7. LO5: Prevention of Cross Contamination
1/102
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
103 Terms
Q: What concepts must be differentiated and defined regarding infection control practices?
Universal precautions and routine practices
Q: What is the purpose of a total office infection control program?
To prevent or reduce the spread of disease
Q: Name the six pathways for cross-contamination in the dental setting.
Patient to dental team
dental team to patient
patient to patient
dental office to community (including the dental team’s families)
community to patient
dental team to family
Q: What are the three factors required for infectious disease to develop?
Virulence, Dose, and Resistance
Q: What is the primary goal of infection control concerning the three factors for disease development?
To reduce the dose of microorganisms that may be shared between individuals or between individuals and contaminated surfaces
(the more dose reduction, the less the chance of disease spread)
Q: Who provides infection control recommendations?
The CDC (Centers for Disease Control) and Health Canada
Q: Which organization regulates the practice of dentists in Ontario under the Regulated Health Professions Act, 1991 (RHPA)?
The Royal College of Dental Surgeons of Ontario (RCDSO)
Q: Which college regulates dental hygienists in Ontario?
The regulatory college for the dental hygienists in Ontario (CDHO)
What are the colleges responsible for regulating? (RHPA)
Practice of dental professionals under provincial legislation (RHPA - regulated health professions act)
Q: What is the concept that Routine Practices are based upon?
That all patients are potentially infective
Q: How is occupational health and safety regulated in Canada?
It is regulated in each of the 14 jurisdictions (provincial, territorial, and federal)
Q: What are the five principles inherent in routine practices?
1) Risk Assessment
2) Hand hygiene
3) Use of PPE
4) Environmental controls
5) Administrative controls
Q: Define Universal Precautions.
The concept that all human blood and certain body fluids that may contain blood are treated as if known to be infectious for HIV and HBV and other blood borne pathogens
Q: According to CDC guidelines, what must an Infection Control Program include?
A written program
Q: What testing is required for all dental office personnel according to CDC guidelines?
Testing for antibody hep B surface antigen
Q: What type of infection control precautions are required by CDC guidelines?
Standard precautions [routine practices]
Q: What PPE should be included according to CDC guidelines, besides proper hand hygiene?
Clean eyewear and face shields (with proper cleaning)
Q: Where should a central instrument processing area be designated?
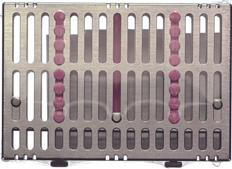
Into receiving, cleaning, decontamination, preparation, packaging, sterilization, and storage
Q: What type of equipment is included in the central instrument processing area?
Automated equipment (ultrasonic). Should use barriers and puncture-resistant gloves
Q: What type of instruments must be packaged and heat sterilized according to CDC guidelines, and what must be used during this process?
Critical/semi-critical instruments, using chemical indicators and sterilization monitors
Q: What standard of water quality must be used for dental care in dental unit water lines?
Water that meets the Environmental Protection Agency (EPA) drinking standard (500 CFU/mL)
Q: What flushing procedure is required for handpieces, A/W syringes, and ultrasonic scalers between clients?
Flushing with water and air for 30 seconds after use and prior to removal from water lines between clients
Q: What instruction is given regarding patients and low volume dental handpieces?
Do not advise patients to close their lips around low volume handpieces
Q: What measures are required for dental radiology to prevent cross-contamination?
Use of heat tolerant/disposable film-holding devices, including use of barriers and proper disinfection of digital sensors
As per CDC guidelines, what is stated about the dental laboratory?
Wearing PPE and proper decontamination
Optimal use of vaccines ++
Q: Why are tetanus endospores challenging for infection control?
They are present continually in the environment and are resistant to disinfection efforts
Q: Which infectious complication is associated with a cut/puncture wound caused by Clostridium tetani (proliferation in anaerobic environment)?
Tetanus ("lock jaw")
Q: How often are tetanus boosters recommended after the first two inoculations?
Every 10 years
Q: Which vaccine-preventable disease is one of the most frequently reported in North America?
Hepatitis B
Q: Which two types of influenza viruses are mentioned?
Influenza type A or B
Q: How often does the CDC advise all healthcare workers to be vaccinated against influenza?
Yearly
Q: Why can the influenza vaccine not be administered to all individuals?
It is grown in eggs and cannot be given to those with hypersensitivity to eggs
Q: Name three important vaccines often missing for dental professionals.
HepC, HIV, tuberculosis, and some forms of human herpesviruses
Q: What are three purposes of using Personal Protective Equipment (PPE)?
To protect the operator, reduce direct contact, minimize indirect transmission, minimize exposure to spatter, or minimize exposure to aerosols
Q: What is the Bacterial Filtration Efficiency standard for a standard mask?
It blocks particles greater than 3µm with 95% filtration
Q: How should a protective mask be removed?
By the loops
Q: How should protective eyewear be removed?
By the ear rests
Q: Name one factor that affects the integrity of gloves.
Length of time worn (approx. 1 hour), procedures that perforate them, packaging, poor fit, storage, alcohol, rings, or washing of gloves
Q: Why should patient care gloves never be washed with detergents or chemicals?
It will weaken them and enhance penetration/wicking
Q: What material are latex gloves derived from?
Hevea brasiliensis (rubber tree)
Q: Name the three types of reactions that occur to latex gloves in an increasing level of severity.
Irritant contact dermatitis, Allergic contact dermatitis, and Latex allergy
Q: Name two common dental/medical products that contain latex.
Gloves, masks, prophy cups, rubber dams, blood pressure cuffs, carpule stoppers, ortho rubber bands, or impression materials
Q: Name a group considered high risk for latex sensitivity.
Healthcare workers (HCW 8-12%), individuals with multiple medical surgeries, or those with food allergies (avocado, banana, kiwi, chestnut, papaya)
Q: Define instrument processing and why it must be performed carefully.
A collection of procedures to prepare contaminated instruments for reuse
important to:
– To ensure that disease agents are not transferred
– To keep instrument damage to a minimum
Q: Name one design consideration for the instrument processing area.
It should be as far away as possible from the dental chairs.
Store sterile packages, trays, and cassettes in closed cabinets or drawers;
Do not process instruments or handle sterile packages during client care
Q: What is the recommended workflow pattern for instrument processing?
A U-shaped workflow pattern in a room with a single door
Q: What are the three main areas of activity that must be separated in the instrument processing area to prevent cross-contamination?
Decontamination area, Preparation and Packaging area, and Sterilizing and storage area
Q: Before any cleaning procedure, what PPE must always be worn and what must be prevented?
Mask, gloves, protective eyewear, and clothing (gown)
handle contaminated instruments carefully to prevent cuts and punctures from sharp items
To transport instruments carefully, where should they ideally be placed in?
Ideally, they should be in closed cassettes and covered with the plastic lid.
Q: What characteristic often makes single-use devices unsuitable for reuse?
They are usually not heat-tolerant and cannot be reliably cleaned or disinfected
Q: List the seven steps to instrument processing.
Holding (presoaking)
Pre-cleaning
Corrosion control, drying, and lubrication
Packaging
Sterilization or high-level disinfection
Sterilization monitoring
Handling processed instruments
Q: What is the purpose of the Holding (presoaking) step?
To prevent drying of saliva and blood for contaminated instruments that cannot be cleaned right away
Q: Why is extended presoaking (more than a few hours) not recommended?
It may cause instruments to corrode
Q: What is "bioburden"?
A client’s microbes
Q: How do organic components in blood and saliva affect sterilization?
The fats and protein protect bioburden from sterilization agents
Q: How does pre-cleaning increase sterilization effectiveness?
It reduces bioburden
Q: Name the two types of cleaning systems approved by the FDA for safety and effectiveness.
Ultrasonic cleaning and Instrument washers or washer-disinfectors
Q: Why is manual scrubbing of instruments not recommended?
It is dangerous due to the risk of cuts and puncture during the procedure
Q: How does ultrasonic cleaning dislodge debris?
Ultrasonic energy produces millions of tiny bubbles in the cleaning solution that collapse and create high turbulence at the surface of the instruments
Q: What safety measure eliminates the need to scoop up instruments by hand at the end of the ultrasonic cycle?
The use of a cleaning basket or cassette rack
Q: What is the general range for ultrasonic cleaning time?
4-16 minutes
Q: Why do instruments in plastic/resin cassettes require longer ultrasonic cleaning times?
The plastic/resin absorbs some of the ultrasonic energy
Q: Why must instruments be thoroughly rinsed after ultrasonic cleaning?
Rinsing removes residual cleaning solution and reduces the bioburden
Q: Name one precaution that should be taken to prevent injury when handling contaminated, sharp instruments.
Using puncture-resistant utility gloves; Not reaching into trays or containers holding sharp instruments that cannot be seen; Using a long-handled brush if manually scrubbing; or Wearing a mask, protective-eyewear, and gown to protect from sprays, splashes and spatter
Q: Which instruments require lubrication after rinsing?
Hinged types instruments
Q: What is the primary purpose of instrument packaging?
Maintains the sterility and prevents contamination after sterilization during storage or distribution to chairside
Q: List two required items that must be labeled on each package before sterilization.
Date processed, sterilizer used, cycle or load number, or initials of the OHCW who packaged the instruments
Q: Where must labels be placed on a plastic/paper pouch?
On the transparent side of the pouch
Q: What is required to be included inside all packages?
Both external and internal chemical indicators
Q: What is the term for sterilizing unwrapped instruments?
Flash sterilization
Q: What two reasons do NOT qualify for using flash sterilization?
Client scheduling and/or lack of instruments
Q: When should flash sterilization be used?
Only in urgent emergency situations where the instrument will be used immediately and no other options are available
Q: Name one requirement regarding the use of flash sterilization.
A log must be kept of all particulars when this method is used (i.e., client name, procedure, and instrument used); Instruments must be clean and dry prior to sterilization; Every cycle must be monitored; or Care must be taken to prevent contamination of instruments prior to use
Q: Define a Microbicidal agent.
Is one that kills microbes ("cide" or "cidal" refers to "killing")
Q: Define Bactericidal.
Kills bacteria (but not necessarily endospores of bacteria)
Q: Define Asepsis.
The absence of pathogens on living tissues
Q: Define Sterilization.
A process intended to kill all microorganisms; the highest level of microbial kill that can be achieved
Q: Define Disinfection.
A less lethal process than sterilization; intended to kill disease-producing microorganisms but not bacterial endospores. Usually refers to the use of liquid chemicals to kill microorganisms at room temperature on surfaces
Q: What are chemicals used to disinfect inanimate objects called?
Disinfectants
Q: What are solutions used to disinfect the skin or other living tissues called?
Antiseptics
Q: Define Sanitization.
Reduces the microbial population to levels considered safe by public health standards, such as those applied to restaurants
Q: What is the standard challenge in sterilization?
Bacterial endospores
Q: Name the three common types of sterilizers used in dental offices.
Steam sterilization, Unsaturated chemical vapor sterilization, and Dry heat sterilization
Q: Which sterilization method is considered the "first method of choice"?
Steam Autoclave (moist heat under pressure)
Q: What is the action mechanism of steam sterilization?
Moist heat coagulates protein and pressure elevates the temperature
Q: What conditions are required for operating a steam autoclave at 121°C?
121°C at 15 pounds of pressure for 15 minutes
Q: Why must air be removed from the sterilizer chamber during steam sterilization?
So steam can reach all instrument surfaces
Q: What is one advantage of steam sterilization?
Quick and easy to use; Allows loads to be packaged; Penetrates fabric and paper wrappings; Very reliable; or Can be monitored for effectiveness
Q: What is one disadvantage of steam sterilization?
May cause rust or corrosion; May damage plastics; May dull sharp instruments; or May leave items still wet
Q: List the four steps of a typical dental office steam sterilizer operating cycle.
- Heat-up cycle (generates steam and removes air), 2. Sterilizing cycle (sterilization temp. held for set time), 3. Depressurization cycle (steam slowly released; items still wet), and 4. Drying cycle (dries packages)
Q: What is the action mechanism of dry heat sterilization?
Oxidation of cells parts, and heat conducted from the exterior surface to the interior object
Q: What is the standard temperature range and time for dry heat sterilization using sterilizing ovens?
160-170°C for 1-2 hours
Q: Name one advantage of dry heat sterilization.
Does not dull cutting edges; Does not rust or corrode (if items are dry); Easy to use with little maintenance; Very reliable; Items dry after cycle; or Least expensive form of sterilization
Q: Name one disadvantage of dry heat sterilization.
Usually requires a longer cycle; Damages some plastics; May discolor or char fabric; Poor penetration requires careful loading; High temperatures may prohibit use with some items and may melt or destroy some metal or solder joints; or instruments must be pre-dried
Q: What are the typical operation conditions for chemical vapor sterilization?
127-132°C with 20-40 pounds pressure for 20 minutes
Q: Why is adequate ventilation required for chemical vapor sterilization?
Due to fumes
Q: What items are chemical vapor sterilizers incompatible with?
Fabric packs, plastics, and rubber, or materials sensitive to chemicals, temperature, and pressure
Q: What type of items is liquid chemical sterilization good for?
Items sensitive to high heat temperatures (plastics and rubbers)
Q: Why is liquid chemical sterilization not considered the most reliable method?
It cannot be monitored by bacterial spore testing routinely, although it kills spores in a controlled lab setting