mens health
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
Benign prostate hyperplasia
Patients with enlarged prostate
Majority of men above 50 years old and the frequency of the disease is increased with age
BPH is dependent on the androgen 5-alpha dihydrotestosterone (5α-DHT)
Testosterone secreted by the testicles and the adrenal glands, is quickly metabolized into DHT by the enzyme 5α-reductase at the prostate gland
Can become malignant -> good to treat early
Characterized by a non-malignant growth of some components of the prostate (e.g. transitional zone)
Progressive condition: Lower urinary tract signs and symptoms (LUTS), Negative impact on Quality of Life (QoL)
BPH - physiology of prostate
Composed of:
Epithelial (glandular) tissue → androgens stimulate its growth
Stromal (smooth muscle) tissue → innervated by α1 adrenergic receptors
Testosterone is converted to dihydrotestosterone (DHT) by enzyme called Type II 5α-reductase, in the prostate
DHT is needed for normal growth/enlargement of prostate
BPH - physiology
Physiology: tone of the human prostate smooth muscle is maintained primarily by noradrenaline released from adrenergic nerves and stimulating post-junctional α1-adrenoceptors.
Prostate and lower urinary tract tissues exhibit a high proportion of α1A receptors.
This provides the rationale for the use of α1- adrenoceptor antagonists for lower urinary tract symptoms associated with BPH
Activation of adrenoceptors leads to a contraction of the internal sphincter of the bladder, stops urine flow
Outcome of blockage: relaxes smooth muscle of bladder and urethra to improve urine flow
BPH - pathophysiology
Etiology is not well known => Likely age & hormonal factors
Static component (slowly over time) -> Hormonal Factors (Testosterone → DHT) -> enlargement of prostate tissue
Dynamic component -> increased smooth muscle tissue & agonism of a1 receptors -> narrowing of urethra outlet
Both lead to Urethral Obstruction / Signs & Symptoms
Long term - bladder response to obstruction
In the early phases, the bladder muscle can force urine through the narrowed urethra by contracting more forcefully
Over time, the bladder muscle gradually becomes thicker (hypertrophy) to overcome the obstruction
Once the detrusor muscle has achieved the highest state of hypertrophy, the muscle decompensates
Detrusor muscle becomes irritable and/or overly sensitive (detrusor overactivity or instability), contracting abnormally in response to small amounts of urine in the bladder, resulting in a need to urinate frequently
BPH - signs and symptoms
Many patients remain asymptomatic -> s/s start to occur in 1/3 men older than 65 yo. Symptoms only when detrusor decompensates
Lower urinary tract symptoms (LUTS): Weak stream, frequency, nocturia, intermittent stream, incomplete emptying, straining, and urgency
LUTS is not specific to BPH, many other causes: Urinary tract infections (UTIs), prostate or bladder cancer, diabetes mellitus
Obstructive/ Voiding Symptoms -> Early in disease course: Hesitancy, Weak stream, Sensation of incomplete emptying, Dribbling, Straining, Intermittent flow
Irritative/ Storage Symptoms -> Occurs after several years of untreated BPH: Dysuria, Frequency, Nocturia, Urgency, Urinary Incontinence (UI)
BPH - assessment
Digital Rectal Exam (DRE)
Ultrasonography
Maximum Urinary Flow Fate (Qmax)
Postvoid Residual (PVR): < 100 ml normal, > 200 ml inadequate emptying
Prostate specific antigen (PSA)
Might be elevated in BPH and positively correlated with prostate volume
Can help predict progression of BPH (> than 1.5 ng/mL)
Higher risk for prostate cancer
Controversial – not clear cut
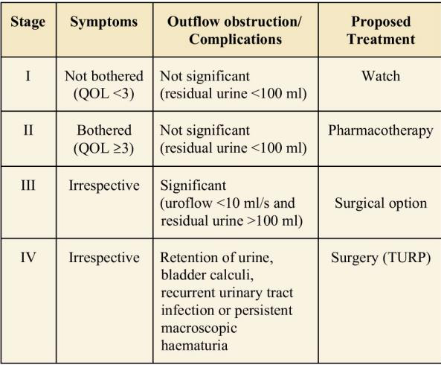
BPH - MOH guidelines
BPH - medication history
Anticholinergics -> decrease bladder muscle contractibility
Antihistamines, tricyclic antidepressants (TCAs), etc
α1 adrenergic agonist -> contraction of prostate smooth muscles
Decongestants
Opioid Analgesics -> increase urinary retention
Diuretics -> increase urinary frequency
Testosterone -> can stimulate prostate growth
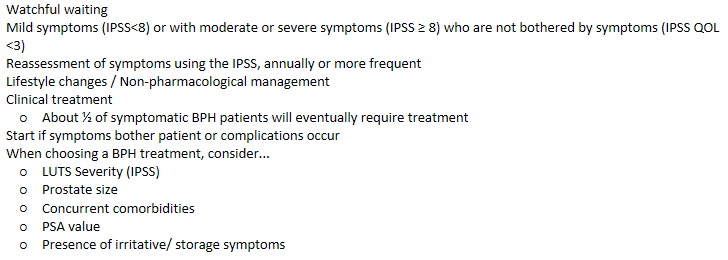
BPH - management
BPH - non-pharm management
Limit fluid intake in evening
Minimize caffeine and alcohol intake
Educate pt to take time to empty bladder completely and often
Avoid medications that can exacerbate symptoms
BPH - Current treatment guidelines
The goal of treatment is to relieve LUTS* and slow the clinical progression of BPH while improving patient QOL.
The 2010 updated treatment guideline from the AUA recommends that if the patient presents with LUTS, with or without uncomplicated prostate enlargement, and the symptoms are not affecting his QOL, then no further evaluation or treatment is recommended
LUTs: Obstructive symptoms (include urine hesitancy, straining, weak flow, prolonged voiding, partial or complete urinary retention, and urinary incontinence), and Irritative symptoms (include urinary frequency, urgency, nocturia, dysuria, and decreased void volume)
PSA = prognostic factor, but its not a 100% confirmation
Current oral pharmacotherapy options for managing BPH
(1) alpha-adrenergic antagonists (α-blockers),
(2) 5α-reductase inhibitors (5ARIs),
(3) muscarinic receptor antagonists (MRAs), and
(4) phosphodiesterase 5 (PDE5) inhibitors
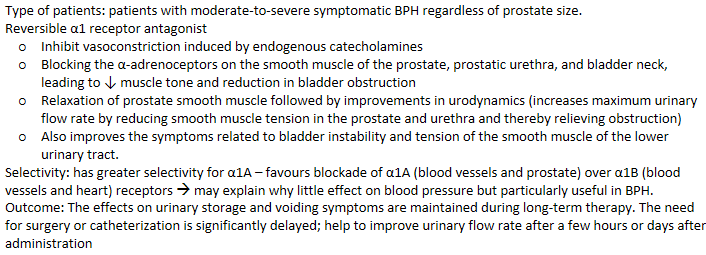
BPH - selective Alpha Adrenergic Antagonist (tamsulosin)
BPH - tamsulosin safety consideration
A: well absorbed orally (0.4mg once a day)
D: highly bound to plasma proteins (>90%) small V d (0.2L/kg)
M: metabolized by CYPs (eg. CYP3A4, CYP2D6). T1/2 ~10 - 15h
E: ~10% excreted unchanged in urine
Adverse effect: abnormal ejaculation, back pain
Contraindication: Concurrent use of another α1-adrenoceptor antagonist (eg. Prazosin – non-selective α1 blocker)
BPH - NS Alpha Adrenergic Antagonist
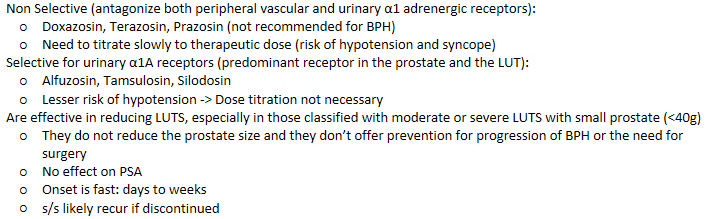
BPH - Alpha Adrenergic Antagonist AE
General side effects: muscle weakness, fatigue, ejaculatory disturbance, headache, etc
Bedtime administration to decrease orthostatic effects
Non selective: Dizziness (most common), first dose syncope and orthostatic hypotension
Uroselective:
Low to none peripheral vascular dilatation → less hypotension or syncope
Ejaculatory Disturbance (delayed or retrograde ejaculation) Silodosin > Tamsulosin > Alfuzosin
Still related with less sexual dysfunction than 5ARI
BPH - Alpha Adrenergic Antagonist - Intraoperative Floppy Iris Syndrome (IFIS)
Condition that complicates cataract surgery
MOA linked to blockage of α1 receptors in iris dilator muscle
Most commonly associated with tamsulosin
Men with planned cataract surgery should avoid the initiation until the surgery has been completed (or hold at least 14 days before surgery)
BPH - Alpha Adrenergic Antagonist selection
Non selective agents-
Could be beneficial in those hypertensive patients that need additional blood pressure (BP) lowering effect
In BEERs List as drugs to avoid in Should not be used as monotherapy for a patient that has HTN and BPH concurrently
Selective agents may be used in patients that don’t need added BP lowering effect
BPH - 5 alpha reductase inhibitors (5ARIs)
MOA: Competitive inhibitors of 5α-reductase (Type II). Inhibit conversion of testosterone to dihydrotestosterone (DHT), which drives prostate growth and male-pattern hair loss
↓ DHT levels, ↓ prostate size, ↑ hair growth. Improve urine flow and reduce acute urinary retention
Lower need for prostate surgery (e.g., transurethral resection, prostatectomy)
Do not bind to androgen receptors
For moderate to severe lower urinary tract symptoms (LUTS) with large prostates (>40g)
Suitable for patients wanting to avoid surgery or unable to tolerate α1-antagonist side effects
Slow onset: effects take 6–12 months
Decreases serum prostate-specific antigen (PSA) levels; consider if PSA >1.5 ng/mL
BPH - 5ARIs safety consideration
A: well absorbed orally (5mg once a day) F ~ 0.65. No dosage readjustment needed for patients with renal insufficiency, liver failure and elderly patients
D: high plasma protein bound (~90%)
M: metabolized by liver (eg. CYP3A4) T 1/2 ~6h
E: 50% unchanged drug excreted in feces; metabolites excreted in urine & feces
Contraindications: Women and children, pregnancy
BPH - 5ARIs AE
Ejaculatory disorders (reduced semen during ejaculation or delayed ejaculation) -> higher risk than alpha antagonist
Decreased Libido (3 - 8%)
Erectile Dysfunction (ED) (3-16%)
Gynecomastia and breast tenderness (1.0%)
Lesser risk of hypotension
BPH - 5ARIs considerations
Pregnant/ child bearing age females should NOT handle these agents
Obtain PSA before initiating therapy -> not easily interpretable after initiation
BPH - Phosphodiesterase 5 Inhibitor (PDE5I)
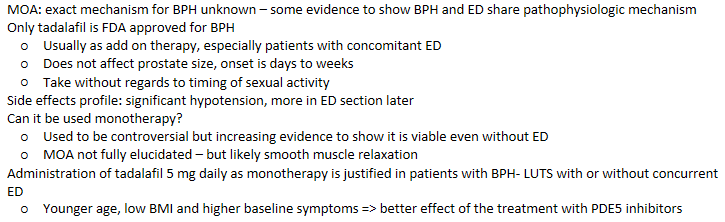
BPH - combi therapy
MTOPS & CombAT study – both support that combination therapy provided benefits beyond monotherapy
MTOPS - finasteride + doxazosin
CombAT - dutasteride + tamsulosin
Provide empiric evidence that long-term use of this combination is safe with only mild adverse effects
Individuals with moderate symptoms (e.g., IPSS 8–19, IPSS QOL 5-6) and prostate size > 25 g are most likely to benefit from an initial treatment that encompasses two drugs
BPH combi - a1 antagonist + 5ARI
Most common combination: α-blockers typically provide benefit within weeks, whereas 5-ARIs require months for optimal effect
Reserved for symptomatic patients with an enlarged prostate
SMART-1 trial: after 6 months of combination therapy, discontinuation of the α-blocker can be considered in moderate BPH
BPH combi - 5ARI + PDE5 inhibitor
Beneficial to mitigate the sexual adverse effects that may arise from 5-ARIs / Concomitant erectile dysfunction
However, individuals with BPH & ED often have cardiac comorbidities
If unstable angina, should not be initiated on a PDE5 inhibitor as contraindicated with concomitant use of nitrates
BPH combi - a1 antagonist + PDE5 inhibitor
Rarely used initial combination therapy: can cause severe life threatening hypotension
If used, recommend to choose uro-selective α1 instead
Must optimize/stabilize α1 antagonist dose first before adding PDE5i
Use lowest effective PDE5 inhibitor dose possible
Would not address enlargement of the prostate
BPH - anti-muscarinics
Add on for those patients who present irritative voiding symptoms, which mimic overactive bladder (OAB)
MOA: Block muscarinic receptors in detrusor muscle→ decreasing involuntary contraction of the bladder
Agents: oxybutynin, tolterodine, solifenacin, trospium, darifenacin, fesoterodine
PVR must be less than 250 ml (or 150 ml for more conservative guidelines)
Historically, anticholinergics were considered contraindicated in BPH because of concern for urinary retention
A meta-analysis of seven controlled trials showed minimal risk
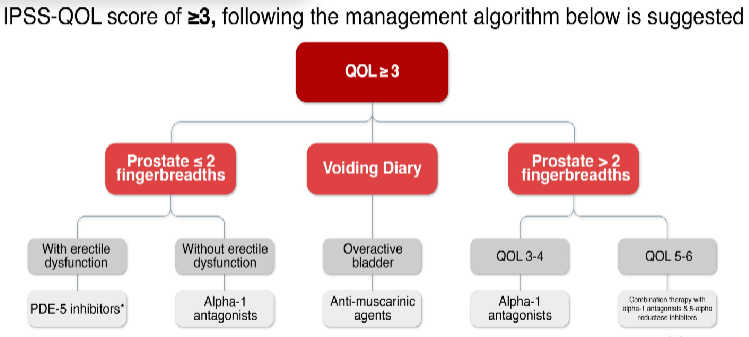
BPH - treatment pathway
BPH - conclusion
Lifestyle changes are recommended at any stage for a person with LUTS secondary to BPH
Watchful waiting should be consider for patient with mild symptoms, who are not bothered by LUTS
Pharmacotherapy is considered as an alternative for moderate to severe symptoms, which are bothersome
Surgery is indicated when complications of BPH are present
erectile dysfunction
Inability to achieve or maintain an erection of sufficient duration and firmness to complete satisfactory intercourse
Can get an erection sometimes, but not every time sex is desired or Can get an erection, but it does not last long enough for fulfilling or satisfactory sex or Are unable to get an erection at any time
Low in men < 40y/o, increases as age increases. Estimated that around 50% of men 40 y/o and older experience ED
Highly correlated with CV disease, DM, HTN, hyperlipidemia, obesity, smoking, alcoholism, BPH, depression
Usually if symptoms for > 6 months is ED
ED - physiology of erection
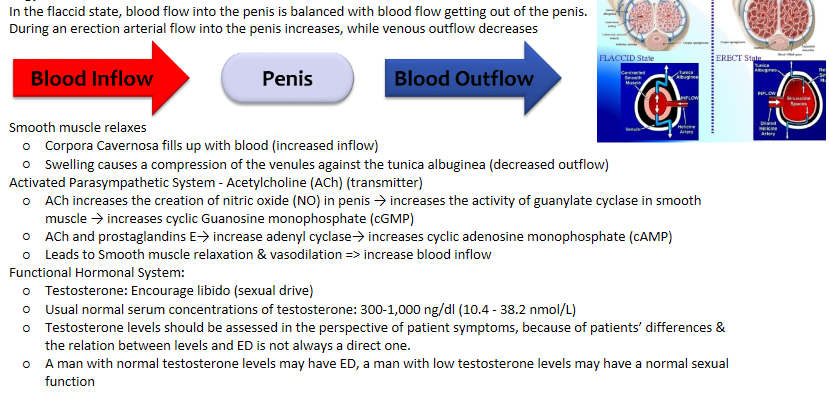
ED - physiology of detumescence
Deactivating of Parasympathetic System
cGMP is deactivated by an enzyme called phosphodiesterase type 5 (PDE-5) => stops the vasodilation
PDE-5 is the predominant enzyme found in penis
Activated Sympathetic System
Induces smooth muscle contraction via α2 adrenergic receptors of arterioles resulting in a reduction of blood flow
Serotonin has been postulated to have inhibitory effects on sexual arousal
ED - etiology
Organic ED: Vascular, nervous, or hormonal systems compromised, Medication Induced
Psychogenic ED: Due to thoughts or feelings (psychological reasons) rather than physical pathology
Mixed ED: Combination of both: Organic and Psychogenic ED
Others:
Social habits: smoking, excessive ethanol intake, and illicit drug use
Obesity
organic ED - causes
Vascular: Arteriosclerosis, Peripheral vascular disease(PVD), HTN, Diabetes
Hormonal
Hypogonadism - not enough testosterone
Hyper-prolactinemia - too much prolactin -> inhibits testosterone
Nervous
Central: Spinal cord trauma or disorders, Stroke, CNS Tumors
Peripheral: Diabetes, Neuropathy, Urethral surgery
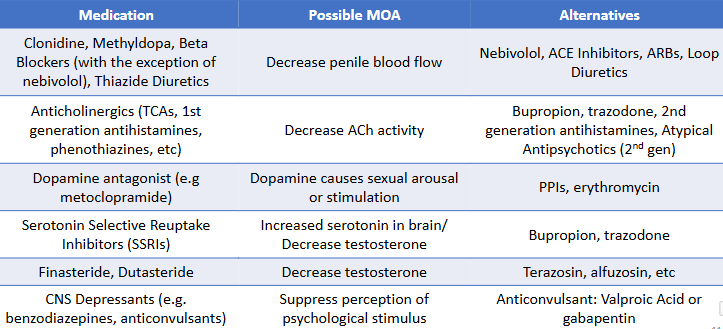
organic ED - medication induced
psychogenic ED - causes
Malaise
Loss of attraction
Stress
Performance anxiety
Mental Disorders
Sedation
ED - signs and symptoms / complications
Loss of interest in sexual activities
Depression
Performance anxiety
Embarrassment
Angry
Low self-esteem
Disharmony in a relationship
ED - evaluation
Signs/symptoms
Sexual Health Inventory for Men (SHIM)
Mild to no ED: 17 to 21 points
Moderate to Severe: <11 points
Workup to identify underlying causes of ED
Medical history / Medications
Social history
Surgical history
Lab results -> blood glucose, lipid profile, testosterone, among others
ED - CVD evaluation
Cardiovascular (CV) evaluation should be conducted, in all patients with ED:
ED might be an early symptom of unidentified comorbid CVD
Sexual activity -> sympathetic activation may increase BP and heart rate (HR) → increasing the risk of myocardial infarction (MI)
Low risk of CV: okay
If unknown/ not low risk: Exercise stress testing to evaluate exercise capacity
If unstable or severe symptomatic CVD: defer until condition stabilized
Cardiac rehabilitation and regular exercise useful to reduce the risk of CV complications with sexual activity
ED - non-pharm management
First step is to recognize and, if possible, reverse or treat the underlying cause(s)
Non-pharmacological:
Addressing modifiable risk factors: Stop smoking, Control weight, Control glucose / BP / lipids, Exercise, Decrease alcohol
Psychotherapy
Devices: Vacuum erection devices (VEDs)
Surgery eg penile implant
ED - pharm management
Phosphodiesterase Type 5 Inhibitors (PDE-5 Inhibitors)
Testosterone replacement
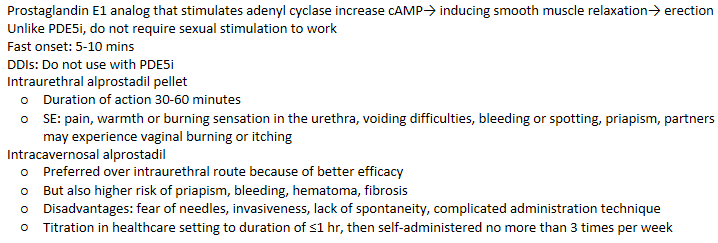
Alprostadil (Prostaglandin E1 analog)
Yohimbine (Derivative of African yohimbine tree, α-2 Antagonist. Efficacy controversial; not recommended according to HSA)
ED - PDE-5 inhibitors
MOA: Inhibit PDE 5 enzyme which induces catabolism of cGMP → enhancing cGMP activity →inducing smooth muscle relaxation→ erection
Considered as first line agents
Cause and enhance erection only after sexual stimulation
Failure rates is approximately 30 to 40% -> similar among the agents
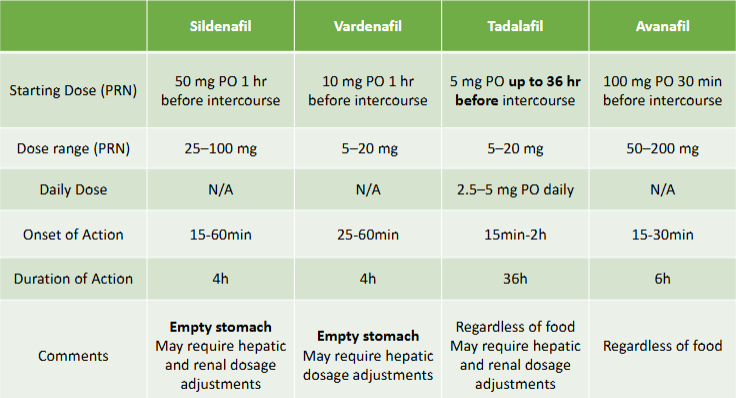
ED - PDE-5 inhibitors dose
A lower initial dose for:
Patients ≥ 65y/o
Those taking alpha blockers
Patients with renal failure
Taking CYP3A4 Inhibitors (e.g. erythromycin, cimetidine, ketoconazole, itraconazole, clarithromycin, grapefruit or grapefruit juice, ritonavir, saquinavir, among others), as they may increase the serum concentrations of PDE5 Inhibitors
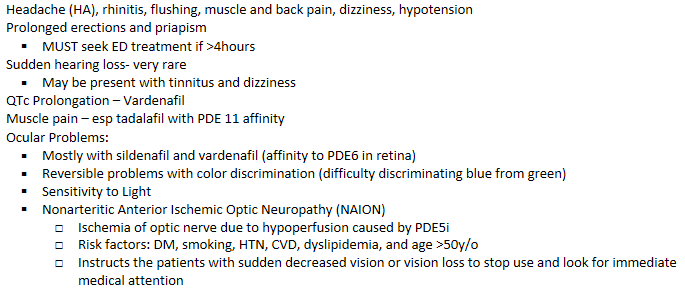
ED - PDE-5 inhibitors AE
ED - PDE-5 inhibitors DDI
Contraindication: Nitrates + PDE5 Inhibitors = potentially fatal hypotension
Nitrates should be avoided for 12 hrs after avanafil, 24 hrs after sildenafil or vardenafil, and 48hrs after tadalafil
Risk of hypotension increases with use of multiple antihypertensives
PDE5 Inhibitors + Alcohol = hypotension
CYP3A4 Inhibitors + PDE5 Inhibitors (3A4 substrates) = ↑ Concentration of PDE5 Inhibitors
ED - PDE-5 inhibitors monitoring
Efficacy:
If failure reported; Administration with food? Timing and frequency of dosing. Lack of adequate sexual stimulation. Titration to maximum dose
If all modifiable factors are addressed, may be treated with a different PDE5 inhibitor or proceed with other more invasive therapy
Safety: BP, Side effects, Drug interactions
Changes in cardiac health status
ED - testosterone replacement
Restore serum testosterone levels to normal range (300–1100 ng/dL; 10.4– 38.2 nmol/L)
Indicated for symptomatic hypogonadism as confirmed by (1) decreased libido and (2) low serum testosterone concentrations
SE: irritability, aggressive behaviour, undesirable hair growth, increased BP, hepatotoxicity, dyslipidemia, polycythemia, prostatic hyperplasia (CI for prostate CA)
Dosage forms: IM injection, buccal, patches, topical gel, body spray, nasal spray & PO
Monitor serum testosterone within 1–3 months and at 6- to 12-month intervals -> discontinue if no improvement after 3 months
ED - Alprostadil
ED - conclusion
ED is defined as failure to achieve and/or maintain a penile erection appropriate for sexual intercourse
Evaluation of a patient with ED requires identifying organic and/or psychological causes & CVD workup
PDE5 Inhibitors are consider as first line agents for ED
Have similar efficacy profile, but have different onset and duration of action, and side effect profile
Pain and priapism may occur with alprostadil, and should be avoided in those at risk of priapism
Testosterone indicated as first line agent for those patients with ED and symptomatic hypogonadism