side of the maxillary process
The palatal plates fuse…
from the front to the back
Nasal septum grows downward and meets the palatal plates in the midline
Soft palate starts forming around ___ weeks and is complete by ___ weeks
10
12
Velopharyngeal Port
Opening between oral and nasal cavities
Velopharyngeal Port is important for: (motor functions)
Speech, blowing, whistling, sucking, swallowing, vomiting
Velopharyngeal Port is important for: (speech sounds)
All vowels, most consonants (plosives, fricatives, affricates), pressure and nasal consonants
Velopharyngeal dysfunction
Velopharyngeal value does not close consistently and completely
Results in abnormal resonance, airflow and articulation
Velopharyngeal Valving
Closure of nasal cavity from oral cavity accomplished by coordinated action of:
Velum
Lateral pharyngeal walls
Posterior pharyngeal wall
Levator veli palatini (LVP)
Superior constrictor (SC)
Tensor veli palatini
Musculus uvulae
What is the Levator veli palatini (LVP)
Main velar elevator
Pulls velum up & back like a sling
What is the Superior constrictor (SC)
Primary sphincter
moves lateral pharyngeal walls medially and posterior pharyngeal wall anteriorly
What is the Tensor veli palatini
Tenses the soft palate
What is the Musculus uvulae
Increases velar mass during speech, making it larger target for pharyngeal contact
LVP + SC + increased mass of velum =
VP closure
Craniofacial Anomalies
Malformations that affect the head and face, and often cause speech problems
A Cleft:
Abnormal opening in an anatomical structure
Caused by failure of the structures to fuse during early embryological development
Cleft Lip and Palate Epidemiology
2nd most frequently occurring congenital deformity
Most common diagnosis: unilateral cleft lip and palate, followed by isolated cleft palate
Cleft lips show racial variability
What causes clefts?
Genetic Disorders
Chromosomal Aberrations
Teratogenically induced abnormalities
Mechanically induced abnormalities
Genetic Predisposition + Environmental Factors
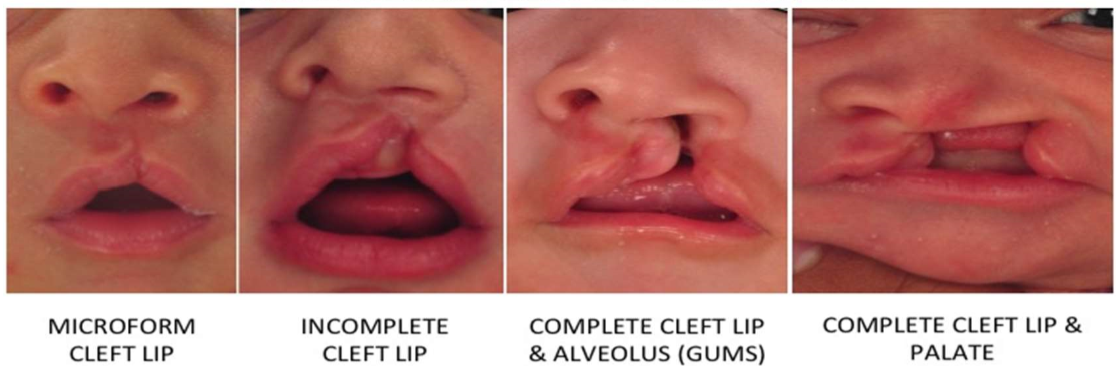
Types of Cleft Lip and Palate
Cleft lip only
Complete
Incomplete
Microform
Cleft palate only
Complete (hard and soft palate)
Incomplete (soft palate only)
Cleft lip and palate
Unilateral
Bilateral
Submucous cleft palate
Overt
Occult
Incomplete (partial) Cleft Lip
Minor “V” shaped notch in vermilion border
Complete Cleft Lip
Separation of upper lip tissue into the nostril floor

Identify:
Microform, incomplete, complete

Identify:
Bilateral and mixed one
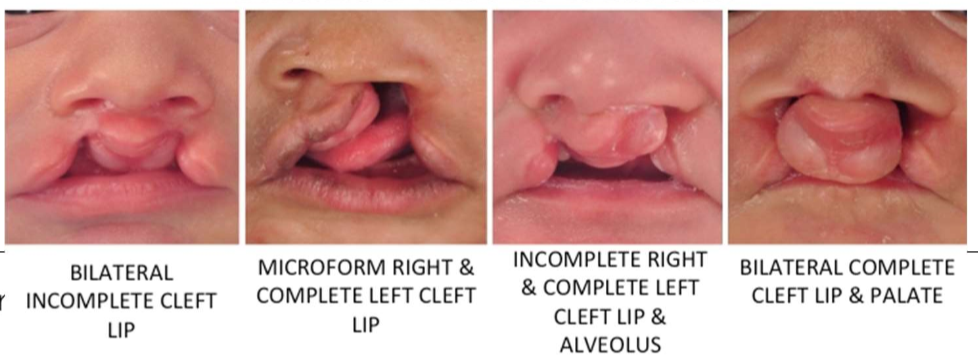
Unilateral Cleft Lip and Palate
Extends from the upper lip through the alveolus and hard and soft palate
Nasal septum attaches to the larger of the two palatal segments
Bilateral Cleft Lip and Palate
Most severe due to tissue loss
Lip and alveolus are cleft under both nostrils
Lip and premaxilla are abnormally positioned (free-floating premaxilla)
Palatal shelves completely separated
Overt (Classic) Submucous Cleft
Muscular cleft is covered by thin layer of mucosal membrane
(Can see the blue line)
Some signs that a submucous cleft is present are:
Bifid uvula
Bluish color/furrow in the middle of the soft palate zona pellucida
Notch that can be felt in hard palate
Occult Submucous Cleft
Palate appears to be normal
Lack the triad (bifid uvula, hard palate bony notch, furrow in midline of soft palate)
Muscle fibers are abnormally oriented
Leads to velar dysfunction
Velar Dysfunction
Insertion of the palate muscles onto the hard palate rather than onto the midline soft palate
Related Issues of CLP: Feeding
Can’t build up negative pressure to extract milk
Related Issues of CLP: Otitis media
Middle ear inflammation w/ accumulation of thick, mucus-like fluid
Eustachian tube often doesn’t function well
May lead to hearing loss (tubes inserted early to equalize pressure)
Related Issues of CLP: Dental Problems
Cleft usually involves the alveolus (gums)
Related Issues of CLP: Parental concerns
Can be traumatic for parents
Requires immediate professional intervention
28% of pregnancies electively terminated
Related Issues of CLP: Later Social Consequences
Teasing
Self-concept
Challenges Throughout Life: At Birth
Obstructive breathing problems, food intake problems
Can be life-threatening
Challenges Throughout Life: Early Years
Surgical closure, middle ear infections, VPD evaluations, dental construction, speech therapy
Challenges Throughout Life: Adolescence
Orthodontic treatment, secondary surgeries, psychological counseling, continuing speech therapy
Challenges Throughout Life: Adulthood
Genetic counseling
Causes of Speech Disorders Secondary to Clefts
Nasal Obstruction
Short Upper Lip
Dental/Occlusal Abnormalities
Palatal Fistula
Hearing Loss
Tonsils and Adenoids
Velopharyngeal Dysfunction
Nasal Obstruction
Anomalies of the nose and septum
Narrowing of the nares post-surgery
Midface retrusion with growth
Nasal Obstructions can cause:
Hyponasality
Cul-de-sac resonance
Airway problems
Sleep apnea
Short Upper Lip
Due to scar contraction
Possible bilabial incompetence
Dental/Occlusal Abnormalities
Quite common
Missing, malpositioned or extra teeth
Malocclusion (Class III - greatest impact)
Obligatory vs compensatory errors
Oronasal Fistula: Classifications
Post-surgical palatal hole
Most common surgical complication
Recurrence rate = 4-35%
Classified as small, medium, or large
Oronasal Fistula: Factors
Preoperative size/type of cleft
Surgical procedure
Skill of surgeon
Postoperative infection
Hearing Loss
Muscle that opens the ET during swallowing starts in the velum (tensor veli palatini)
Middle ear effusion & otitis media
Conductive HL
Pressure equalizing tubes often used
Tonsils
Lymphoid tissue
Several different types
Pharyngeal Tonsil
Palatine Tonsil
Lingual Tonsil
General term “tonsils” refers to the palatine tonsils
Adenoids (Pharyngeal Tonsils)
Lymphoid tissue
Directly above and behind the velum
Disappear with age and growth (no change in hypernasality)
May be removed for sleep apnea, hyponasal speech, poor olfaction, chronic OM
Palatine Tonsils
Do not assist with VP closure
May interfere with medial movement of the lateral pharyngeal walls or movement of the velum
Tonsillectomy: no risk for hypernasality (may improve resonance)
Velopharyngeal Dysfunction
Resonance Disorder (hyper/hyponasality)
Articulation Disorder (pharyngeal fricatives)
Communication Disorders
Abnormal resonance
Abnormal airflow and pressure
Abnormal articulation
Abnormal phonation
Abnormal Resonance
Hypernasality
Hyponasality
Cul-de-sac resonance
Mixed nasality
Hypernasality
Too much sound resonating through the nose
Most perceptible on vowels and stops (/s/, /b/, /k/)
Almost always requires surgical or prosthetic management
Hyponasality
Results from too little air escaping through the nose
Most perceptible on nasal consonants, but also vowels
Abnormal Airflow and Pressure
Nasal Emission
Nasal rustle/nasal turbulence
Nasal grimace
Nasal emission
Air emission from nose during speech due to leak in VP value
Occurs in pressure-sensitive consonants (plosives, fricatives, affricates)
Articulation problems in children with clefts may be due to:
VPD
Structural deviations
Missing/misaligned teeth
Faulty learning
Most are compensatory
Persist post surgery until the correct ways to produce phonemes are taught
Abnormal Articulation
Obligatory distortions
Compensatory articulations
Obligatory Disortions
Nasalized phonemes
Nasal emission on all pressure sounds
Compensatory Articulations
Posterior nasal fricative
Pharyngeal plosive
Pharyngeal fricative/affricate
Glottal stop
Abnormal Phonation
Increased risk for dysphonia: hoarseness, breathiness, abnormal pitch
Glottal stops
Laryngeal hyperfunction to achieve VP closure
Other congenital abnormalities of vocal cords/larynx
Breathiness may be strategy to mask hypernasality/nasal emission
Oronasal Fistula
Articulation errors and nasal emission
Midface hypoplasia and dental maloocculsion
Obligatory articulation errors
Velopharyngeal dysfunction
Hypernasality, nasal emission, weak intraoral pressure, oral for nasal sound substitutions
Vocal fold nodules
Can occur with velopharyngeal dysfunction
Can be caused by glottal stops
Nasal occlusion
Hyponasality or mixed resonance
Bilabial incompetence
Articulation errors
Effect of Cleft Lip on Feeding
May have initial difficulty latching
Usually able to breastfeed
Effect of Cleft Palate on Feeding
Babies with small SP cleft may breastfeed
Babies with complete cleft palate have feeding problems
Difficulty generating negative pressure for sucking
Problems with nasal regurgitation of milk, choking, swallowing air
Successfully bottle-fed with modifications
Assessment for Resonance Problems
Indirect procedures: nasal emission (mirror, straw), Seescape, nasometer
Perceptual Ratings
Direct Procedures: videofluoroscopy, nasoendoscopy
Assessment for Articulation Problems
Standard articulation tests
IPAT
Articulation inventories
Phonological process analysis
Oral mechanism examination
Speech Sound and Resonance Evaluation
Perceptual evaluation
Intraoral evaluation
Instrumental evaluation
Perceptual Evaluation
Use connected speech if possible
Evaluate articulation, nasal emission, resonance, voice
Intraoral evaluation
Can evaluate oral structure and function, not VP function
Instrumental evaluation
Nasometry, nasopharyngoscopy, some centers use pressure flow studies
Oral Exam
Dentition and occlusion
Oral cavity size
Presence of fistulae
Signs of submucous cleft
Movement and symmetry of uvula
Size of tonsils
Signs of upper airway obstruction
Signs of oral motor dysfunction
Mouth opens bigger
Speech Sample
Prolongation of speech
Repetition of syllables
Counting
Repetition of sentences with pressure sensitive consonants
Connected speech
Nasometry
Measure acoustic energy from oral and nasal cavities
Give objective nasalance score: ratio of oral/total (oral+nasal) energy
SeeScape
Detects nasal emissions
Indirect Assessment of Resonance
Straw and Mirror Tests
Nonvoiced, high pressure sounds
Nasopharyngoscopy
Allows direct observation of structures and function of the VP mechanism
Can see location and size of the opening
Avoids “false negatives” seen in videofluoroscopy studies
Perceptual Rating of Resonance
Best way to assess is during connected speech
Ask clients to produce sentence full of oral sounds with the nose unoccluded then occluded
Management of Resonance Problems
Persons with mild resonance problems can try behavioral therapy
Most of the time, prosthetic and surgical management is necessary and most effective
Management of Articulation Problems
Surgery/prosthetics may indirectly improve articulation
Most children will require some behavioral intervention
Typical Surgical Timelines: Lip Repair
2 ½ to 6 months