Chapter 06 Bones and Skeletal Tissues, chapter 5 the integumentary system, Chapter 04 Part A and B- Tissue: The Living Fabric, Chapter 02 Part B Chemistry Comes Alive, Chapter 03 Part A B C D, Cells: The Living Units, Chapter 02 Part A Chemistry Come…
1/590
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
591 Terms
What are the three levels of bone structure?
Gross anatomy, microscopic anatomy, chemical composition.
Describe a long bone structure.
Diaphysis: shaft with compact bone surrounding medullary cavity (yellow marrow). Epiphyses: ends, mostly spongy bone covered by compact, articular cartilage on joint surfaces. Metaphysis: between diaphysis and epiphysis, contains epiphyseal plate/line.
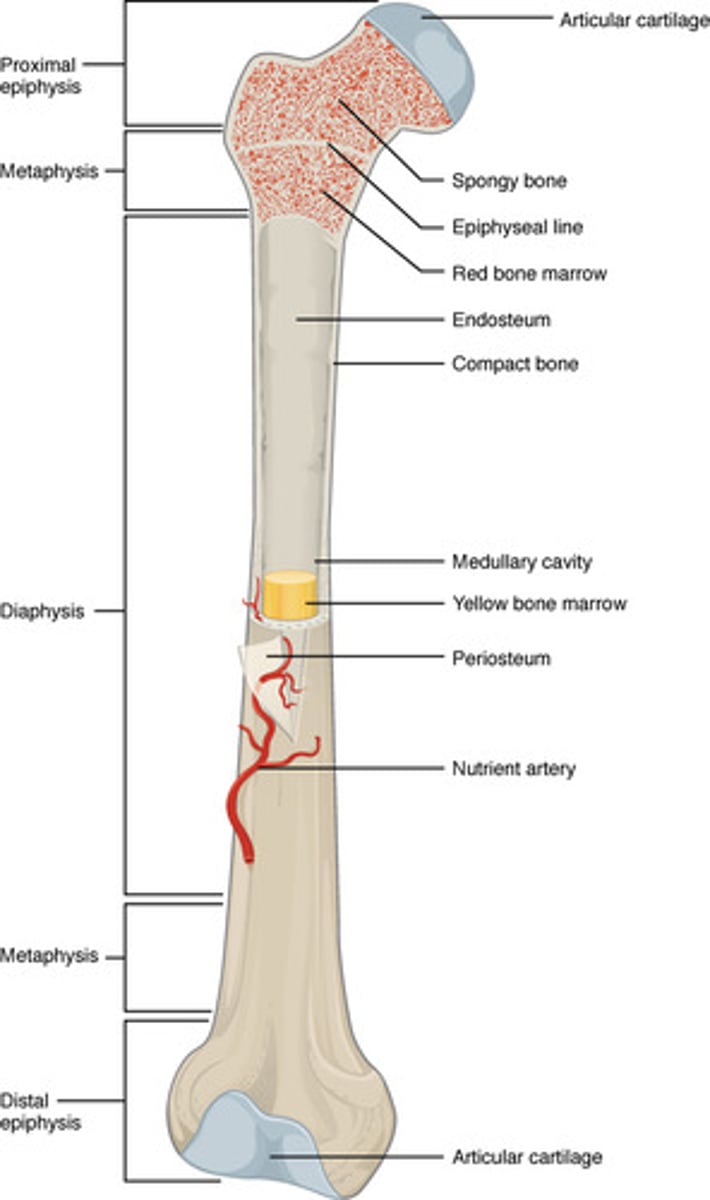
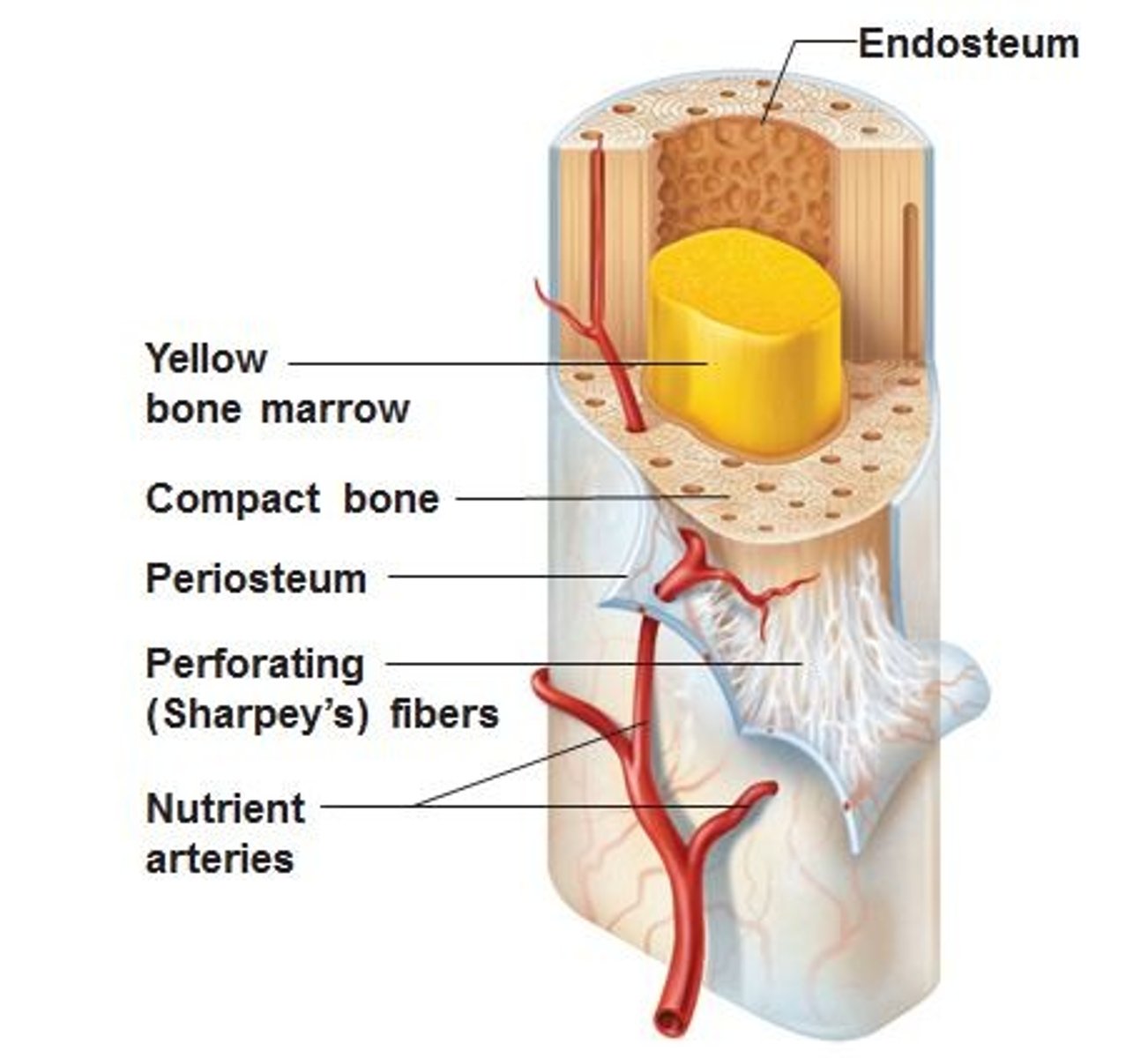
What membranes cover bone?
Periosteum: double-layered (outer fibrous dense irregular CT, inner osteogenic with osteoblasts/osteoclasts/osteogenic cells); rich in blood vessels and nerves; anchored by Sharpey's fibers; covers external bone (not joints). Endosteum: delicate CT covering trabeculae and canals inside bone.
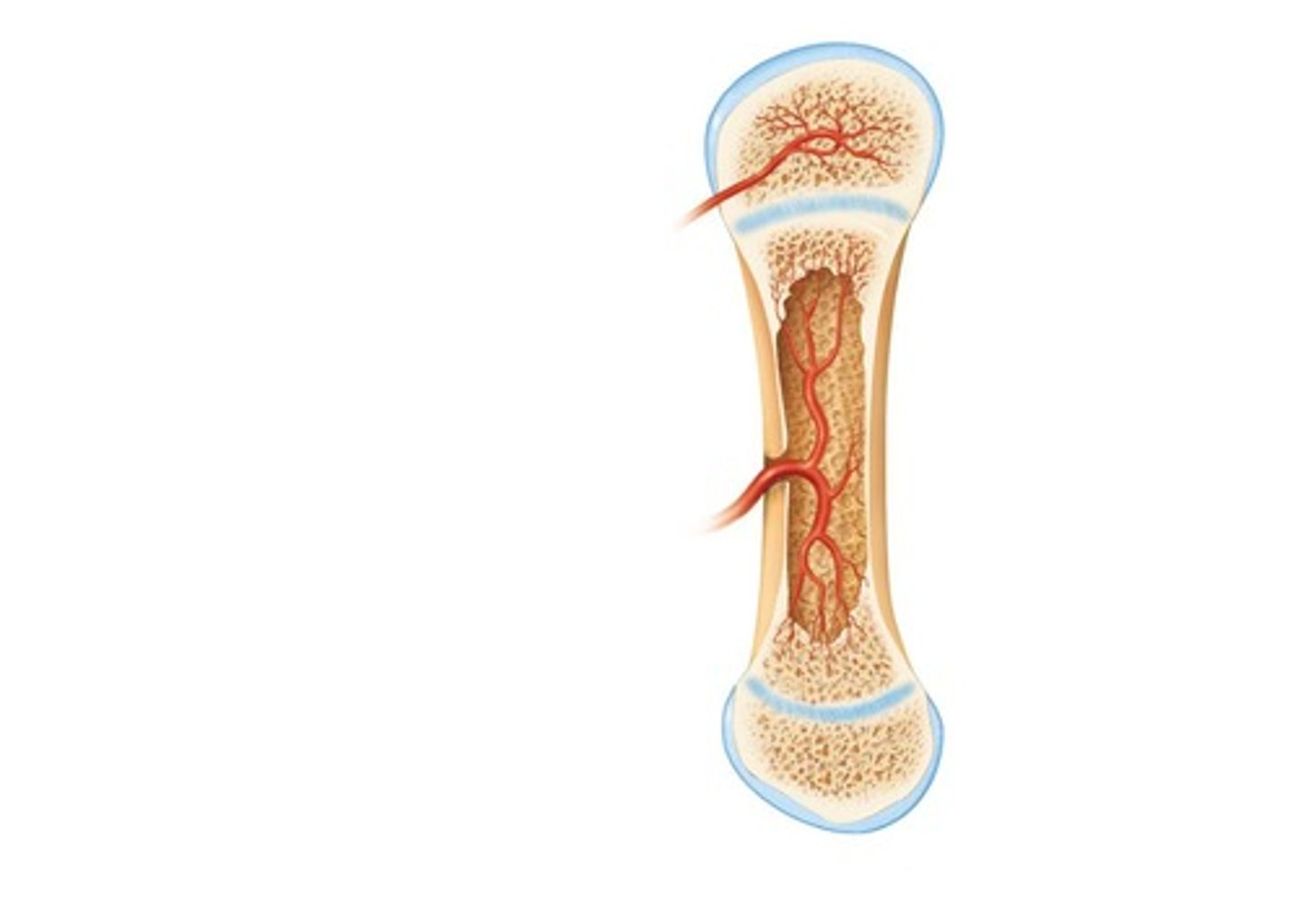
Where is hematopoietic tissue found?
Red marrow. In newborns: medullary cavities and all spongy bone. In adults: heads of femur/humerus, flat bones (sternum), irregular bones (hip). Yellow marrow can revert to red if necessary.
What are bone markings?
Projections (sites of muscle/ligament attachment, e.g., tuberosity, crest, trochanter, spine, process), surfaces (form joints, e.g., head, facet, condyle, ramus), depressions/openings (passageways, e.g., foramen, groove, fissure, notch, fossa, meatus, sinus).
What are the four cell types in bone tissue?
Osteogenic (stem cells), osteoblasts (secrete bone matrix/osteoid), osteocytes (mature cells in lacunae, maintain matrix, sense stress/strain), bone-lining cells (periosteal and endosteal, maintain matrix), osteoclasts (multinucleated, resorb bone).
Describe compact bone structure.
Osteon (Haversian system): structural unit, concentric lamellae around central canal. Canals/Canaliculi: central canal (blood vessels/nerves), perforating canals connect osteons. Lacunae: small cavities with osteocytes. Canaliculi: tiny canals connecting lacunae.
What is spongy bone structure?
Trabeculae align along stress lines, no osteons, contain irregular lamellae and osteocytes connected by canaliculi, nutrients diffuse from endosteum capillaries.
What is the organic component of bone?
Osteoid: ground substance (proteoglycans, glycoproteins) + collagen fibers. Provides tensile strength, flexibility.
What is the inorganic component of bone?
Hydroxyapatites (mineral salts, mainly calcium phosphate crystals). Provide hardness and resistance to compression. Bone is half as strong as steel in resisting compression, as strong as steel in resisting tension.
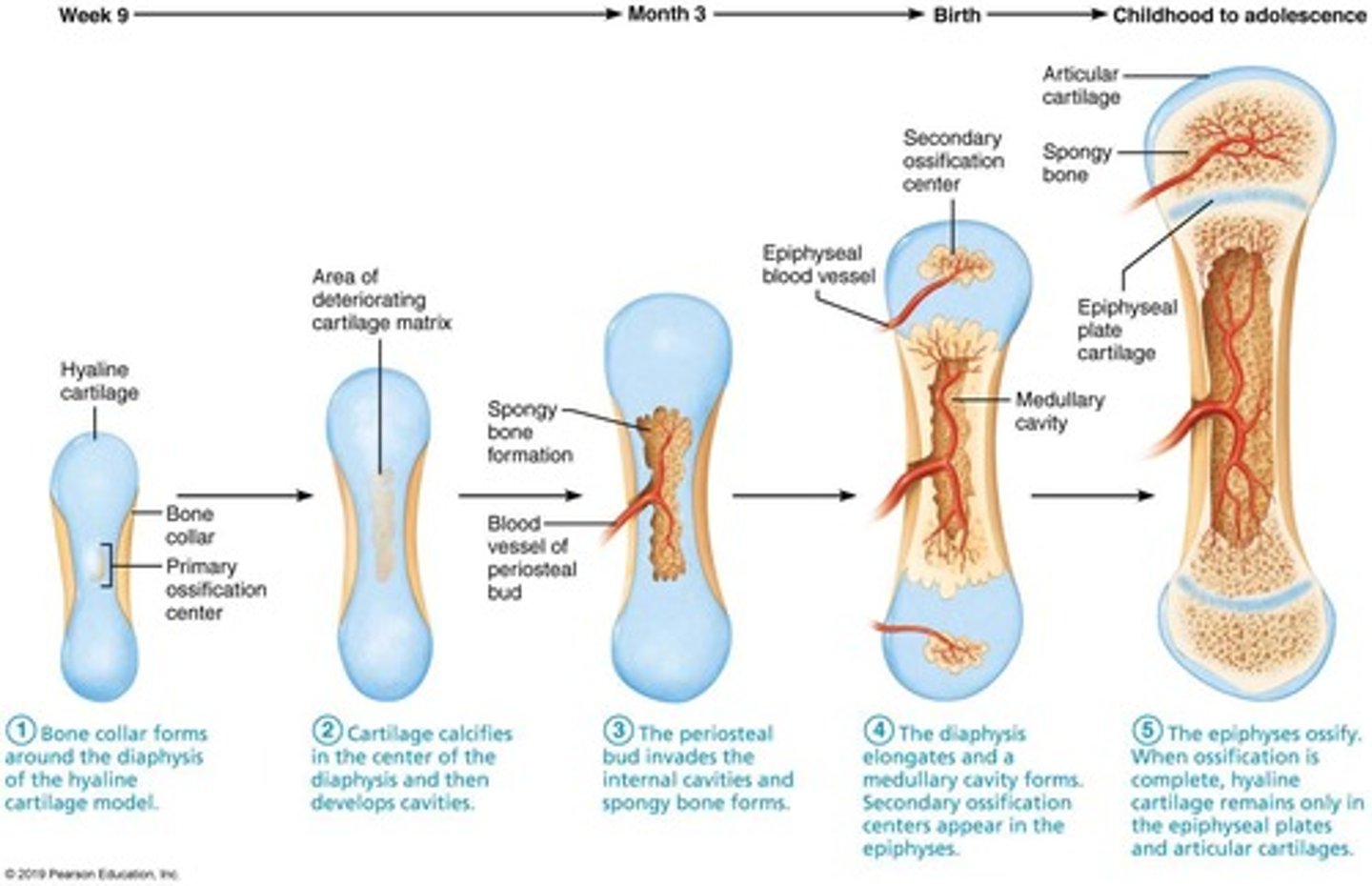
When does ossification (osteogenesis) occur?
Embryonic development (formation of bony skeleton), postnatal bone growth, bone remodeling/repair.
What are the two types of ossification?
Intramembranous (from fibrous membrane, forms flat bones like skull and clavicle).
Endochondral (from hyaline cartilage, forms most of skeleton).
Describe intramembranous ossification.
Forms flat bones. Steps: ossification centers form in fibrous membrane; osteoid secreted and calcifies; woven bone and periosteum form; lamellar bone replaces woven bone, red marrow appears.
How does interstitial growth occur at epiphyseal plates?
Epiphyseal plate maintains constant thickness. Zones: resting, proliferation (chondrocytes divide), hypertrophic (cells enlarge), calcification (matrix calcifies, cells die), ossification (new bone forms).
What happens at the end of adolescence in bone growth?
Epiphyseal plate closure: chondroblasts divide less, plate thins and is replaced by bone. Epiphyseal plate becomes epiphyseal line. Bones lengthen until ~18 (females), 21 (males).
How does appositional growth occur?
Increase in bone thickness. Osteoblasts beneath periosteum secrete matrix; osteoclasts remove bone endosteum. Usually more building than breaking → stronger bones.
What hormones regulate bone growth?
Growth hormone (stimulates epiphyseal plate). Thyroid hormone (modulates growth hormone). Sex hormones (testosterone, estrogens) at puberty promote growth spurt and plate closure.
What is bone remodeling?
Continuous bone deposit/resorption (5-7% of bone mass recycled each week). Occurs at periosteum and endosteum. Involves osteoblasts and osteoclasts.
What is bone resorption?
Osteoclasts secrete lysosomal enzymes (digest matrix), H+ to dissolve minerals. Accomplished by transcytosis into interstitial fluid and blood. Controlled by parathyroid hormone and mechanical stress.
What is bone deposition?
Occurs when bone is injured or strength needed. Requires osteoblast activity. Osteoid seam (new matrix), calcification front marks transition.
What controls bone remodeling?
Hormonal control (parathyroid hormone increases resorption, calcitonin weakly lowers blood calcium, leptin may inhibit osteoblasts, serotonin affects osteoblast activity). Mechanical stress (Wolff's Law: bone grows/remodels in response to forces).
What is Wolff's Law?
Bones remodel according to stress demands. Trabeculae align along lines of stress. Thickened midshaft where bending stress is greatest. Explains handedness, bone features, atrophy with disuse.
What are common bone fractures?
Comminuted (broken into 3+ pieces), compression (crushed), spiral (ragged break from twisting), epiphyseal (epiphysis separates from plate), depressed (pressed inward), greenstick (incomplete, one side breaks, other bends).
What are the stages of bone repair?
1. Hematoma forms. 2. Fibrocartilaginous callus forms. 3. Bony callus forms. 4. Bone remodeling occurs.
What is osteoporosis?
Group of diseases, bone resorption outpaces deposit. Spongy bone of spine/neck of femur most vulnerable. Leads to fractures.
What structures make up the integumentary system?
Skin, hair, nails, sweat glands, sebaceous (oil) glands.
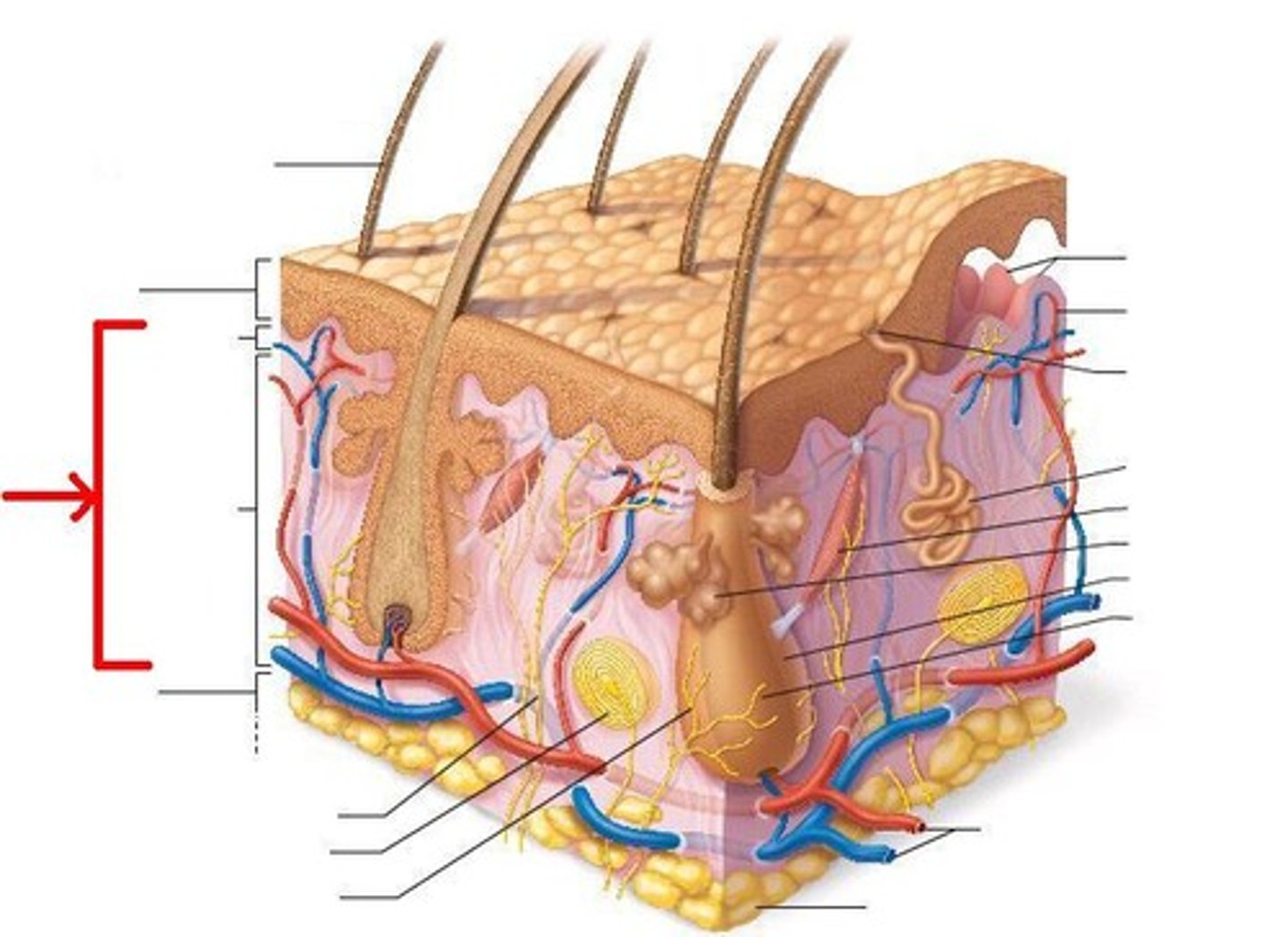
What are the main regions of the skin and their characteristics?
Epidermis: superficial, epithelial tissue, avascular. Dermis: fibrous connective tissue, vascular. Hypodermis (superficial fascia): not technically part of skin; mostly adipose tissue that absorbs shock, insulates, and anchors skin to muscles.
What are the four main cell types of the epidermis and their functions?
1. Keratinocytes - produce keratin; tightly connected by desmosomes; millions shed daily.
2. Melanocytes - produce melanin in deepest epidermis, stored in melanosomes, protect DNA from UV damage.
3. Dendritic (Langerhans) cells - immune macrophages.
4. Tactile (Merkel) cells - sensory touch receptors.
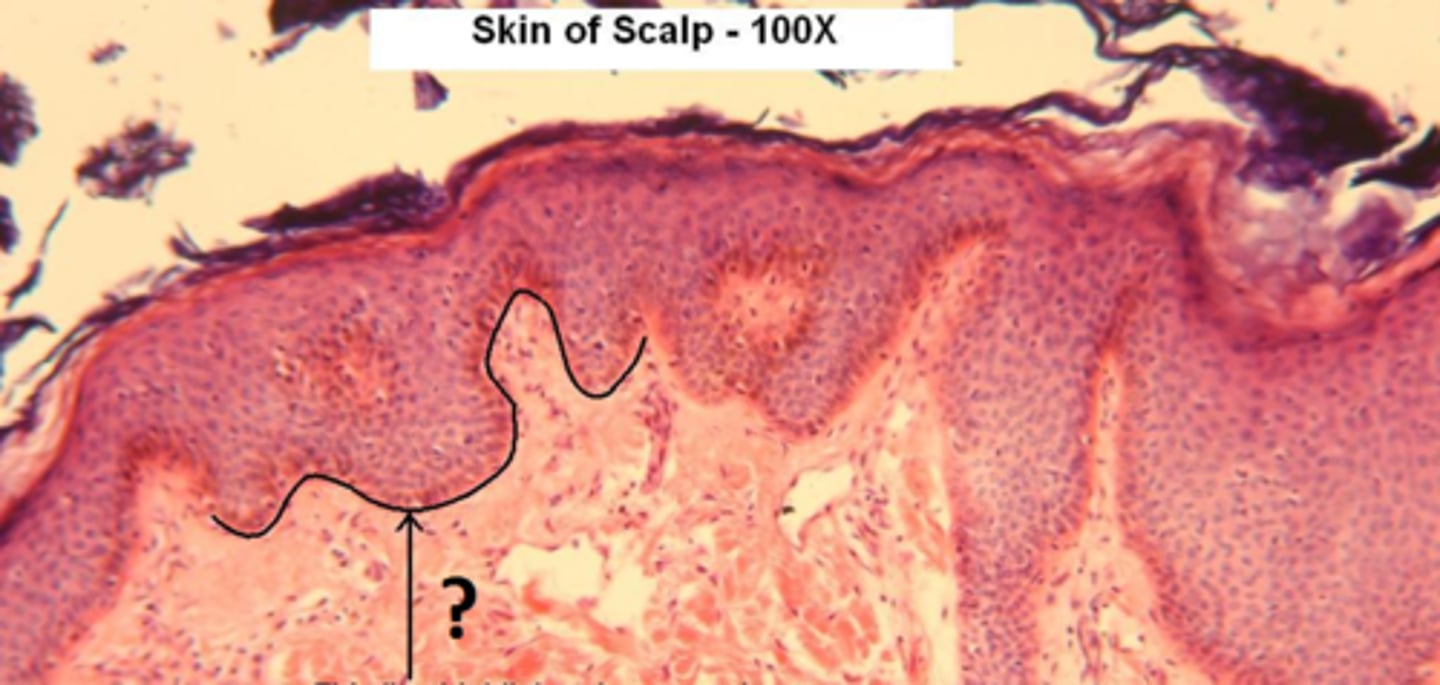
What are the layers of the epidermis (from deep to superficial)?
Stratum basale, Stratum spinosum, Stratum granulosum, Stratum lucidum (only in thick skin), Stratum corneum.
Describe the stratum basale.
Deepest layer, attached to dermis, single row of actively dividing stem cells; produces daughter cells (one migrates upward, one remains as stem cell). Also called stratum germinativum. 10-25% melanocytes.
Describe the stratum spinosum.
Several layers thick; keratinocytes appear spiny due to desmosomes (prickle cells). Contains prekeratin filaments, abundant melanosomes, dendritic cells.
Describe the stratum granulosum.
4-6 layers thick; cells flatten, nuclei and organelles disintegrate. Keratinization begins. Cells accumulate keratohyaline granules (form keratin fibers) and lamellar granules (glycolipid to slow water loss). Cells above die.
Describe the stratum lucidum.
Found only in thick skin. Thin, translucent band of 2-3 rows of clear, dead keratinocytes. Superficial to stratum granulosum.
Describe the stratum corneum.
Outermost layer, 20-30 rows of flat, dead, keratinized cells. ¾ of epidermal thickness. Functions: protects deeper cells, prevents water loss, resists abrasion and penetration, barrier to biological/chemical/physical assaults.
How do epidermal cells change as they move from basal layer to surface?
They undergo apoptosis (programmed cell death). Dead cells slough off as dandruff/dander (~50,000 per minute).
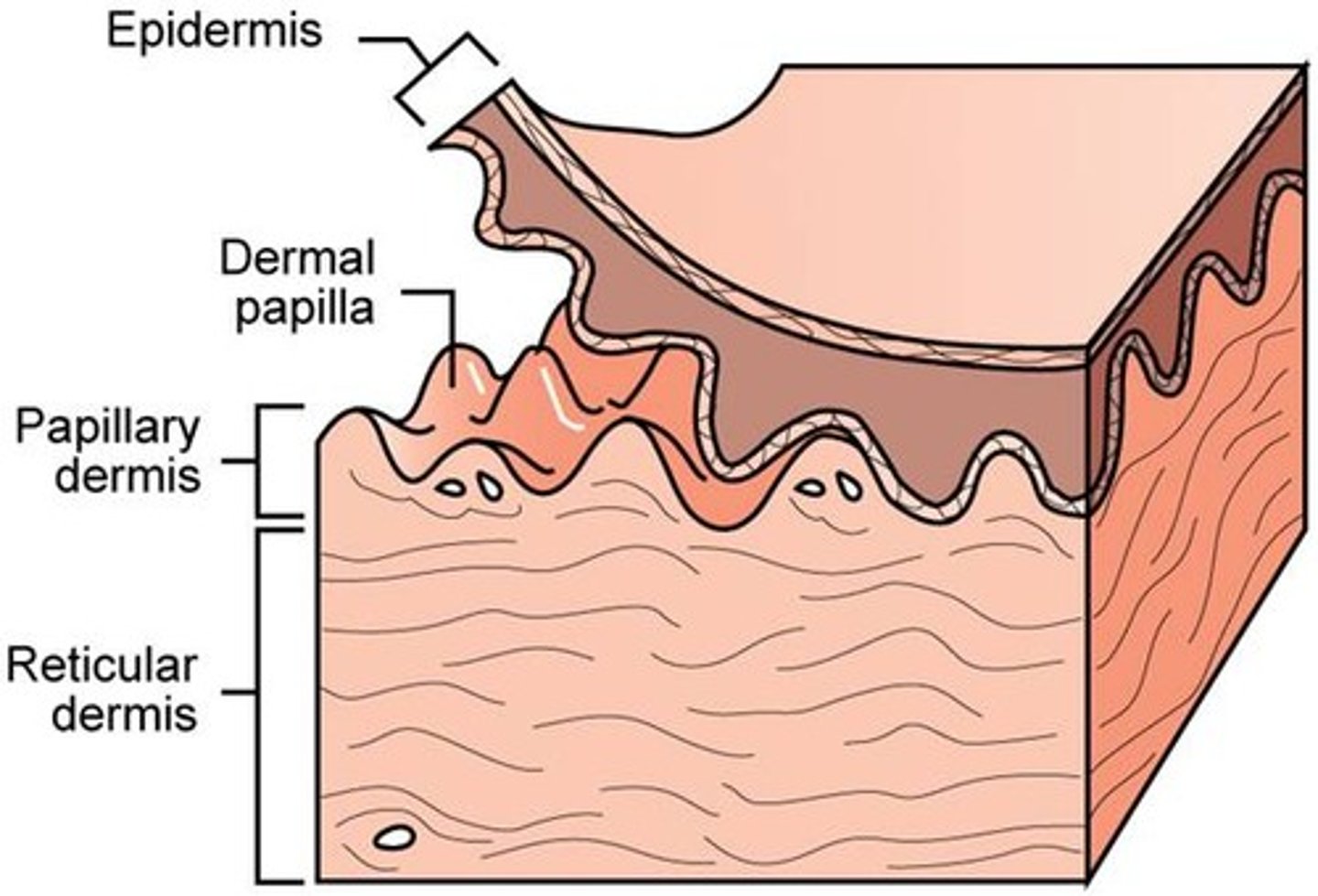
What is the dermis composed of?
Strong, flexible connective tissue with fibroblasts, macrophages, mast and white blood cells. Contains nerves, blood vessels, lymphatics, hair follicles, oil and sweat glands. Two layers: papillary and reticular.
Describe the papillary layer of the dermis.
Superficial areolar connective tissue with collagen/elastic fibers and blood vessels. Dermal papillae project into epidermis (capillary loops, free nerve endings, tactile/Meissner's corpuscles). In thick skin, forms friction ridges (fingerprints).
Describe the reticular layer of the dermis.
~80% of dermis. Dense irregular connective tissue with elastic fibers (stretch-recoil) and collagen (strength/resiliency, binds water). Contains cutaneous plexus (blood vessels), adipose pockets. Has cleavage lines (important for surgery) and flexure lines (near joints, deep creases).
What pigments contribute to skin color?
Melanin: only pigment made in skin by melanocytes, shields DNA from UV, more sun → more melanin. Carotene: yellow-orange pigment, visible in palms/soles, accumulates in stratum corneum/hypodermis, converted to vitamin A. Hemoglobin: pinkish hue of fair skin due to low melanin.
What are effects of excessive sun exposure?
Elastic fibers clump (leathery skin), immune suppression, DNA alteration (skin cancer), folic acid destruction (important for embryonic development), photosensitivity reactions (from drugs, perfumes, etc.).
What alterations in skin color can indicate disease?
Cyanosis: blue skin, low oxygen. Pallor: pale, due to anemia, low BP, fear/anger. Erythema: redness from fever, hypertension, inflammation, allergy. Jaundice: yellow cast, liver disorder. Bruises: clotted blood (ecchymoses/hematomas). Brown/black "necklace" in axilla/neck: may indicate insulin resistance and high blood glucose.
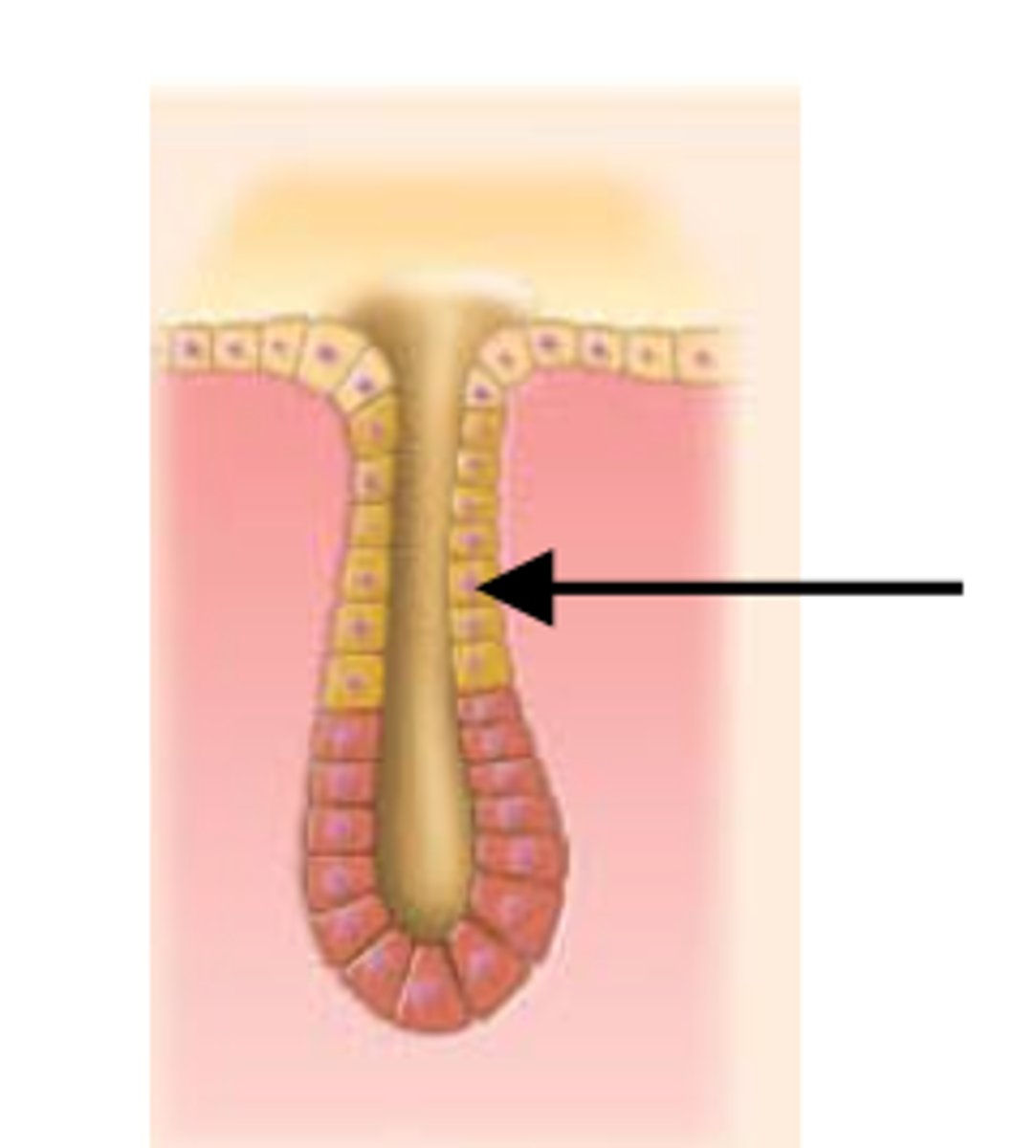
What is the structure of hair?
Flexible strand of dead keratinized cells produced by follicles. Hard keratin (durable, cells do not flake). Regions: shaft (above scalp, keratinization complete), root (in scalp, keratinization ongoing). Shaft layers: medulla (core), cortex (layers of flattened cells), cuticle (outer single cell layers). Hair pigment: melanins (yellow, rust, brown, black); pheomelanin (red); gray/white = decreased melanin + air bubbles.
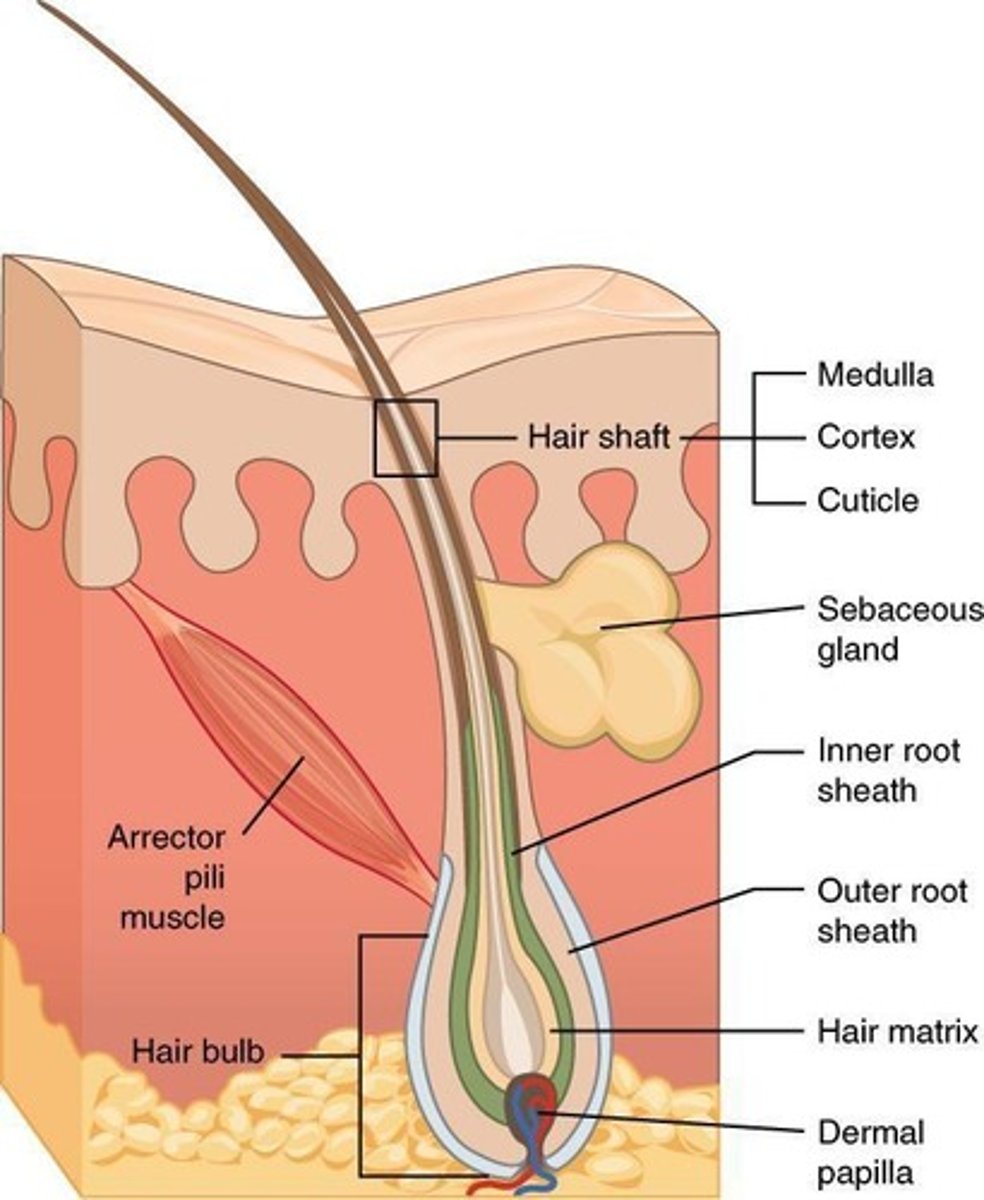
Describe hair follicles and associated structures.
Follicle extends from epidermis into dermis. Bulb at base with hair matrix (actively dividing cells) and papilla (capillaries). Root hair plexus: nerve endings (touch receptor). Arrector pili: smooth muscle causing goosebumps. Walls include connective tissue sheath, glassy membrane, epithelial root sheath.
What are alopecia and male pattern baldness?
Alopecia: hair thinning after age 40. Male pattern baldness: genetically and sex-influenced, due to follicular response to dihydrotestosterone (DHT).
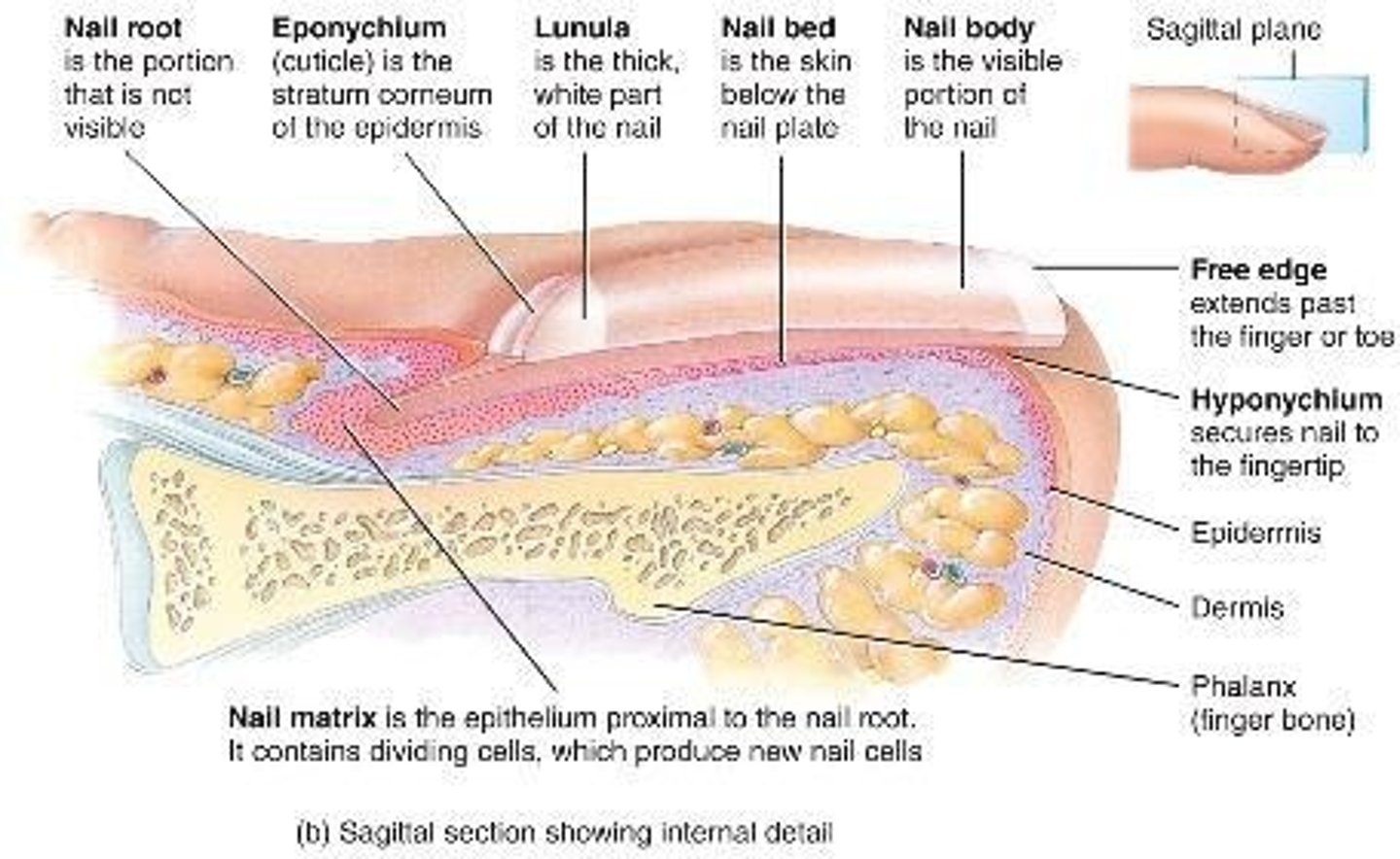
What are nails and their structure?
Scale-like modification of epidermis with hard keratin. Protects finger/toe tips. Parts: free edge, nail plate, root. Nail bed = epidermis beneath plate. Nail matrix = growth area. Nail folds = skin overlaps. Cuticle (eponychium). Hyponychium (under free edge). Lunule = white crescent (thickened matrix). Nails appear pink from capillaries.
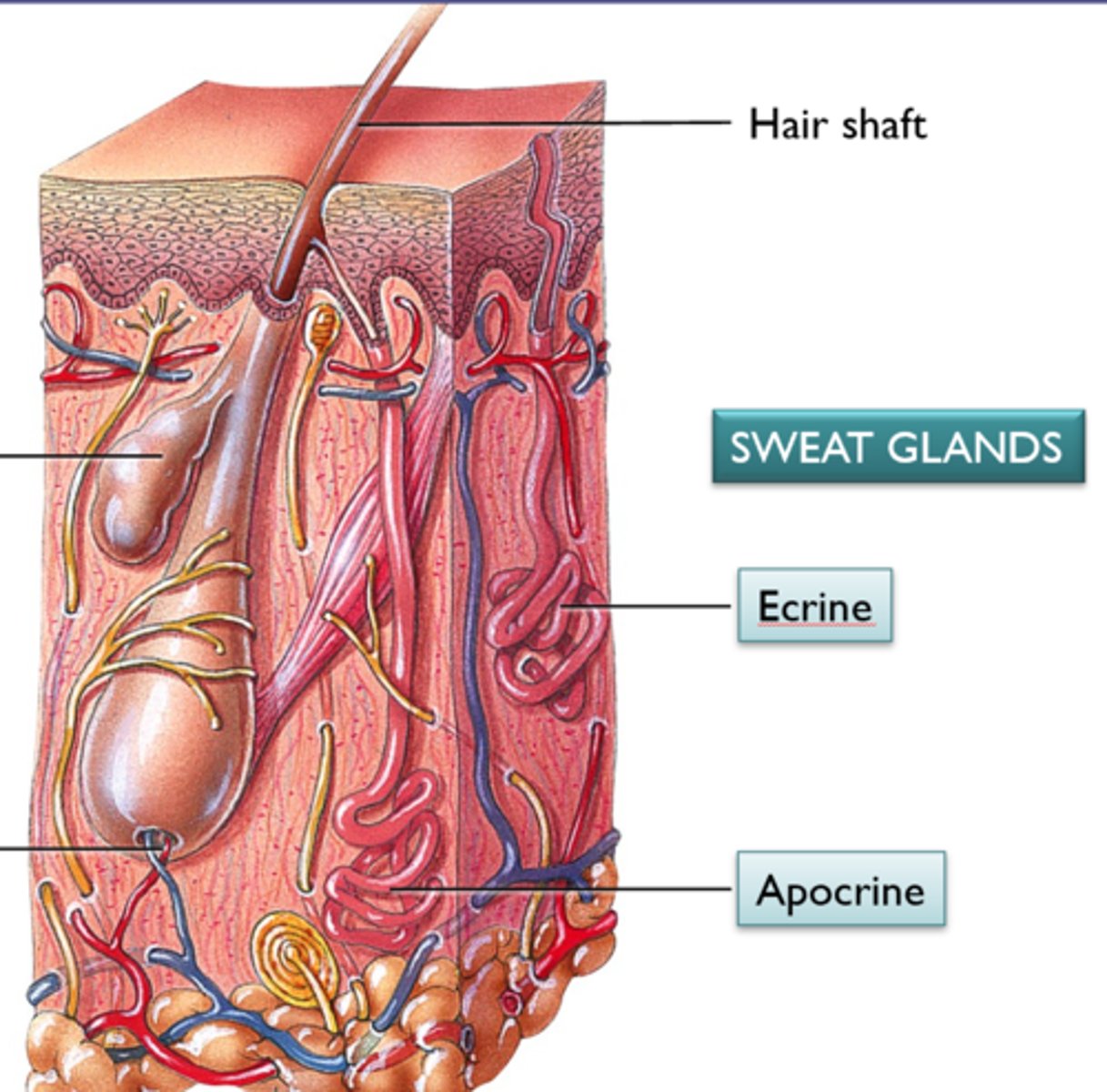
Describe eccrine sweat glands.
Most numerous, abundant on palms/soles/forehead. Ducts open to pores. Function in thermoregulation (sympathetic nervous system). Secrete sweat = 99% water + salts, vitamin C, antibodies, dermcidin, wastes.
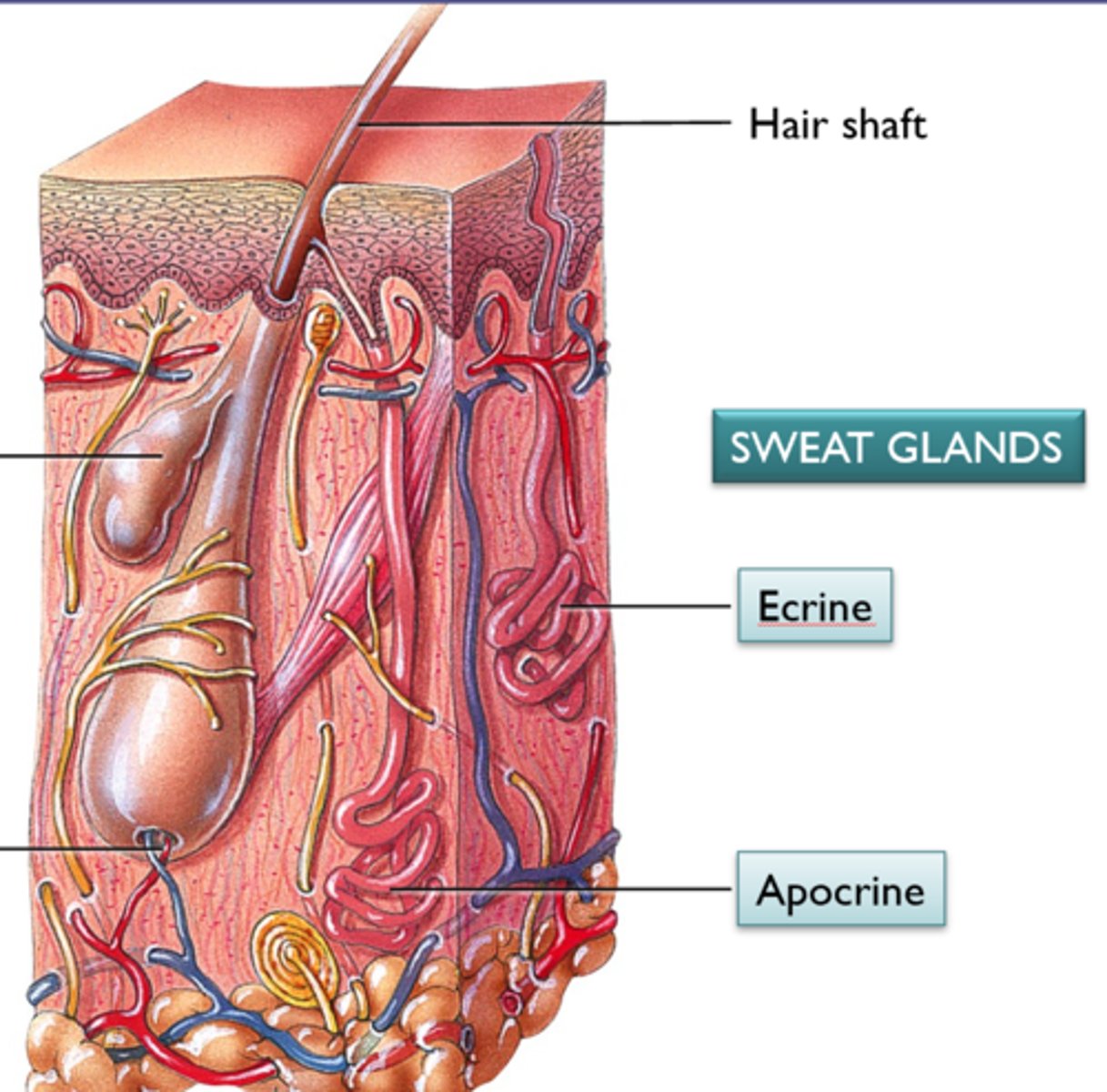
Describe apocrine sweat glands.
Confined to axillary/anogenital areas. Secrete milky/yellow sweat with fats and proteins → body odor when broken down by bacteria. Larger than eccrine, ducts empty into hair follicles. Begin at puberty, may act as scent glands. Modified apocrine: ceruminous (earwax), mammary (milk).
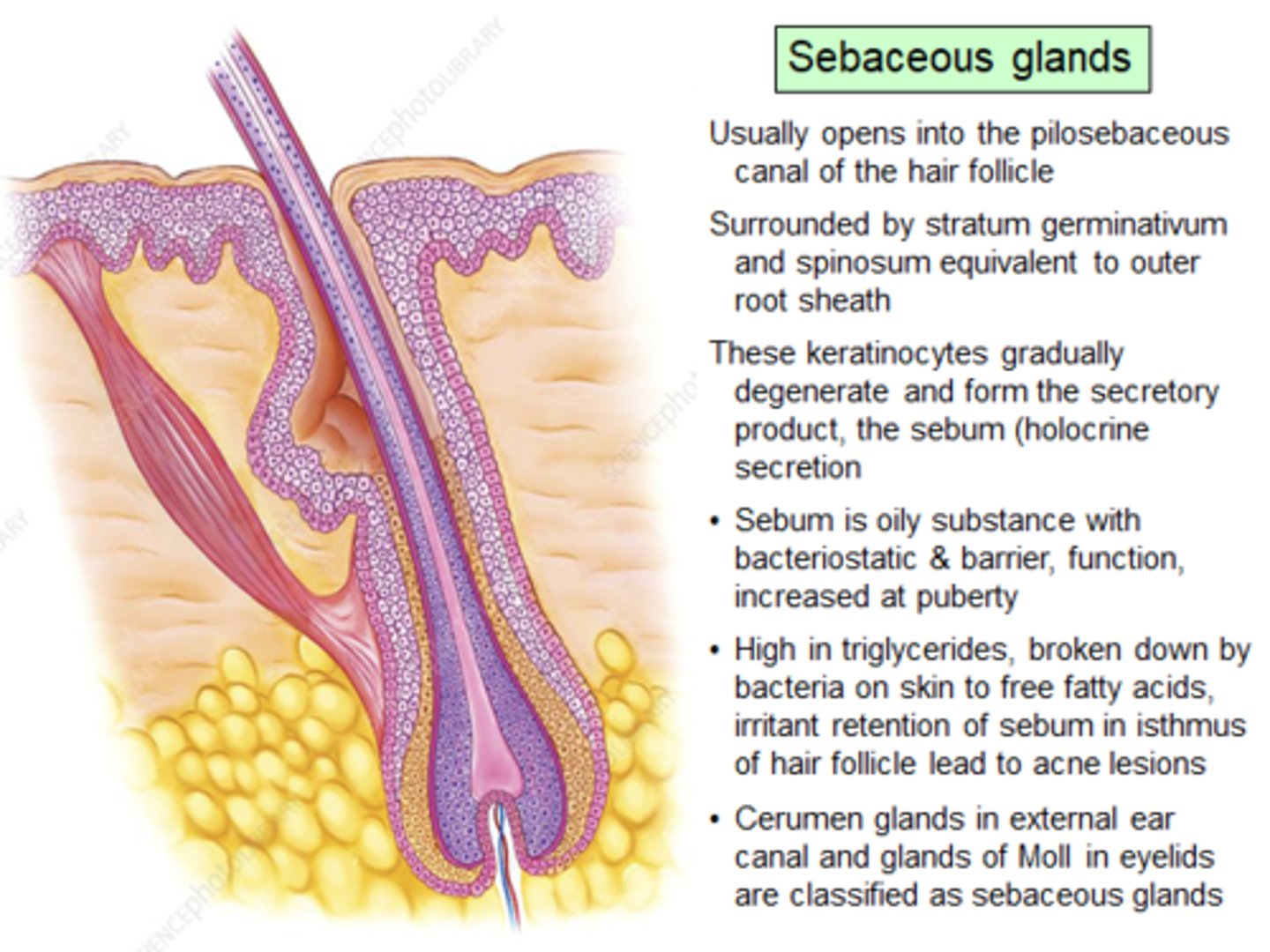
Describe sebaceous glands.
Oil glands, everywhere except palms/soles. Develop from hair follicles, secrete into follicles. Inactive until puberty (stimulated by androgens). Secrete sebum: oily holocrine secretion, bactericidal, softens hair/skin.
What are the main functions of skin?
Barrier (protection), body temperature regulation, sensations, metabolic functions, blood reservoir, excretion.
How does the skin protect the body?
Chemical barrier: sweat (antimicrobials), sebum/defensins, acid mantle, melanin (UV). Physical barrier: keratinized cells + glycolipids, limit penetration of most substances; some chemicals can cross (lipid-soluble, solvents, heavy metals, some drugs). Biological barrier: dendritic cells and macrophages activate immune system, DNA absorbs UV and converts to heat.
How does skin regulate temperature?
At rest: insensible perspiration (~500 ml/day). When hot: dermal vessels dilate, sweat increases to ~12 L/day (sensible perspiration). When cold: dermal vessels constrict, conserve heat.
What sensory functions does the skin provide?
Exteroceptors sense temperature, touch, pain via nerve endings and receptors.
What metabolic functions does the skin have?
Synthesizes vitamin D for calcium absorption. Keratinocytes disarm carcinogens, activate hormones (e.g., cortisone to hydrocortisone). Produces collagenase to prevent wrinkles.
How is the skin a blood reservoir?
Holds up to 5% of blood volume. Vessels can constrict to shunt blood to other organs.
What waste excretion does the skin perform?
Secretes nitrogenous wastes (ammonia, urea, uric acid). Sweat also removes salt and water.
What causes burns and what is the main immediate threat?
Tissue damage from heat, electricity, radiation, chemicals. Proteins denature, cells destroyed. Immediate threat = dehydration and electrolyte loss → renal shutdown, circulatory shock.
How are burns evaluated?
Rule of Nines: body divided into 11 sections, each = 9% surface area (genitals = 1%). Used to estimate fluid loss.
Four basic tissue types
Epithelial, connective, muscle, and nervous tissue.
Two main forms of epithelial tissue
Covering/lining epithelia and glandular epithelia.
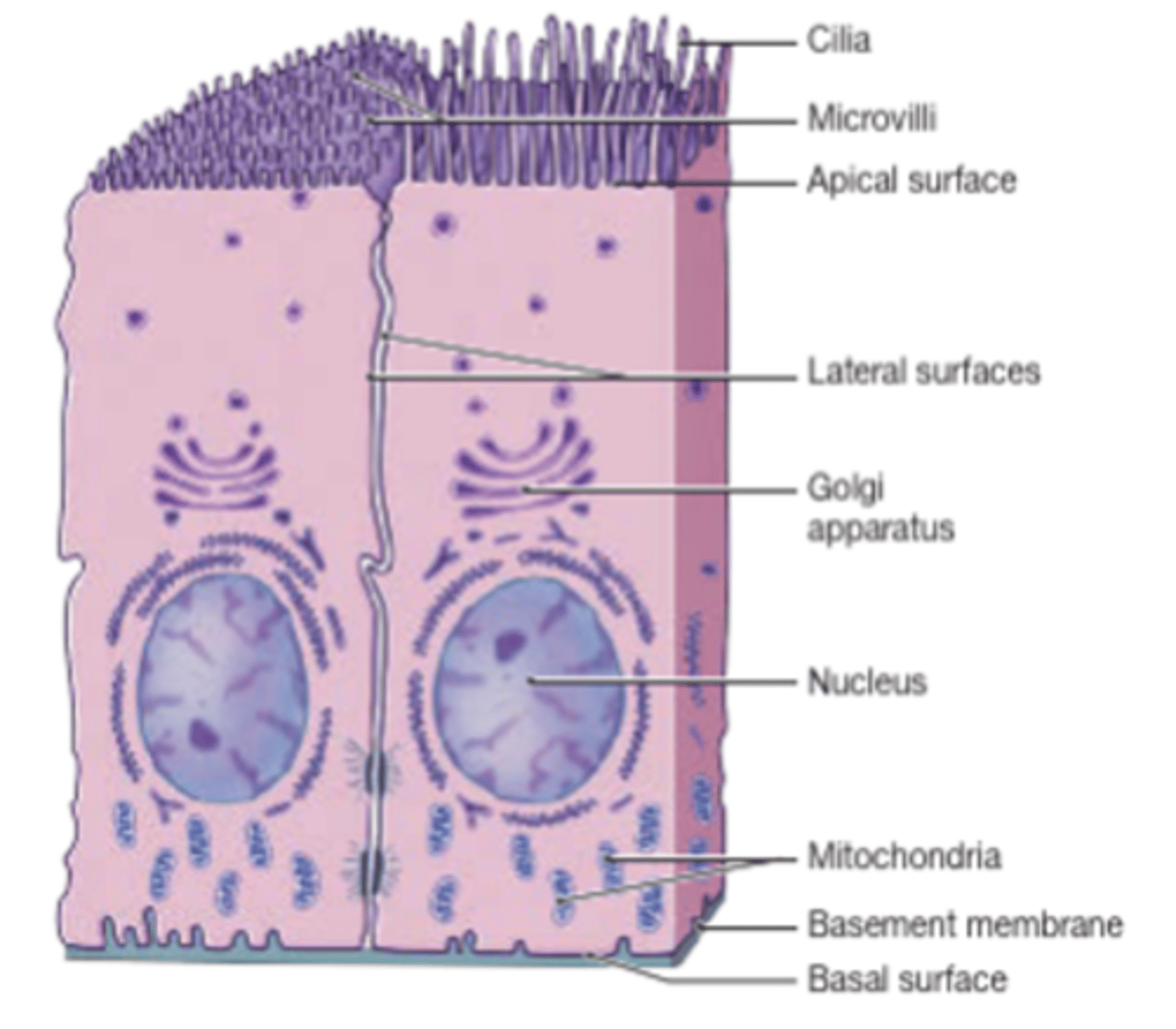
Apical surface of epithelial cells
The upper, free side exposed to the body surface or cavity; may have microvilli or cilia.
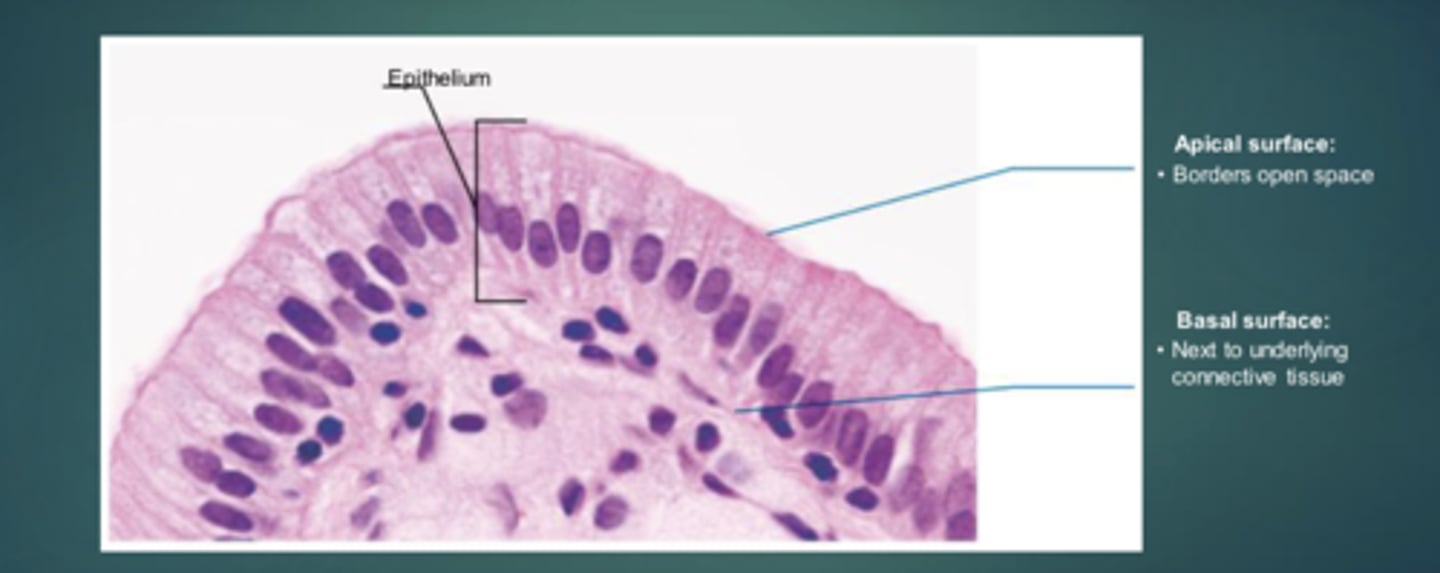
Basal surface of epithelial cells
The lower, attached side facing inward toward the body, attached to basal lamina.
Basal lamina
A glycoprotein and collagen adhesive sheet holding epithelial cells to underlying cells.
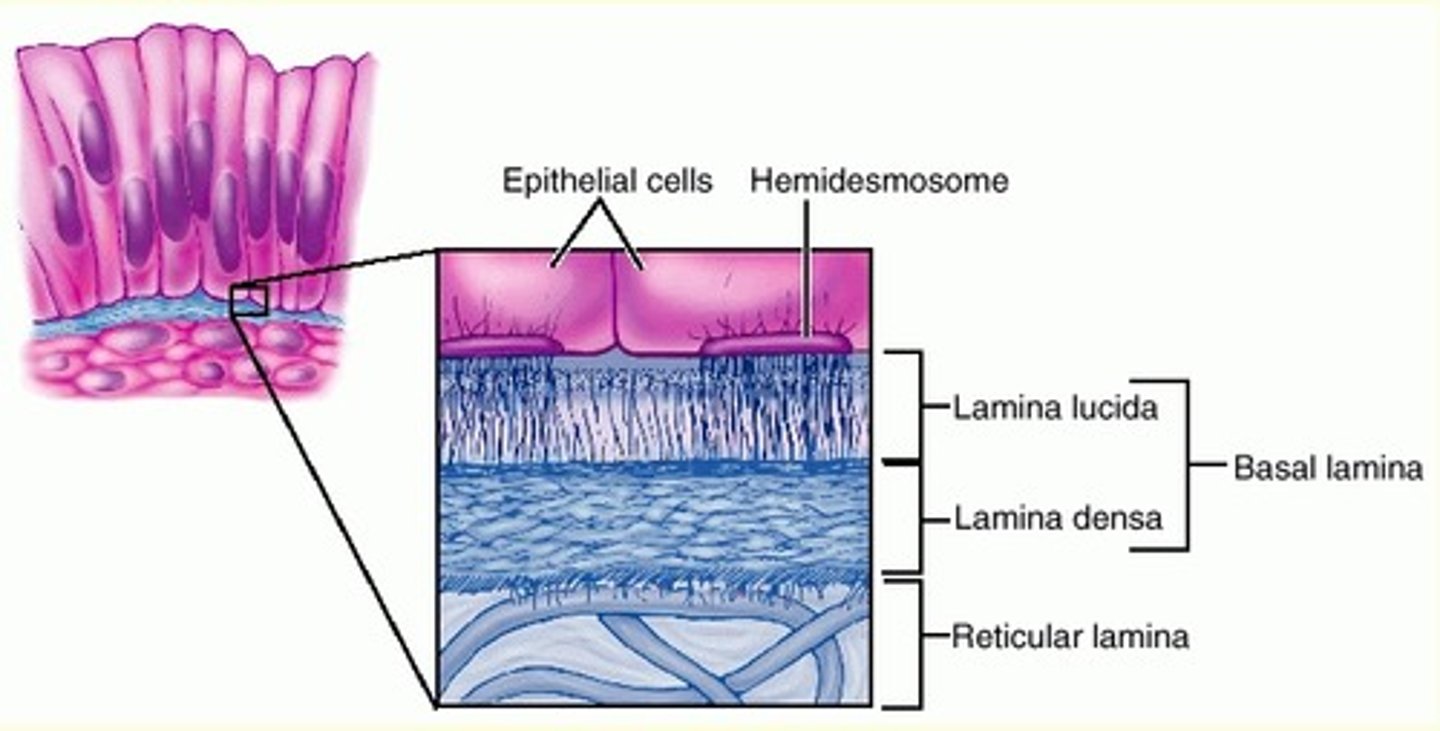
Reticular lamina
A network of collagen fibers deep to the basal lamina.
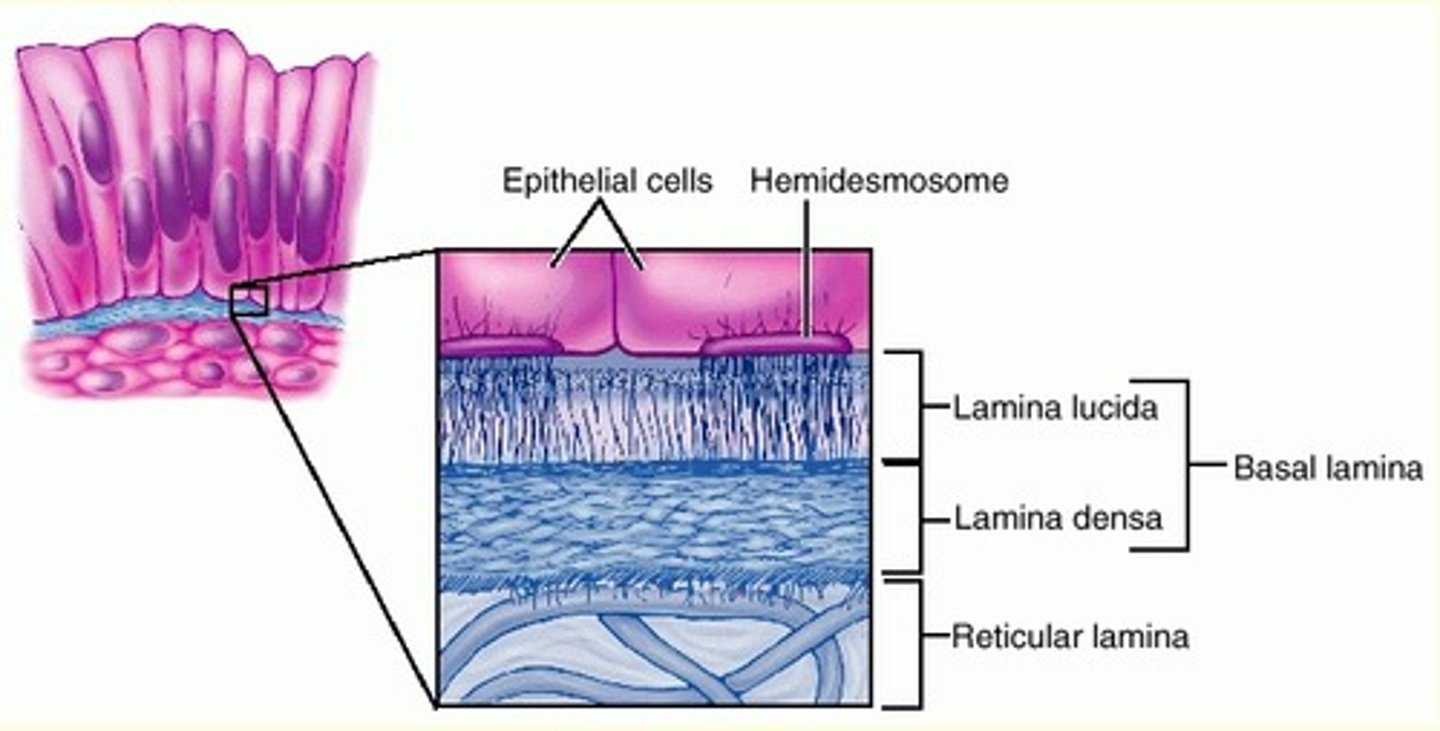
Basement membrane
Made of basal lamina and reticular lamina; reinforces epithelium, resists tearing, defines boundary.
Specialized contacts that bind epithelial cells
Tight junctions and desmosomes.
Epithelial tissue avascular but innervated
It has no blood vessels but receives nutrients by diffusion and has nerve supply.
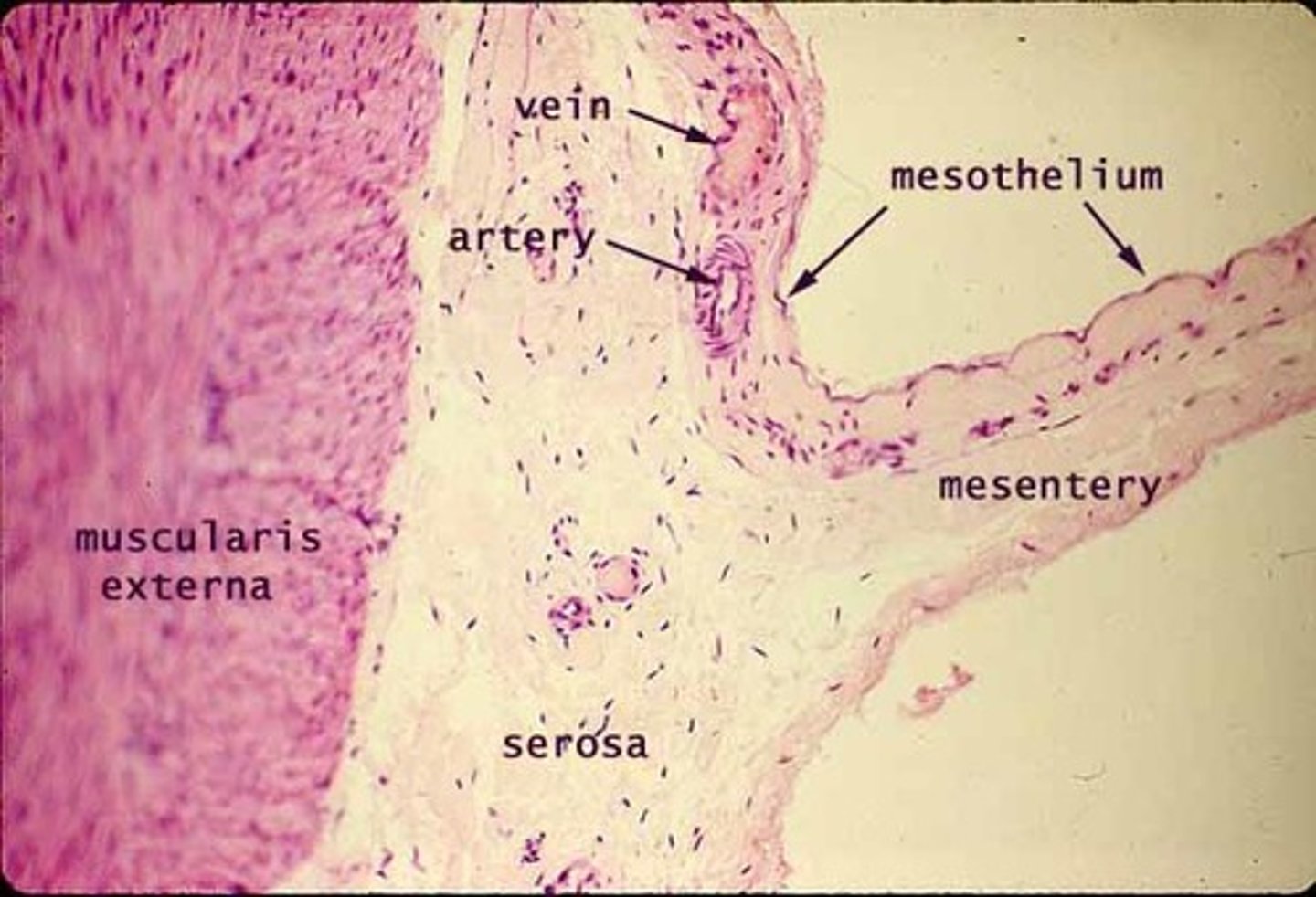
Endothelium
Simple squamous epithelium lining blood vessels, lymph vessels, and the heart.
Mesothelium
Simple squamous epithelium of serous membranes in ventral body cavity.
Simple cuboidal epithelium
Specialized for secretion and absorption; found in kidney tubules and small gland ducts.
Simple columnar epithelium
Specialized for absorption and secretion of mucus, enzymes, etc.; found in digestive tract, gallbladder.
Goblet cells
Unicellular glands secreting mucus in simple columnar epithelium.
Pseudostratified columnar epithelium
Appears stratified but is single-layered; many cells ciliated; found in upper respiratory tract.
Stratified squamous epithelium
Specialized for protection; found in skin, mouth, esophagus.
Keratinized stratified squamous epithelium
Forms epidermis; surface cells full of keratin, tough and protective.
Nonkeratinized stratified squamous epithelium
Found in moist linings (mouth, esophagus, vagina).
Stratified cuboidal epithelium
Rare; found in sweat and mammary glands.
Stratified columnar epithelium
Rare; found in pharynx, male urethra, and gland ducts.
Transitional epithelium
Found in urinary organs; cells change shape when stretched for urine storage.
Endocrine glands
Ductless glands secreting hormones into interstitial fluid/blood.
Exocrine glands
Glands that secrete products onto surfaces or into cavities via ducts (sweat, oil, saliva).
Unicellular exocrine glands
Goblet and mucous cells producing mucin.
Multicellular exocrine glands
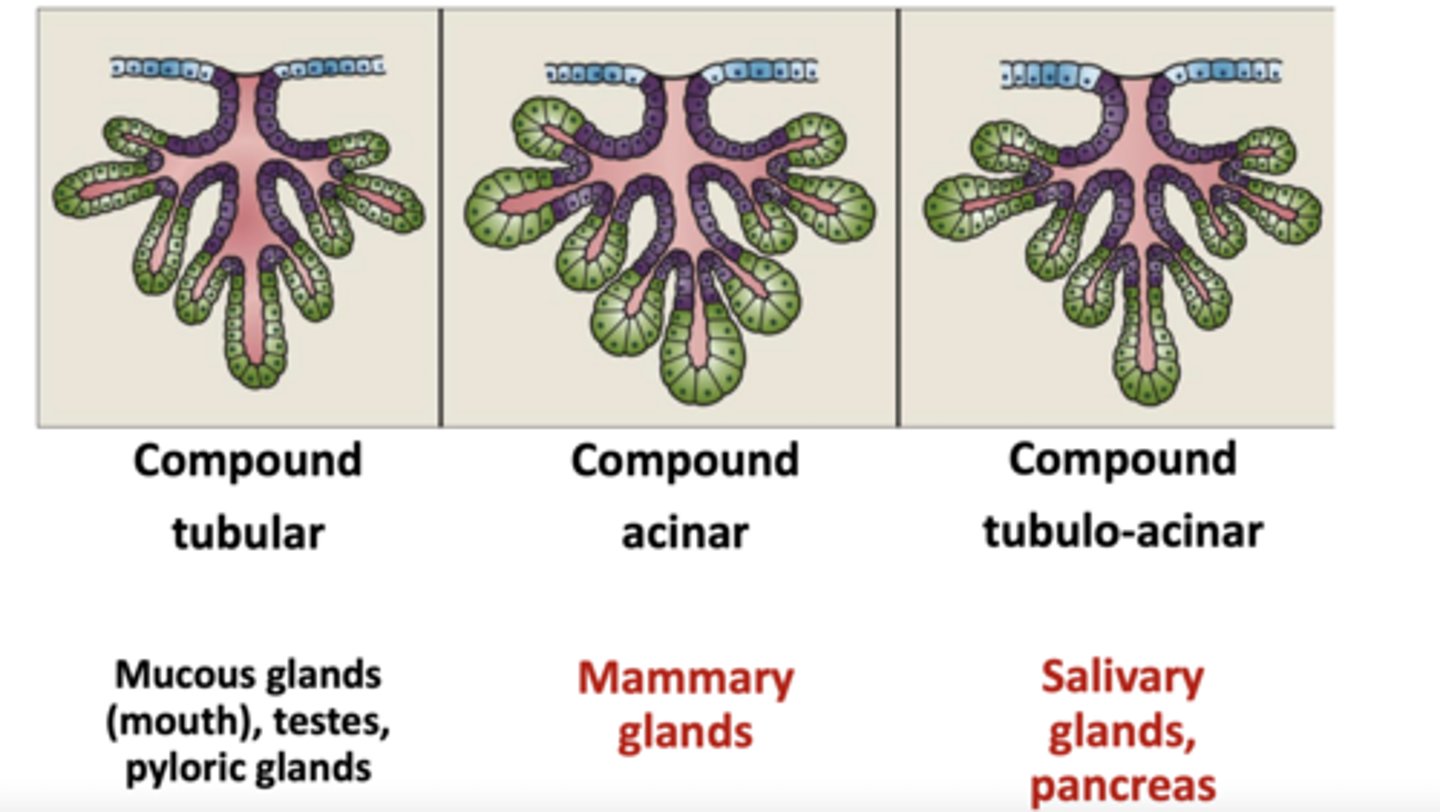
Composed of a duct and a secretory unit, often supported by connective tissue.
Simple ducts
Unbranched ducts.
Compound ducts
Branched ducts.
Holocrine secretion
Secretion by rupture.
Apocrine secretion
Secretion where the apex ruptures.
Functions of connective tissue
Binding, support, protection, insulation, storage, transport.
Four main classes of connective tissue
CT proper, cartilage, bone, blood.
Ground substance
Gel-like material between cells; medium for diffusion; contains interstitial fluid, adhesion proteins, proteoglycans.
Collagen fibers
Strongest, most abundant fibers; high tensile strength.
Elastic fibers
Thin elastin fibers allowing stretch and recoil.
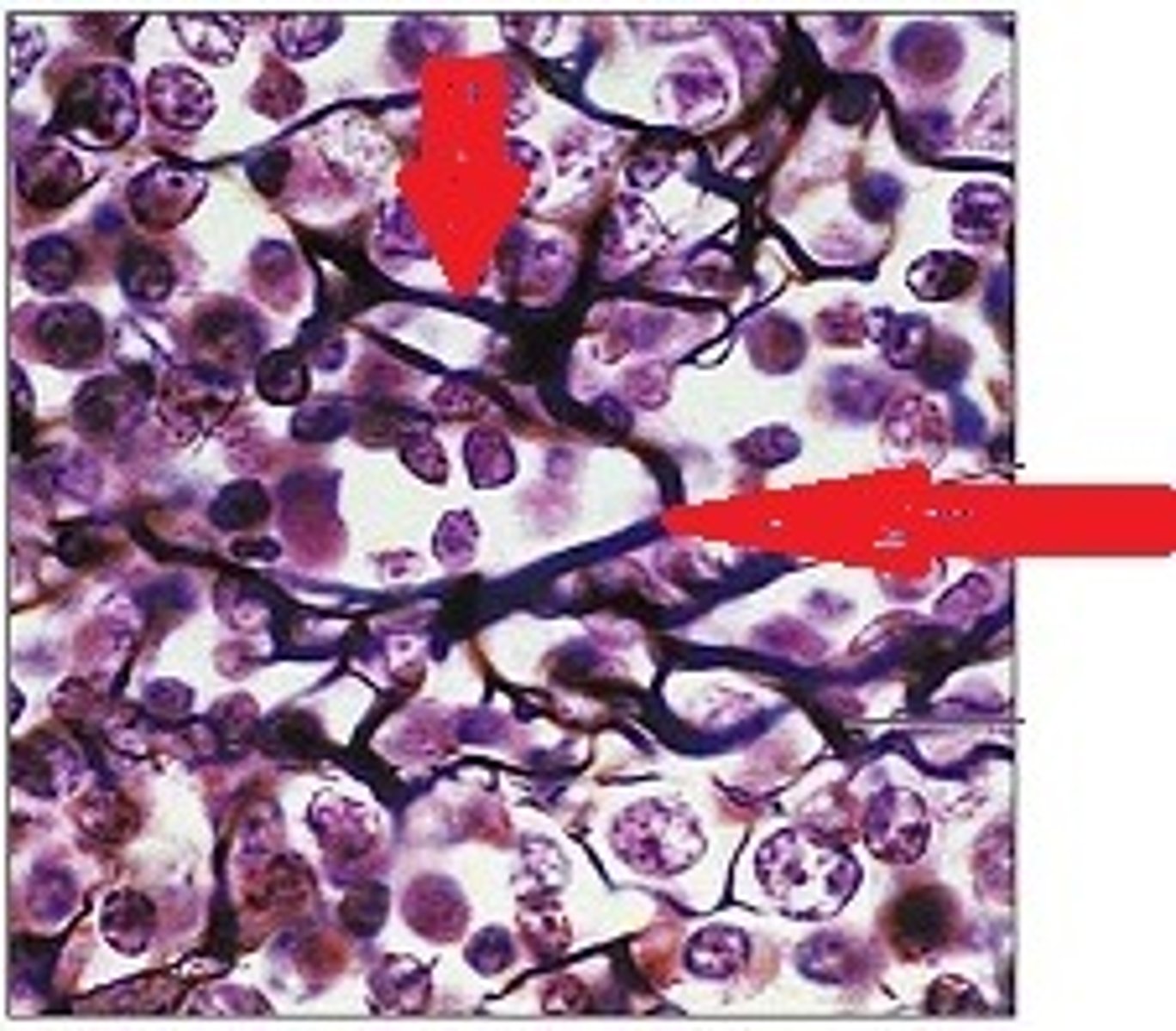
Reticular fibers
Short, fine collagenous fibers forming supportive networks.
Fibroblasts
Blast cells of connective tissue proper.
Chondroblasts
Blast cells of cartilage.
Osteoblasts
Blast cells of bone.
Hematopoietic stem cells
Blast cells producing blood cells in bone marrow.
Adipocytes
Fat cells that store nutrients.
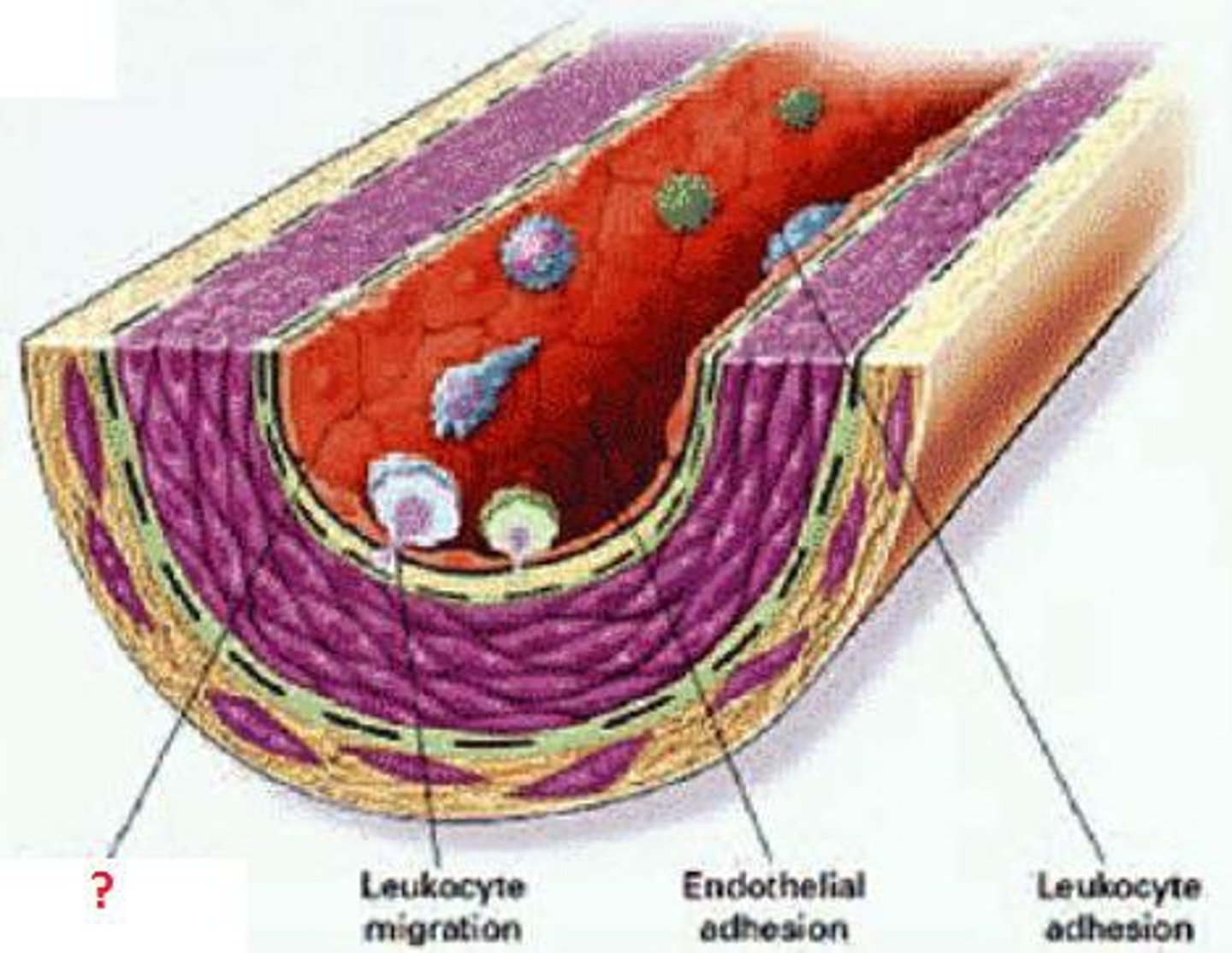
Macrophages
Phagocytic cells that engulf debris and pathogens.
Mast cells
Cells that initiate inflammation.
Areolar connective tissue
Loose CT; supports, binds, holds fluids, defends against infection.