ALL - flashcards for credit 1 RADIO
1/255
Earn XP
Description and Tags
ALL LECTURES
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
256 Terms
Basic principles of x-ray include?
Guidelines ensuring patient benefits, professional competence, and safety during x-ray examinations.
1 examination per time in x-ray room, dorr is closed, minimal with people in the room, no pregnant women + children.
machine with certificate, protective equipment.
Protection against external x-rays → distance, time, shielding, rotating of workers + equipment.
Secondary radiation is?
Radiation emitted by materials when exposed to primary radiation, contributing to overall exposure.
When primary radiation (from machine) hits a body, some of the energy can bounce off or scatter. This bouncing is called secondary radiation.
one way this happens is by compton scattering.
Tissue weight factors is?
Values used to calculate effective radiation doses absorbed by different tissues, reflecting their sensitivity to radiation.
can optimize imaging techniques to minizime radiation exposure while ensuring safety.
Factors:
0.12 bone marrow, colon, lungs, stomach, mammary gland
0.08 gonads
0.04 bladder, esophageus, liver
0.01 bone surface, brain, salivary glands, skin
Wilhelm Conrad Røntgen is?
The father of radiology, credited with the discovery of x-rays.
Electromagnetic radiation is?
Energy waves that can be classified into non-ionizing and ionizing types based on their energy levels.
non-ionizing: low energy, not enough to give electrons from atoms (travels in form of electromagnetic waves/particles) ex. UV radiation, light, infrared, microwaves.
ionizing: high energy, can release electrons from atom packages → ions. ex. X-rays, gamma.
Properties of x-ray beam?
x-ray beam: x-rays travel in straight lines and a beam of x-rays comes from its source. The beam hits structures → magnified.
properties: straightforward motion, penetration, ionization effects.
X-ray tube
Device consisting of a cathode and anode used to make x-rays within a vacuum-sealed envelope.
cathode emits electrons when heated, anode is target that electrons collide with → makes x-rays
Sciascopy vs Sciagraphy
Sciascopy provides real-time imaging using x-rays
mainly for checking stomach, intestines.
uses CCD sensor amplifier → can monitor images.
sciagraphy captures still images for diagnosis.
Primary radiation is?
The initial beam of radiation emitted from the x-ray tube.
Stationary vs rotating anode.
Types of x-ray tubes
stationary anodes have fixed positions in the x-ray tube. This anode will get localized heating + limited heat dissipation. Heat is hitting the same spot over and over → can deform the surface → reduction of efficiency.
rotating anodes distribute heat evenly for better performance.
heat is distributed as the anode rotates → longer scans and at higher doses.
Compton scattering is?
A process where primary radiation interacts with particles in the body, making them move which makes them able to send out their own energy, resulting in secondary radiation.
Radiopacity vs radiolucent.
Terms describing how different materials appear on x-ray images:
radiopacity: going to white
radiolucent: going to black
what are the 5 basic elements in x-ray when it comes to absorption?
air (black)
fat (dark-grey)
water (grey)
bone (blue grey)
metal (white)
x-ray have 3 important aspects, what are these?
kV (kilovolts) - power
mA (miliamperes) - number of x-ray photons
Time - how long they have been used
Digital radiography
Techniques for capturing x-ray images digitally, including indirect and direct methods.
Indirect (IR): uses phostimulable phosphor plate to capture the image → processed → convert stored energy into digital image.
direct (DR): uses flat-panel detector that directly converts x-rays → digital signal → processing.
Computer Tomography (CT)
Imaging technique using x-rays to create detailed cross-sectional images of the body.
Consist of rotating x-ray source + detectors, encircling the object being examined, as they rotate → gather data on how much x-ray is absorbed by different tissues → data computer processing → displayed in grayscale on screen (giving visualiation).
technique relies on inverse radon transform.
Ultrasound
Imaging method using ultrasonic waves to visualize soft tissues, requiring an aqueous environment like ultrasound gel) for effective transmission.
X-ray cassette is?
Device used to hold x-ray film or digital plates during exposure to x-rays. It is made to protect the film or plate from light and damage, + proper positioning.
can be used in traditional + diital systems.
X-ray artifacts are?
Unwanted distortions (inaccuracies) in x-ray images that can hinder accurate diagnosis.
radiograph distortion (shape, position mistakes)
magnification (incorrect distance)
summing effect (overlapping tissues)
siluet effect (tissues with same density overlap)
Darkroom principles
Guidelines for setting up a lightproof environment:
setup needs to be lightproof, services need to work, safe light (low intensity) and ventilation.
dry side - for handling undeveloped film, clip hangers
wet side - chemical processing place
converting invisible images on film to visible inage → turning exposed silver halide crystals → black metallic silver.
storage of x-rays - sensitive to light, need light-proof container/original film box, sensitive to high temperatures, need info on the film.
DICOM
DICOM is?
Digital Imaging and Communications in Medicine, a protocol for storing and transmitting medical imaging data securely.
Bone Pathology
The study of diseases and disorders affecting the bones, often involving diagnosis and treatment in veterinary medicine.
Definition of bone density, what do we evaluate when looking at it?
Bone density: amount of mineral matter per square cm of bone, Important indicator of bone strength and health. We assess it in radioloogy, for various conditions. When evaluating bone density, we look at:
Density (appearance of bone, normal, decreased (osteoporosis) or increased (like inflammation)
size + shape: abnormalities in this can indicate pathological conditions, like sunburst pattern or disorganized structure can suggest lesions.
Location: specific location, can help narrow down potential diagnoses, like presence of a thin radiolucent line at growth plate can be conditions like hypertrophic osteodystrophy (HOD).
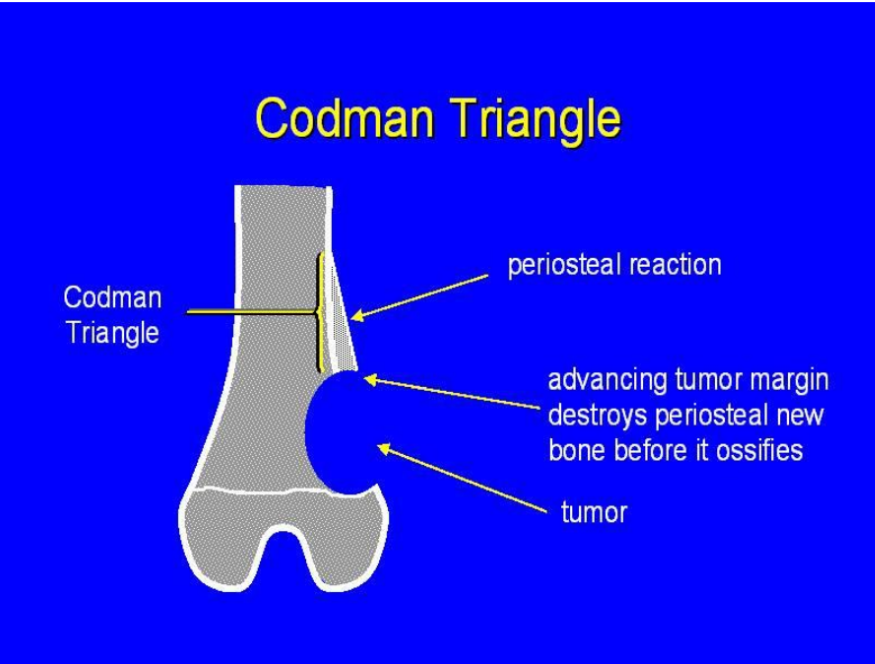
Periosteal Reaction: changes in the periosteum, like “codman`s triangle, indicating lesions or tumours.
The bone density can become low or increased due to pathological condition, what are the types of causes for low density and increased?
Low:
Rachitis
Osteoporosis
Tumours
Increased:
Inflammation
tumour productive
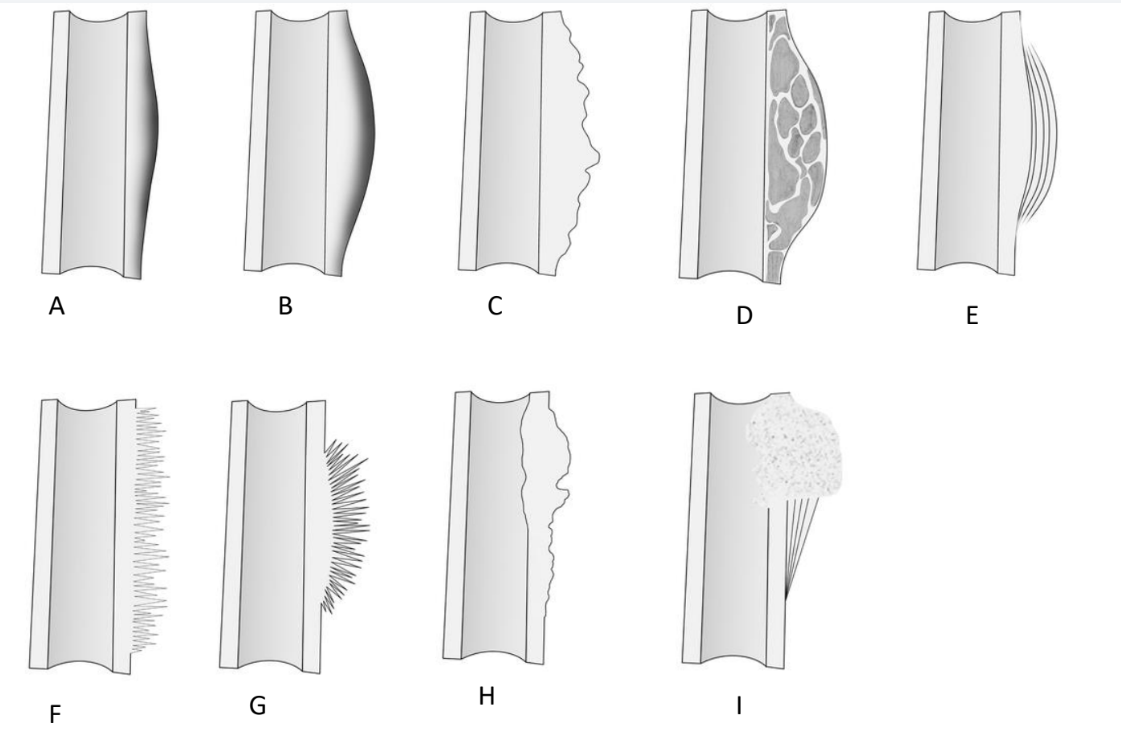
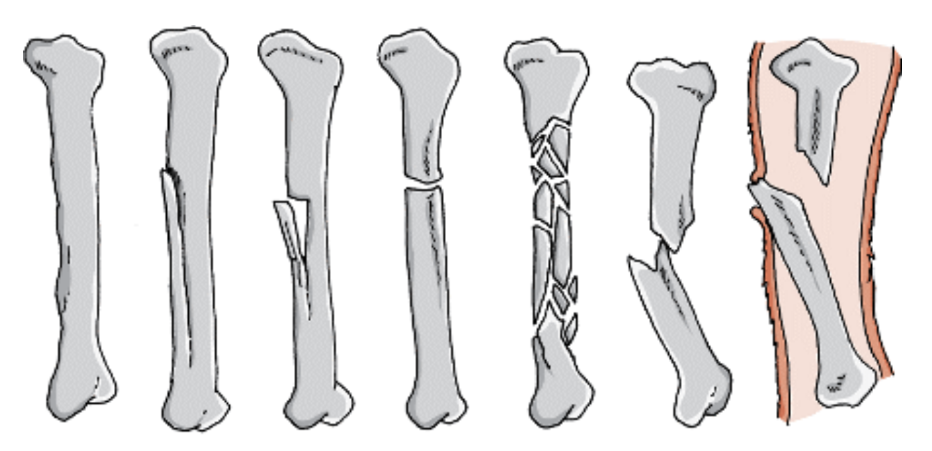
What do we see in the diagrams?
Periosteal reaction: formation of new bone in response to various stimuli affecting the periosteum (CT surrounding outer surface of bones)
subtypes of nonagressive and aggressive periosteal reaction.
A) Thin
B) solid
C) thick irregular
D) Septated
E) laminated (onionskin)
F) perpendicular/hair on end
G) sunburst
H) disorganized
I) codman triangle

Which periosteal reaction is this?
Laminated (Onionskin) periosteal reaction, appearing along lateral cortex of distal femur
Osteomyelitis (infection of bone) which can be often due to open fractures or other conditions. In cases of osteomyelitis, a periosteal reaction can happen, which may appear as localized laminated periosteal reactions on radiograph.
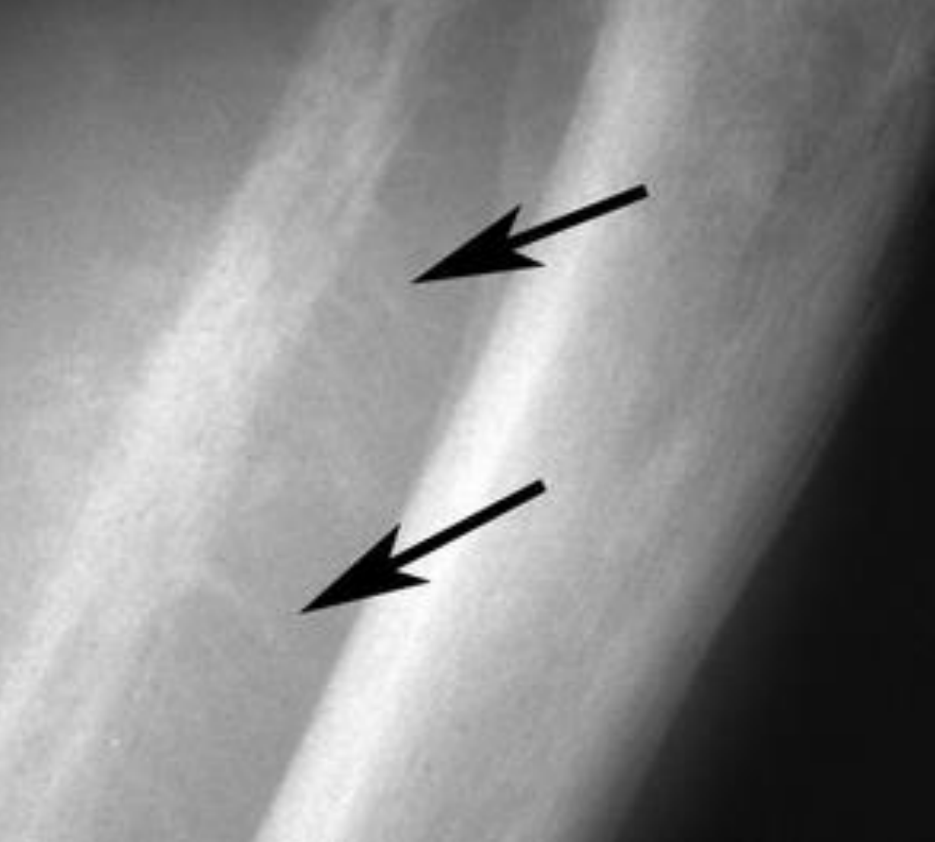
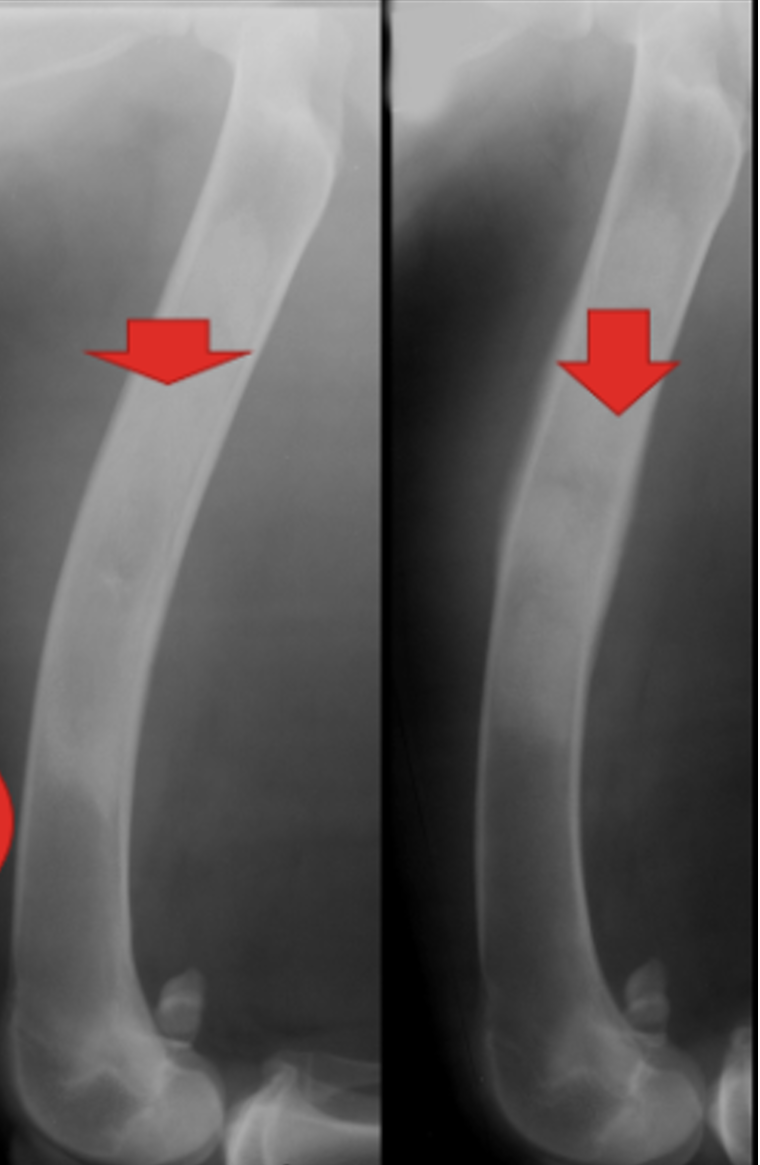
Which periosteal reaction is this?
hair-on-end periosteal reaction
Hair-on-end periosteal reaction is a characteristic radiographic finding associated with Ewing`s sarcoma (type of bone cancer).
Lateral radiograph of lower leg shows bony spicules emanating perpendicular to cortex (arrows).

Which type of periosteal reaction is this?
Palisade type of reaction - pattern of bone formation/periosteal reaction characterized by layered/organized arrangement of bone or periosteal tissue.
may resemple a onlionskin or lamellated pattern.
can be indicative of tumours or chronic inflammation.

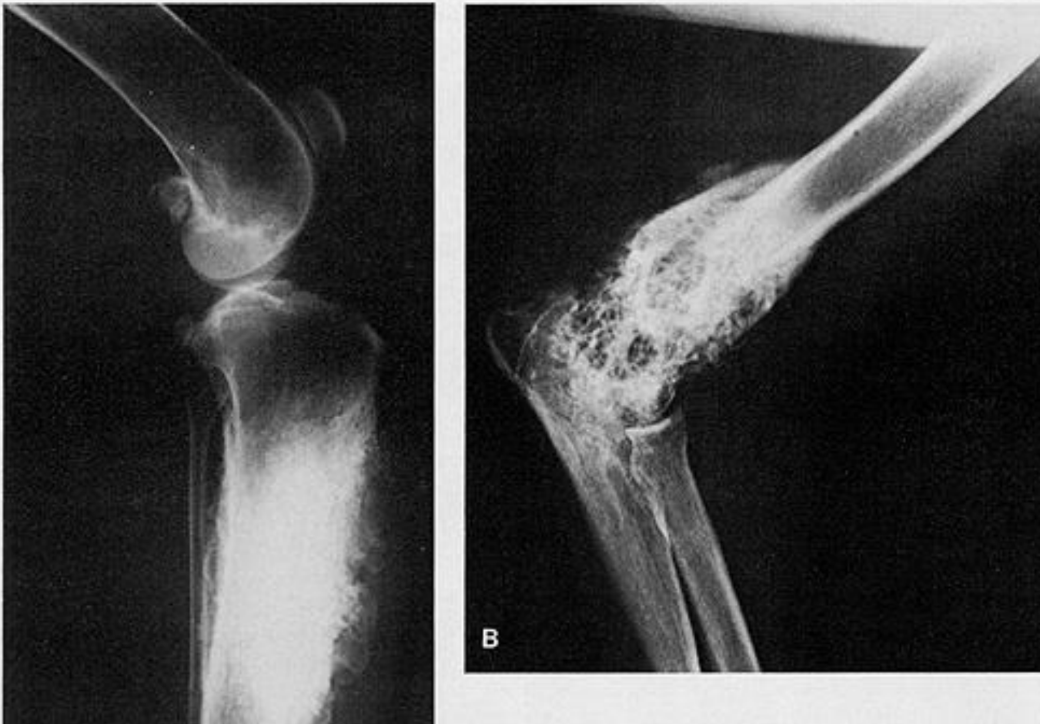
which periosteal reaction is this?
Sunburst and disorganized aggressive perosteal reaction on femur.
in second picture, we can see a very aggressive sunburst reaction.


which periosteal reaction is this?
Codman triangle

Hypertrophic Osteodystrophy (HOD) is?
A bone disease in fast-growing large and giant breed dogs, first presents between 2-7 months old.
marked by decreased blood flow to the metaphysis → failure of ossification → resulting in necrosis and inflammation of cancellous bone (spongiosis).
usually bilateral in limb bones.
Diagnosis: history, symptoms, physical exam with pain + swelling on growth plates and ex-rays.
X-ray: thin radiolucent (dark) line at metaphysis (growth plate) in end of ulna, radius or tibia.
bony inflammation and bone remodelling may be seen, fever + hgih WBC count.
Treatment: supportive, anti-inflammatories, painkillers (carprofen).


Hypertrophic osteopathy is?
rare condition that occurs as a secondary disease, often due to neoplastic or infectious masses in the thoracic cavity.
It can leads to the formation of new bone (periosteal reaction) on the outer surface of existing bones, particularly affecting the limbs, while the joints remain unaffected. Swelling and pain occur,
X-ray: irregular proliferation of periosteal new bone on fingers + small bones.
Hypertrophic osteopathy is a conditon which can lead to periosteal reactions as a part of its pathologic process. Important to note that periosteal reactions can happen in various conditions, not just hypertrophic osteopathy.The condition is secondary to underlying health issues, part. invl. thoracic cavity, so it can be triggered by a chronic lung infection for instance.
Nutritional Secondary Hyperparathyroidism
A condition resulting from a calcium-phosphorus imbalance, often seen in puppies fed a meat-based diet.
can result in lower bone density, pain, deformation and fracture

Early closure of growth plates on dog can be?
Early closure of growh plates in dog can be a bad condition. This premature closure can lead to complications, deformities like lateral valgus deformity, which affect limb distal to growth plate.
Can result also in subluxation of the elbow joint and incongruity in the elbow joint → dysplasia and arthrosis.
cause: trauma
Location: distal ulna, radius

Describe Panosteitis
A condition characterized by inflammation of the long bones, often seen in young, rapidly growing dogs, large breeds (5-12 month)
affects medullary cavity
radiopacity - incr. osteoblastic activity leads to denser bone formation in affected areas.
by palpation → pain
describe osteomyelitis
serious infection of the bone, often caused by bacteria, fungi → inflammation and necrosis.
can result from open fractures, surgery, or spread from nearby infections.
symptoms: localized pain, swelling, fever, chills
X-ray appearance - depends on whether it is acute or chronic:
acute: indefinite image, signs of inflammation (swelling) and possible presence of gas.
chronic: periosteal reaction, radiographic changes like increased radiopacity in marrow due to presence of sclerotic bone or sequestrum, which are avascular segments of bone that have died due to infection.

Tumours can be divided into?
Tumors → can be benign (only affecting one place) or malignant (affecting several)
Primary
from tissue where they are found
types: multiple myeloma in blood/bone marrow, chondrosarcoma in cartilage, osteosarcoma in bone, fibrosarcoma in CT
secondary
cancer that have spread from another part of body, through blood or lymphatic vessels.


Identify the type of tumour.
osteosarcoma.
we can see the appearance of “sunburst”, typical for osteosarcoma.


Identify the tumour.
Chondrosarcoma.
periosteal reaction can be present in various forms, like solid, lamellated, spiculated. Spiculated is most notable.
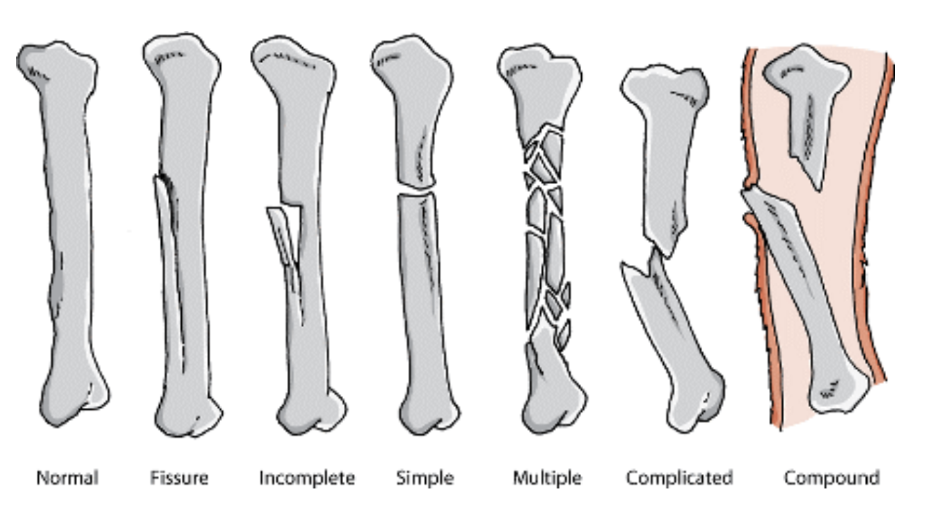
fractures can be what?
Closed
open
By location:
humerus
radius
femur
tibia
can be on proximal epiphysis, diaphysis and distal epiphysis.
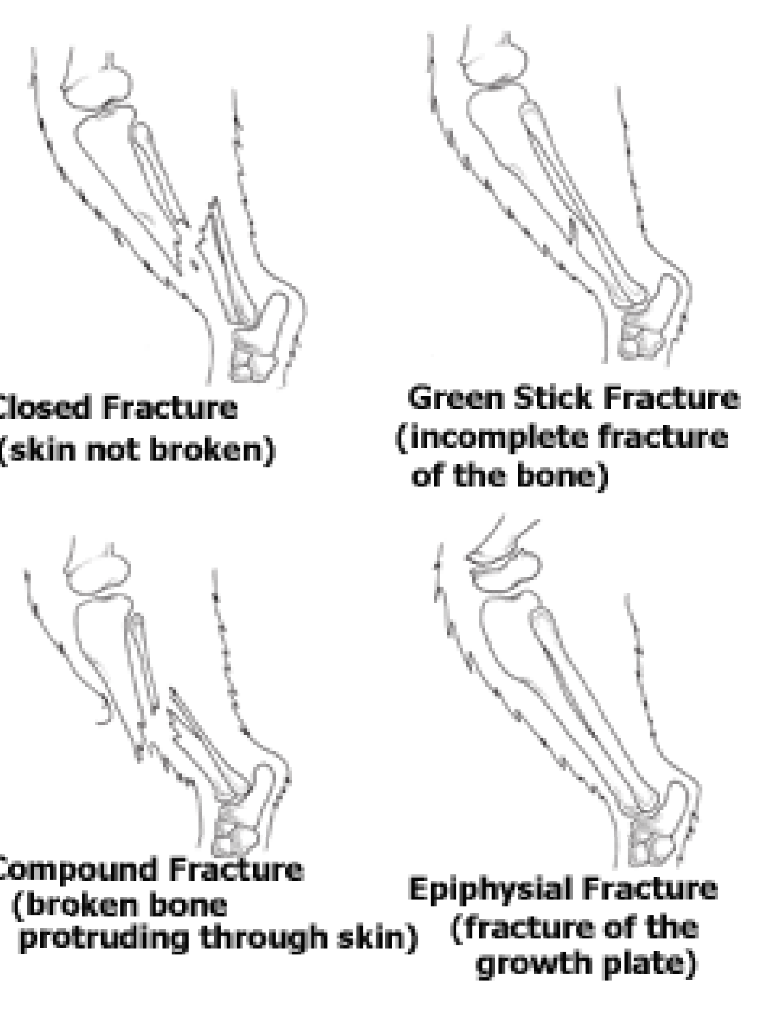
Types of fractures:
Linear fracture - parallel to bone`s long axis
Transverse - at right angle to axis
oblique - diagonal
spiral - min. one part of bone is twisted
fragments:
incomplete - bone fragments are partially joined
complete
comminuted - bone has been broken into several pieces
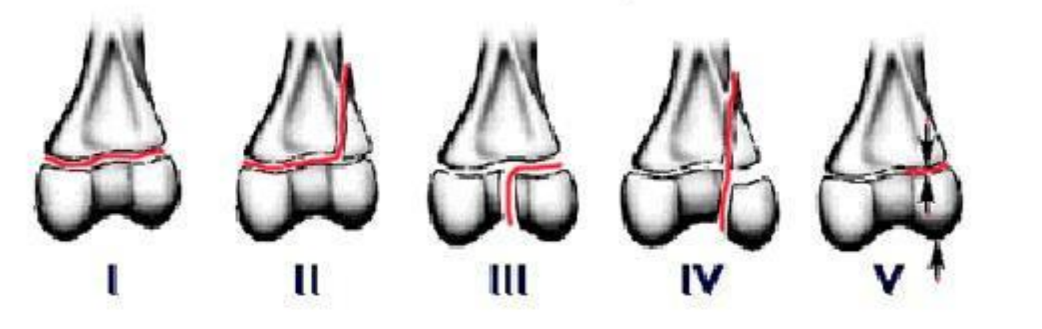
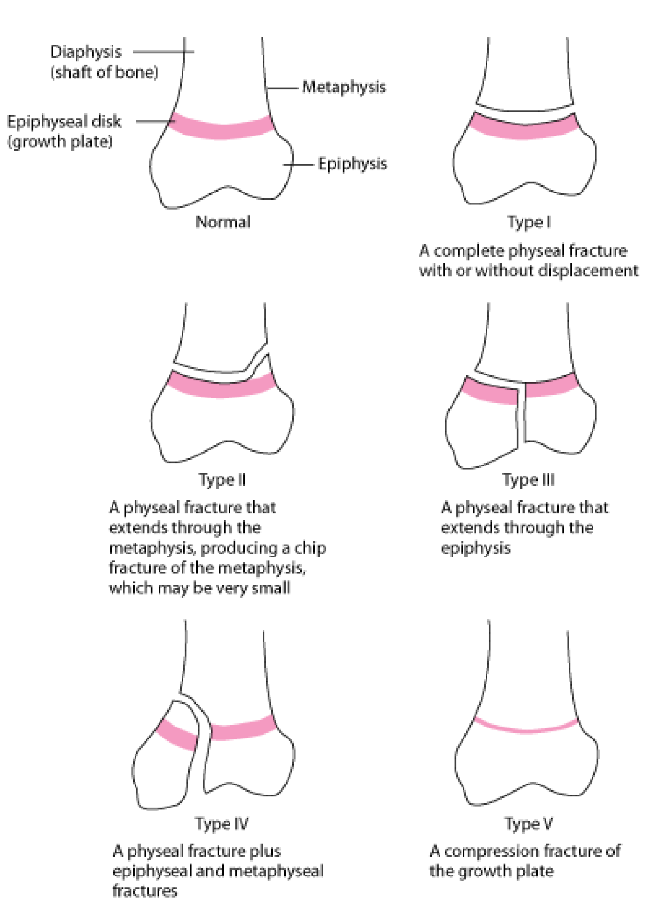
Fractures seen in young growing dogs can be classified into?
Salter-Harris classification
used to classify fractures in young growing dogs. Specifically adressing injuries to the growth plate (epiphyseal disc) and is crucial for understanding implications of such fracturs on growth and development of bones in young animals.
Types of fractures:
Type I: complete physial fracture with/without displacement
Type II: Physeal fracture, extending through metaphysis, making a chip fracture of metaphysis (small)
Type III: physeal fracture extending through epiphysis
Type IV: physeal fracture + epiphyseal and metaphyseal
Type V: compression fracture of growth plate

What condition can we see here?
hypertrophy osteopathy. severe.
hind limb

which condition is this?
osteosarcoma - tumour. (cancer)
primary bone cancer, from osteoblasts typically, occurs in long bones, around knee particularly, can be in young and adults, reveals a sunburst pattern on x-rays or mixed lytic and sclerotic lesion.

which condition is this?
Codman triangle (periosteal reaction) and can see sunburst pattern.
osteosarcoma

what type of condition is this?
incomplete fracture

What condition is on the left and right?
left: osteosarcoma (cancer of bone)
right: normal

what condition is this?
fracture, complete
location: pelvis, left side (opposite of our), on ala ossis illium

what condition is this?
complete fracture, displaced of humerus. medial-lateral taken.
Humerus diaphysis located.

what condition is this?
complete fracture. displaced, compound.

what condition is this?
fracture, incomplete, non-displaced.
Radiograph is? and what 3 quality properties does it have?
X-ray image is a 2-dimensional shadow summing a 3-dimensional object.
contrast (difference of density between tissues)
sharpness
truth of the image
what do we evaluate on the radiograph?
size, shape, position, surface, contours, structure of the organ
Radiography of bones shows?
highest radiopacity (bright)
only mineralised bone is visible
osteoid matrix of bone - soft tissue opacity
the osteoid (unmineralized component of bone) does not appear dense or opaque as the mineralized bone.
articular cartilago and invertebral disc shows soft tissue opacity
A good radiographic technique include?
highest definition film-screen
small distance bw. film and object
good collimation
no grid for small bodies
min. 2 orthogonal view or oblique position
stress radiograms - views taken while giving stress to a joint or structure
define lesions.
lesions → damage/abnormal change in tissue
describe these anatomical structures of bone.
cancellous bone
compact bone
medullary cavity
epiphysis
metaphysis
in between meta and epiphysis, we have physis
diaphysis
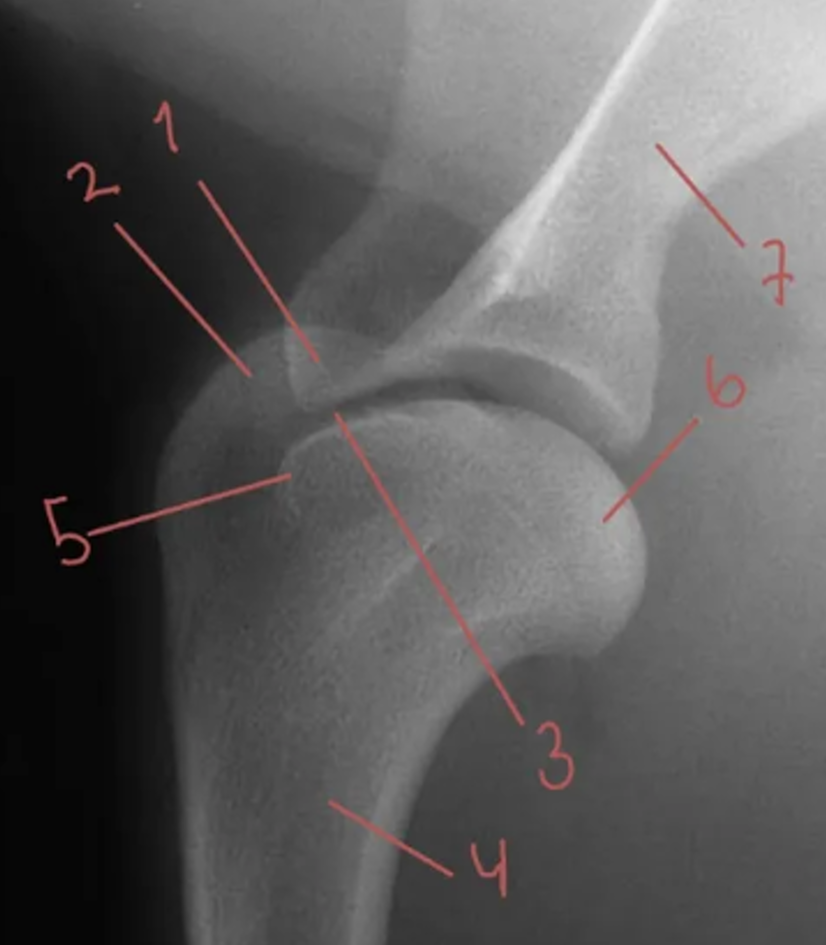
describe these parts of shoulder joint.
processus coracoideus of scapula
tuberculus majus of humerus
tuberositas scapulae
humerus
tuberculus minus
caput humeri
scapula
explain the terms: enchondral ossification and intramembranous ossification.
Enchondral ossification and intramembranous ossification are two distinct processes by which bone tissue forms in the body.
Enchondral ossification: process of bone developing from cartilage.
forming long bones + involving replacement of hyaline cartilage with bone tissue.
happens during fetal development and continues as growth plates (physes) closes.
stages: formation of cartilage template, growth of cartilage, calcification, eventual replacement by bone → development of diaphysis and epiphysis
Intramembranous ossification: happens directly from mesenchymal tissue (no cartilage stage)
for flat bones, like skull and clavicle.
mesenchymal cells → osteoblast → makes bone matrix.

what do we see here?
elbow growth
condylus distalis humeri
epicondylus medialis
proximal radial epiphysis
processus anconenus
what are the 2 responses of bone to disease or injury?
bone loss (osteolysis)
osteoporosis (reduced mineral components and osteoid (bone matrix) in adult dog)
osteomalacia (insufficient mineralisation of the organic osteoid in young dog)
focal bone loss patterns (neoplasia)
osteosarcoma - form of osteolysis, type of malignant neoplasia → bone loss.
bone production (hypertrophy)
sclerosis
bigger trabeculae
superimposed periostal or endostal reaction

what are the 2 main groups of periosteal reaction?
periosteal → new bone formation, 7-10 days post-trauma. Young ones are more sensitive.
continuous: steady formation of new bone, slows disease process, inform radioopacity, non-aggressive and low grade.
interrupted: fluctuating response
what are the various types of periosteal reactions?
onion skin-laminar
lamellar/linear: with callus formation, metabolic disease or irritation
sunburst: malignancy or osteosarcoma
codman`s triangle: elevation of periosteum due to bone tumor → subperiosteal new bone formation.
palisade-like: in hypertrophic osteopathy (condition with underlying diseases like lung tumors, periosteum reacts to the irritation/inflammation => palisade-like) and sometimes in osteomyelitis (infection of bone causing the periosteum to react)

Lesions can cause changes, what are these?
Generalised or diffuse changes: Metabolic or nutritional changes, Neoplasia
Focal lesions: Congenital or developmental changes, Trauma, Infection, Inflammation
what are the common disease conditions of bone?
diseases of the bones include:
Fractures - Breaks in the bone that can occur due to trauma or stress.
Periostitis - Inflammation of the periosteum, the tissue surrounding the bone.
Osteomyelitis - An infection in the bone, often caused by bacteria.
Retained growing plate - A condition where the growth plate does not close properly, affecting bone growth.
Bone tumors - These can be benign, such as bone cysts, or malignant, including osteosarcoma, chondrosarcoma, and fibrosarcoma.
Osteolysis - The process of bone loss or destruction.
Metabolic diseases - Conditions that affect the metabolism of bone, potentially leading to disorders.
Osteodystrophy - Abnormal bone development often associated with metabolic issues.
Hypertrophic osteopathy - A condition characterized by the proliferation of bone tissue, often linked to underlying diseases.
Panosteitis - A painful inflammation of the long bones, commonly seen in young dogs.
Rickets - A disease caused by vitamin D deficiency, leading to weakened bones.
what is salter-harris?
types of fractures of the physis in growing dogs can be classified according to salter-harris.
type I: complete physeal fracture
type II: fracture through metaphysis
type III: fracture through epiphysis
type IV: physeal fracture plus metaphyseal fracture.
type V: compression fracture of growth plate

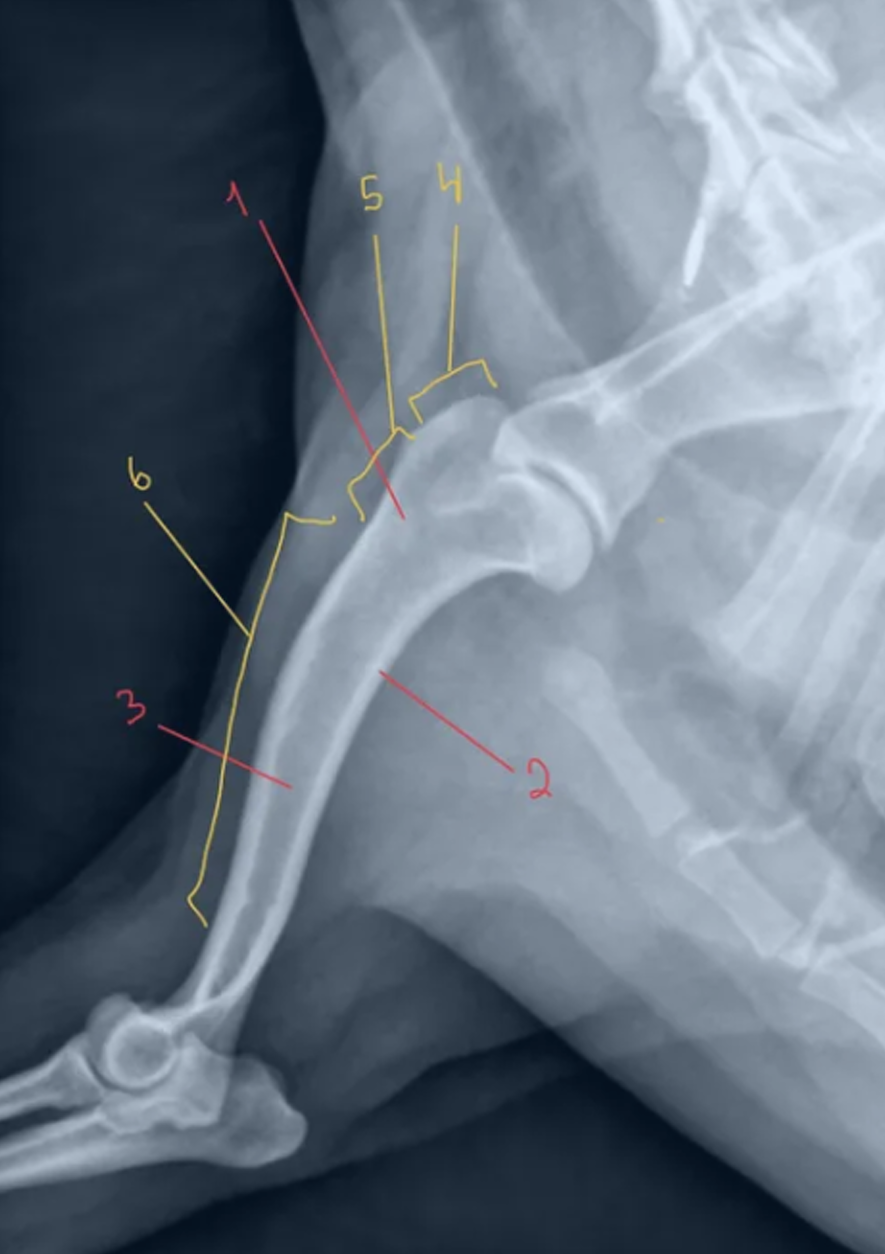
In a radopgraphic protocol, we need to include?
location, type, displacement of fragments, evaluate bone density (pathological fractures), intraarticular fractures, presence of foreign material, soft tissue injuries
Picture:
what: fracture of humerus
how: transversal, sharp fracture line
where: diphyseal fracture
dislocation of the fracture ends.
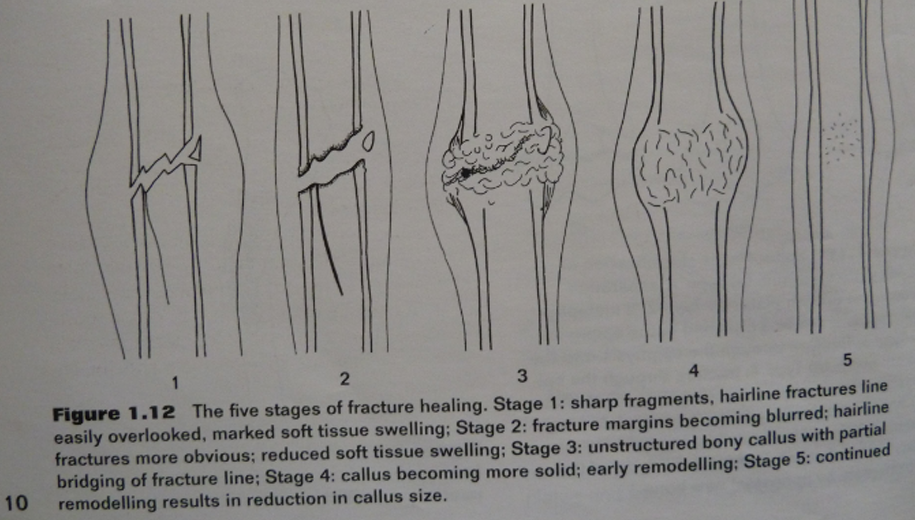
The difference of primary and secondary bone healing.
primary: when there is perfect anatomical alignment of bone ends, direct contact without callus
secondary: sharp fracture ends, fracture line blurred, unstructured bony formation, remodeling, reduction of callus.
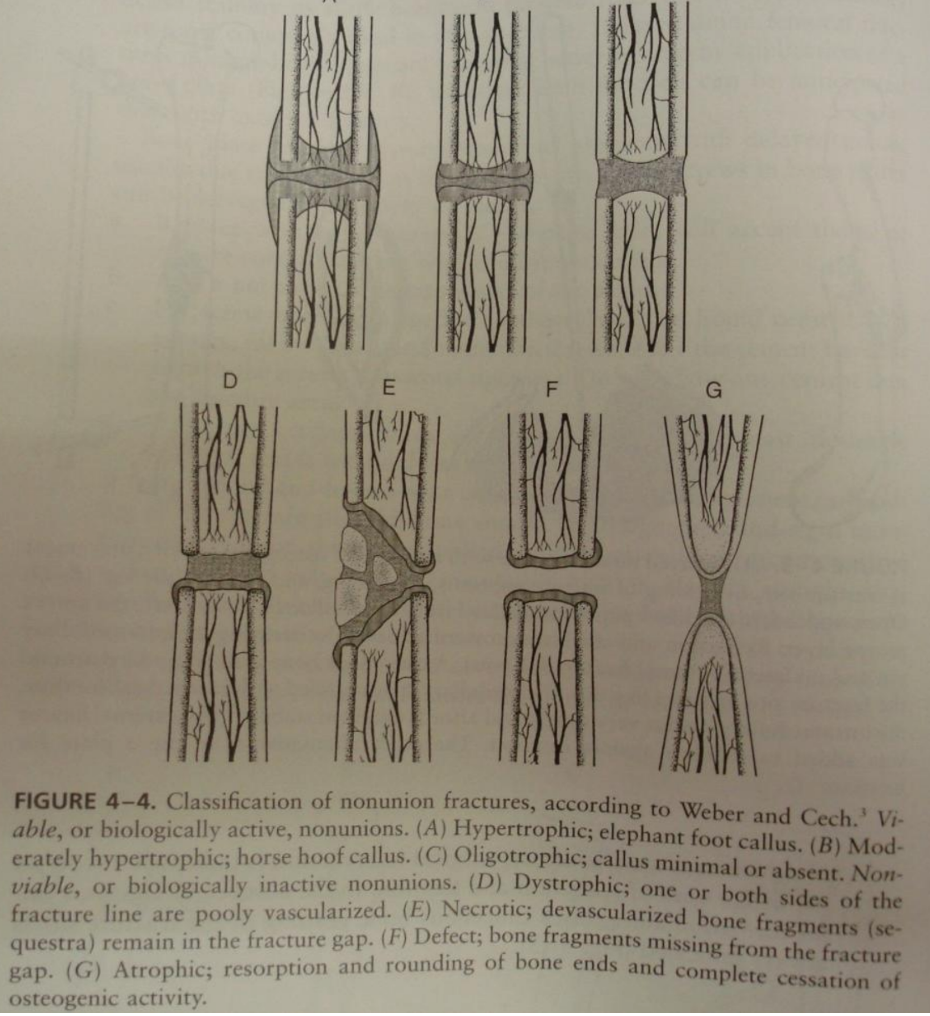
Weber-cech classification is of?
Non-union fractures - categorizes non-unions based on their bio activity and characteristics of fracture site.
viable (biologically active)
hypertrophic - “elephant foot” callus
moderately hypertrophic - “horse hoof” callus
oligotrophic - minimal/absent callus
non-viable (biologically inactive)
dystrophic - poorly vascularized bone fragments remain in fracture gap
necrotic - devascularized bone fragments present
atrophic - resoprtion + rounding of bone ends - severe lack of healing

what is this?
premature closing growing plate on ulna.
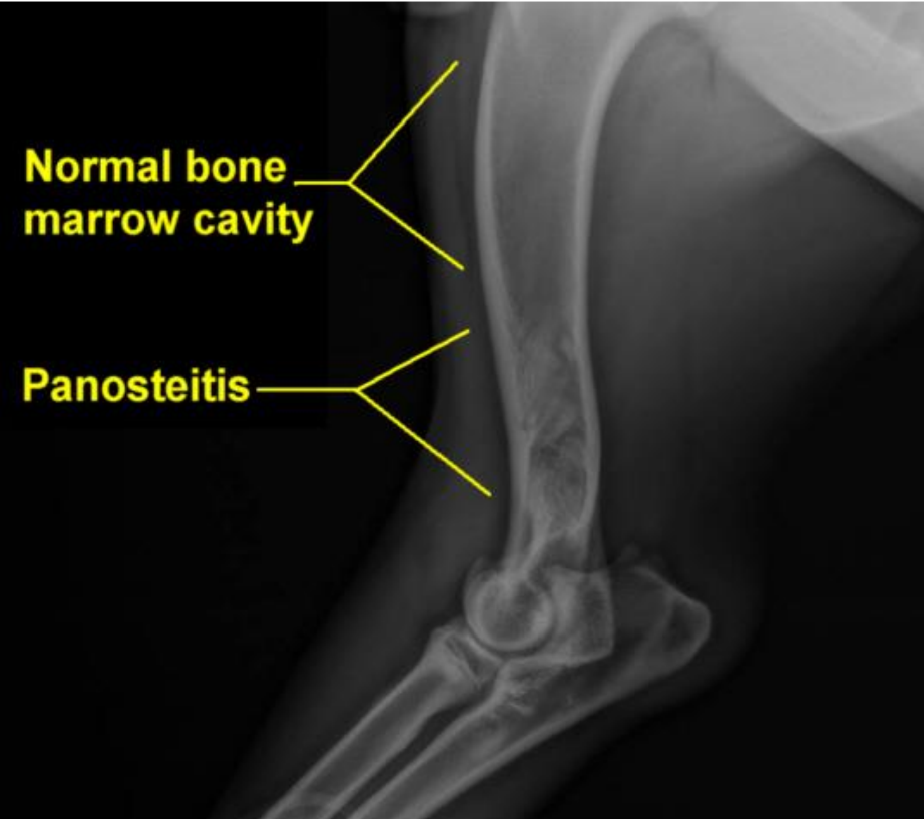
what is this?
panosteitis - incr. medullary radio-opacity, smooth periosteal reaction.

what is neoplasia?
Neoplasia refers to the process of abnormal and uncontrolled cell growth, the formation of tumor.
These tumors can be benign (non-cancerous) or malignant (cancerous).
bone cyst (benign neoplasia) is seen in the picture.
Characterize bone, its main components and function
Bone is a hard tissue primarily composed of hydroxyapatite, calcium hydrogen phosphate, and calcium carbonate
provide strength and structure.
functions:
support, protecting organs
for movement by serving as attachment points for muscle
storing minerals and housing bone marrow for blood cell production.
responsible for calcium homeostasis. Stores and releases Ca as needed.
Characterize osteocytes, osteoblasts and osteoclasts.
Osteocytes: maintains bone tissue (release of mineral phase of bone tissue) and regulates Ca levels.
osteobasts: making bone matrix and facilitating the mineralization process → synthesizing new bone.
osteoclasts resorb bone tissue, by breaking down the mineral matrix and collagen.
What comprises up to 65% by weight of bone?
Mineral constituents.
What is the structural difference between compact and spongy bone?
Compact bone has a dense structure that resists pressure. Contains havers system.
spongy bone has a sponge-like structure that supports movement. Does not have havers system.
The types of bone formation include?
Intramembranous ossification
happens directly within a layer of mesenchyme. Forms flat bones (skull ex.), where osteoblast → mesenchymal cells → secretes bone matrix. It allows for development of bone without a cartilage model, involving direct formation of bone tissue.
Endochondral ossification
replacement of hyaline cartilage with bone tissue, forms long bones, where cartilage model is first made, then gradually becomes replaced by bone as ossification progresses.
what is bone remodeling?
Continuous process involving the resorption of old bone and formation of new bone → for maintenance and repair of bone tissue.
Regulated by hormones like parathyroid hormone (PTH) and calcitonin, mechanical stress on the bones and actions of osteoblasts and osteoclasts.

name components.
epiphysis - first arrow
growth plate
metaphysis
diaphysis
What type of joint allows for free movement?
Diarthroses - two bone ends covered with articular cartilage, synovial fluid. ex. shoulders, knees.
what type of joint are relatively rigid?
synarthroses.
Fibrous joints, cartilaginous joints and synovial joints are?
fibrous → syndesmosis, ex. connection bw. tibia and fibula.
cartilaginous → synchondrosis ex. epiphyseal plates in growing long bones and symphisis, ex. pubic symphysis
synovial (allows for a wide range of motion) → ex. hinge joints like the elbow and knee, ball-and-socket joints like the shoulder and hip.
Articulatio simplices vs. compositae?
Art. simplices → consist of two bones ex. joint between humerus and radius.
Art. compositae → consist of 3 or more bones, or 2 bones and articular disc or meniscus. ex. knee joint (femur, tibia and patella)
What are the components of the periosteum?
Outer fibrous layer and inner osteogenic layer.
What is the role of the nutrient artery in bone health?
It nourishes the bone marrow and is crucial for the health of the bone.
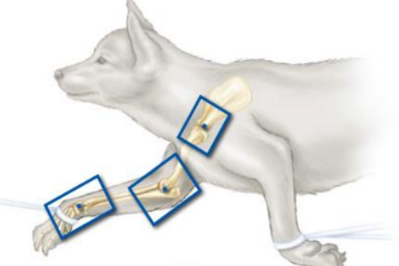
which position is this?
lateral shoulder, limb to be examined must be down and extended cranially and ventrally. Pull opposite limb caudally and ventrally (not over back).
lateral elbow
lateral carpus
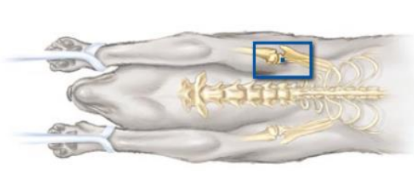
which position?
caudocranial shoulder.
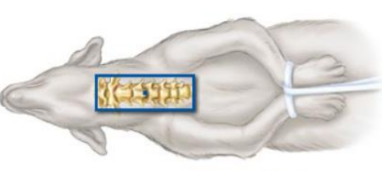
which position?
ventrodorsal position of cervical spine
which position?
craniocaudal elbow, dorsopalmar carpus
Canine Elbow Dysplasia (ED)
A condition involving multiple developmental abnormalities of the bones in the elbow joint, primarily affecting large and giant breed dogs, from 5 months (4-6 months).
causes pain and lameness, both fore legs.
arthrosis can be a result of various abnormalities assiciated with ED. It can be a consequence of the conditions affecting the elbow joint.
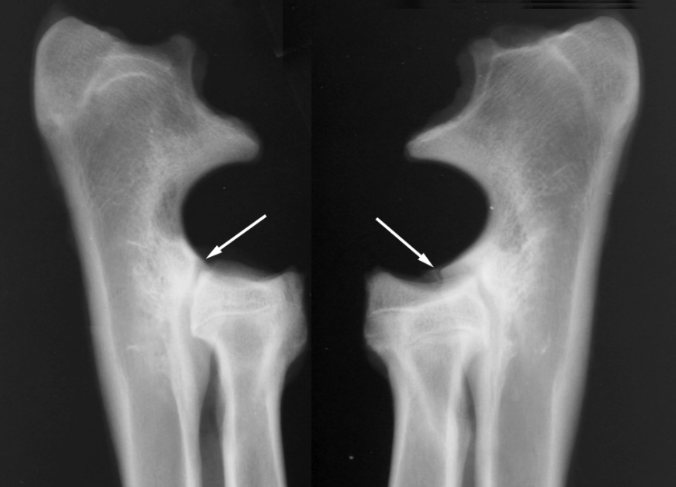
Arthrosis
A degenerative joint disease that results from abnormal development in the elbow joint, often leading to lameness.
right picture is arthrosis, left is healthy.
osteochondrosis
Disorder characterized by the failure of enchondral ossification and the maturation of growth cartilage.
Can happen on growth paltes on the epiphysis of long bones and on joint surfaces of heads.
involves irregular arrangements of chondrocytes, chondrocyte necrosis, loss of proteoglycans from cartilage matrix, leading to decreased elasticity of the cartilage → prone to fissures and may separate from the subchondral bone.
What is the leading cause of forelimb lameness in dogs?
elbow dysplasia (ED): from abnormal bone growth and development.
condition includes diseases of the elbow joint, like:
fragmented coranoid process (FCP) - fragment of medial coranoid process of ulna → joint incongruity
osteochondrosis (OC) and/or osteochondritis dissecans (OCD)
ununited anconeal process (UAP)
joint incongruency - joint surfaces do not fit together properly, often due to asynchronous growth of the radius and ulna.
Occurrence of Canine elbow dysplasia and diagnosis.
occurrence: more males, most intensive development and growth is bw. 4-6 months of age, symptoms show at 6-8 months.
x-ray confirmation of the diagnosis after the end of growth, CT.
in what 3 joints can ED be seen?
radio-ulnar
humero-radio
humero-ulnar

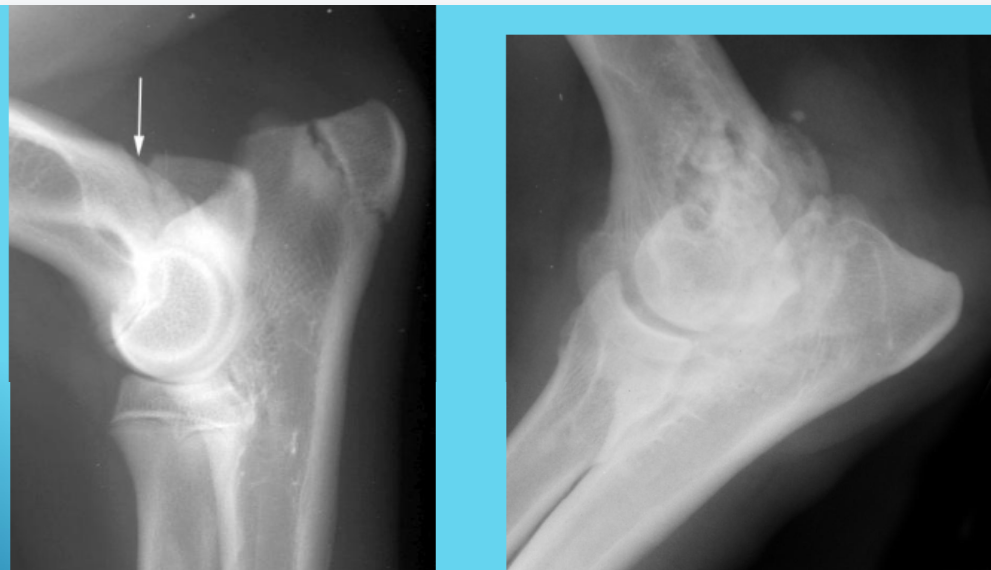
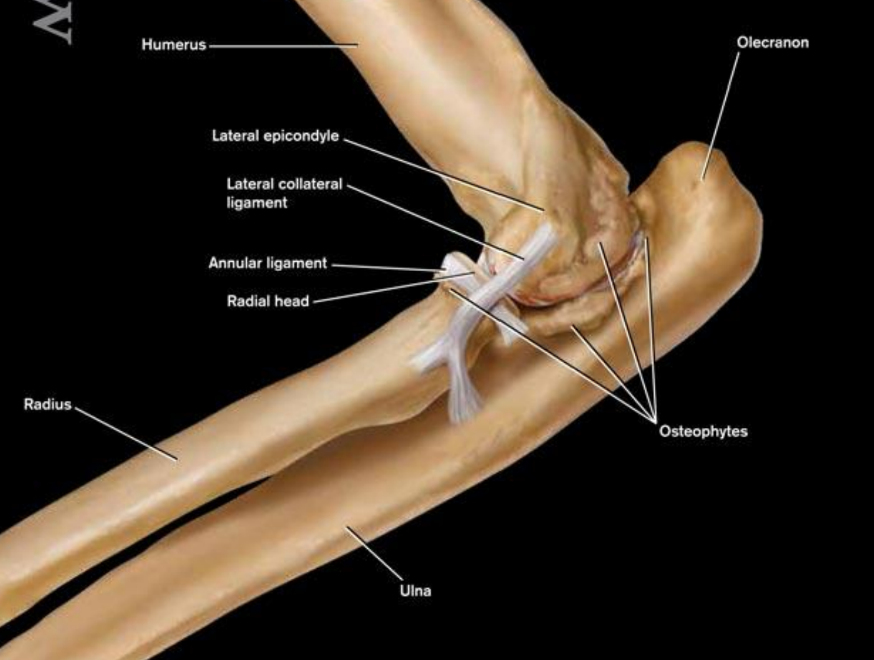
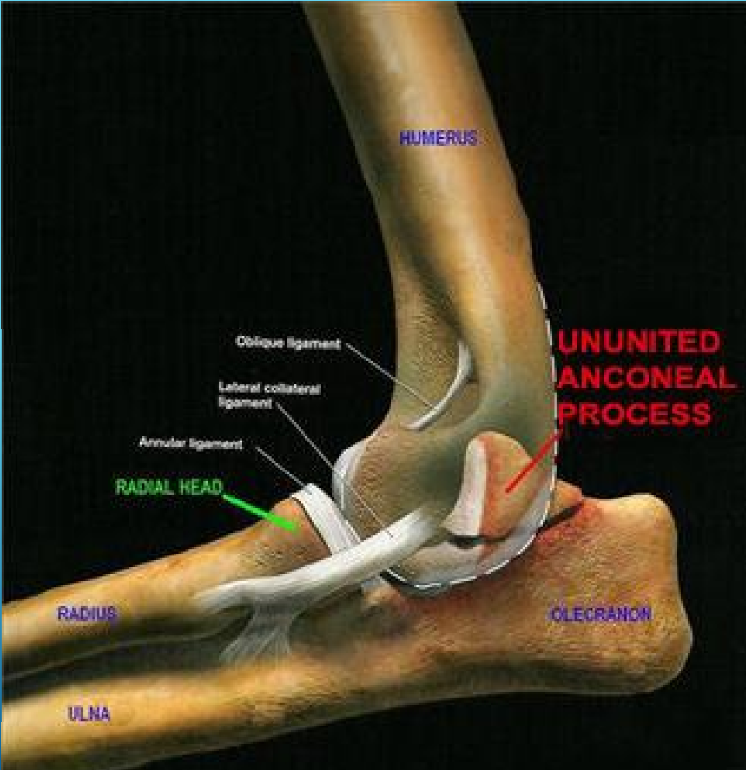
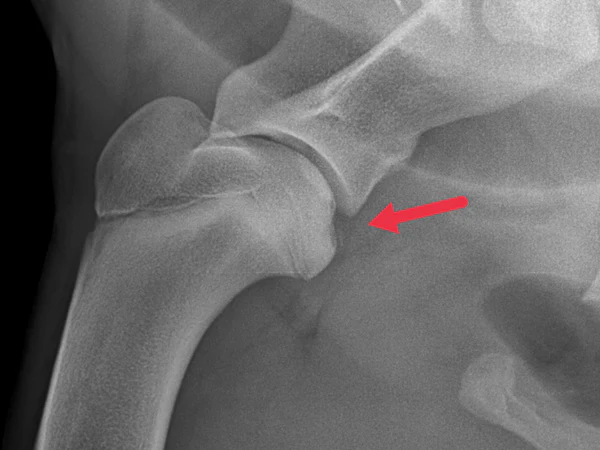
this is?
Ununited anconeal process (UAP)
characterized by a failure of the anconeal process of the ulna to fuse with the ulna, typically seen in dogs. We will see a separate bone fragment at the anconeal process, which is located at the proximal ulna.
Key features are: separation, osteophyte formation, joint changes and soft tissue swelling.
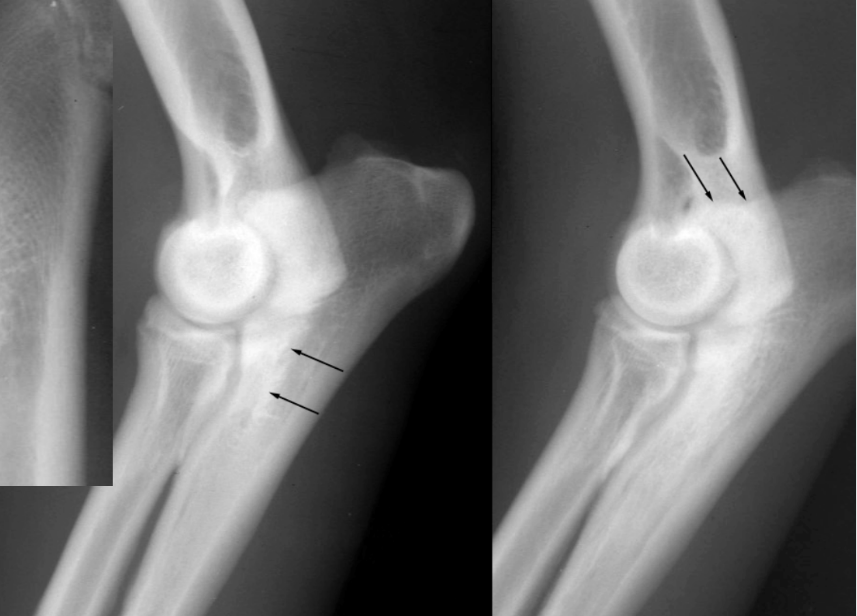
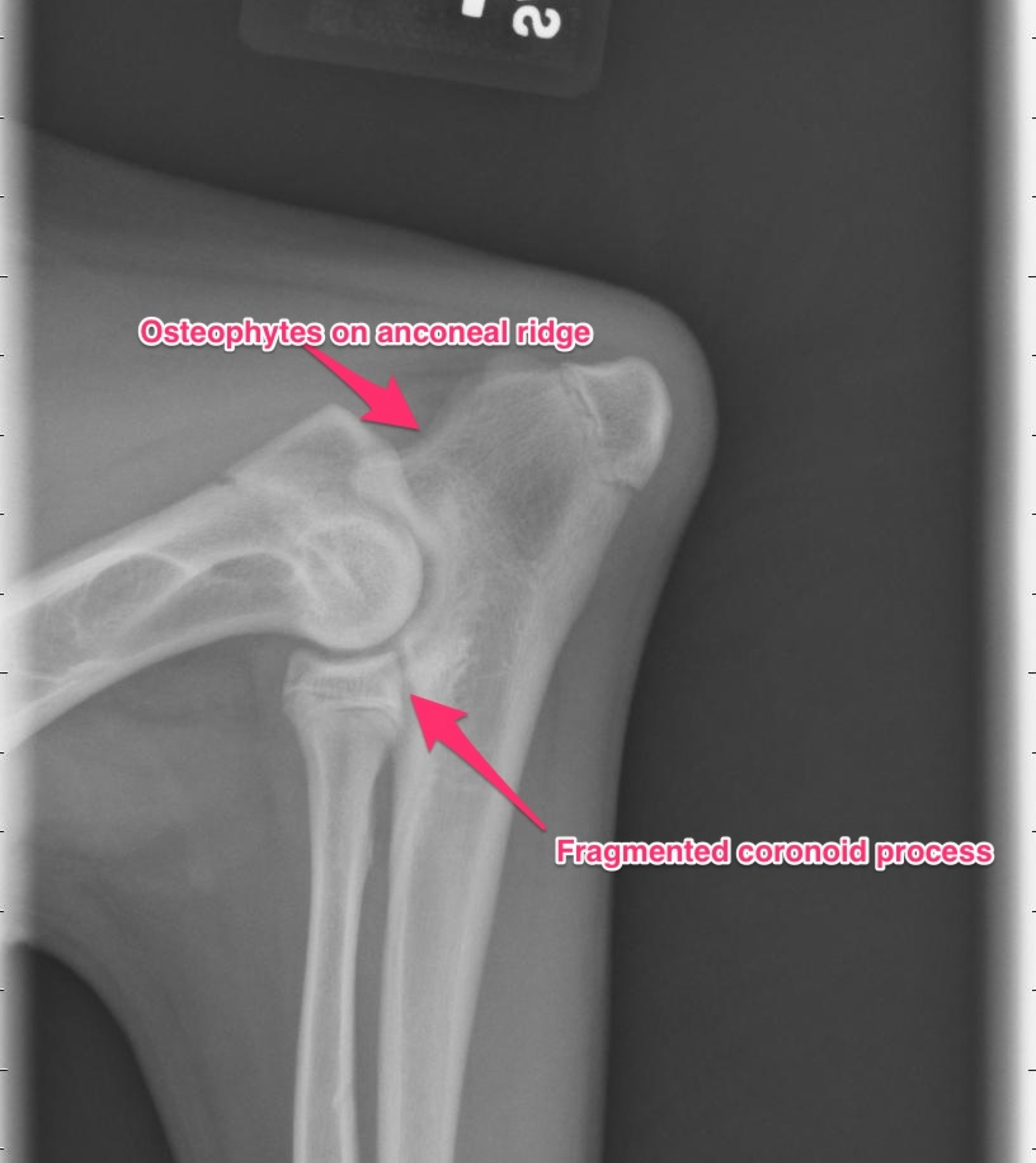
what is this?
fragmented coranoid process (FCP)
presence of fracture or irregularity in the processus coranoideus of ulna.
fragment size: rice, corn, fragment has three forms - loss of the tip of coranoid processus, fragmentation at the junction of ulna and radius, fissure or erosion on articular cartilage.
key features: fracture line, fragmentation, soft tissue swelling, joint alignment, associated inuries.
clinical signs: more males, 50% not lame at young age, lameness only after damage of articular cartilage, excess body weight.

what is this on the medial condyle of humerus?
Osteochondritis dissecans (OCD) - osteochondrosis
clinical form of osteochondrosis (disorder affecting cartilage + bone)
in this, cartilage thickens but fails to ossify correctly, meaning it does not turn into bone as it should.
often assoicated with joint incongruity and FCP
disorder of enchondral ossification, disruption lead to development of lesions in the cartilage → can result in detachment of bone and cartilage fragments.
the condition may result in a joint mouse (small fragment of cartilage/bone that becomes loose within a joint space)

what is this?
incongruency
mismatch/misalignment between the surfaces making up the joint, which leads to joint dysfunction or pain.
relevant in the evaluation of joint disorders, like osteoartiritis or post-traumatic changes.
characterization: difference in joint space witdth between the two sides of a joint, bone alignment difference, sclerosis, cyst formation, osteophytes (bone spurs), irregularities.
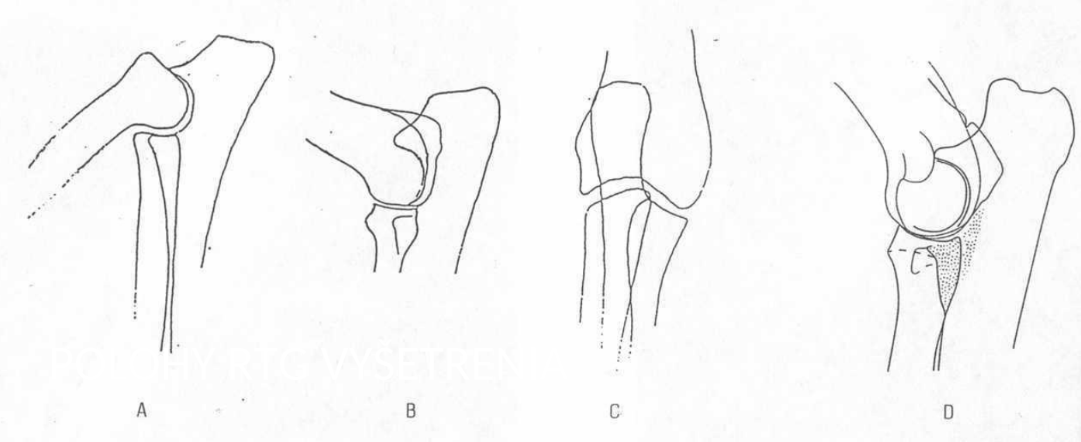
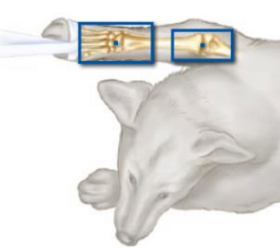
The different joint positions during radiography diagnosis of ED
A: M-L projection: 45
B: M-L projection: 95
C: D-P projection
D. M-L projection 120