RBC DO: MICROCYTIC / HYPOCHROMIC ANEMIA
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
Iron deficiency anemia
Most common form of anemia world widely
Iron deficiency anemia
It is an example of a nutritional anemia
Iron deficiency anemia
ETIOLOGY
Inadequate intake of iron
Increase demand (e.g., Pregnancy, infancy, and childhood)
Impaired iron absorption (e.g., Celiac disease and decrease stomach acidity)
Chronic blood loss (e.g., Chronic GI bleeding, prolong menorrhagia, fibroid tumors, or hemorrhoids)
Iron deficiency anemia
Clinical signs and symptoms
Fatigue, weakness, and shortness of breath, especially with exertion, sore tongue (glossitis), inflamed cracks at the corners of the mouth (angular cheilosis), Koilonychia (spooning of the fingernails) may be seen if the deficiency is long-standing. Patients also may experience cravings for nonfood items, called pica.
Functional
IRON COMPARTMENTS IN NORMAL HUMAN
Hemoglobin iron in the blood
Functional
IRON COMPARTMENTS IN NORMAL HUMAN
Myoglobin iron in muscles
Functional
IRON COMPARTMENTS IN NORMAL HUMAN
Peroxidase, catalase, cytochromes, riboflavin enzymes in all cells
Storage
IRON COMPARTMENTS IN NORMAL HUMAN
Ferritin and hemosiderin mostly in macrophages and hepatocytes; small amounts in all cells except mature RBC
Transport
IRON COMPARTMENTS IN NORMAL HUMAN
Transferrin in plasma
1 - STORAGE DEPLETION
STAGES OF IDA
Hemoglobin: NORMAL
Serum Iron: NORMAL
TIBC:NORMAL
Ferritin: DECREASED
2 - TRANSPORT DEPLETION
STAGES OF IDA
Hemoglobin: NORMAL
Serum Iron: DECREASED
TIBC: INCREASED
Ferritin: DECREASED
3 - Functional depletion / Frank’s/ Full-Blown IDA
STAGES OF IDA
Hemoglobin: DECREASED
Serum Iron: DECREASED
TIBC: INCREASED
Ferritin: DECREASED
Hookworms
Trichuris trichiura
Schistosoma mansoni
Schistosoma haematobium
Parasites associated with IDA
Anemia of Chronic disease/Inflammation
The Second most common type of anemia world widely
Anemia of Chronic disease/Inflammation
It is the most common anemia in hospitalized patient (nosocomial anemia)
Anemia of Chronic disease/Inflammation
Commonly associated with systemic diseases, including chronic inflammatory conditions such as rheumatoid arthritis, chronic infections such as tuberculosis or human immunodeficiency virus infection, and malignancies
Anemia of Chronic disease/Inflammation
ETIOLOGY
Due to inability to use available iron for hemoglobin production
Anemia of Chronic disease/Inflammation
ETIOLOGY
Impaired release of storage iron associated with increased Acute phase reactants such as Hepcidin (decreases release of iron from stores), Ferritin, and Lactoferrin
Sideroblastic anemia
Caused by blocks in the protoporphyrin pathway resulting in defective hemoglobin synthesis and iron overload
Sideroblastic anemia
In this type of anemia, the body has adequate iron but is unable to incorporate it into hemoglobin synthesis. The iron enters the developing erythrocyte but then accumulates in the perinuclear mitochondria of metarubricytes
Ring sideroblasts
is an erythroid precursor containing at least five iron granules per cell, and these iron-containing mitochondria must circle at least one-third of the nucleus
ringed sideroblasts
Sideroblastic anemia
From 10% to 40% of the nucleated erythrocytes in the bone marrow are
Sideroblastic anemia
Excess iron accumulates in the mitochondrial region of the mature RBC in circulation; cells are called ringed siderocytes; inclusions are siderotic granules (Pappenheimer bodies on Wright’s- stained smears)
Perl’s Prussian blue stain
Sideroblasts and Siderocytes are best demonstrated using
Sideroblastic anemia
ETIOLOGY
♥ Miscellaneous disorders (e.g., uremia, thyrotoxicosis, and porphyria)
Sideroblastic anemia
ETIOLOGY
♥ Idiopathic -unknown cause
Sideroblastic anemia
ETIOLOGY
♥ Toxins, including alcohol, and chronic lead poisoning
Sideroblastic anemia
ETIOLOGY
♥ Secondary to drugs: isoniazid (INH), chloramphenicol; after chemotherapy
Sideroblastic anemia
ETIOLOGY
♥ Association with malignant marrow disorders: acute myelogenous leukemia,
polycythemia vera, myeloma, myelodysplastic syndromes
Sideroblastic anemia
ETIOLOGY
♥ Acquired defect: primary (one of the myelodysplastic syndromes); may evolve into
acute myelogenous leukemia
Sideroblastic anemia
ETIOLOGY
♥ Congenital defect: hereditary sex linked (primarily males); autosomal
Primary
Types of Sideroblastic anemia that is irreversible; causes of block is unknown
Secondary
Types of Sideroblastic anemia that is reversible; causes include alcohol, anti-TB drugs, Chloramphenicol
T
Anemia, when present in lead poisoning, is most often normocytic and normochromic; however, with chronic exposure to lead, a microcytic, hypochromic clinical picture may be seen (t/f)
lead poisoning
Multiple blocks in the protoporphyrin pathway that affect heme synthesis
lead poisoning
Presence of many coarse Basophilic stipplings
lead poisoning
what will lead to acquired sideroblastic anemia and acquired porphyria
lead poisoning
It inhibits ferrochelatase and D-ala synthase enzyme in Heme/Protoporphyrin pathway
Iron Deficiency Anemia (IDA)
LABORATORY FEATURES IN MICROCYTIC / HYPOCHROMIC ANEMIAS
SERUM IRON: ↓
SERUM TIBC: ↑
% SATURATION: ↓
% SIDEROBLASTS: ↓
IRON STORES: ↓
SERUM FERRITIN: ↓
ZPP: ↑
Hb A2: N-↓
Hb F: N
Beta thalassemia
LABORATORY FEATURES IN MICROCYTIC / HYPOCHROMIC ANEMIAS
SERUM IRON: N(↑)
SERUM TIBC: N
% SATURATION: N
% SIDEROBLASTS: N(↑)
IRON STORES: N-↑
SERUM FERRITIN: N-↑
ZPP: N
Hb A2: ↑
Hb F: N-↑
Anemia of chronic dx
LABORATORY FEATURES IN MICROCYTIC / HYPOCHROMIC ANEMIAS
SERUM IRON: ↓
SERUM TIBC: N-↓
% SATURATION: ↓
% SIDEROBLASTS: ↓
IRON STORES: N-↑
SERUM FERRITIN: N-↑
ZPP: ↑
Hb A2: N
Hb F: N
Sideroblastic anemia
LABORATORY FEATURES IN MICROCYTIC / HYPOCHROMIC ANEMIAS
SERUM IRON: ↑
SERUM TIBC: ↓
% SATURATION: ↑
% SIDEROBLASTS: ↑
IRON STORES: ↑
SERUM FERRITIN: ↑
ZPP: ↑
Hb A2: N
Hb F: N-↑
Serum Iron
Indicator of available transport iron
Serum Iron
Used for the differential diagnosis of disorders of iron metabolism
non hemolyzed serum and should be obtained in the morning (because serum iron levels may be approximately 25 % lower in the evening)
Spx of Serum Iron
12 hrs
How many hours of fasting is required for Serum Iron
12 hrs
How many hours of fasting is required for TIBC
50 to 160 ug/dl
ref range of Serum iron
250 to 400 ug/dl
ref range of TIBC
40 to 400 ng/ml (rodaks)
Men: 15 to 200 ug/ L
Women:12 to 150 ug/L
ref range of Serum Ferritin
<50 ug/dl of RBC (approximate only bc it depends on the method being used )
ref range of Free Erythrocyte Protoporphyrin
Total iron binding capacity (TIBC)
Indirect indicator of iron stores
Total iron binding capacity (TIBC)
Indirectly measures the concentration of transferrin by measuring its ability to bind iron
non hemolyzed serum
Spx of TIBC
T
TIBC Values are independent on the time of day the sample is drawn (t/f)
Serum Ferritin
Reveals the body’s tissue on iron stores
Serum Ferritin
♥ Good indicator of iron storage status
Serum Ferritin
♥ Useful in diagnosis of iron deficiency
Serum Ferritin
♥ Generally, the first laboratory test to become abnormal when iron stores become to decline
Serum Ferritin
♥ Measured using radioimmunoassay
T
Free Erythrocyte Protoporphyrin (t/f)
RBCs produce slightly more protoporphyrin than is necessary, but in iron deficiency, protoporphyrin levels build up in RBCs to several times the normal
Free Erythrocyte Protoporphyrin
May be measured directly by a hemato-fluorometer or by an extraction and fluorescence method
Free Erythrocyte Protoporphyrin
♥ Differentiating thalassemia, IDA, & anemia of chronic infection
% Transferrin saturation = Serum Iron / TIBC x 100
Formula of % Transferrin saturation
Perl’s Prussian blue (Rous-test) stain
is actually a chemical compound with the formula Fe7(CN). The compound forms during the staining process, which uses acidic potassium ferrocyanide as the reagent/ stain
Perl’s Prussian blue (Rous-test) stain
is considered the gold standard for assessment of body iron stores.
Perl’s Prussian blue (Rous-test) stain
It is used to confirm hemosiderinuria
diffuse cytoplasmic blueness
Perl’s Prussian blue (Rous-test) stain in Ferric reaction
ferritin is not typically detected, likely because of the intact protein cage. In high concentration, it can appear as a -
dark blue granules
Perl’s Prussian blue (Rous-test) stain in Hemosiderin reaction
hemosiderin stains readily, forming distinct -
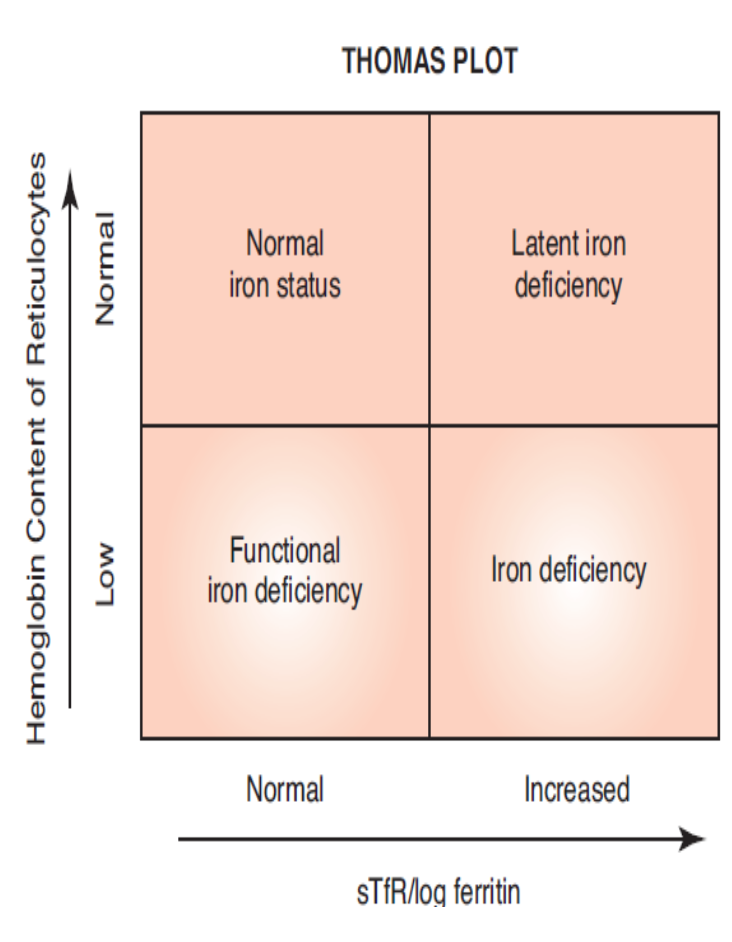
Lower right quadrant
In Thomas Plot TRUE IDA is located in what quadrant
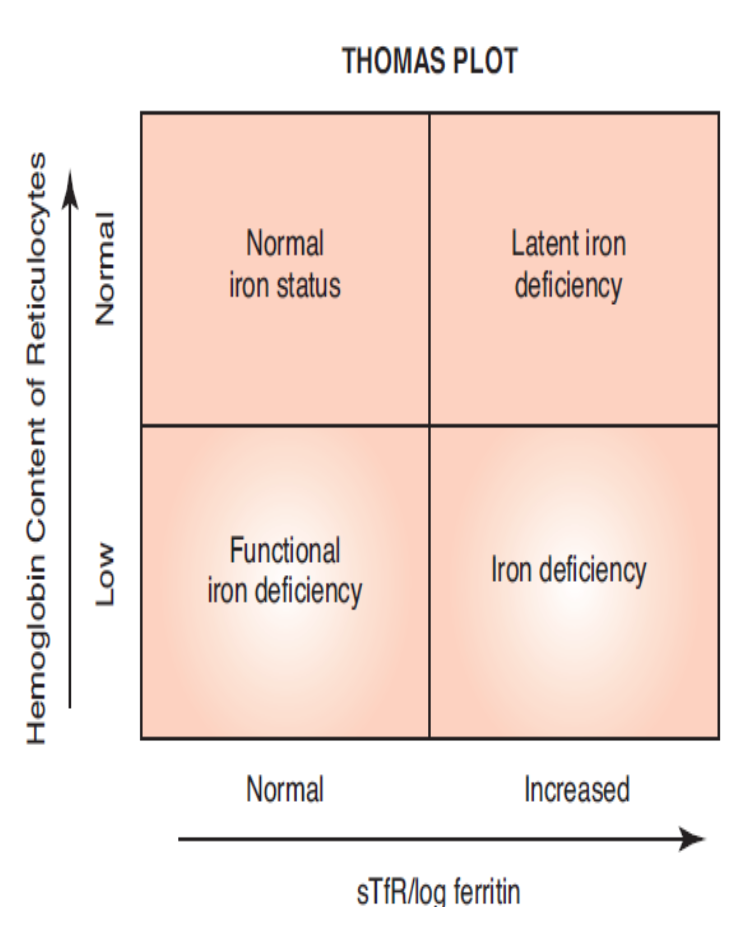
Lower left quadrant
In Thomas Plot FUNCTIONAL IDA is located in what quadrant
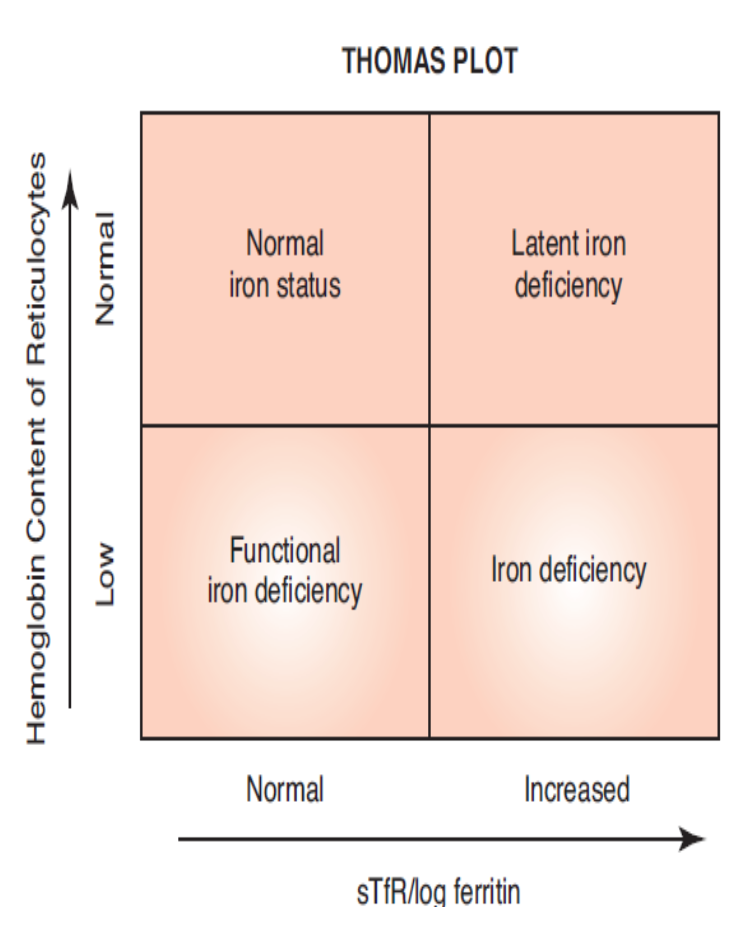
Upper right quadrant
In Thomas Plot LATENT IDA is located in what quadrant