lecture 10,11,12 cardiovascular system, cardiac function, arteries & arterioles
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
the goal of cardiovascular system
maintain adequate delivery of oxygen and nutrients and removal or wastes from all tissues in the body
also
monitor tissue integrity
avenue for signaling

know these:
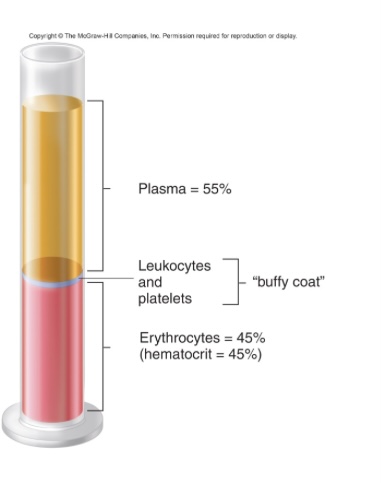
total blood volume = 5.5 L
hemocrit = 45%
hemoglobin = 15 g/dL per micro liter
red cell count = 5 million per micro liter
total white cell count = several thousand
plasma
mostly water; ions like interstitial fluid
gases, nutrients, wastes
hormones and messenger molecules
proteins 7% (4.5 albumin, 2.5 globulins, 0.3 fibrinogen)
plasma vs serum = absence of clotting factors
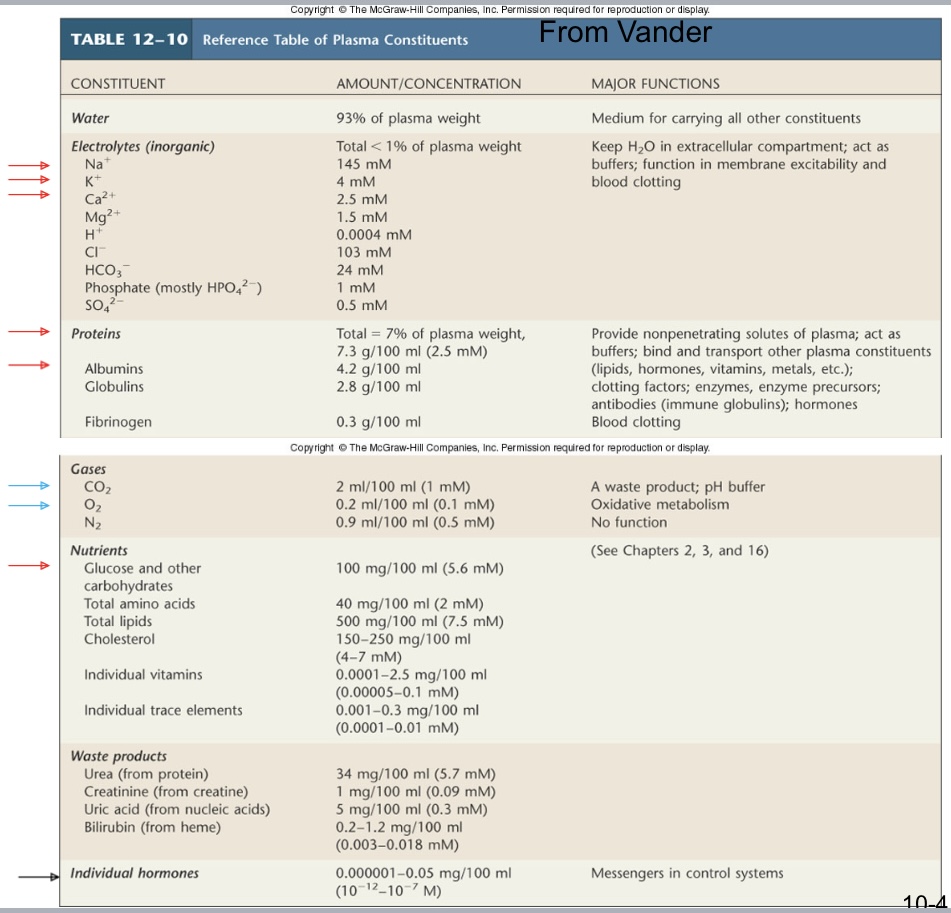
reference table for plasma constituents
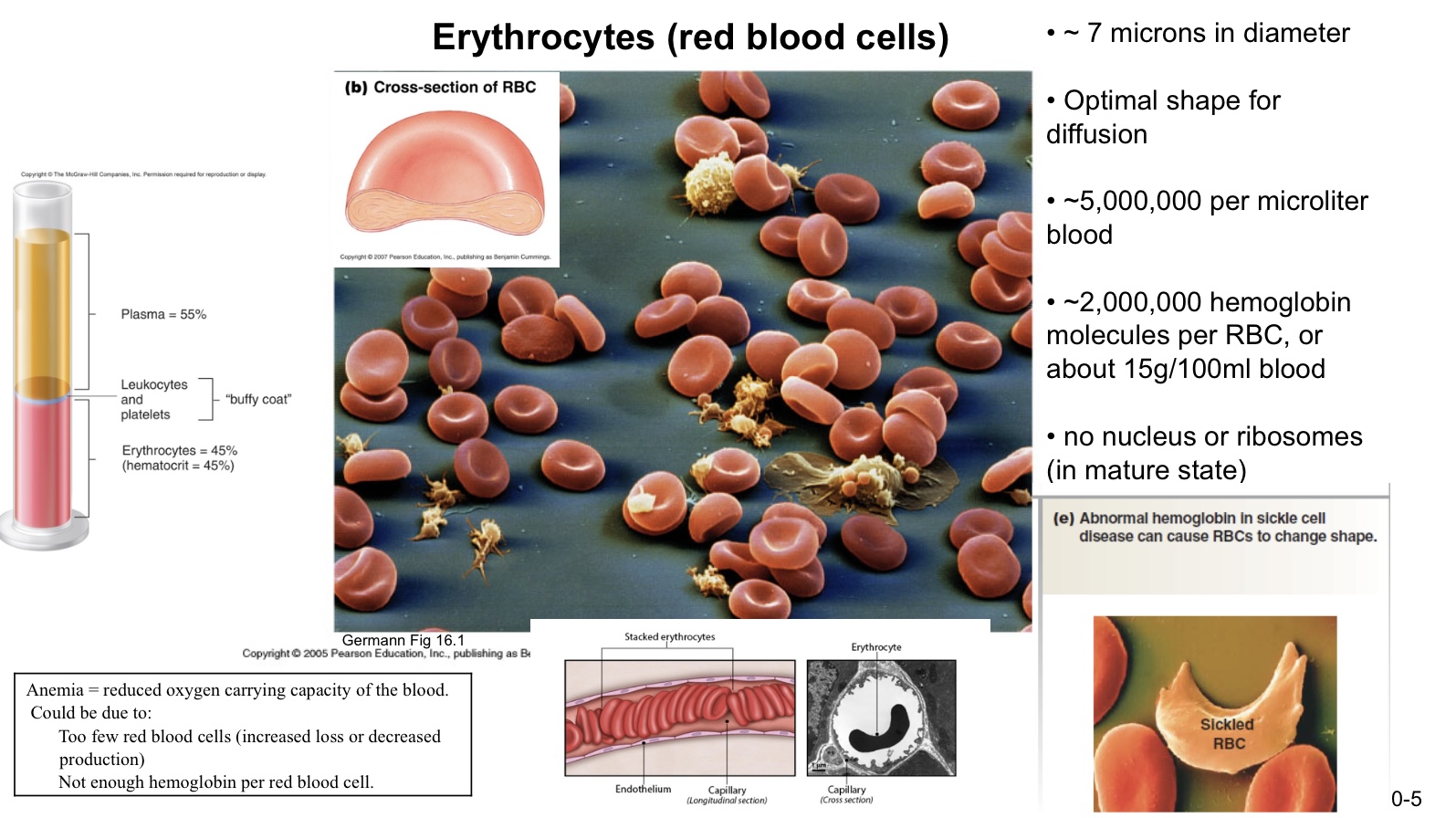
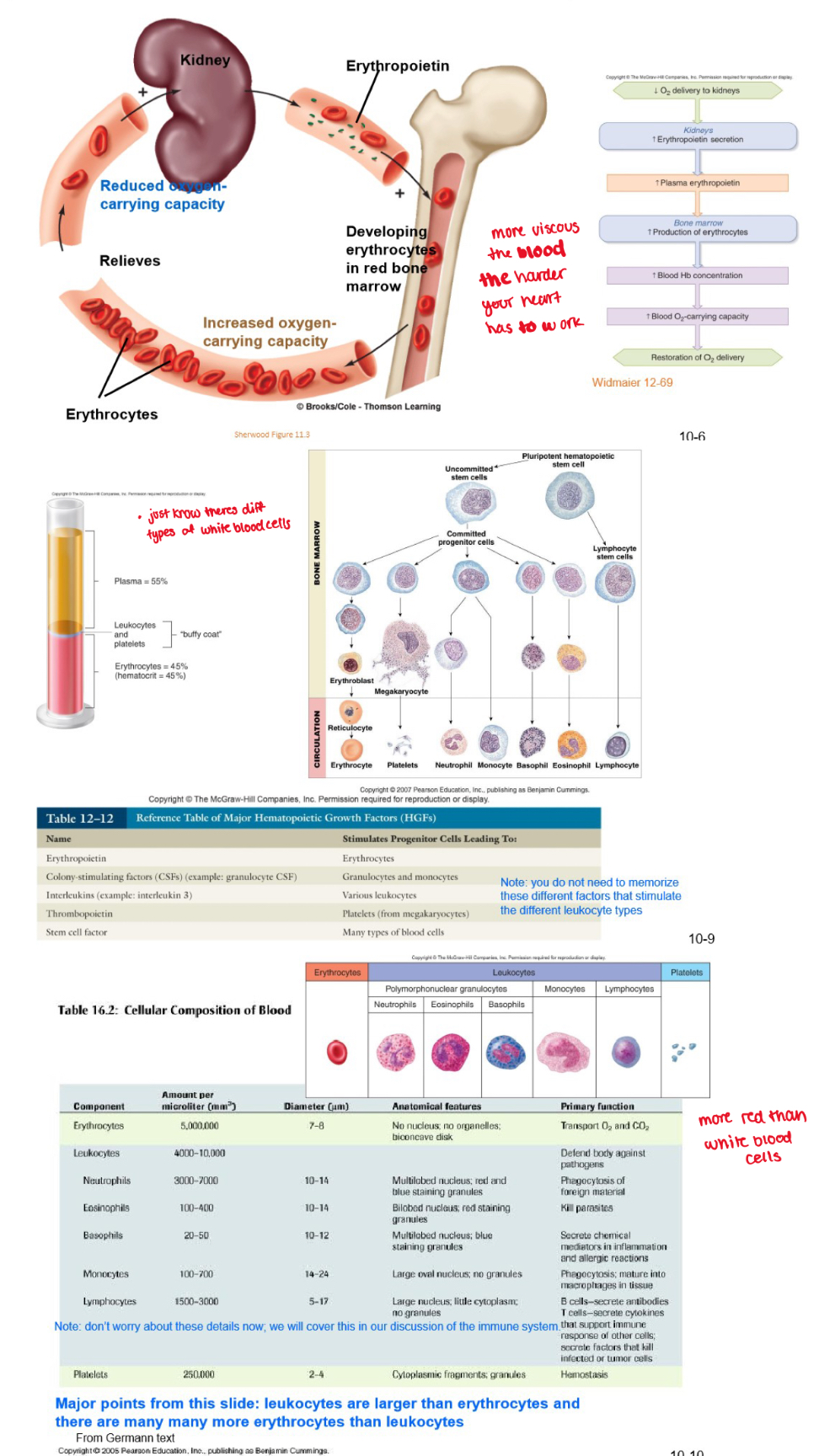
erythrocytes (red blood cells)
7 microns in diameter
optimal shape for diffusion
5 mill per micro liter blood
2 mill hemoglobin molecules per RBC, or about 15g/100mL blood
no nucleus or ribosomes (in mature state)
anemia = reduced oxygen carrying capacity of the blood
due to:
too few red blood cells
not enough hemoglobin per red blood cell
erythropoetin
a hormone released by the kidney, stimulated production of red blood cells
general organization of the cardiovascular system
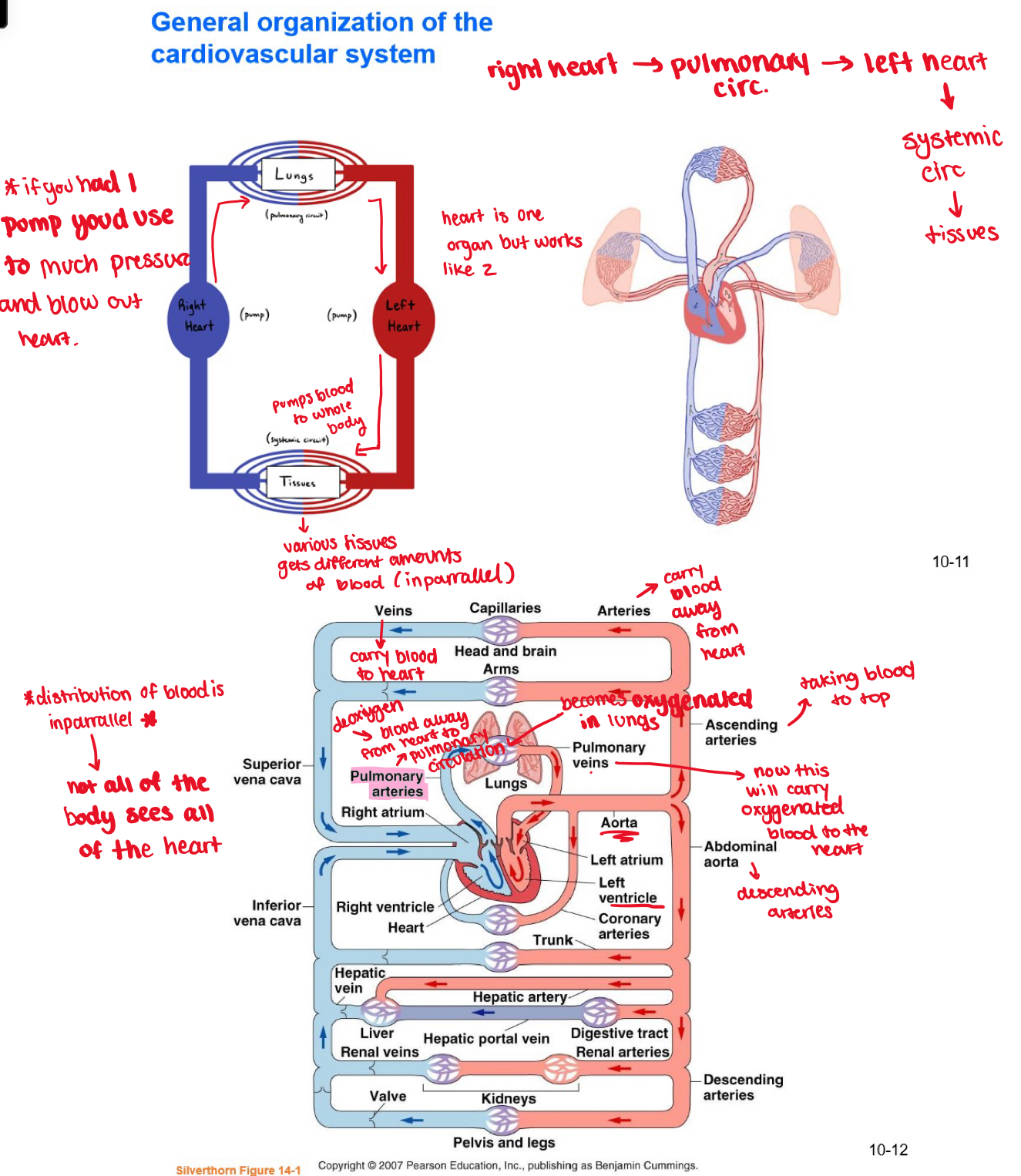
flow of blood
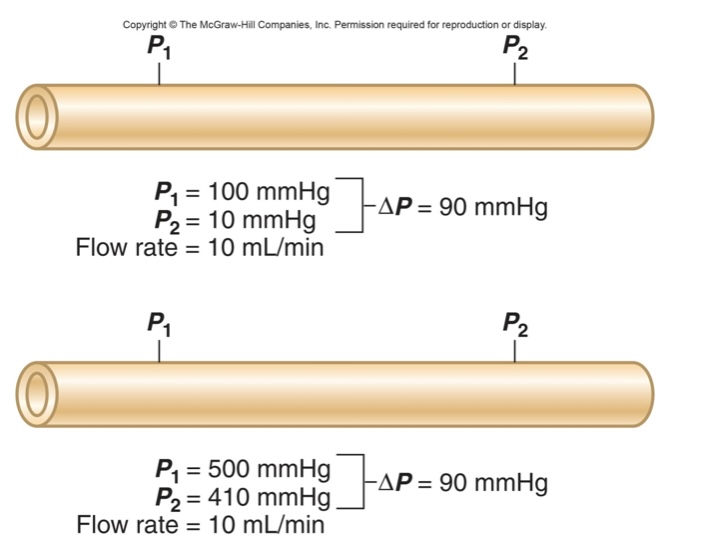
blood will only flow if there is a pressure gradients: blood will flow from higher pressure to lower pressure
consider the flow of blood through one of these vessels
flow is proportional to the pressure gradient
flow is inversely proportional to resistance
flow = ΔPressure/resistance
ΔPressure = flow x resistance
resistance = ΔPressure/flow
resistance to flow
viscosity is not changing much in body
length stays same in adult body
radius is adjustable and is how body regulates modifiable pressure
basic principles about flow:
blood flows if there is pressure gradient, from high → low pressure
flow is opposed by resistance
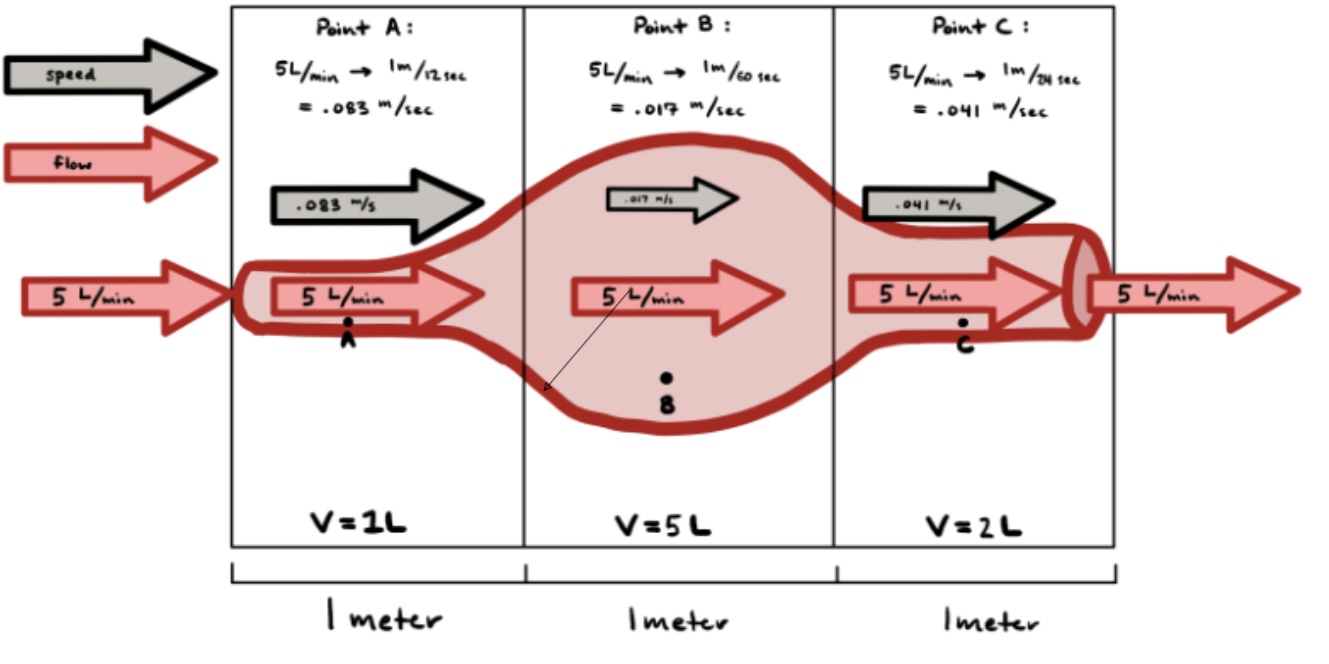
flow rate & velocity are different beings; flow rate (or simply flow) is the volume of blood passing a point in the circulation per unit time (i.e. ml/min) whereas velocity is the distance the blood travels per unit time (i.e. cm/min)
the larger the cross-sectional diameter of the vessel, the slower the velocity of flow
flow rate = volume of blood passing a point in a given amount of time
flow = volume per time
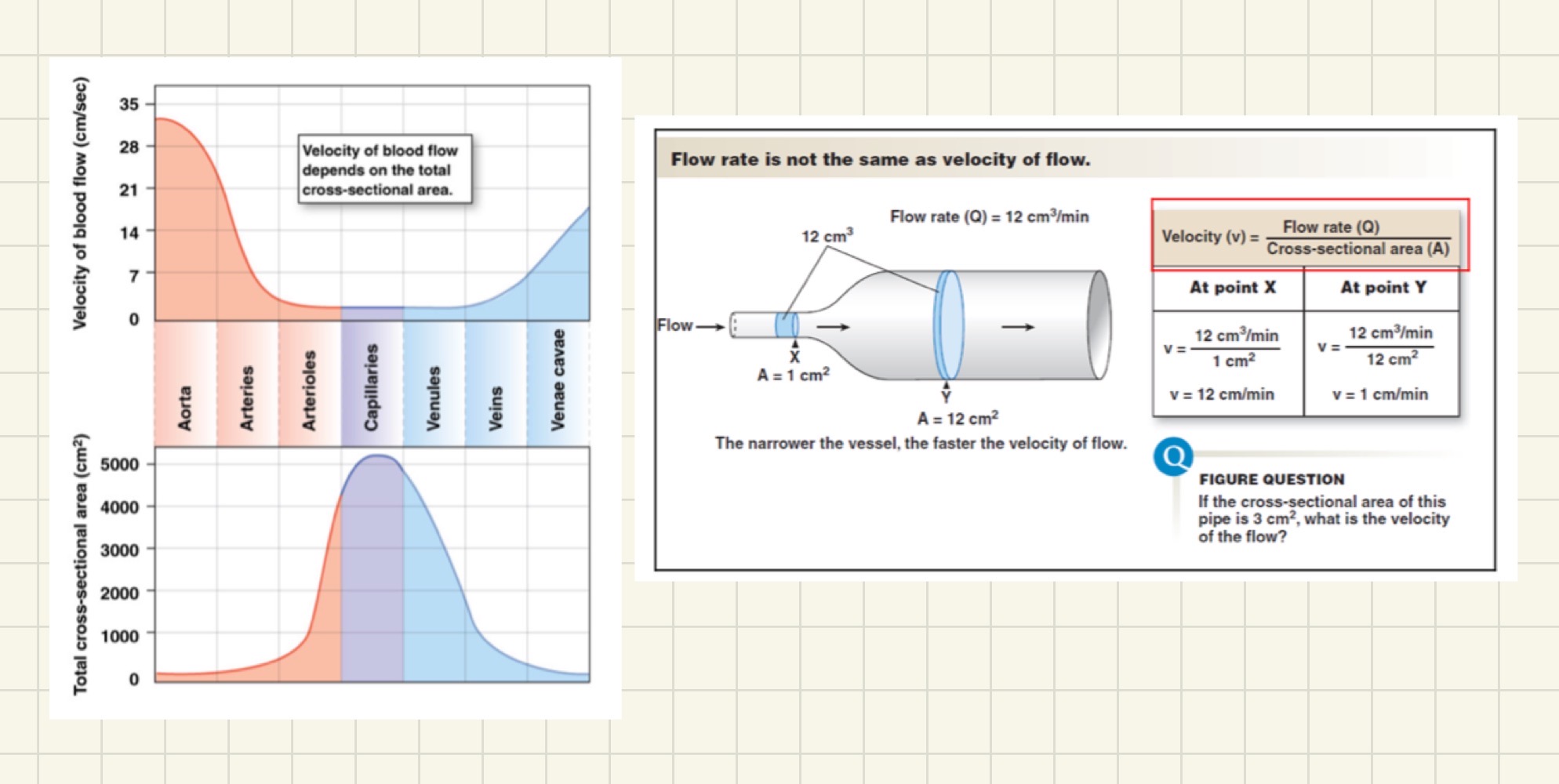
diagram about flow
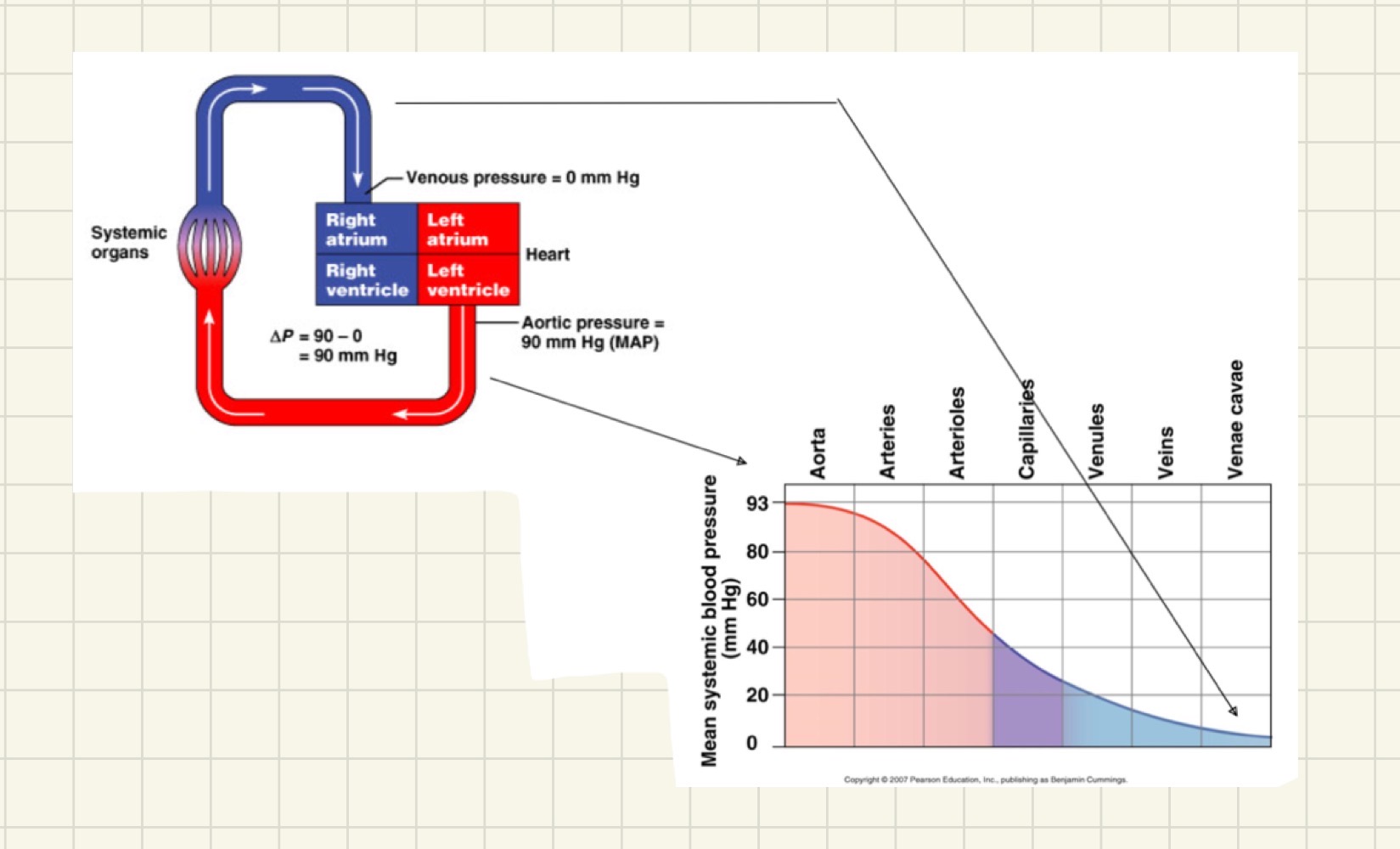
flow resistance causes a pressure drop
out of all these vessels the arterioles are providing the greatest amount in resistance
diagrams of heart, heart wall etc
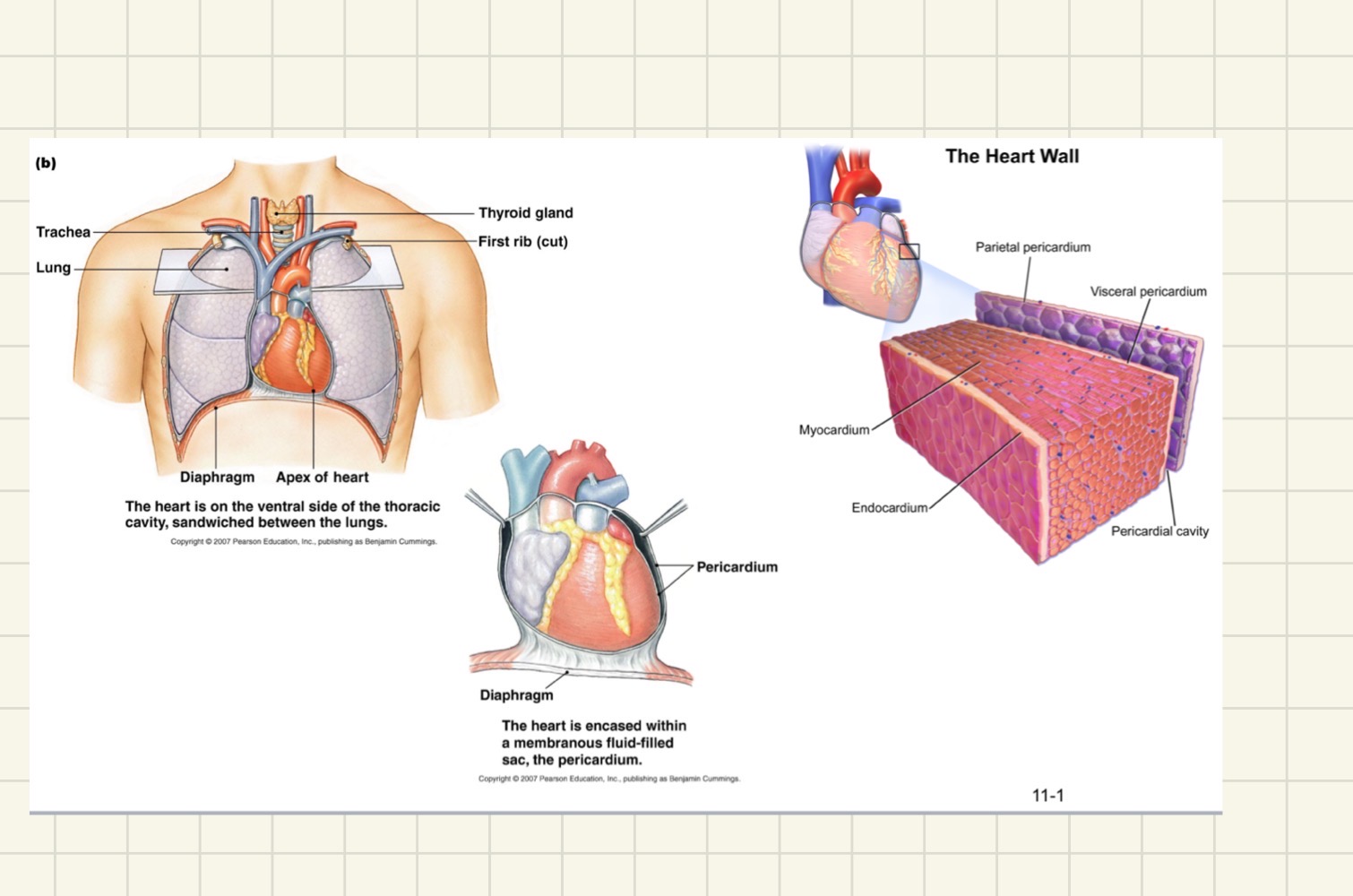
flow of blood in heart
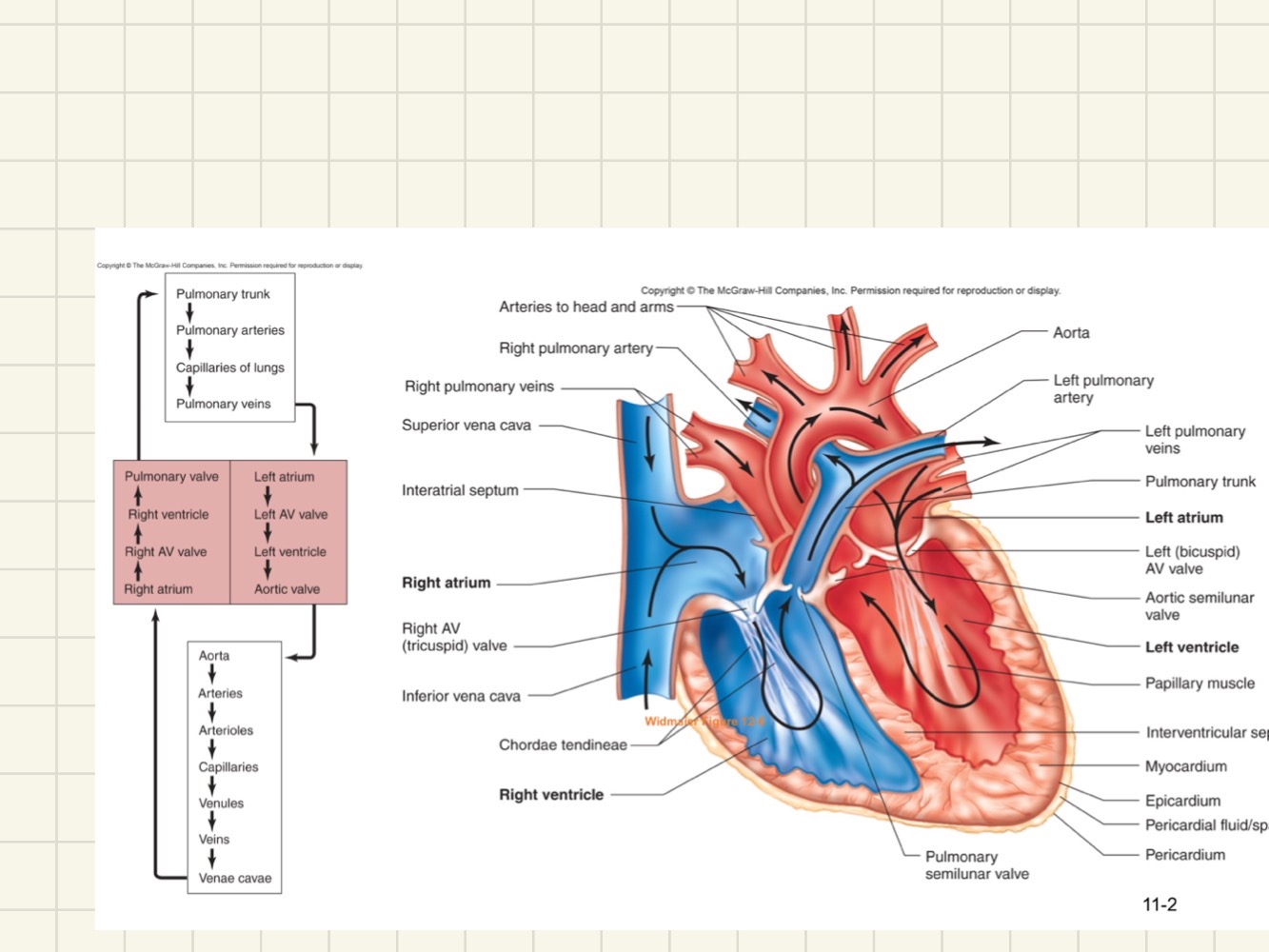
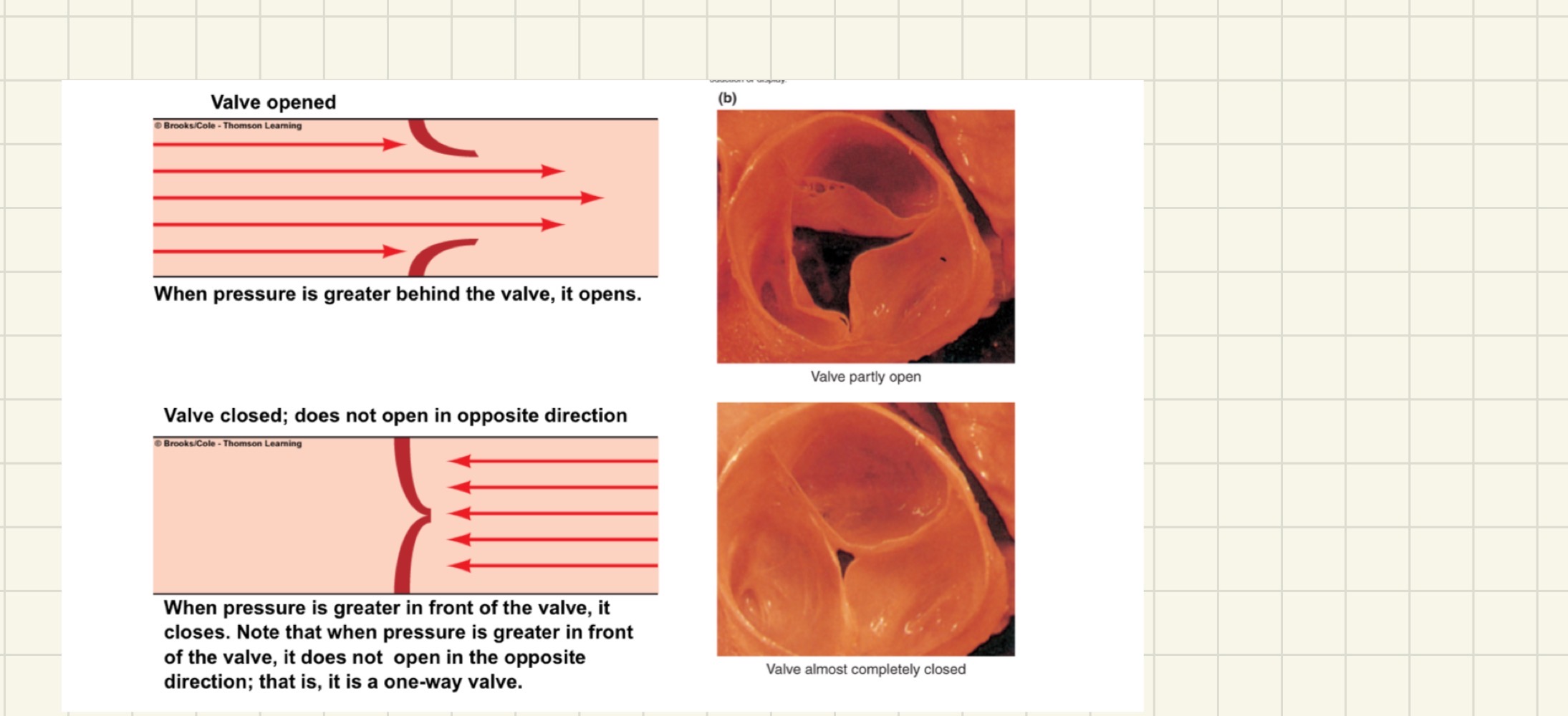
valve opened vs valve closed
valve opened:
when pressure is greater behind the valve (atrium) , it opens
valve closed:
when pressure is greater in front of the valve, it closes
Note that when pressure is greater in front of the valve, it doesn’t open in the opposite direction; its a one-way valve
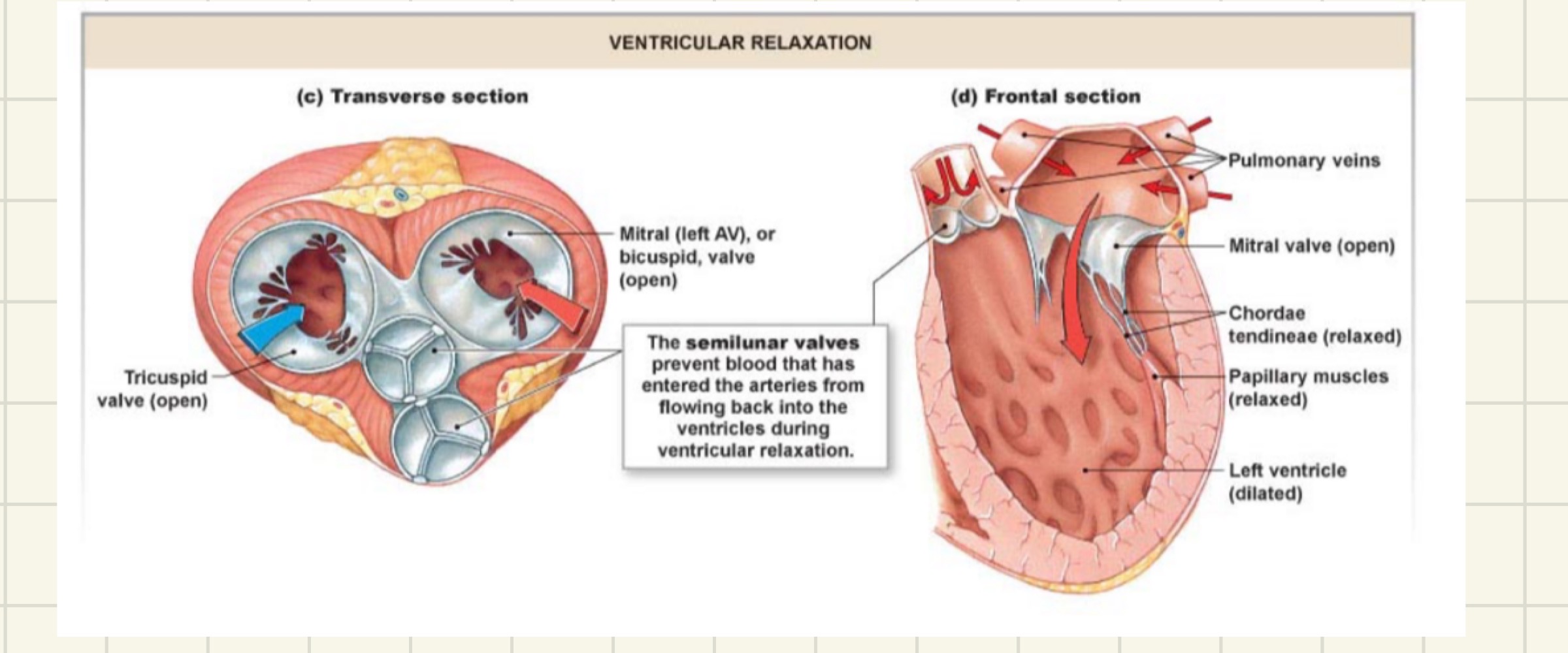
tricuspid and mitral (bicuspid) valves
prevents blood from flowing backwards from the ventricles into the atria during ventricular contraction
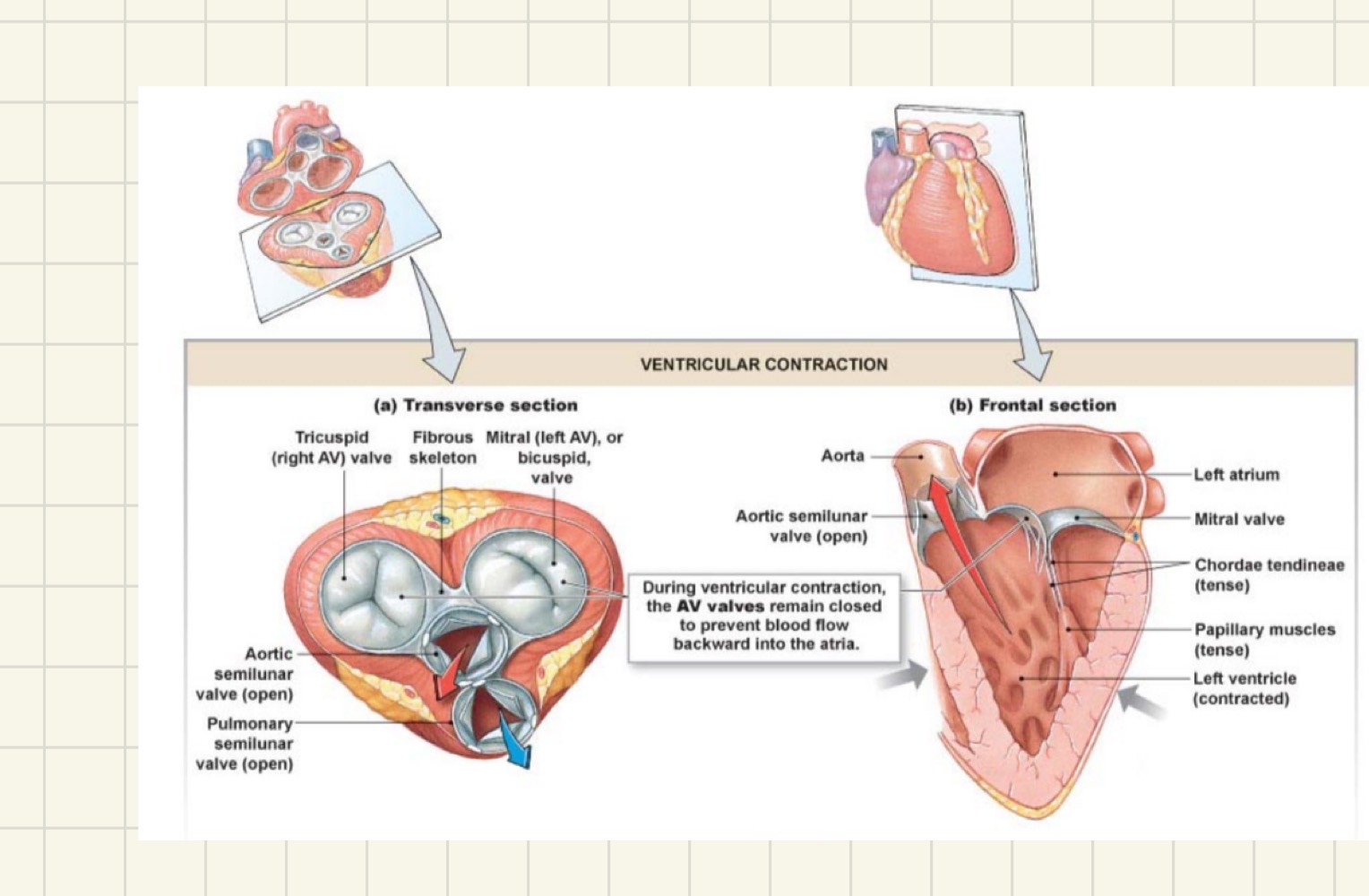
semilunar valves
prevents blood from flowing backwards from the aorta and pulmonary artery into the ventricles
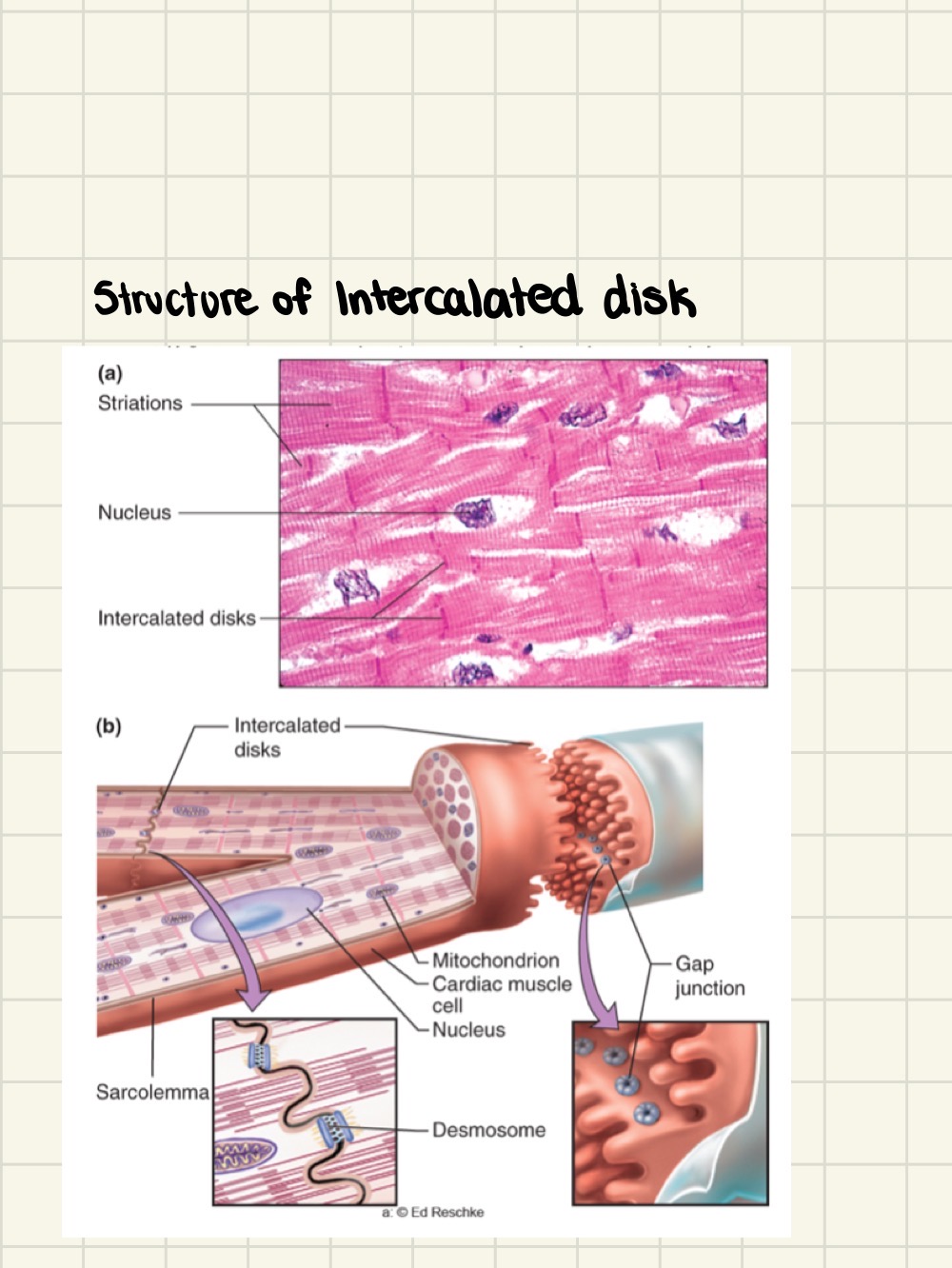
cardiac muscle
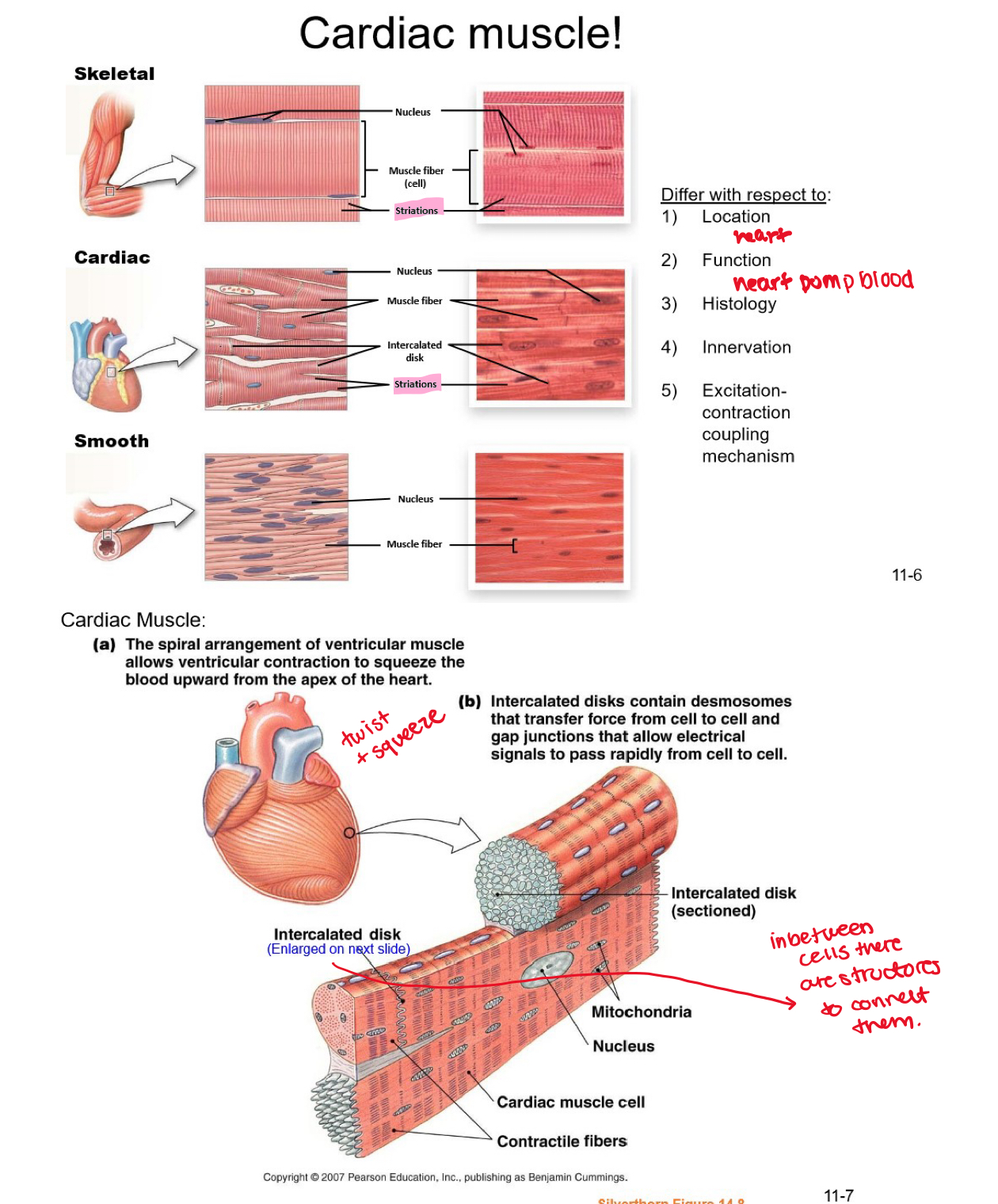
structure of intercalated disk
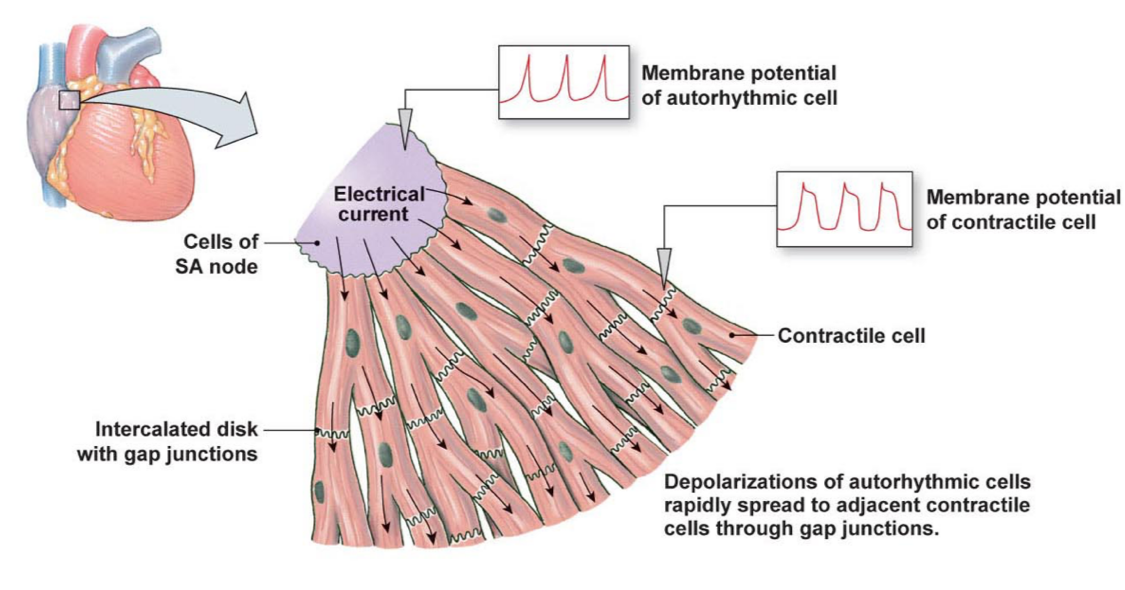
two types of cardiac cells
contractile and autorhythmic (pacemaker)
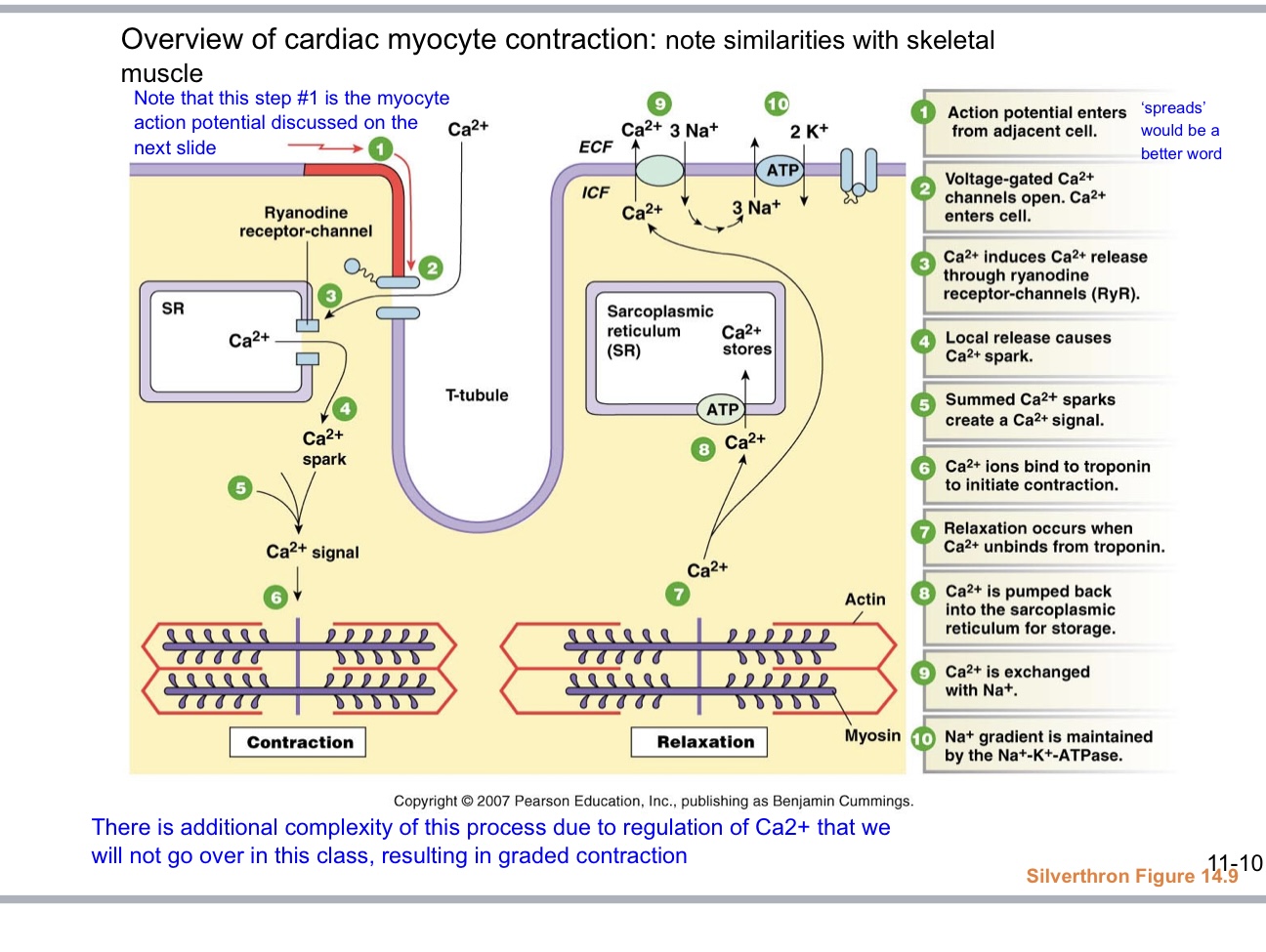
overview of cardiac myocite contraction
ventricular myocyte action potential
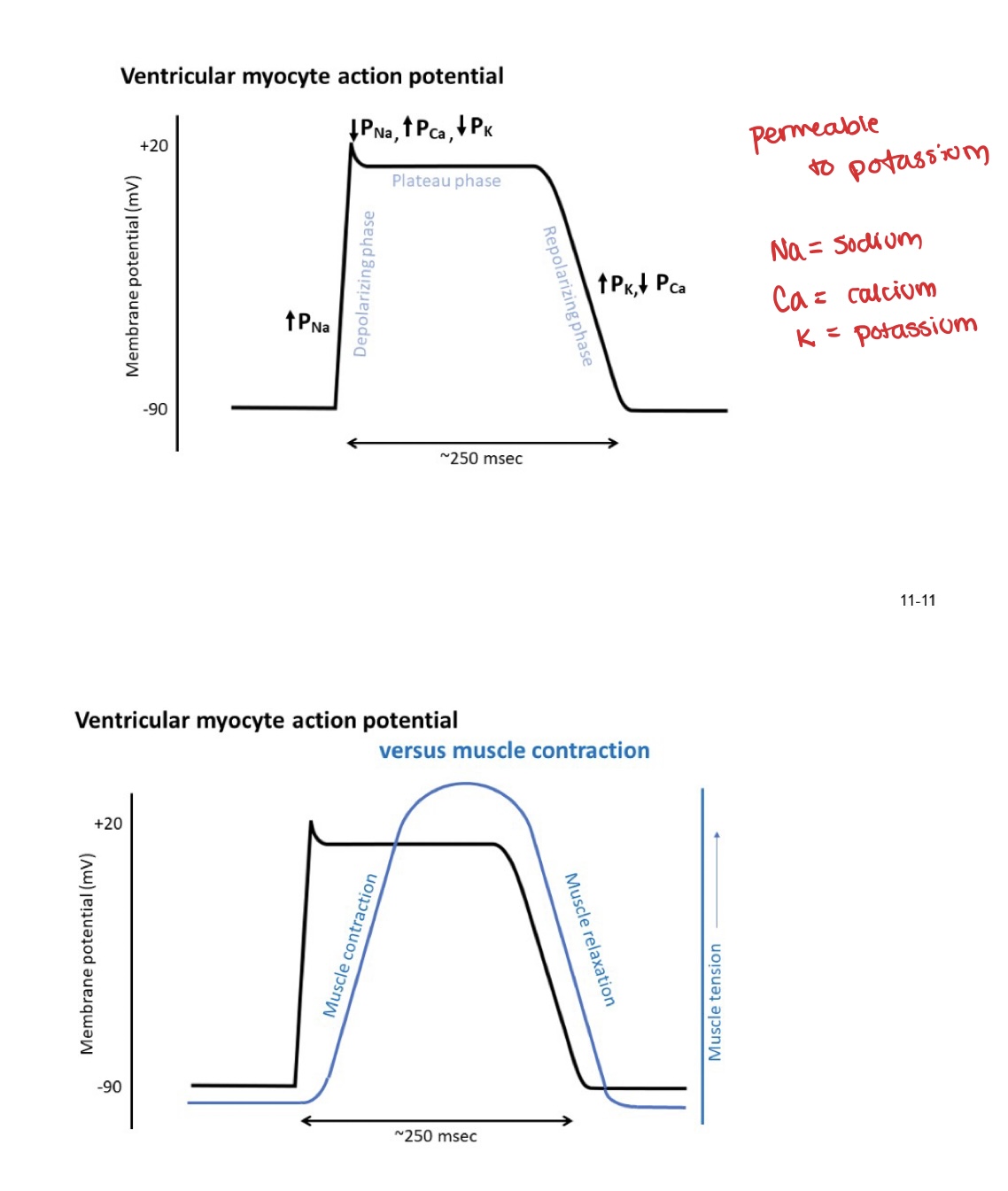
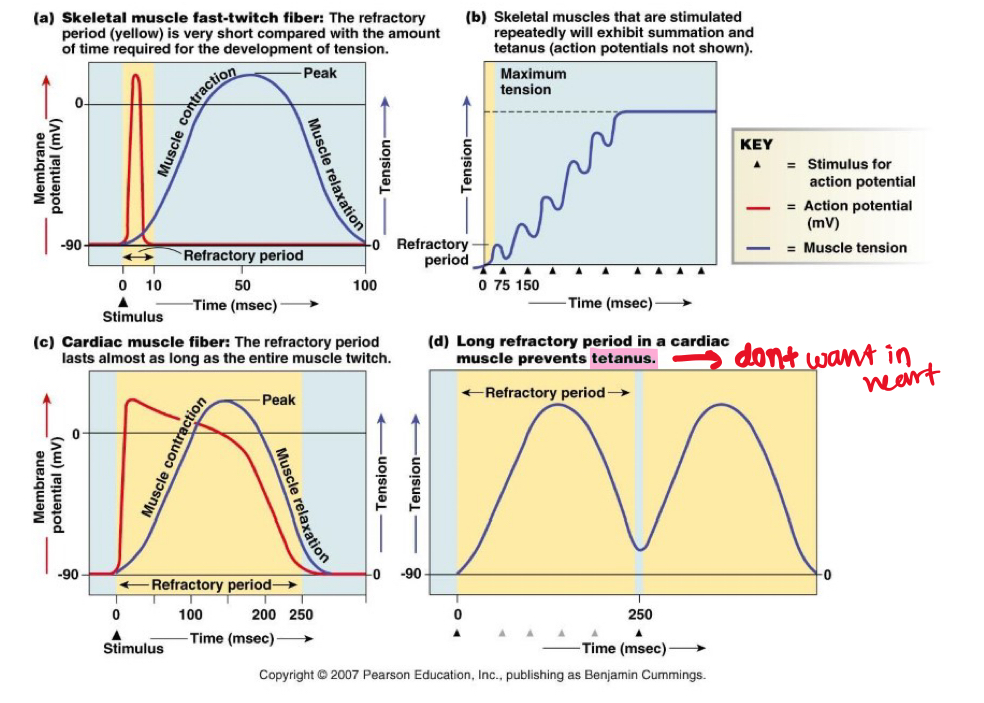
refractory periods
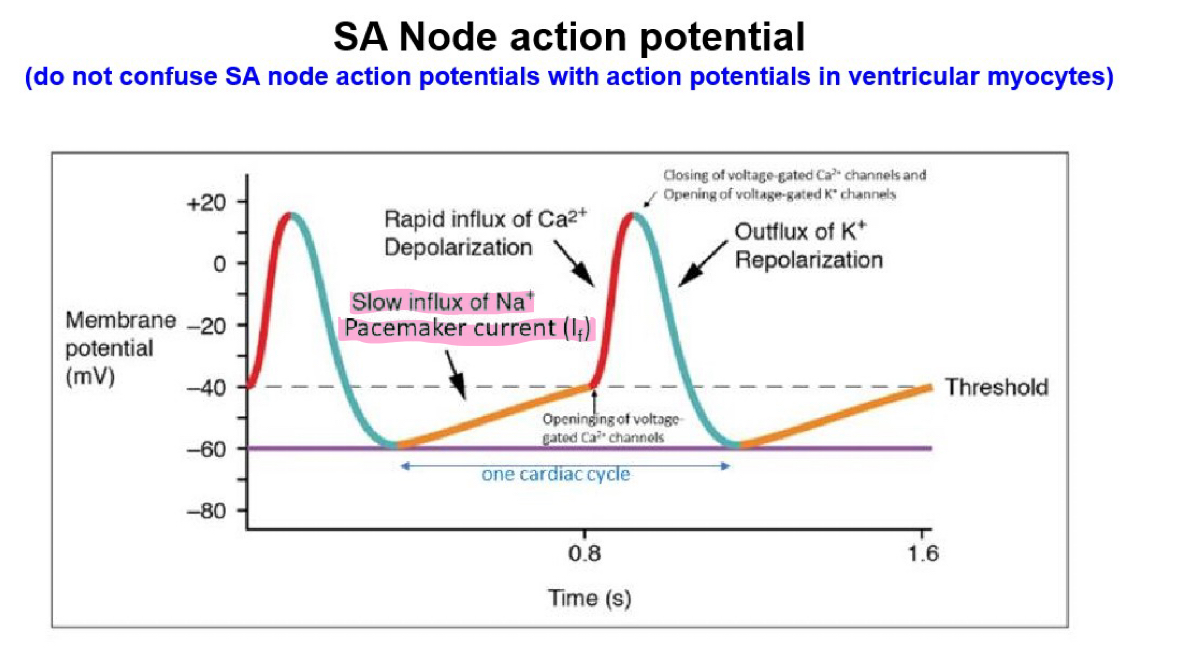
SA Node action potential
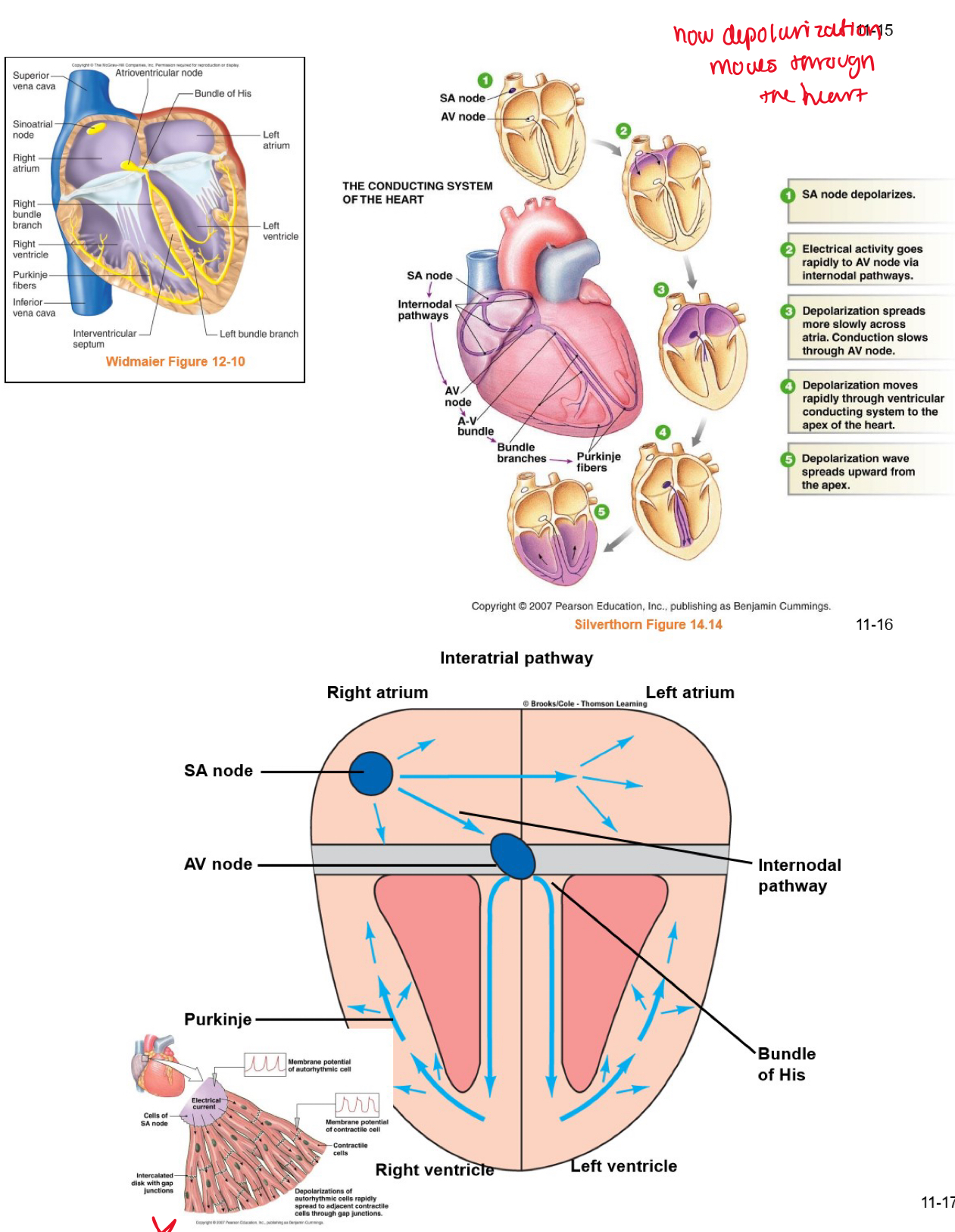
conduction system of the heart
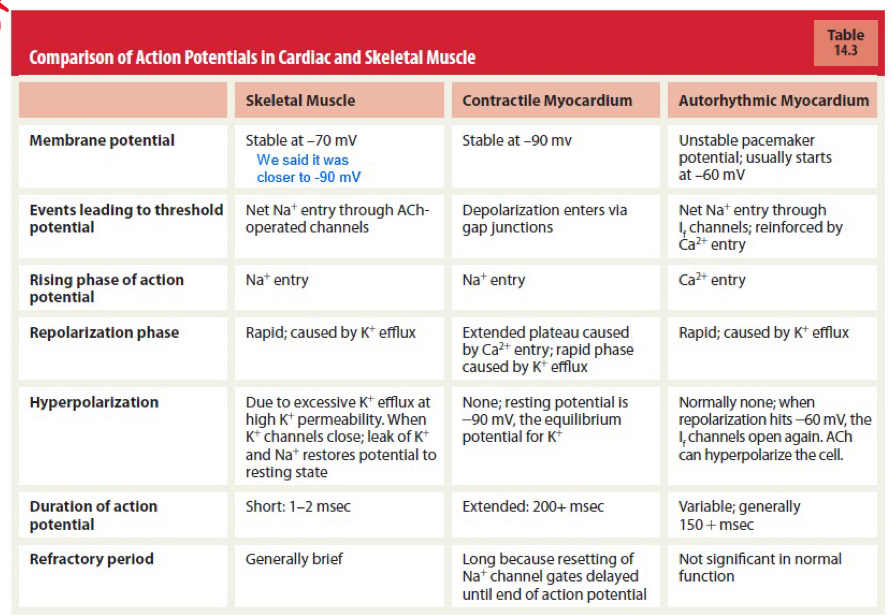
comparison of action potentials in cardiac & skeletal muscle
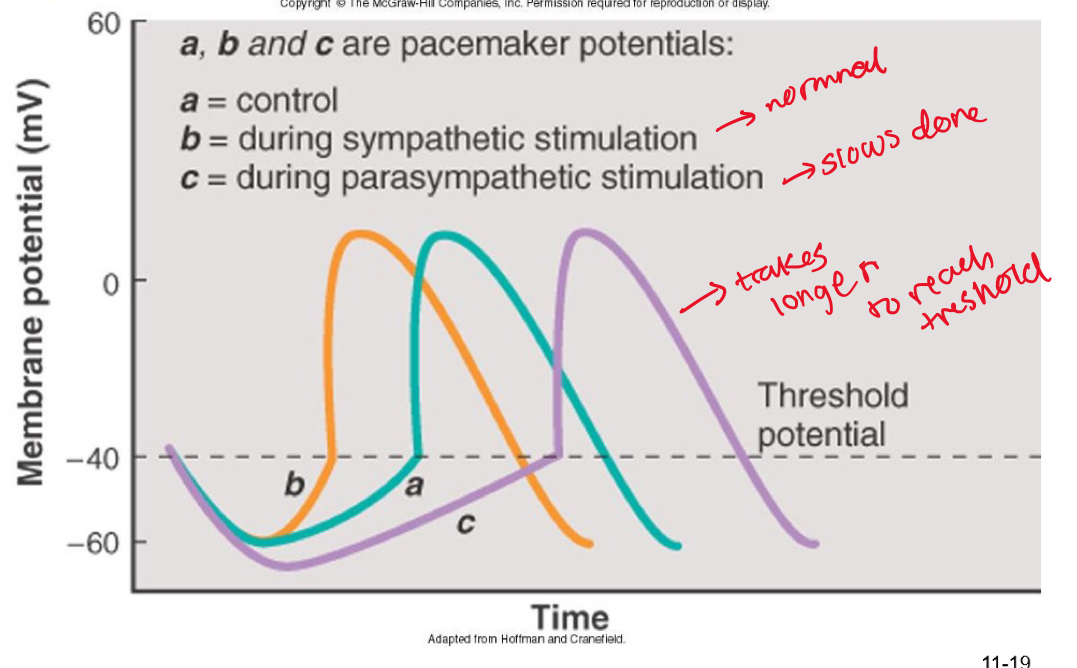
ANS can alter the rate of the pacemaker potential (not the shape of the action potential)
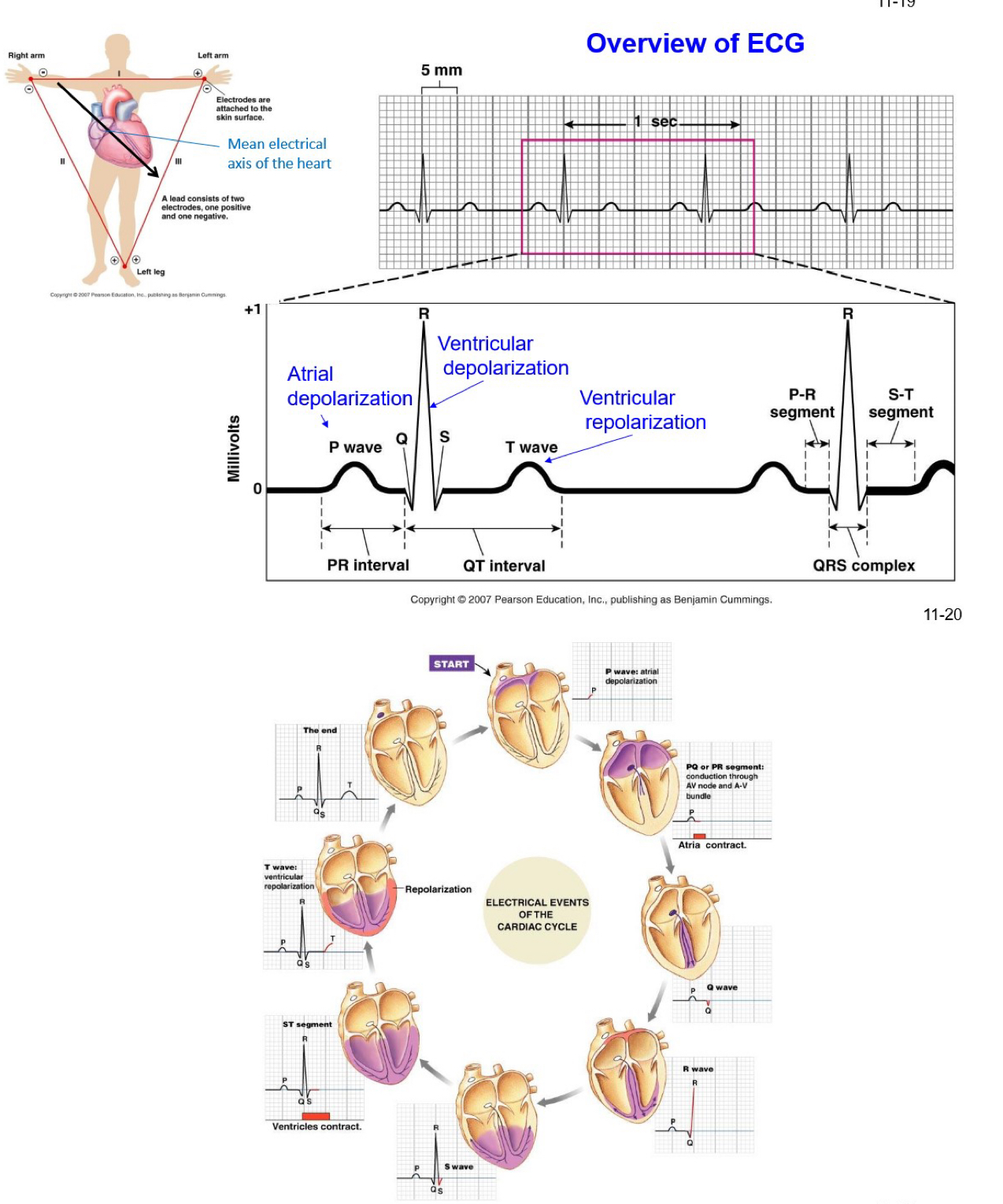
overview of ECG
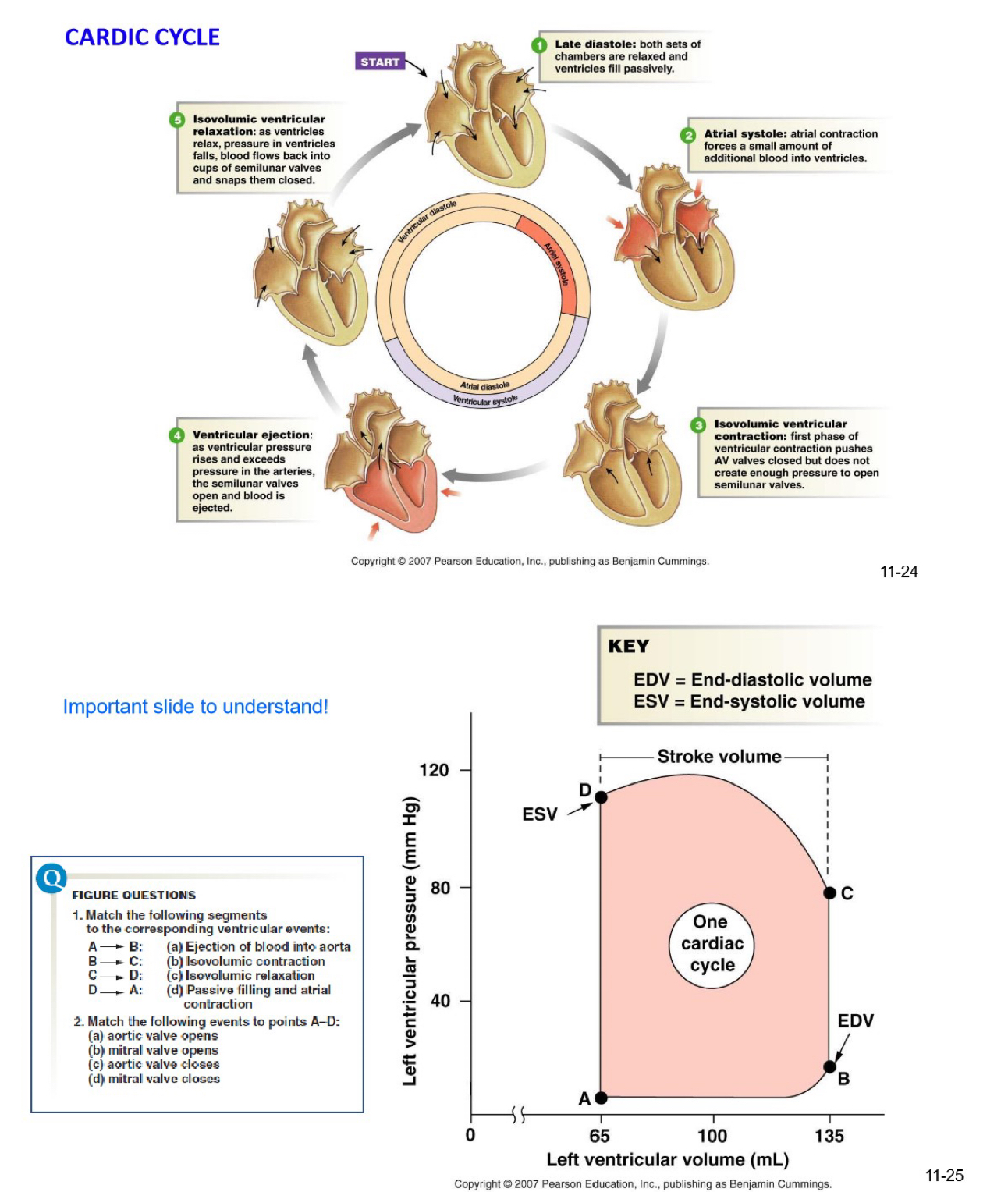
cardic cycle
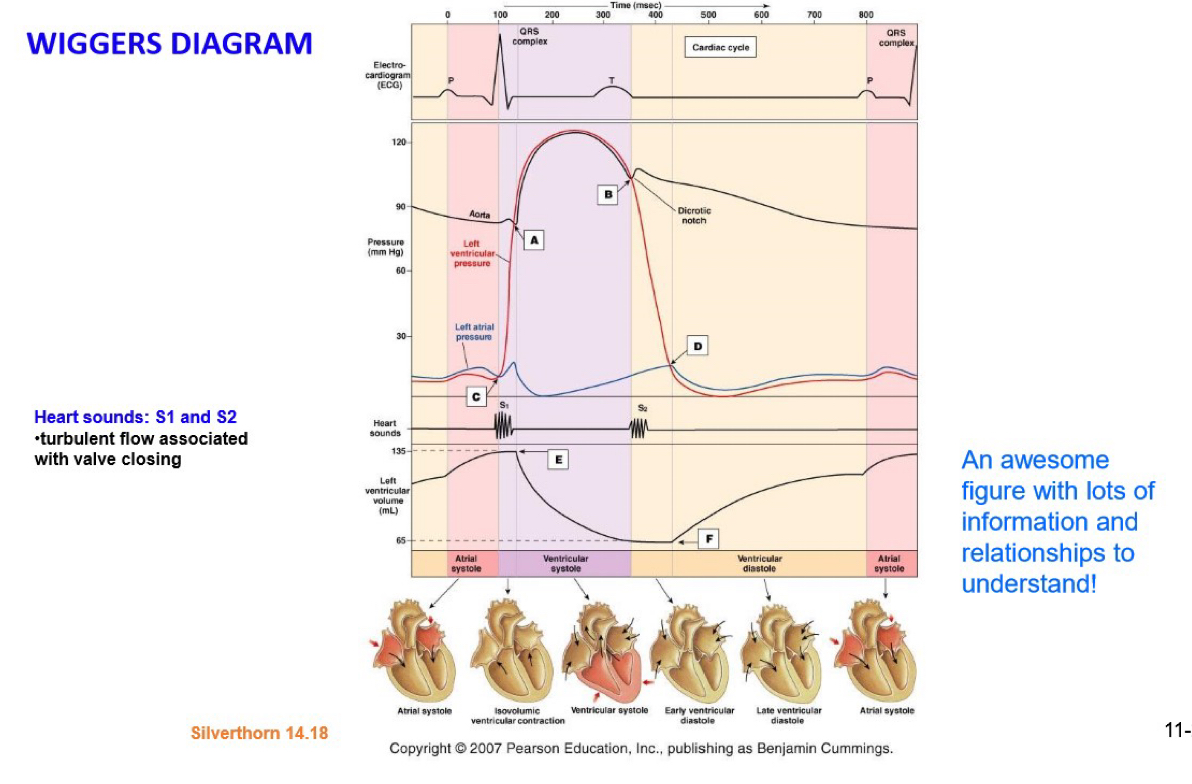
wiggers diagram
stroke volume (SV)
amount of blood pumped by one ventricle during a contraction
stroke volume = end diastolic volume - end systolic volume
SV = EDV - ESV
70 mL = 135 mL - 65 mL
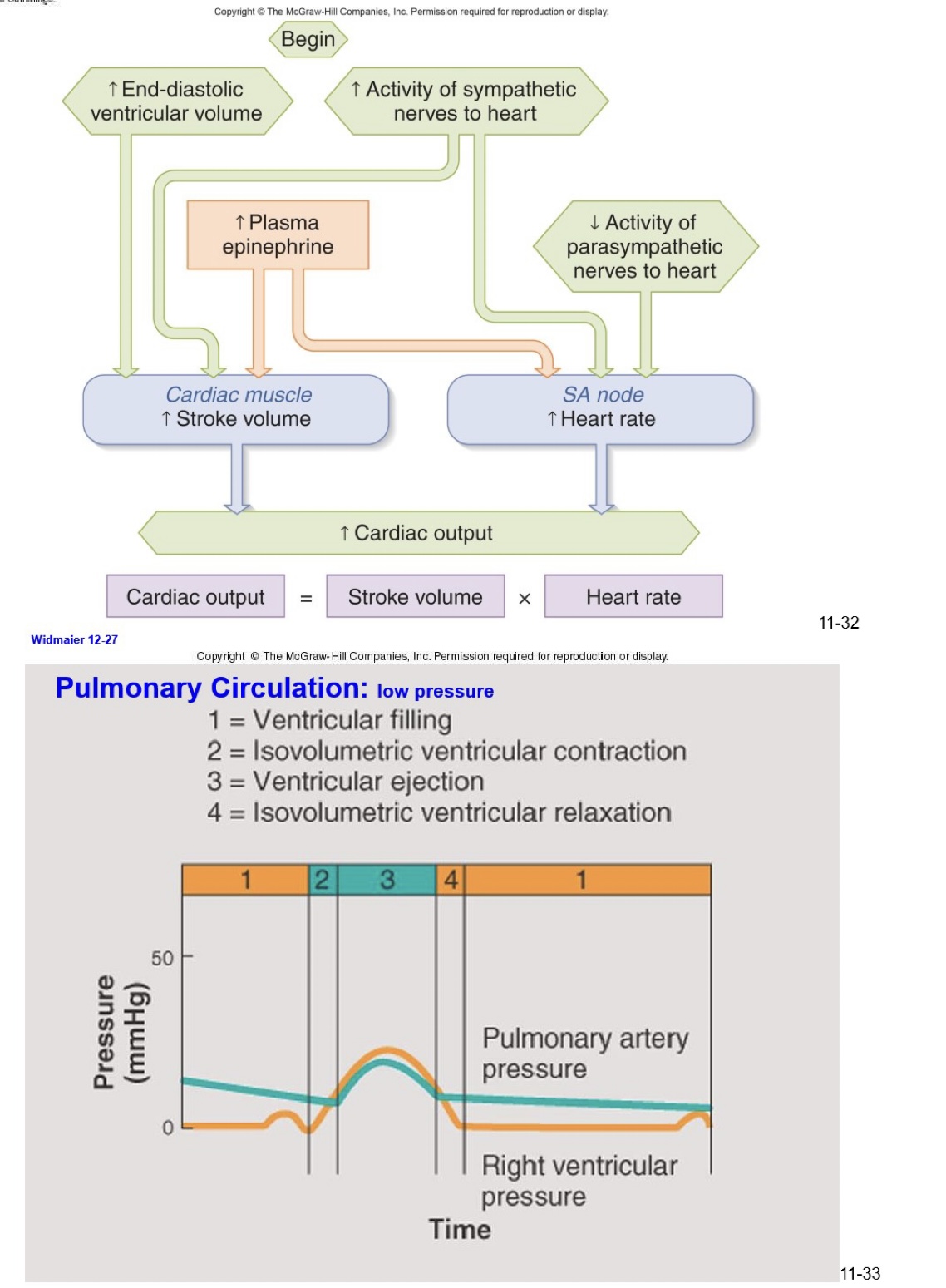
cardiac output (CO)
volume of blood pumped per unit time (by the left heart)
cardiac output = heart rate x stroke volume
CO = HR - SV
CO = in liters per minute
HR = in beats per minute
SV = in liters
5 L/min = 72 b/min x 0.07 L/b
CO = HR x (EDV - ESV) ← all of these parameters are regulated
autonomic control of the heart rate
SA node innervated by both sympathetic and parasympathetic and important for regulating heart rate
AV node also innervated by both, but not very important
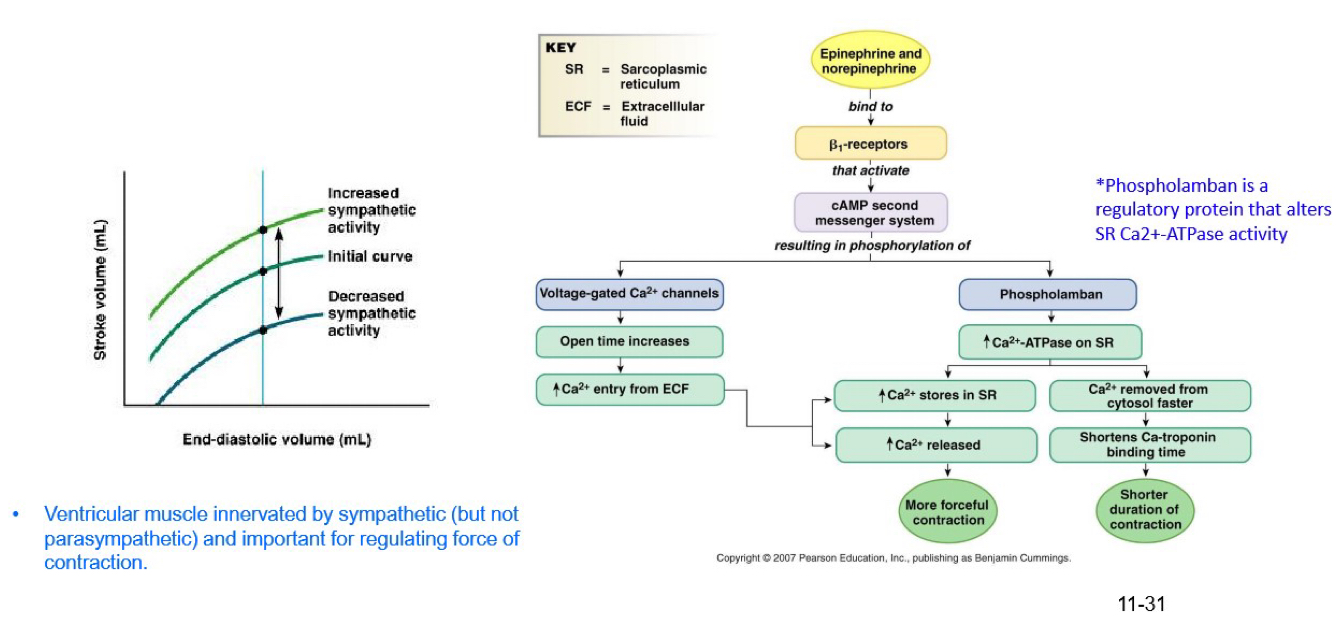
ventricular muscle innervated by sympathetic (but not parasympathetic) and important for regulating force of contraction

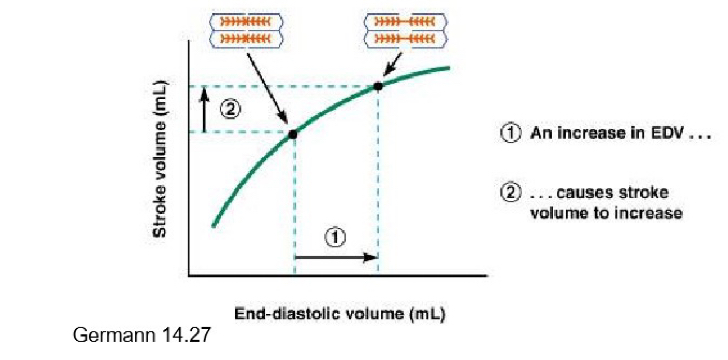
starling law of the heart
stroke volume increases in proportion with EDV
sympathetic nervous system influences cardiac contractility altering the starling curve and ESV
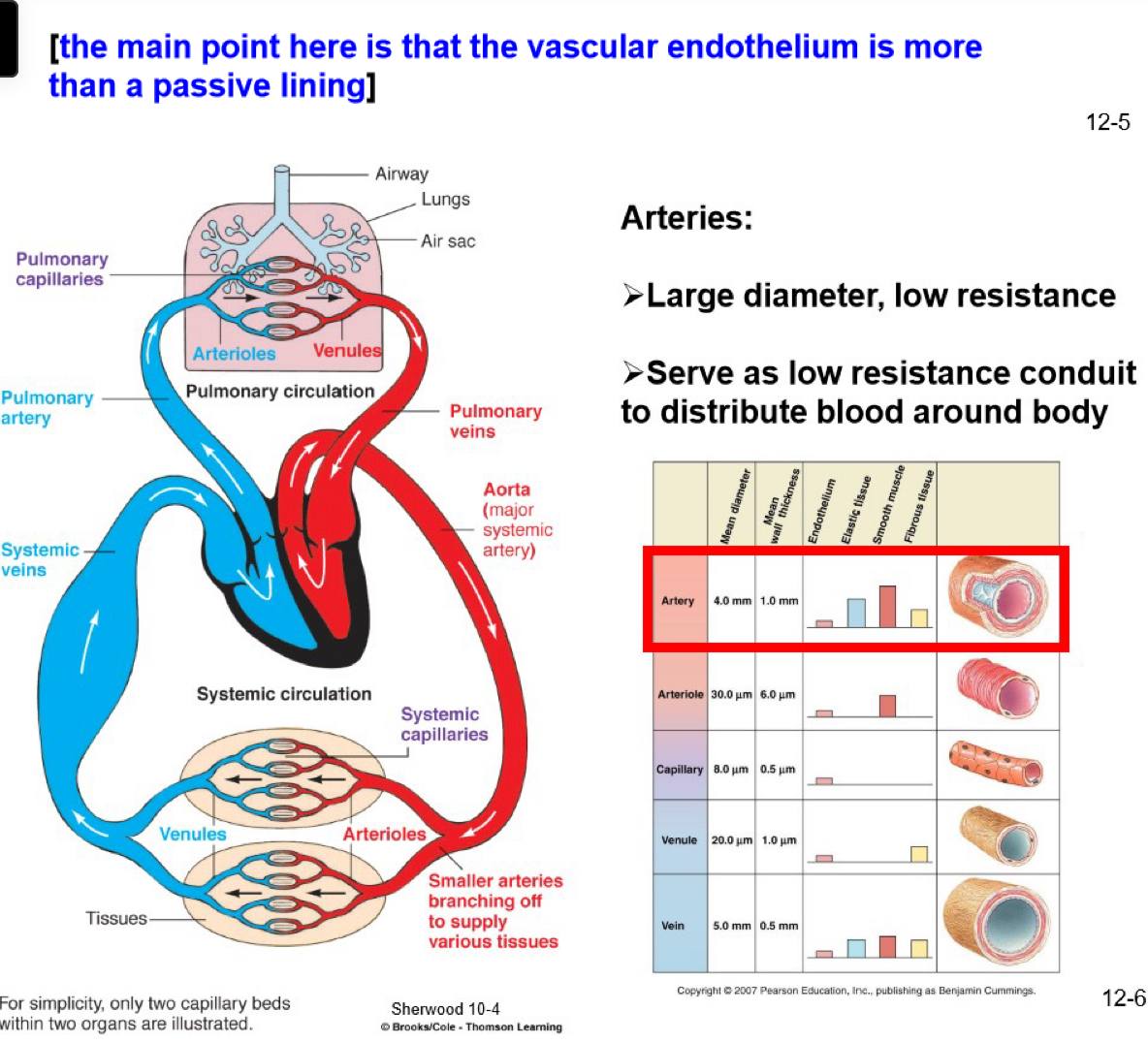
pulmonary circulation diagrams
cardiac output (resting conditions)
cardiac output (resting conditions) - 5 L/min - thats flow
flow = ΔPressure/resistance
the vasculature provides resistance
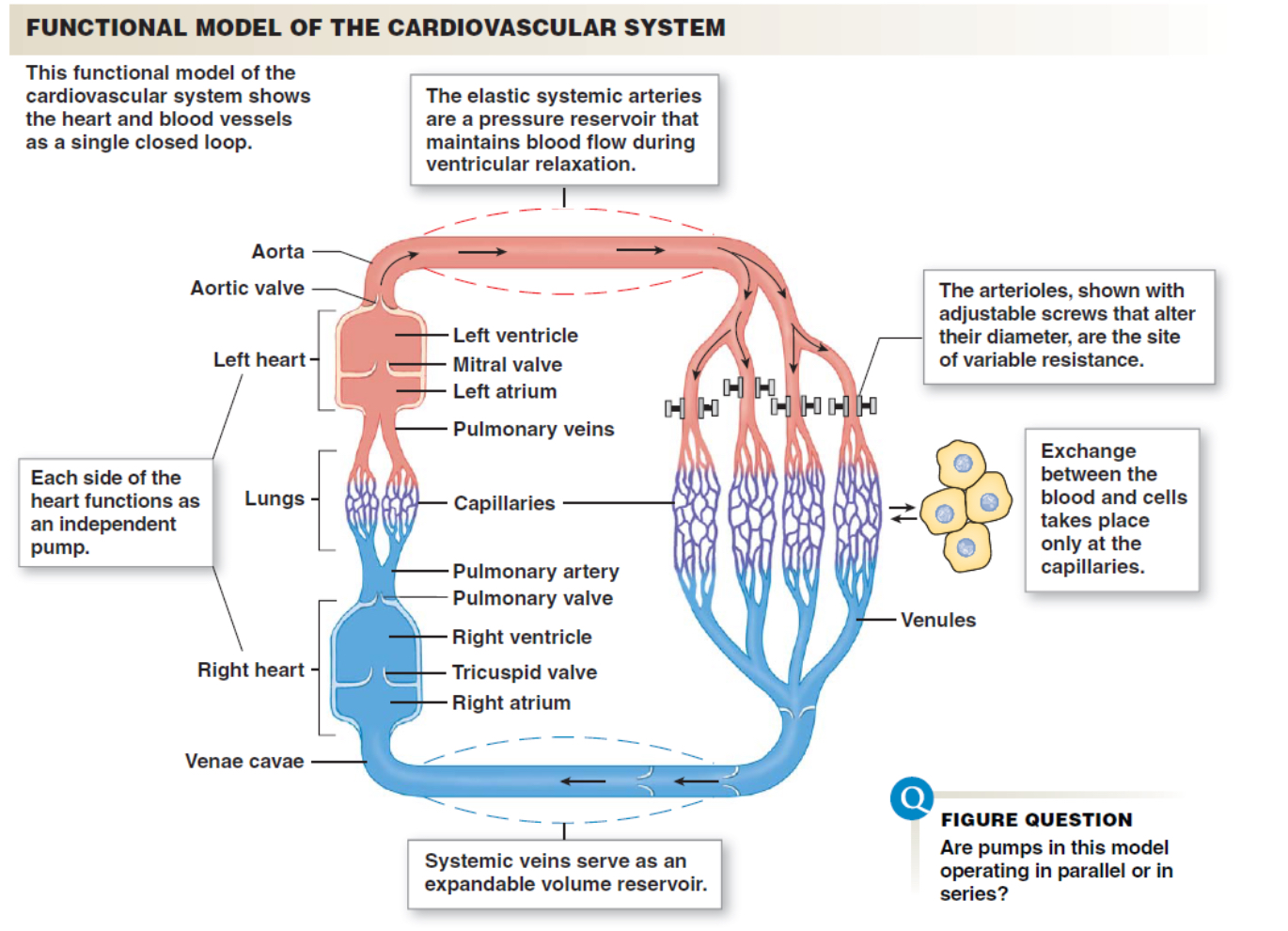
functional model of the cardiovascular system
amount of flow through any level of this system (e.g, arteries, capillaries, veins) is the same
as resistance varies, pressure gradients vary
pressure falls across a resistance
as relative resistance of different arterioles changes, so too does flow
as total cross-sectional area changes, flow velocity changes
blood vessel structure
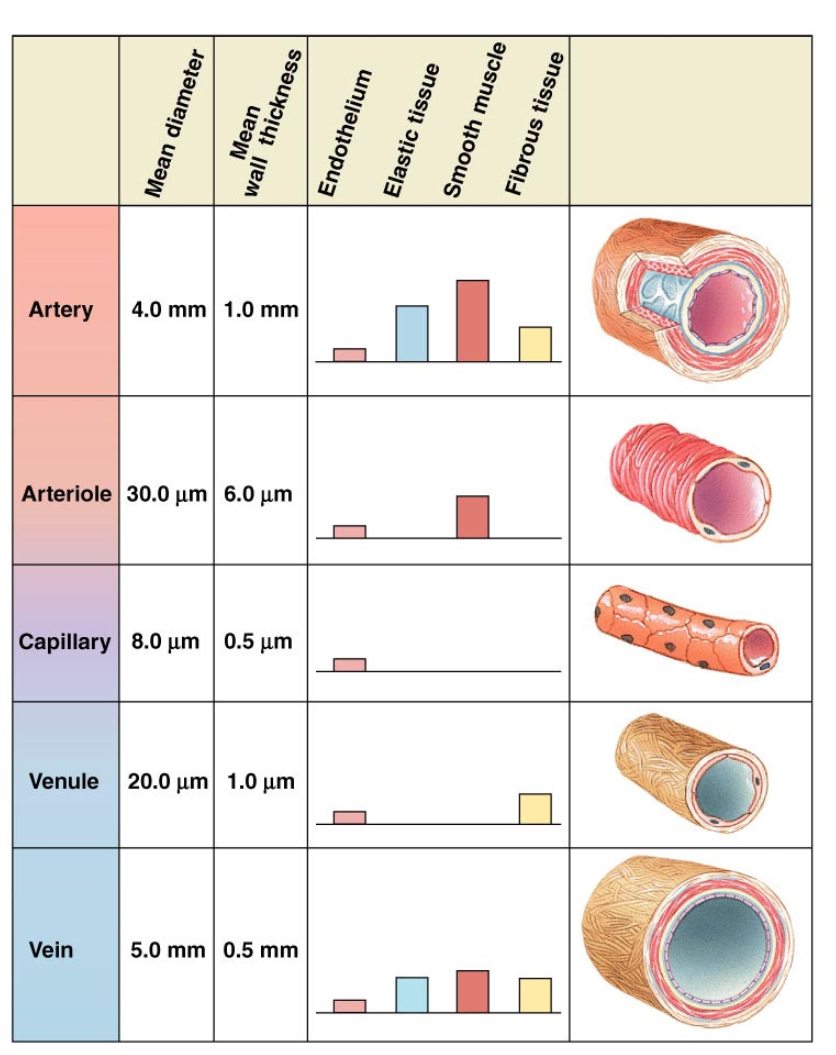
endothelial cells lining blood vessels serve several functions:
only need to know:
physical lining of blood vessels
secrete substances that influence vascular smooth muscle
[main point is that the vascular endothelium is more than a passive lining]
arteries
large diameter, low resistance
serve as low resistance conduit to distribute blood around body
systemic circulation pressures
arteries are not rigid, but rather somewhat compliant (C= dV/dP)
→ as a result of compliance, arteries serve to keep blood flowing during diastole
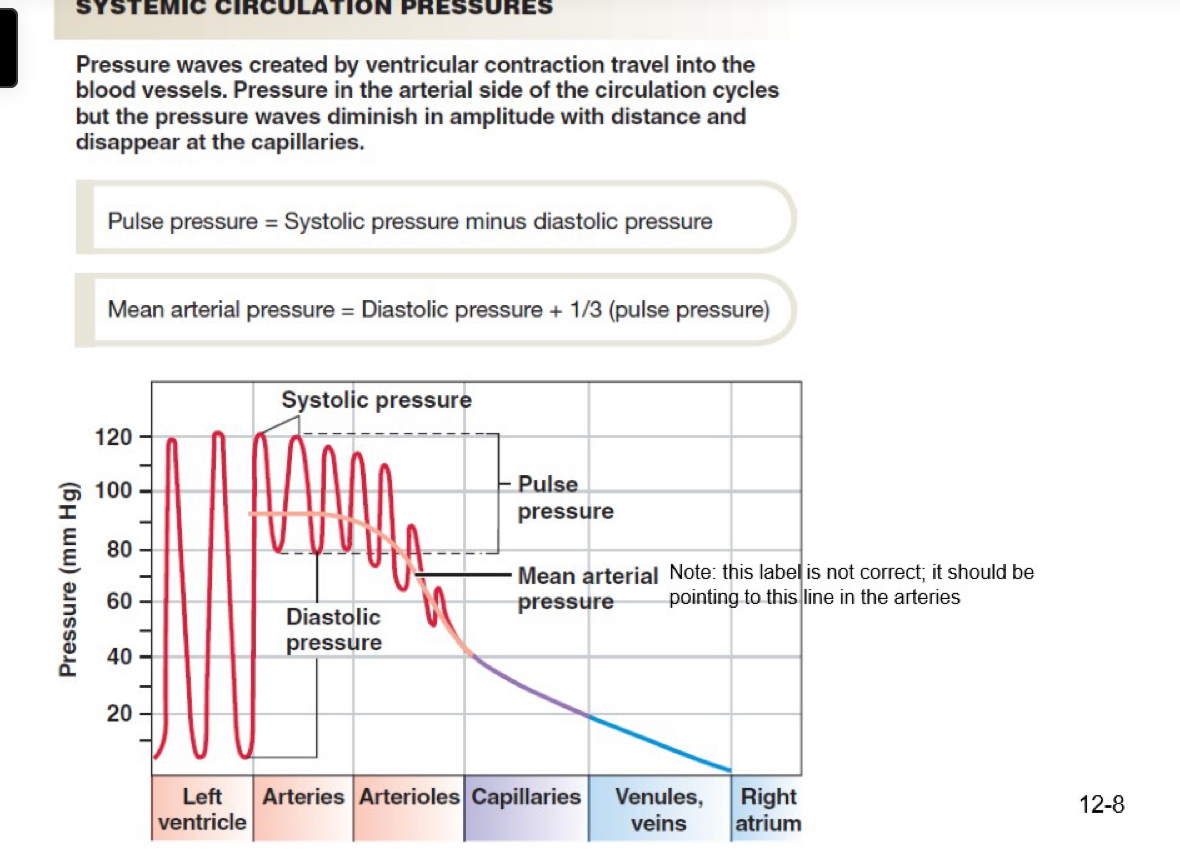
arterial pressure pulse
Mean Arterial pressure = diastolic pressure + 1/3 of the pulse pressure

what factors influence arterial blood pressure?
here we mean the average arterial pressure across the cardiac cycle; mean arterial pressure
dPressure = flow * resistance
what factors influence pulse pressure?
stroke volume and heart rate
arterial compliance
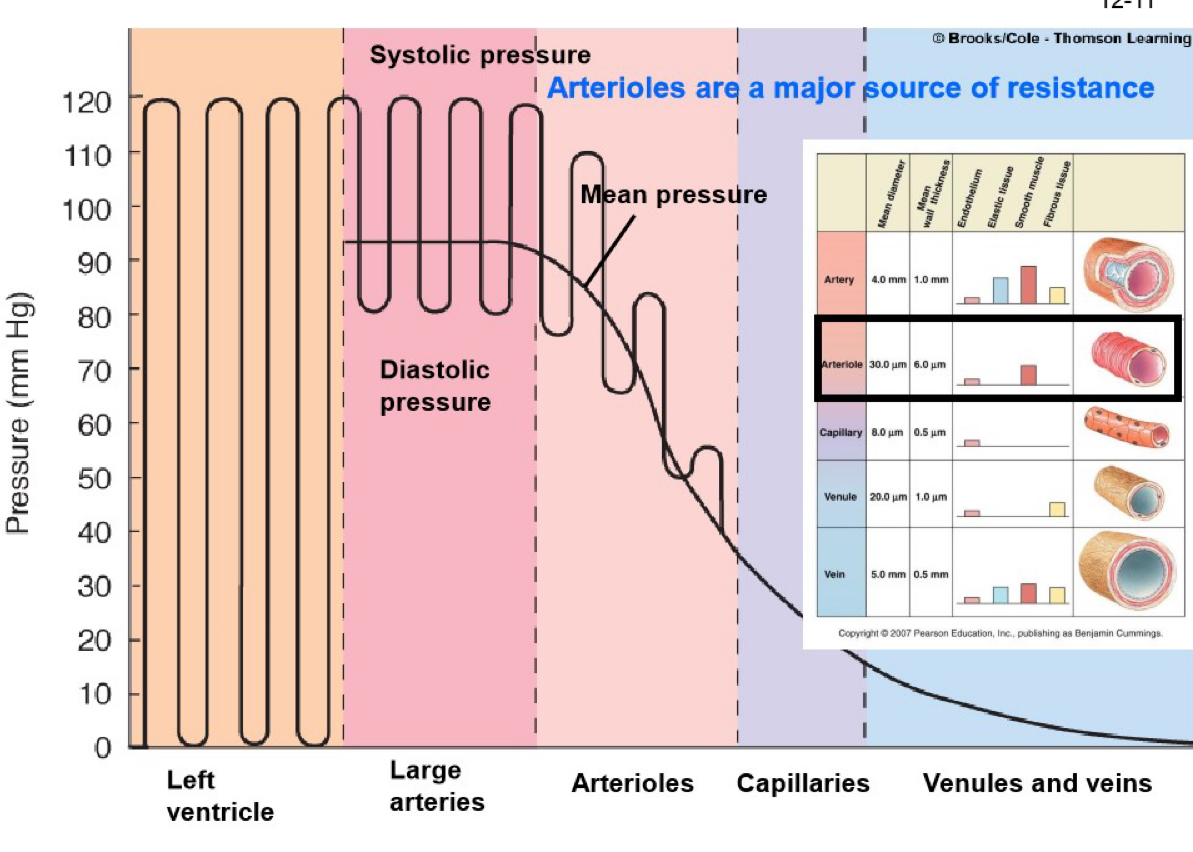
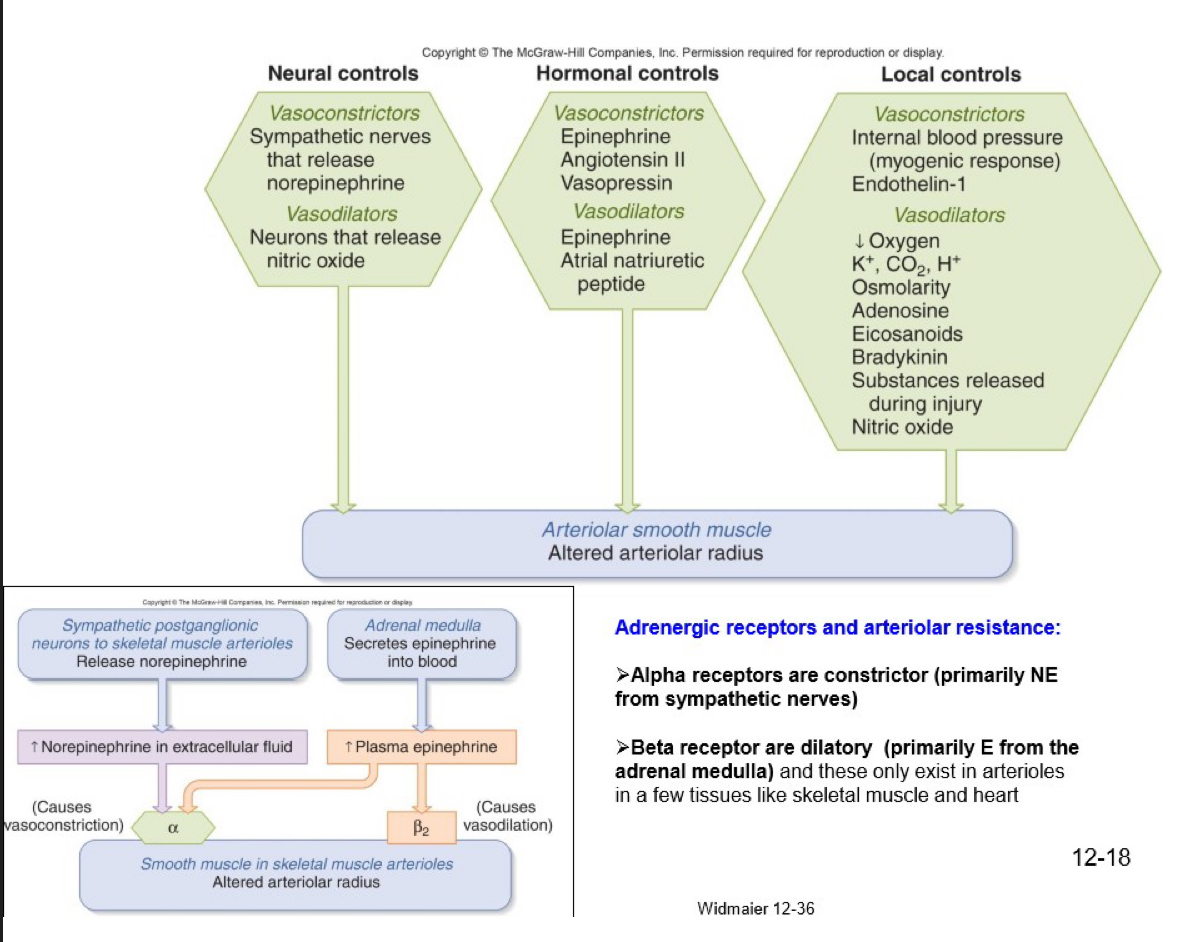
myogenic tone
(muscle tone in the arterioles)
can be regulated by:
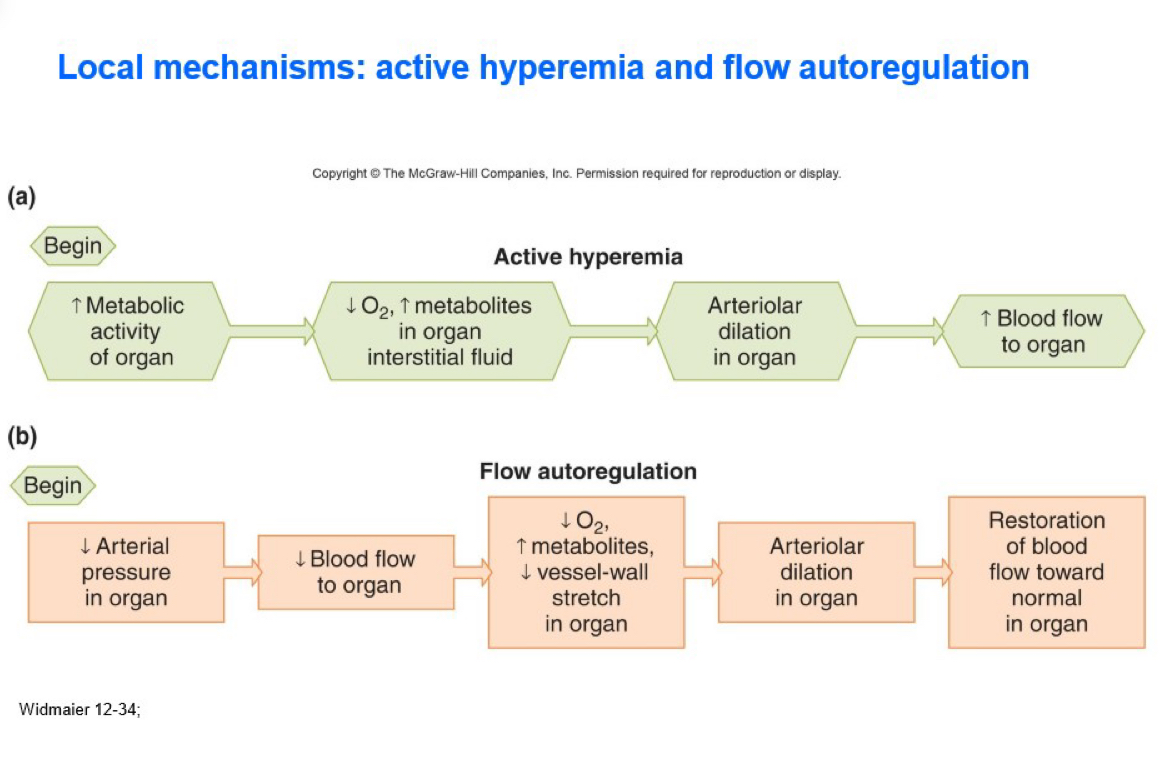
local mechanisms
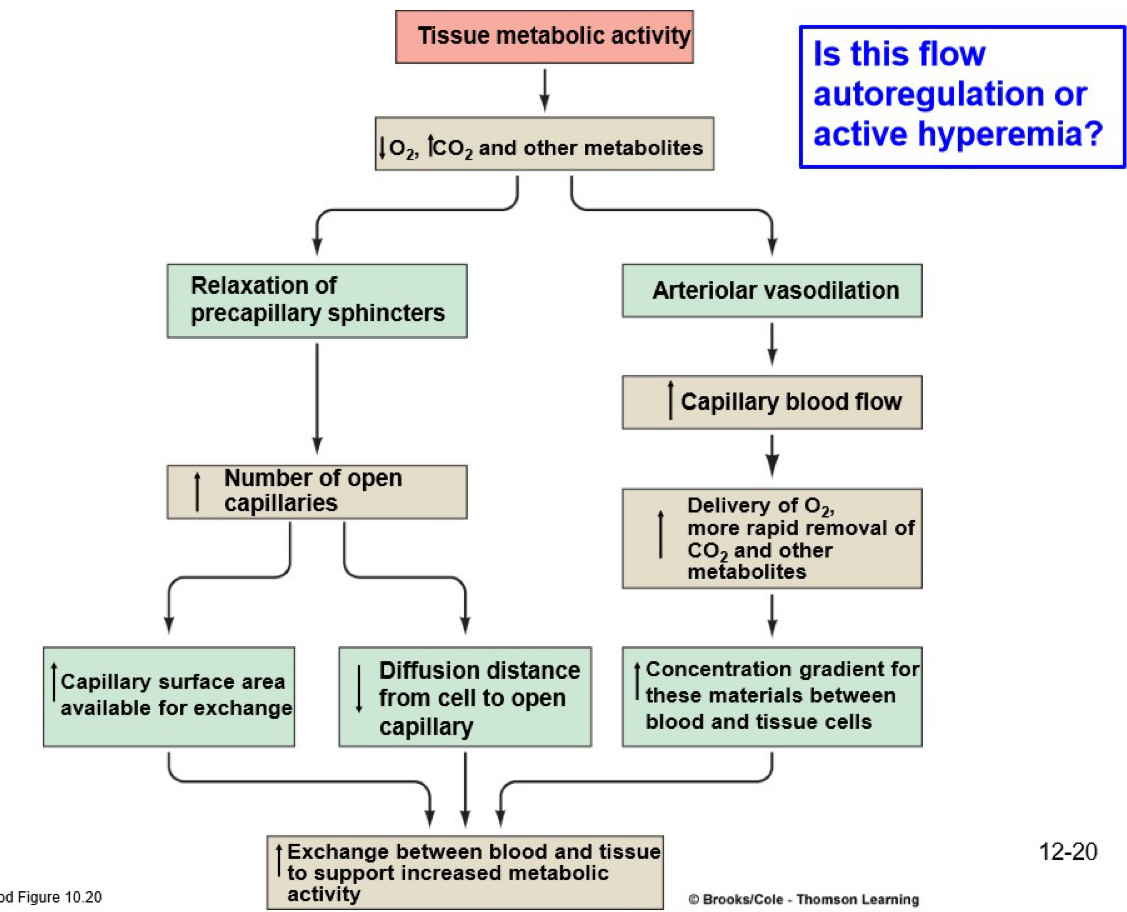
active hyperemia
flow autoregulation
endothelial factors
extrinsic
sympathetic neural control
hormones
epinephrine
angiotensin
vasopressin (antidiuretic hormone)
atrial natriuretic hormone (and many more)
local mechanisms: active hyperemia and flow autoregulation
adrenergic receptors and arteriolar resistance:
alpha receptors are constrictor (primarily NE from sympathetic nerves)
beta receptors are dilatory (primarily E from the adrenal medulla) and these only exist in arterioles in a few tissues like skeletal and heart
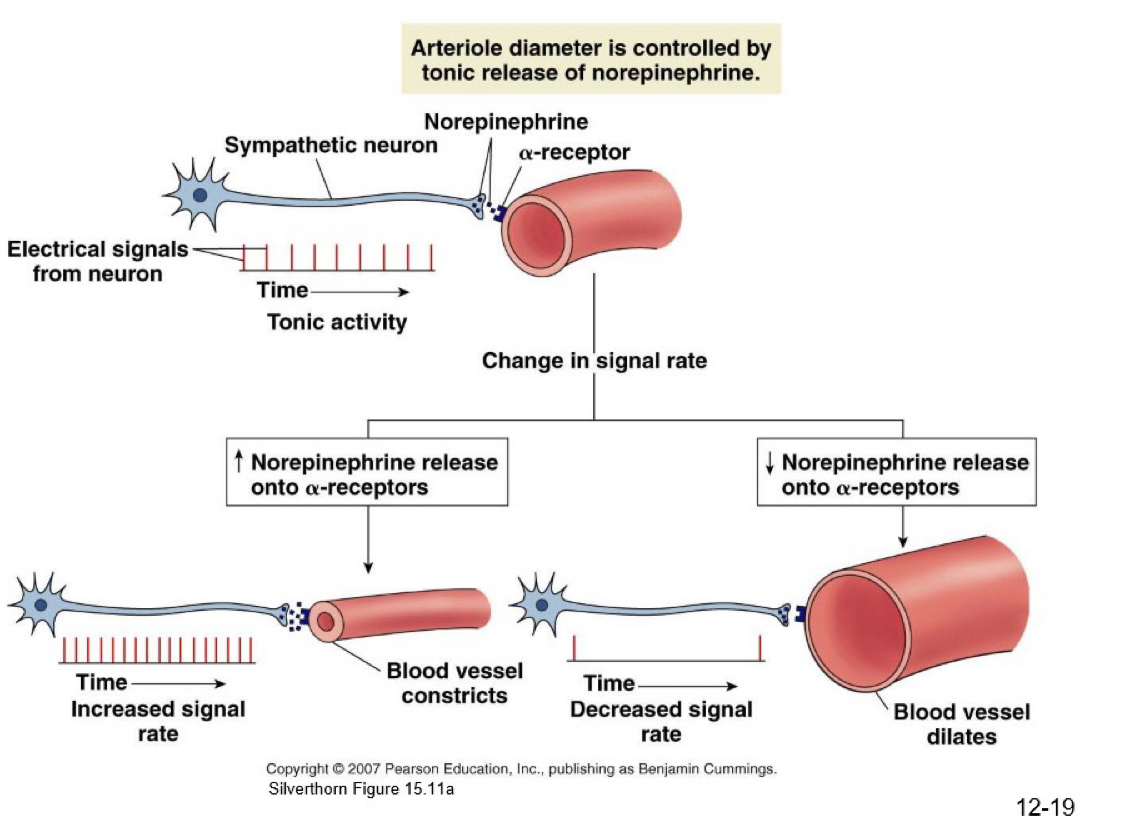
arteriole diameter is controlled by tonic release of norepinephrine
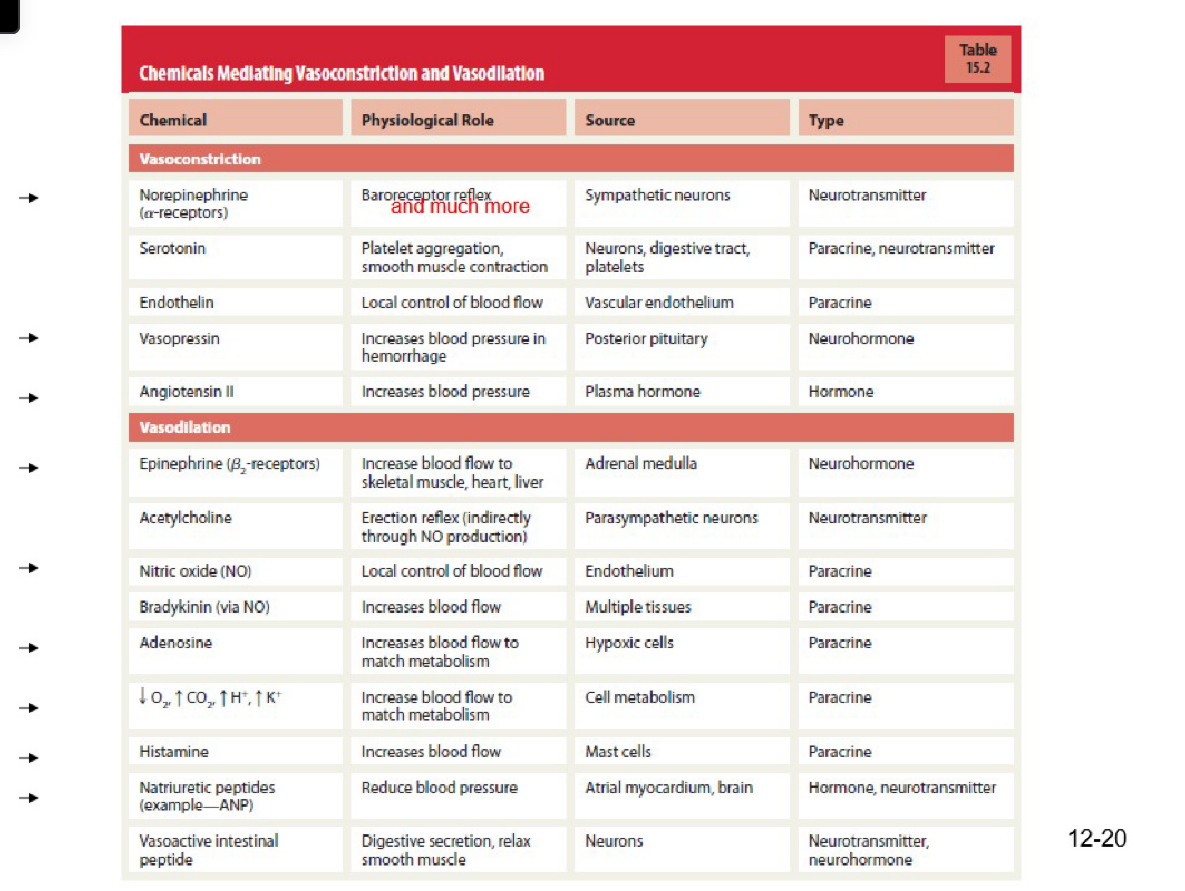
chemicals mediate vasoconstriction and vasodilation (CHART)
tissue metabolic activity
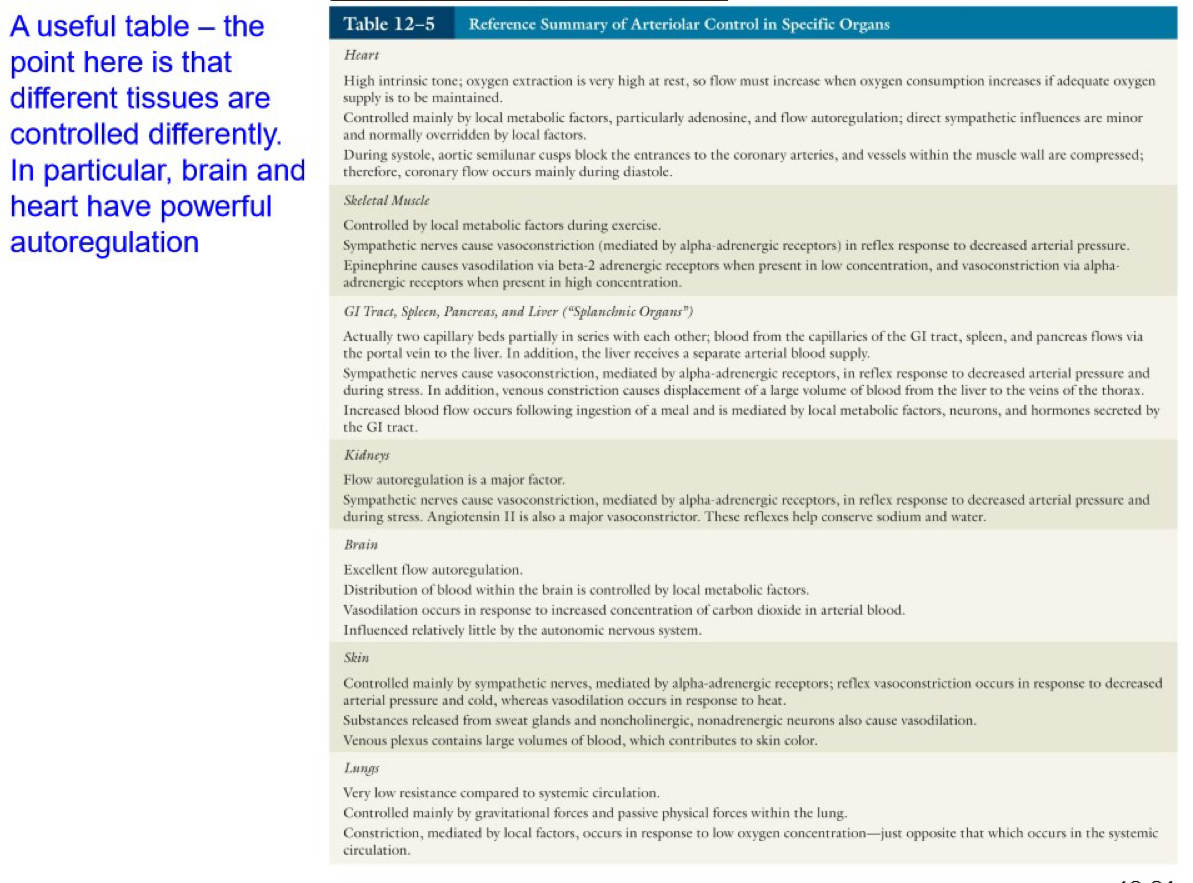
reference summary of arteriolar control in specific organs (CHARTS)