Endocrine disorders - adenohyophysis, neurohypophysis, thyroid gland
1/5
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
6 Terms
Partial hyperpituitarism
Partial hyperpituitarism = overproduction of some pituitary hormones, usually due to pituitary adenomas (benign tumors of the pituitary gland). Hormones often affected are GH, ACTH (adrenocorticotropic hormone) and prolactin
Partial hyperpituitarism → Excess secretion of growth hormone, ACTH and prolactin by adenomas
GH-secreting adenoma (common in cats)
→ before closure of epiphyseal growth plate (youngs) → stimulate excessive longitudinal bone growth → gigantism
→ after closure of epiphyseal plate (adults) → stimulate soft tissue and bone thickening, not lengthening → diabetes mellitus (due to insulin resistance) and acromegaly (enlarged jaw, paws, facial bones, organomegaly)
ACTH-secreting pituitary adenoma
→ stimulate adrenal gland → increase cortisol secretion → cushing´s syndrome
Prolactinoma
→ increased prolactin secretion → reproductive dysfunction
Diabetes insipidus, causes and mechanism of development
Diabetes insipidus = syndrome of polyuria and polydipsia resulting from inability to concentrate urine as a result of lack of vasopressin action. Most affected animals are dog, horse, and cat.
Causes:
· Diseases of the CNS (central diabetes insipidus) – total or partial
· Diseases of the kidney (nephrogenic diabetes insipidus)
· Increased metabolic clearance of vasopressin
Disorders of CNS include: accidental head trauma, intracranial tumor, post-intracranial surgery or idiopathic, inflammatory and parasitic lesions of CNS
Nephrogenic diabetes insipidus may be congenital or secondary to a variety renal and metabolic disorders including chronic renal failure, tubular necrosis, may be idiopathic or drug induced nephrogenic DI results from a sensitivity of the vasopressin receptor to L1, F and other salts.
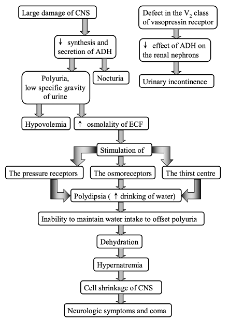
Mechanism of development of diabetes insipidus:
· Large damage of CNS → decreased synthesis and secretion of ADH (antidiuretic hormone) → nocturia and polyuria with low specific gravity of urine → hypovolemia and increased osmolarity of ECF
· Increased osmolarity of ECF → stimulation of pressure receptors, osmoreceptors and thirst center → polydipsia (increased water drinking) → inability to maintain water intake to offset polyuria → dehydration → hypernatremia → cell shrinkage of CNS → neurologic symptoms and coma
NB! Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is the opposite mechanism (too much ADH, inappropriate water retention, decreased blood Na levels)
Mechanism of development of Thyroid storm
Thyroid storm/thyroid crisis = exacerbation of hyperthyroidism, acute life-threatening hypermetabolic state, may be initial presentation of thyrotoxicosis.
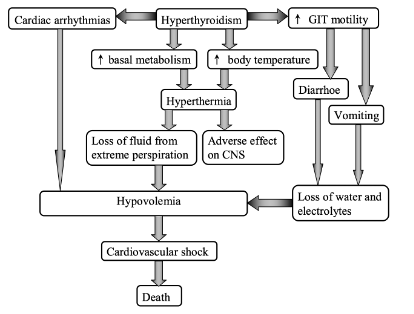
Mechanism of development:
· Hyperthyroidism → increased basal metabolism and increased body temperature, increased GIT motility, cardiac arrhythmias
· Increased metabolic rate and temperature → hyperthermia → loss of fluid from extreme perspiration and adverse effects on CNS → hypovolemia → cardiovascular shock → death
· Cardiac arrhythmias → hypovolemia → cardiovascular shock → death
· Increased GIT motility → diarrhea, vomiting → loss of water and electrolytes → hypovolemia cardiovascular shok → death
Syndrome of inappropriate ADH secretion (SIADH)
Syndrome of inappropriate antidiuretic hormone secretion (SIADH) = when there is too much vasopressin (ADH) with inappropriate water retention and decreased blood Na levels.
Causes:
· Results from many different conditions and drugs
· May be produced by certain tumors such as lung cancer or may result from chronic lung diseases
· Medicines such as antidepressants, antianxiety agents, seizure meds etc.
SIADH compared to diabetes insipidus: low urinary output, high levels of ADH, hyponatremia, overhydrated, retains too much fluid, BOTH will present with excessive thirst
Thyroid hypofunction and consequences
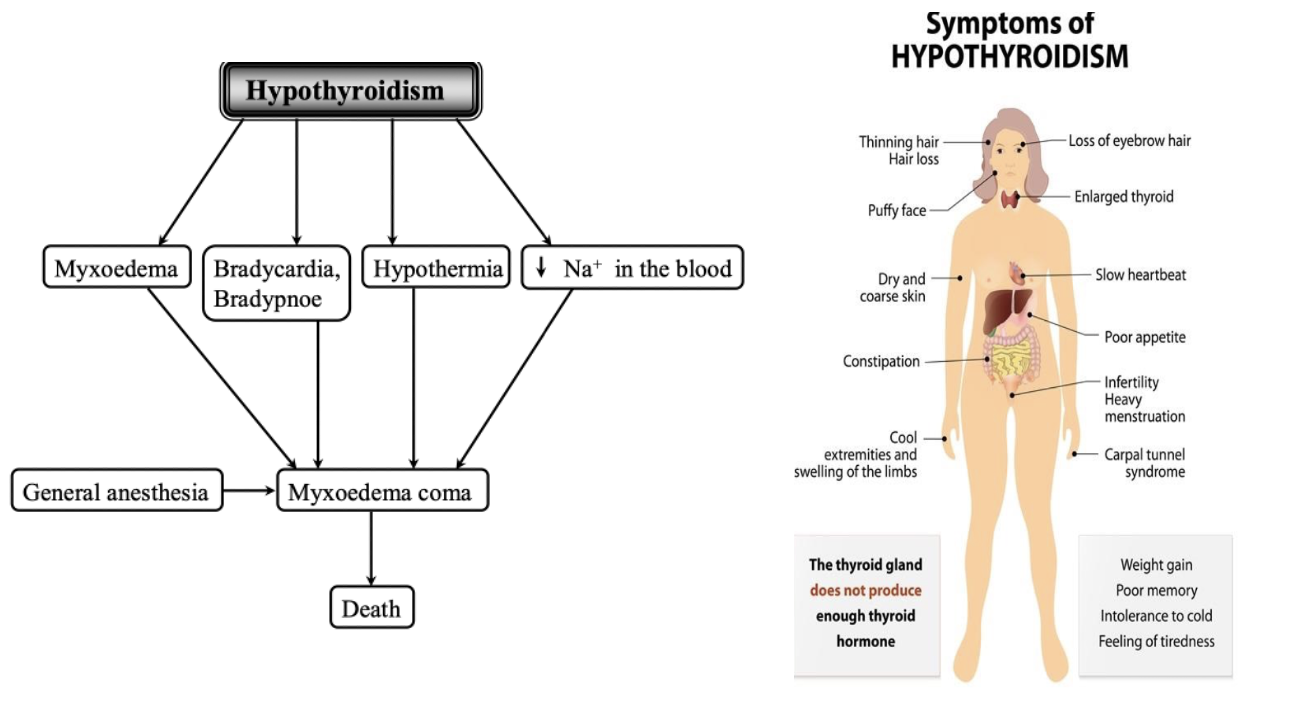
Thyroid hypofunction, also known as hypothyroidism, is a condition where the thyroid gland does not produce enough thyroid hormones, leading to slow metabolism and various systemic effects such as weight gain, fatigue, cold intolerance, and developmental issues in young animals.
Thyroid hypofunction (hypothyroidism) = a condition in which thyroid hormone secretion is inadequate to maintain normal levels of target tissue stimulation. Can be primary, secondary, and tertiary.
· Primary hypothyroidism caused by: Goitrogens, Iodine deficiency, Thyroid neoplasia, Lymphocytic thyroiditis, idiopathic atrophy of thyroid gland, absence of enzymes involved in the thyroidal hormones, thyroid agenesis, or dysharmonogenesis ( congenital hypothyroidism)
· Secondary hypothyroidism caused by: tumors, congenital pituitary malformations, a sequelae of the treatment of pituitary tumors with surgery, isolated TSH deficiency ( pituitary destruction)
· Tertiary hypothyroidism caused by hypothalamic dysfunction
Physiological consequences of hypothyroidism:
Calorigenesis and thermoregulation: decreased basal metabolic rate and O2 consumption lethargy, weakness, hypothermia, cold intolerance
Growth and maturation: mental retardation in youngs and dullness in adults
Carbohydrate metabolism: decreased glycogenolysis and glycolysis weight gain without increase in food intake
Protein metabolism: decreased synthesis, and increased degradation of protein weakness, poor hair coat, alopecia, hyperkeratosis
Cardiovascular system: bradycardia, low blood pressure and pulse
Neuromuscular system: muscle atrophy
GIT: constipation
skin: dry cool, yellow orange color
immunity: suppression of humoral and cellular immunity
hematologic alterations: normocytic, normochromic anemia, von Willebrand disease
respiratory system: bradypnoe
endocrine system: decreased GH secretion
reproductive system: decreased function
lipid metabolism: hypercholesterolemia
Goiter = thyroid gland enlargement resulting from prolonged stimualtion by TSH in hypothyroidism or in hyperthyroidism (TSH in pituitary adenoma)
Goitrogens = factors that block thyroid hormone synthesis either in food or in medication
Thyroid hyperfunction and consequences
Hyperthyroidism (thyrotoxicosis) = disorder resulting from excessive circulating concentration of T4 and or T3. It is common endocrine disorder in cat, but is rare in dogs.
· Primary hyperthyroidism caused by thyroid hyperplasia, thyroid adenoma, toxic multinodual goiter
· Secondary hyperthyroidism caused by TSH-secreting pituitary adenomas increased TSH secretion increased T4, T4 secretion by thyroid gland
· Tertiary hyperthyroidism caused by hypothalamic diseases with excessive TRH secretion increased TSH secretion by pituitary increased secretion of T4 and T3 by thyroid gland. Can also be caused by incorrect dosage in hypothyroid therapy iatrogenic hyperthyroidism
Physiological consequences of hyperthyroidism:
· Calorigeneis and thermoregulation: increased basal metabolic rate and O2 consumption. Hyperthermia, heat intolerance
· Growth, maturation: bone resorption, hypercalcemia, hypercalcinuria, fracture of bones
· Metabolism: progressive weight loss accompanied by polyphagia, vitamin deficiency
· Cardiovascular system: supraventricular tachycardia, increased pulse pressure, cardiac output and heart rate
· Nervous system: hyperactivity, restlessness, pacing or irritability of affected animals
· GIT: vomiting, diarrhea, frecuency of defecation and increased volume, malabsorption
· Skin: warm, sweaty
· Hematologic alterations: relative polycythaemia
· Respiratory system: tachypnoea
· Reproductive system: decreased fertility in females and altered steroid hormone metabolism in males
· Excretory system: increased Na+ excretion with water by kidneys, hypovolemia