Module 1 Healthy Animals
1/167
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
168 Terms
What are the functions of epithelium?
to protect tissue underneath from desiccation (removal of moisture), pathogens, and physical trauma, to regulate and exchange molecules, and to secrete hormones into vascular systems and other substances delivered by ducts.
What are the common features between epithelial types?
number of layers of cells, shape of cells, functions, and surface modifications
What does basolateral mean?
surfaces of cell that faces away from lumen or outside area
How is epithelium classified in terms of cell layers?
simple = one layer or stratified = more than one layer, or pseudo stratified = seems stratified because nuclei are at different levels
What are the differences between glandular and non-glandular epithelium?
glandular epithelia are solid tissue structures while lining epithelia covers free surfaces of the body & cavities
Holocrine
death of entire cell within gland that releases content into lumen
What are some modifications of epithelial cells and what are their functions?
microvilli are for used for the absorption of molecules (smaller than cilia, can only see banding on stains) while cilia assist in movement over epithelial surface
What is the difference between a desmosome and hemidesmosome?
desmosomes attach cells to each other while hemidesmosomes attach epithelial cells to basement membrane
How is epithelium classified according to cell shape?
squamous = wider than long, cuboidal = same width as length, and columnar = longer than wide
Urothelium
specialized epithelial lining that covers the urinary tract (bladder, ureters, and renal pelvis)
What is cornification?
layer of dead cells filled with keratin that form protective barrier
What is the function of connective tissue?
provide structural and mechanical support for tissues and to mediate exchange of nutrients and waste between circulation and tissue
What are the differences between ground substance, collagen and elastic fibers?
ground substance is an aqueous gel of glycoproteins and proteoglycans that occupies space between elements of connective tissue, collagen fibers are inelastic, have great tensile strength and require collagen, and elastic fibers are composed of elastin, dense and regular tissue
What are the cellular components of connective tissue?
contains protein fibers, glycoproteins, proteoglycans, and fibroblasts
What are the differences between embryonic and fibrous connective tissue?
embryonic connective tissue is only located in embryonic tissue and is very delicate
What is collagen and how is it composed?
precursor molecule of connective tissue, makes larger chains called fibrils that make up fibers that make up bundles
What are the two types of adipose tissue?
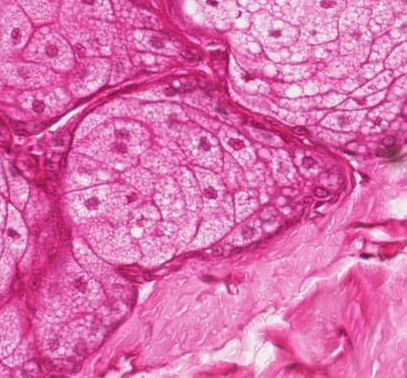
white adipose is specialized of the storage of triglyceride and serves as a energy source and insulator while brown adipose tissue is highly specialized for temperature regulation and is highly abundant in newborns and hibernating mammals
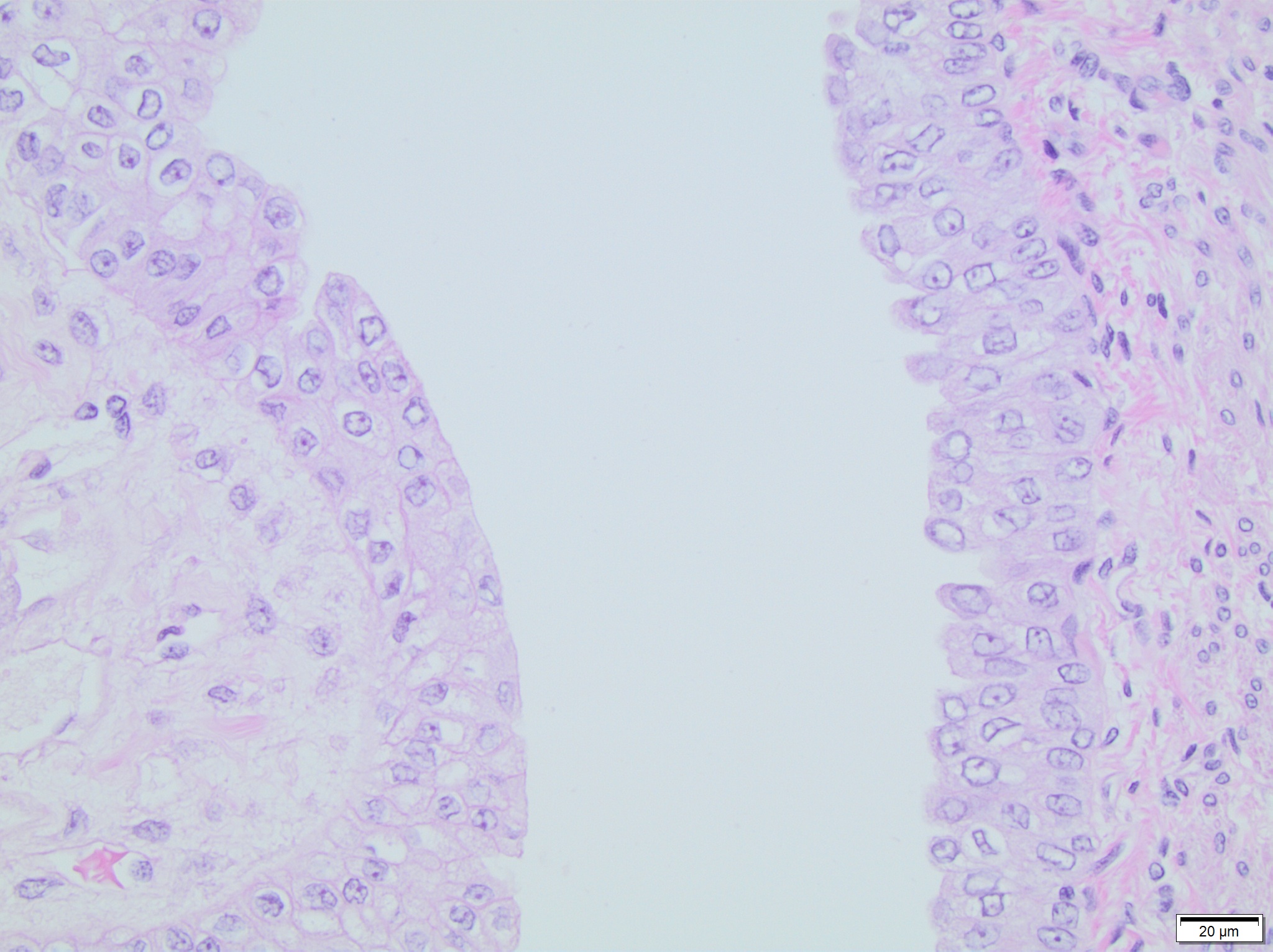
What are the three major types of cartilage and what anatomical locations are they present?
Hyaline cartilage is composed of type 2 collagen and makes up articular structure of joints, fibrocartilage is made of type 1 collagen and is located where tendons attach to bones and elastic cartilage is made of type 2 collagen and located in pinna of ear
What are the major organic and inorganic constituents of bone?
organic = type 1 collagen and ground substance (osteoid) and inorganic = calcium hydroxyapatite (adds rigidity)
Osteoblast structure and function
contribute to bone production by synthesizing osteoids. plump, angular cells and can become osteocytes
Osteocyte structure and function
small elongated cells contained within lacunae, role in detecting changes and calcium homeostasis
Osteoclasts structure and function
multinucleate cells that reabsorb bone
What are the anatomic structures that facilitates communication between osteocytes?
canaliculi
Explain the basic process of osteoclastic resorption, naming one important stimulus for resorption?
osteoblasts release collagenases that reabsorb non-mineral lamina laminates
osteoclasts bind to exposed mineralized bone
carbonic acid secreted across osteoclast resorbs mineral and matrix is dissolved
What is the difference between osteoid and bone?
osteoid is the organic precursor to harden bone that is synthesized by osteoblasts
What is the difference between woven and lamellar bone?
woven bone is randomly arranged fibers (occurs during injury) and is very fragile while lamellar is normal adult bone that is arranged in dense parallel arrays
What is the difference between cancellous and compact bone?
cancellous or trabecular bone is multi-directional struts that reflect loading patterns and compact bone is dense bone that forms cortex
What is an osteon?
osteons are the functional unit of bone that is a long cylindrical structure with center that contains nerves, blood vessels, and osengenic cells
What does the term modeling mean in term of bony tissue?
Modeling is the change in size and shape of bone that responds to loading and abnormal use
What does the term remodeling mean in term of bony tissue?
Remodeling is when bone is removed from one area and replaced in another. The steps are as followed: activation, osteoclastic resorption, reversal, and formation
List two instances where bone remodeling plays an important role in NORMAL bone function
Critical during normal cortical growth as woven bone is replaced by osteonal bone and is important for repairing ‘wear and tear’
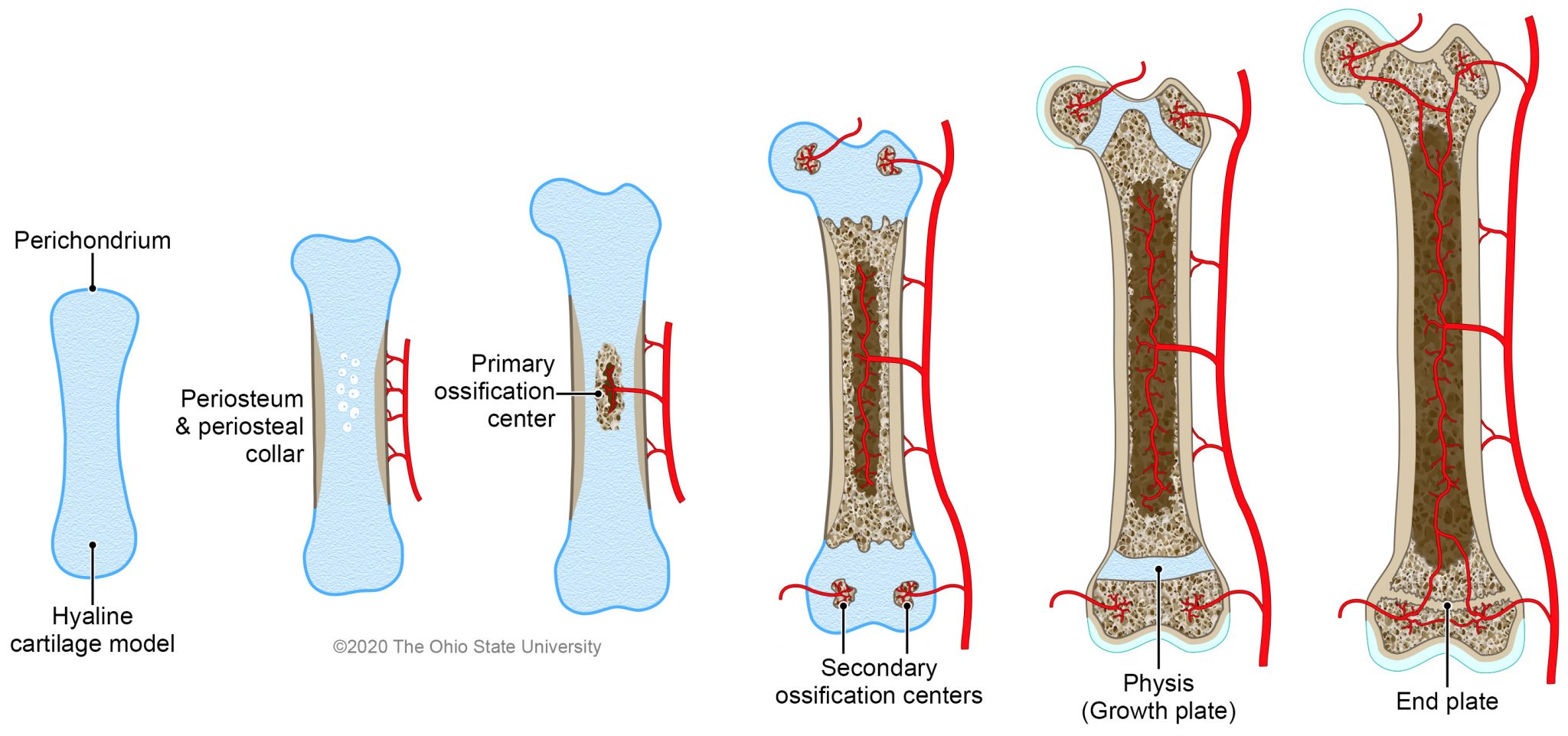
What does the process of intramembranous ossification involve? Where does it occur?
this type of ossification mainly occurs in flat bones and begins as condensation of primitive mesenchyme and differentiate into osteoblastic phenotype. is formed by apposition (on top of bone that just formed) and there is no cartilage intermediate
What does the process of endochondral ossification involve?
endochondral ossification is in long bones and has a cartilage model that becomes almost entirely replaced. This type of ossification grows interstitially (inside matrix). The articular-epiphyseal complex (AEC) is where ossification occurs at a secondary center beneath articular surface. The three processes are as follows: mineralization of cartilage surrounding chondrocyte, death of chondrocyte and vascular ingrowth.
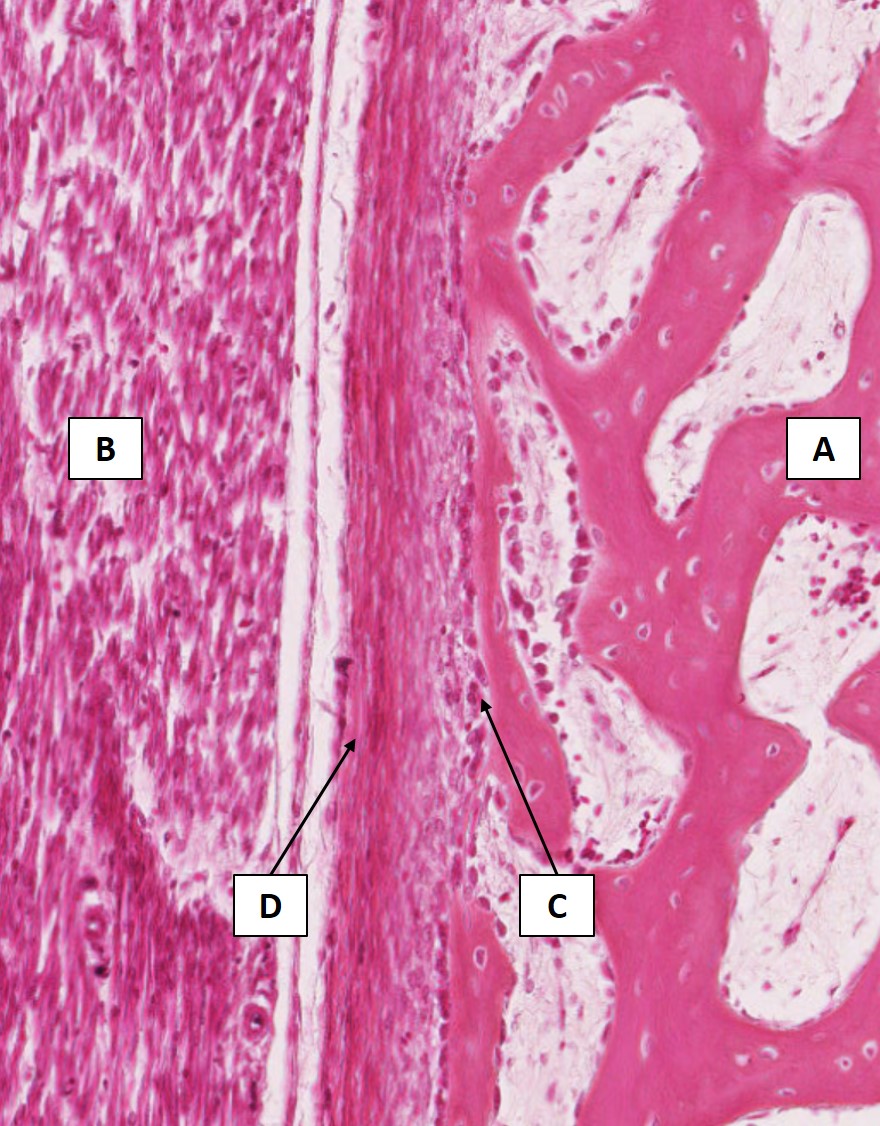
At which location is active endochondral ossification occurring?
d
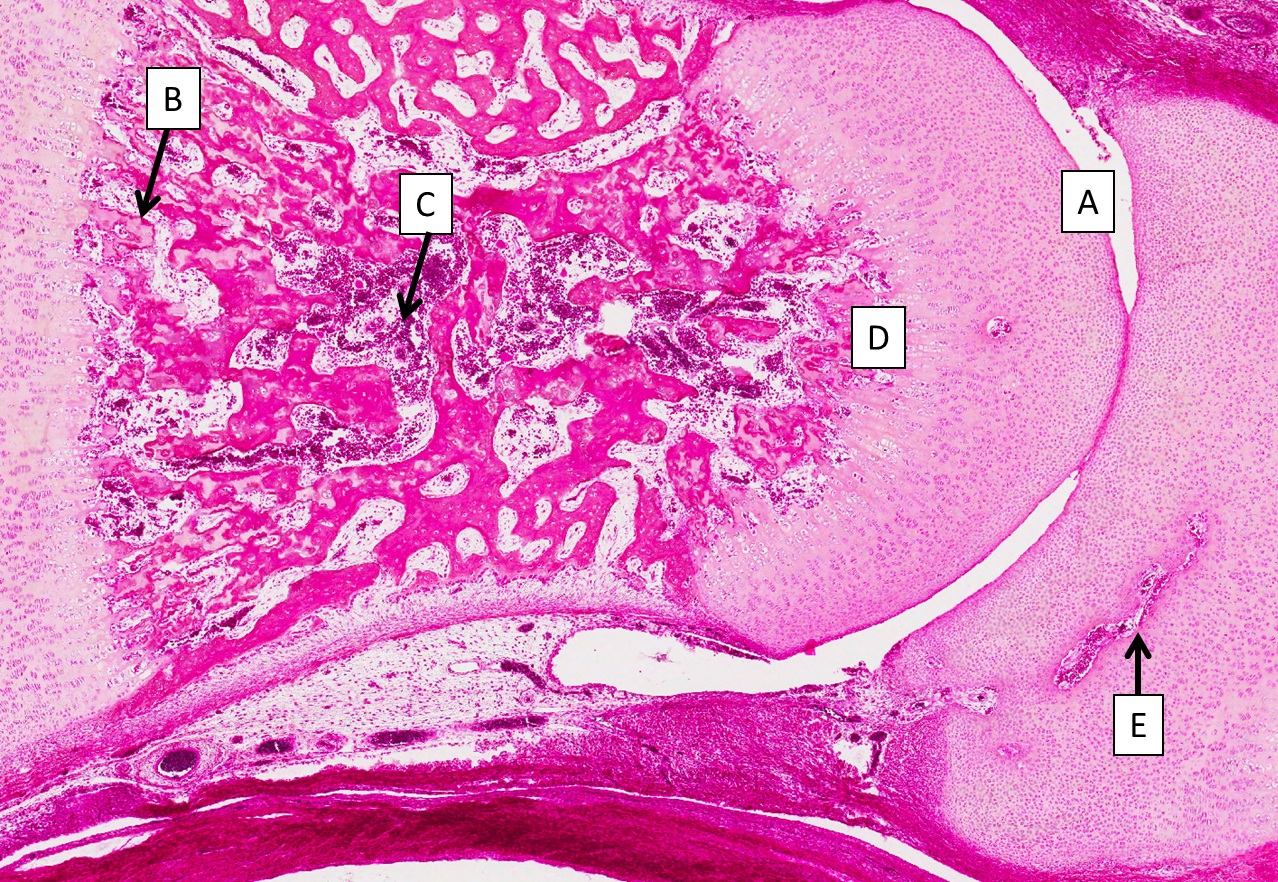
zone of hypertrophy
to the left of c
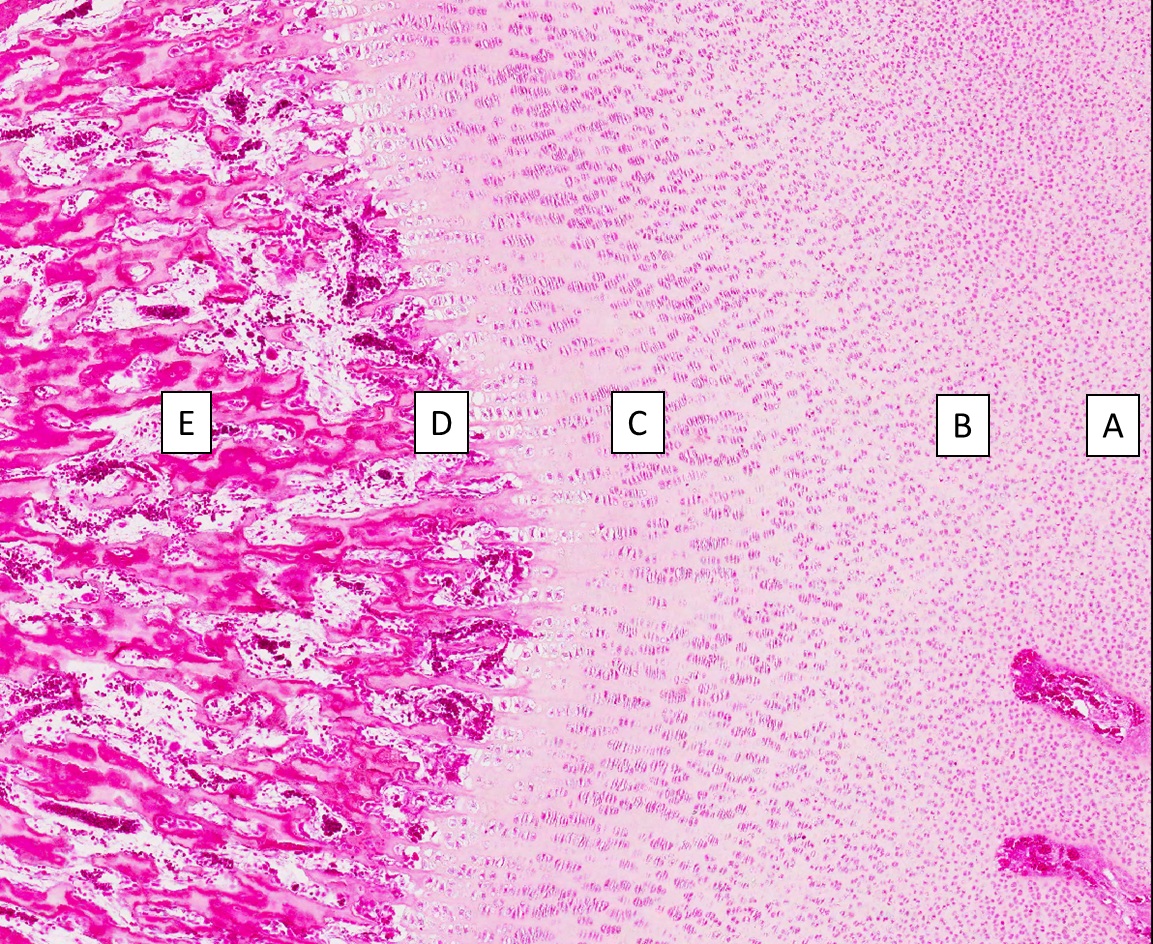
Which is the osteogenic layer of the periosteum?
c
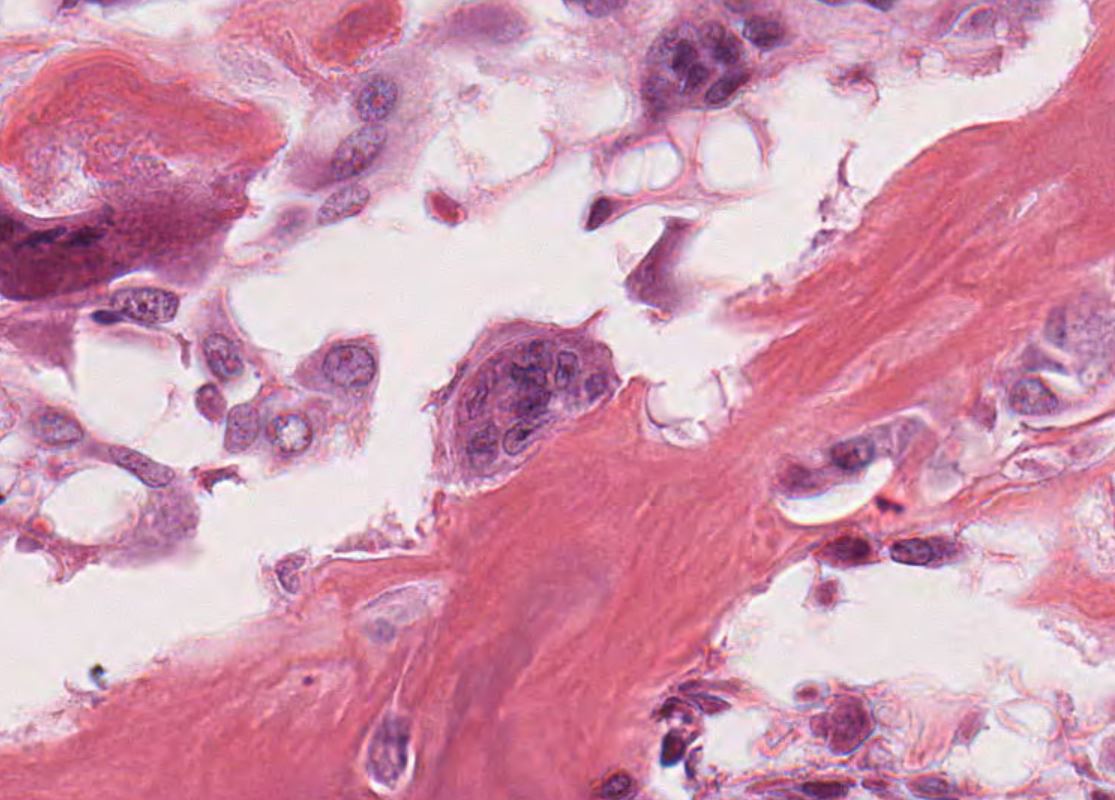
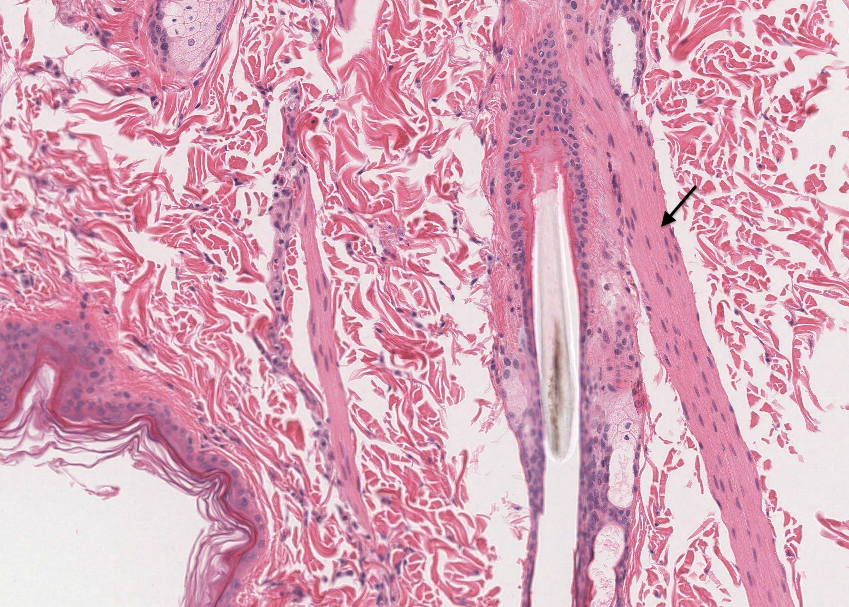
The cell pictured in the center of this photomicrograph is responsible for
resorbs the bone matrix (osteoclasts)
What is the physis and the significance of this finding in a histologic section?
The physis is the line of cartilage that grows between centers which lengthens bone
What are the three types of cartilage and what locations can they be found?
Hyaline cartilage is the most common and covers the surfaces of articular joints, fibrocartilage has abundant collagen bundles and found in menisci and intervertebral discs and elastic cartilage contains elastin fibers and found in pinna of ear
What are the predominant components of cartilage ground substance?
water, glycoproteins and proteoglycans (aggregin)
Chondroblast
immature cartilage cell that is responsible for developing the extracellular matrix
Chondrocyte
mature cartilage cell which functions to produce and maintain chondroid matrix
Perichondrium
connective tissue that envelops cartilage
Sharpey’s fiber
collagenous fibers in tendons that insert into bone
Intervertebral disc
fibrocartilage located between the discs in the spinal column
synovial membrane
innermost aspect of joint capsule that secretes synovial fluid that lubricates joints
What are the three major types of muscle?
skeletal muscle, cardiac muscle and smooth muscle
How are these types of muscle different? List the differences.
Skeletal muscle = contraction and cause voluntary movement, striated, contraction caused by action potential, cardiac muscle = only found in the heart, striated but involuntary contraction, intercalated discs allow muscle to contract uniformly, smooth muscle = no striations, involuntary movement, calcium is extracellular
What locations are each of these types of muscle present?
skeletal muscle = skeleton, cardiac muscle = heart, smooth muscle = internal organs
Skeletal muscle
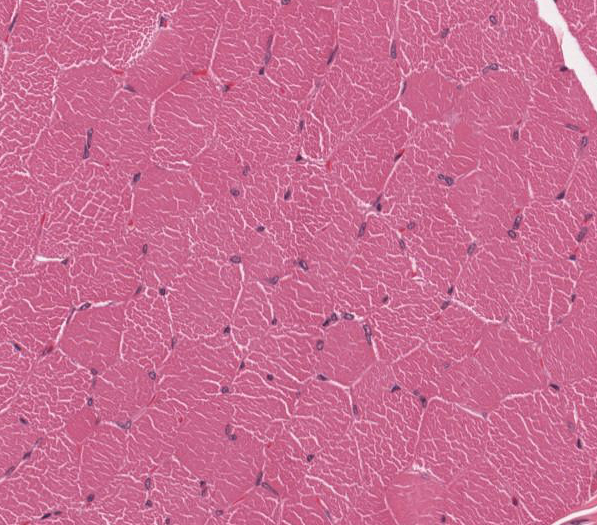
Smooth muscle
Differentiate the following terms. Myofiber, myofibril, sarcomere.
myofiber = muscle cell, myofibril = sarcomeres joined together in long chains, sarcomere = functional unit of skeletal muscle fiber
myofilaments
protein filaments within muscle cells that are responsible for contraction.
T-tubules
are extensions of the sarcolemma into the cytoplasm that run adjacent to the myofibril
List the structural components of a sarcomere. How does a sarcomere function?
actin = thin filament, myosin = thick filament, activated myosin head attaches to actin binding site, phosphate group falls off mysoin head, produces power stroke that forces thin filaments towards each other, atp binds to myosin head causing it to detach from actin site
How is cardiac muscle different than skeletal muscle? How are they the same?
Cardiac and skeletal muscle are both striated (contain sarcomeres) but cardiac muscles’ contraction is involuntary and contains intercalated discs making it uniform
What is the function of smooth muscle?
the involuntary movement of internal organs that helps the movement of substances through the body
What structural components are different in smooth muscle compared to cardiac and skeletal muscle?
smooth muscles’ have no striations and has calcium channels in the sarcolemma
What is myoepithelium?
located in/around glands where extracellular product produced by epithelial cells needs to be moved by contractile actin
Define and explain the basic structural units of a neuron
A neuron contains a axon which is a long extension of the neuron cell body (larger the axon larger the cell body), cell body which contains a nucleus and drives the neuron, and dendrites that receive and release neurotransmitters
Membrane potential
The membrane is charged by having high intracellular concentration of K that will bind to negative charges and as K leaks out of cell, negative charge builds on cell membrane. The resting potential (-90mV) allows the cell to be depolarized.
Depolarization
When high extracellular concentrations of Na+ flow into cell by voltage-gated sodium channels, eliminating the net negative charge, allowing the signal to be transmitted from one end of the neuron to the other.
Repolarization
Occurs by Na entering the cell through voltage-gated sodium channel and K leaving through voltage-gated potassium channel to reestablish membrane potential and allow another signal to be transferred. A Na-K ATP-dependent pump will put Na and K back into their respective areas (Na outside and K inside)
Describe the function of myelin
Used for saltatory conduction by restricting the opening of sodium-voltage gated ion channels to diminish workload of neuron. They support repetitive signaling or long axons. not in every neuron
Explain why glial cells are important
Glial cells help regulate the environment since there needs to be tight control of the central nervous system. Astrocytes eliminate the extracellular space and act as communication between blood vessels and oligodendrocytes. Microglia have an innate inflammatory response.
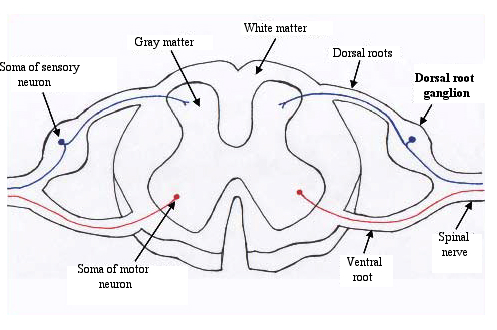
Compare and contrast gray and white matter
Gray matter is where neuron cell bodies are located, reddish pink in life because of its high vascular density. White matter has bundles of axons and is myelin rich.
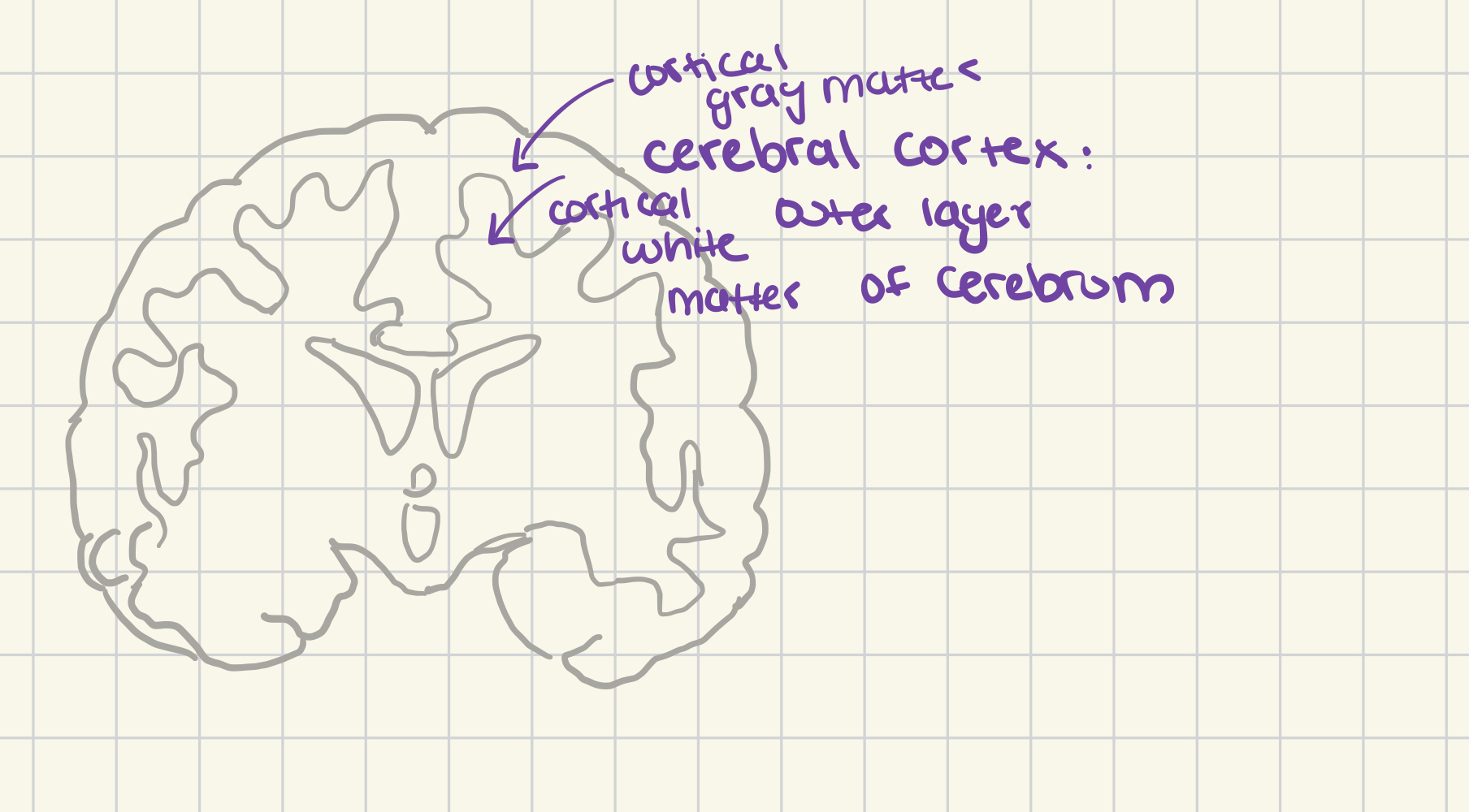
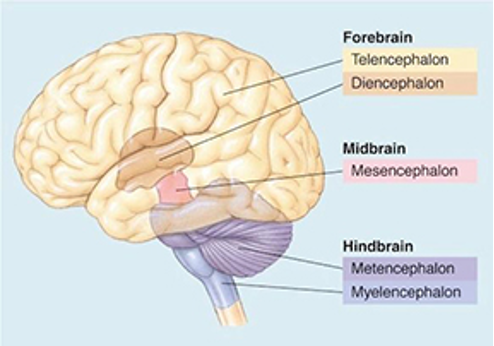
Cerebral Cortex (cortical grey and white matter)
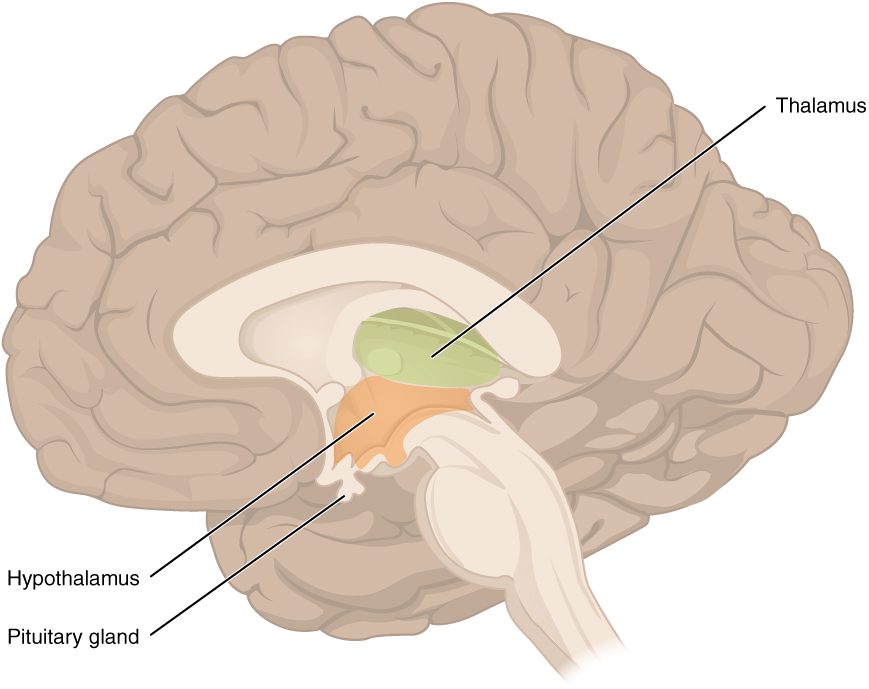
Thalamus and Hypothalamus
constitute the diencephalon
Mesencephalon
“midbrain”
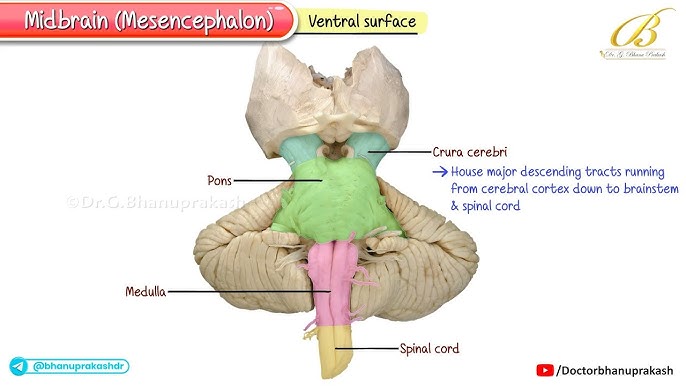
Pons and cerebellum
metencephalon
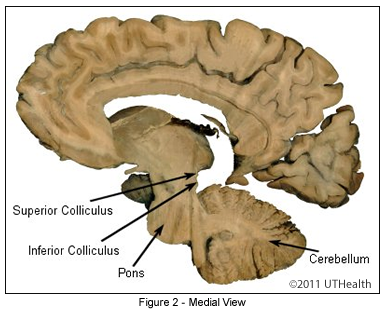
Myelencephalon
contain nuclei, cerebrospinal fluid pathways through ventricles, aqueducts, and canals
White matter tracts
dorsal, lateral and ventral funiculi
ventral median fissure- the cleft at the ventral aspect of the spinal cord that is key to getting orientated, separates the spinal cord into two symmetrical halves
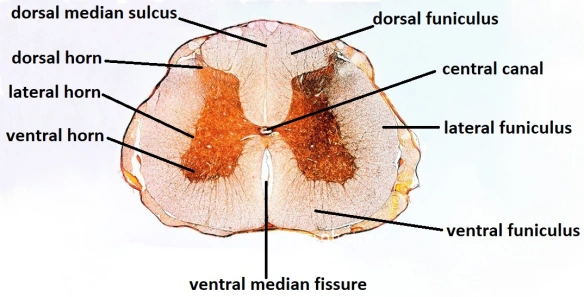
Grey matter horns
dorsal, lateral and ventral horns
dorsal root (sensory input to the central nervous system) and ventral root (axons from motor neurons)
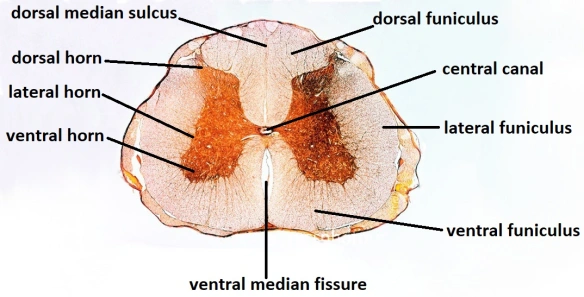
Dorsal root ganglion
carry central neuron signals to central nervous system
Blood brain barrier
Formed by astrocytes, used to control what enters and exits the central nervous system. Either have to lipid soluble or transported by endothelium
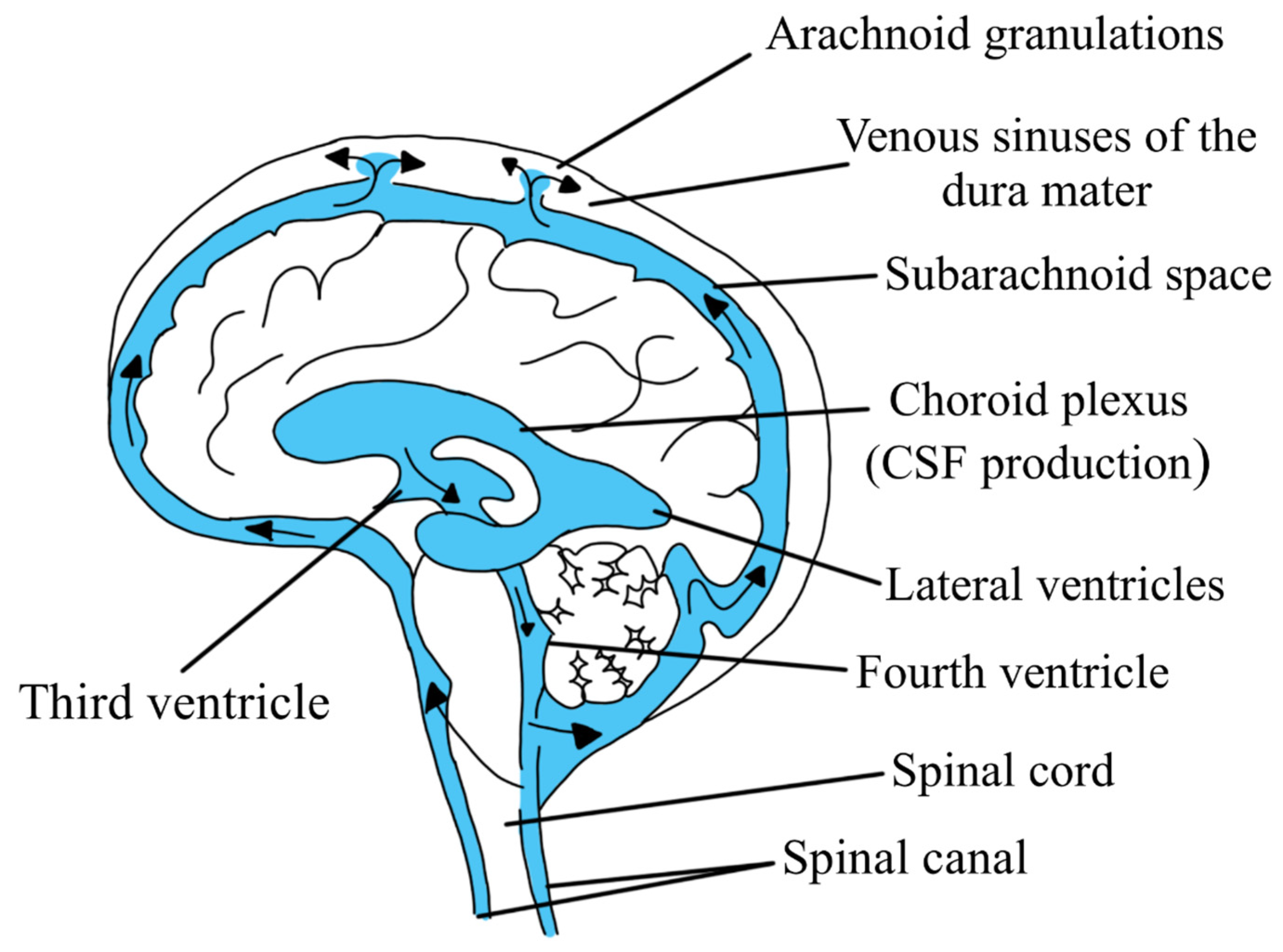
Describe the composition and function of cerebrospinal fluid
Made by choroid plexus and moves from lateral ventricle to interventricular foramen to third ventricle to mesencephalic aqueduct to fourth ventricle
Neonatal period in dogs
0-13 days - deaf, blind, poor sense of smell (can sense pheromones), limited learning
Transitional period in dogs
14-20 days - Eyes open at 10-14 days, tooth eruption, able to stand, learn to avoid pain (no body langauge of fear and no emotional learning), hearing begins
Socialization period in dogs
3-12 weeks - starting to show STARTLE RESPONSE, gradual wean, leave to eliminate, offer play behaviors, social relationships (distance decrease and increase signaling, avoidance response) first fear period is 8-10 weeks
Juvenile period in dogs
3-6 months - rapid growth, increasing independence, sexual interest, teething (destructive chewing)
Sexual maturity in dogs
about 1 year
Adolescence in dogs
1-1.5 years- second fear period, maintain social experience, skills
Social maturity in dogs
18 months-4 years- proactive defense responses (fearful puppies often escalate to aggression)
Neonatal period in cats
0-9 days - deaf, blind, can smell but also use tactile & thermal stimuli, hearing starts day 5, eyes open days 7-10
Transitional period in cats
9-14 days - eyes open 7-10 days, grooming emerges, start orienting to sound, stand & walking, separation (fear/aggression to ppl, locomotor activity, asthma, impaired learning)
Socialization period in cats
2-7(9) weeks - weaning starts around 4 weeks, social relationships with people & animals (distance increasing & decrease signaling), object & social play begins, exploratory behavior, fear responses begins (negative event can cause lifelong, profound consequences), dentition develops and may start to kill mice
Juvenile period in cats
7 weeks-5 months - weaning complete, social play peaks & declines (more predatory), independence increases, separation prior to 12 weeks
Sexual maturity in cats
female matures sexually at 5-9 month, males have spermatogenesis by 5 months, typically not mating until 9-12 months
Social maturity in cats
18 months - proactive defense responses, minimize costs of social errors, self-defense behaviors intensify
Which of the following must be met to consider something a pack/Type III canid structure?
Communal Rearing
Cooperative hunting
Social signals
What are the key features of the correct definition of dominance?
Is about the preferential access to valuable resources
Maintained by deference
Between members of the same species
Relationship established over multiple encounters
Swine are matriarchal groups. However the structure of their relationships is best described by
Dominance in pairs
Which of the following are more commonly seen in horses with musculoskeletal pain when ridden?
ears back
tongue out
going above the bit
tilting the head
unwillingness to go
spontaneous gait change
Feline urination
dig, sniff, urinate, cover
solitary
individuals forage, rest, live alone except for mating, typically rear offspring alone
ex: bears, hamsters, most large felines
pairs
male and female defend a territory and rear offspring together
ex: birds, foxes, some wild carnivores
social pair-bond
territorial/social reasons, may not be sexually monogamous
ex: swans
matriarchal groups
males disperse, intermix during breeding season
ex: cattle, elephants, domestic cats, sheep, goats
lions form matriarchal prides with 1-2 males living alongside
harems
single male lives with group of females
ex: horses, some primates
linear hierarchy
“pecking order” “unidirectional”
high rank is often based on:
rank of parents
age (older)
size (bigger)
Sex (M>F)