Calcium and Bone Disease: Pathology Final
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
Calcium
- Atomic weight of 4g/mol
- Divalent cation
- High in sea water
What form is calcium stored in in the bones
Tricalcium phosphate
Normal serum calcium
2.5 mmol/L
Lab testing for calcium
Normal total calcium is 2.5mmol/L, but only some of that is ionized and able to be biologically useful (1.2mmol/L)
Protein bound calcium
Not biologically available for membranes or bones, level not regulated
Serum calcium includes
Free calcium, protein bound calcium, and complex calcium (aka Ca citrate)
Why is calcium important in the body
- Stability of cell membranes
- Signaling
- Component in bone
- HIGHLY regulated in the body
Effect of high calcium in the cells
Causes phosphates in the cell membrane to stick together, the cell membrane is less fluid, less permeable, and less excitable
Effect of low calcium in cells
Less phosphates in the cell membrane sticking together leading to greater fluidity, permeability, and excitability
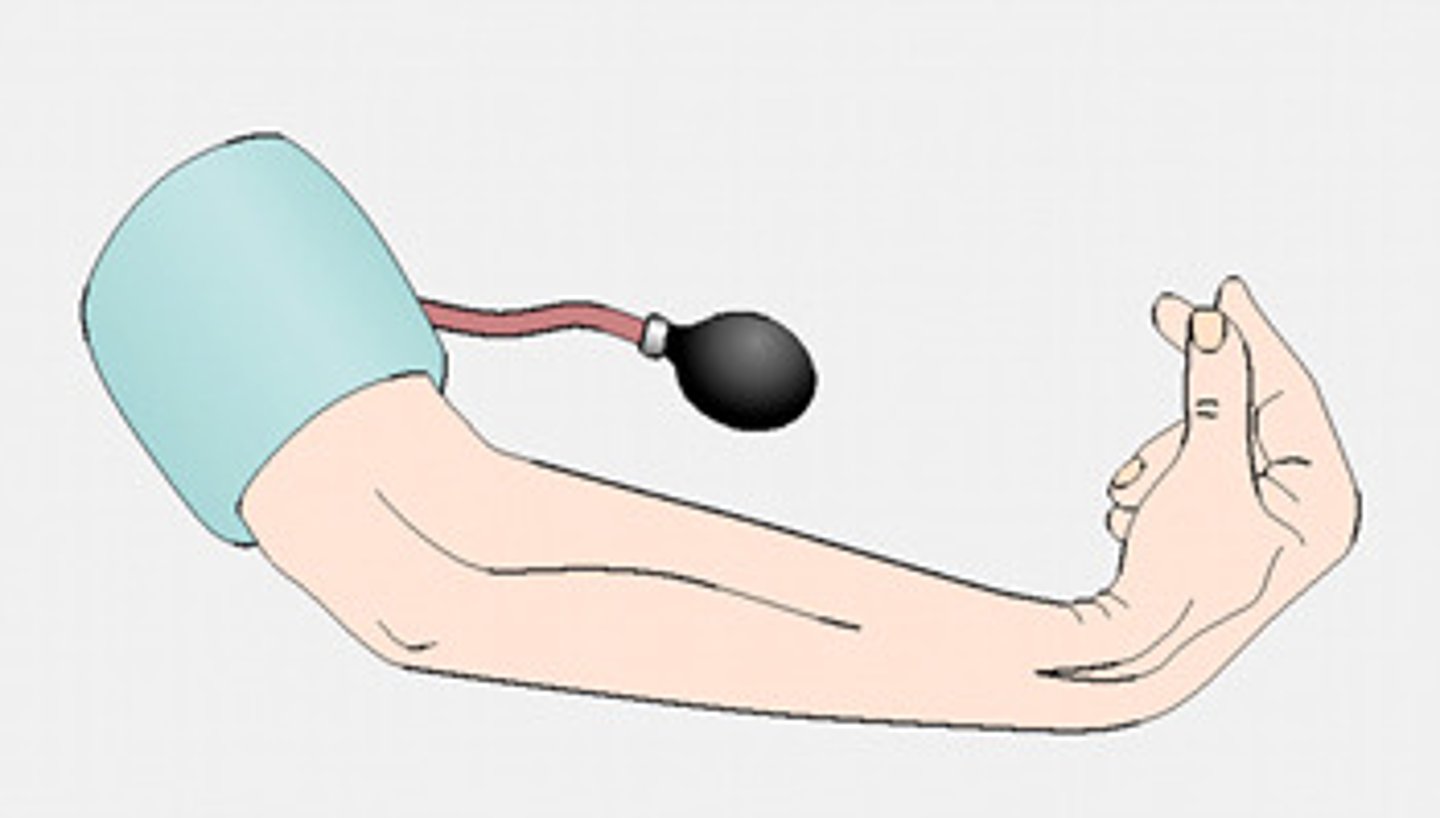
Physical tests that can be done to see low calcium
- Chovstek Sign
- Trousseau sign
Chovstrek sign
Rubbing the side of someone's face and seeing if they twitch, sign of low calcium
Trosseau sign
Hand cramping up, sign of low calcium
Primary purpose of bone
Calcium reservoir
Bone growth
- Bone is first a soft matrix
- Then gets vascularized
- Starts to calcify
- Growth happens from the epiphyseal plates (at the ends of bone, not mineralized)
Growth continues to happen until fusion of the epiphyseal growth plates
Fusion of epiphyseal growth plates
After puberty, you stop growing
Damage of an epiphyseal growth plate
Damage before fusion can lead to that limb not being able to grow properly
Average rate of increase in height (cm/year)
Height growing fast from birth, but then levels off, then increases again at a growth spurt at puberty, but then levels off again after puberty and you eventually lose height
Velocity of growth highest when you are younger and during puberty
Alkaline phosphatase
Marker of bone turnover, highest before the epiphyseal plate fusion but after that becomes lower unless a condition is causing abnormalities in ALP (ex. fractures, etc)
Bone remodelling
Process done by osteoblasts (build bone) and osteoclasts (break down bone)
Every month, we dissolve 1% of our skeleton and build back 0.9% of it, meaning each year we lose 1% of our skeleton
Bone formation lags behind bone absorption
Cortical bone
Dense part of bone that prevents bending
Trabecular bone
Less dense part of bone that prevents crushing
3 hormones that regulate ionized calcium in the body
- Active vitamin D3 (calcitriol)
- Parathyroid hormone
- Calcitonin
Action of parathyroid hormone
Activated when serum calcium is low.
Causes increased activity of osteoclasts which cause bone resorption, cause an increase in active vitamin D3, and causes increased renal absorption of calcium
Action of active vitamin D
Active when serum calcium is low
Cause increase intestinal absorption of calcium
Action of calcitonin
Active when serum calcium is high
Cause increase in bone formation
What happens when calcium is low and parathyroid hormone is low
Primary hypoparathyroidism
What happens when calcium is relatively normal but parathyroid is high
Kidney disease, which cannot make vitamin D to suppress PTH
What happens when calcium is very high but parathyroid hormone is low
Bone metastasis could be happening where the calcium in the bones is getting chewed away leading to very high serum calcium
What happens when calcium is high and parathyroid is high
Primary hyperparathyroid
What happens when you consume calcium (1000mg)
800mg goes out in the stool, 200mg is absorbed and is in equilibrium with bone before it is renally excereted
What happens when you consume calcium (less than the required amount) and do not have vitamin D
Body will use the calcium stores from the bone to normalize serum calcium, leading to low bone density
What happens when you consume calcium and vitamin D
Vitamin D enhances the absorption of calcium
Bone as a biomaterial
Self-engineered material that realigns based on the stress that is imposed on it, dynamic tissue
Z-scores for osteoporosis
Shows your value in comparison to people of the same age group
T-scores for osteoporosis
Compares your value with a person who has ideal bone density (under 35 years old)
Osteoporosis diagnosis
T score of less than -2.5
As people age, their bone density gets less but the reference for osteoporosis stays the same, meaning lots of people get diagnosed with osteoporosis as they get older
When you are over 70, what is a better predictor of life expectancy than blood pressure/cholesterol
Bone density
Survival with and without hip fracture
Survival rates decrease after a hip fracture for both men and women
Hip fractures as a predictor of life expectancy, vertebral or other fractures also decrease life expectancy but not as much as hip fractures
Risk factors for hip fractures
- Low BMD
- Low calcium/vitamin D intake
- Older adult
- Perceived health
- Low BMI
- Low exercise
Bone turnover lab testing
Expensive and not often done, little clinical importance
Osteoporosis treatment and compliance
Bisphosphonates are only working to increase BMD and decrease risk of fractures if people are actually filling and taking their medications as prescribed
No osteoporosis therapy is effective without _______________________
Calcium, vitamin D
All RTCs have been done in the presence of calcium and vitamin D as well as the drug
What effect would an antiresorptive drug (bisphosphonate) have on serum alkaline phosphatase
Lower
Calcium nutrition advice for patients
RDA around 1000mg/day, if you need to figure out how much calcium a patient can have you can use calcium calculators
If you are consuming _____mg of calcium per day there is no need for a supplement
800mg