Vascular occlusion
1/18
Earn XP
Description and Tags
As part of posterior segment disorders
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
19 Terms
What are the two types of retinal vascular occlusion?
Retinal vein occlusion (RVO) and retinal artery occlusion (RAO). Both types can be further subdivided into central or branching occlusions.
CRVO occurs in the central retinal vein at the lamina cribrosa.
BRVO occurs in the branch retinal veins, most often in the superotemporal quadrant.
CRAO occurs in the central retinal artery.
BRAO occurs in the branches of the central retinal artery.
What are the causes of RVO?
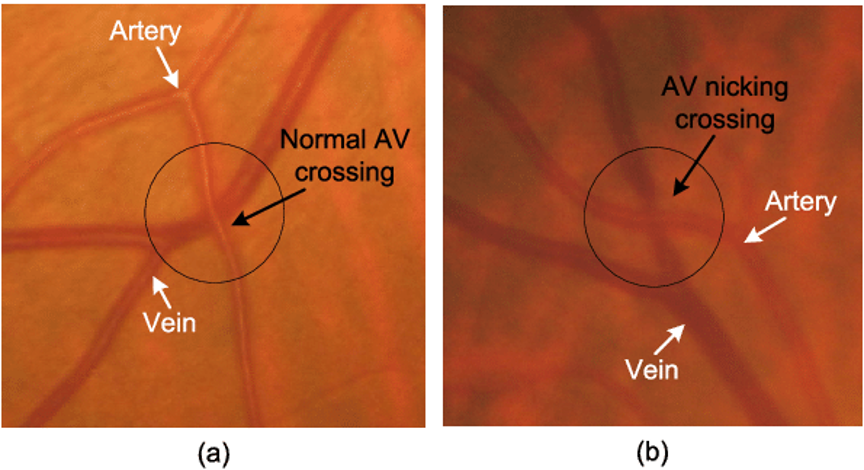
Atherosclerosis leading to venous nipping - most common
Clots/emboli
Ischaemia
Vasculitis
What are the risk factors for vascular occlusions?
Age
Hypertension
History of stroke/TIA or heart attack
Smoking
Diabetes
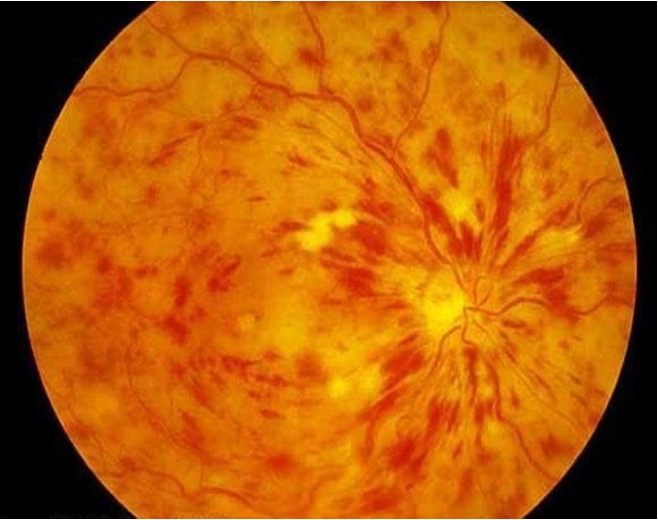
What are the typical findings on fundus exam of a CRVO?
Flame haemorrhage
Dot-and-blot haemorrhage
Cotton wool spots
Oedema
What are the typical findings on fundus exam of a BRVO?
Branch flame haemorrhage
Cotton wool spots
Oedema
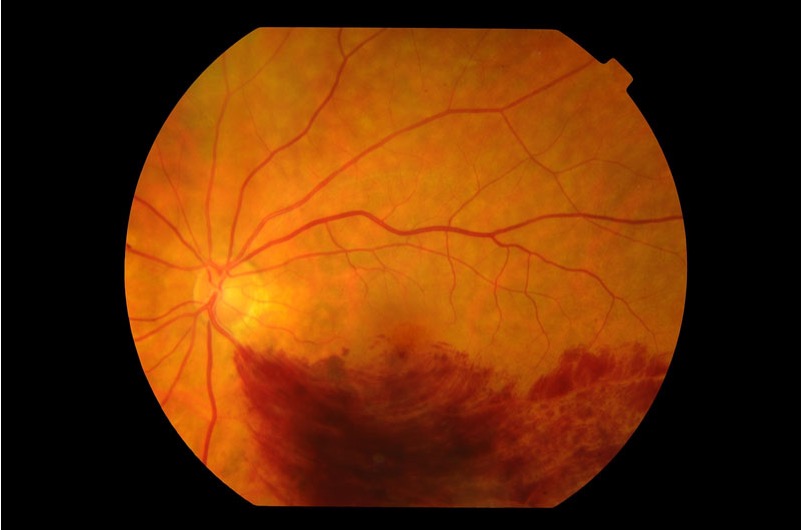
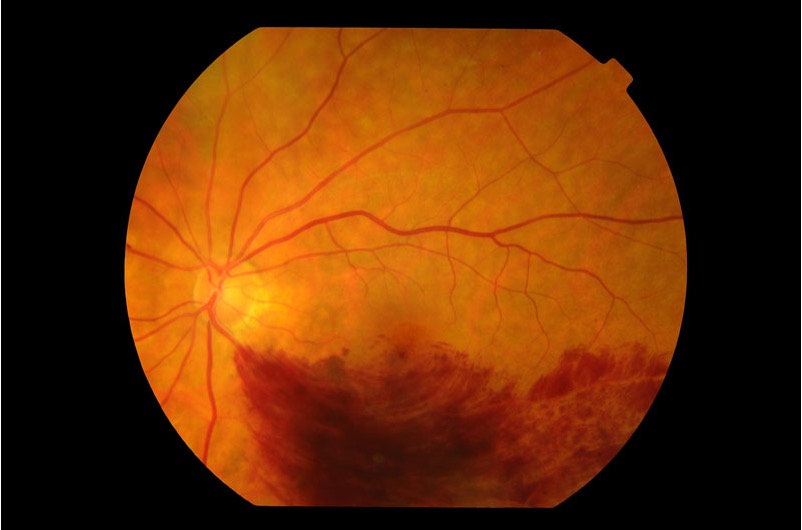
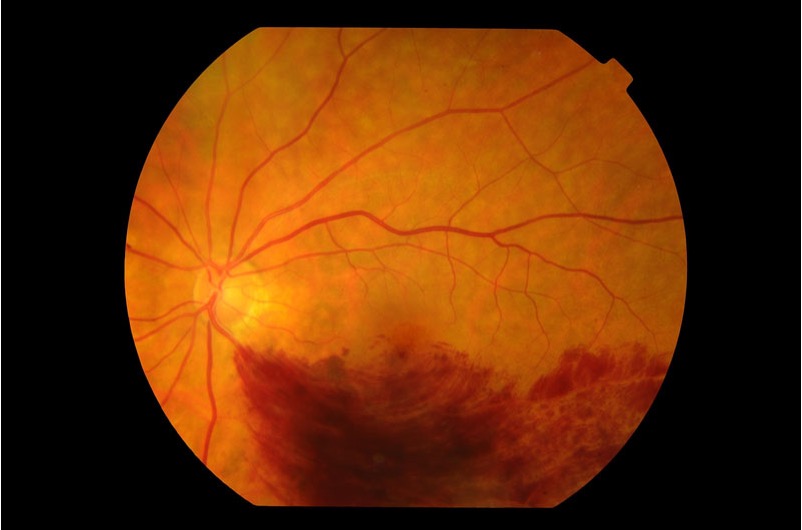
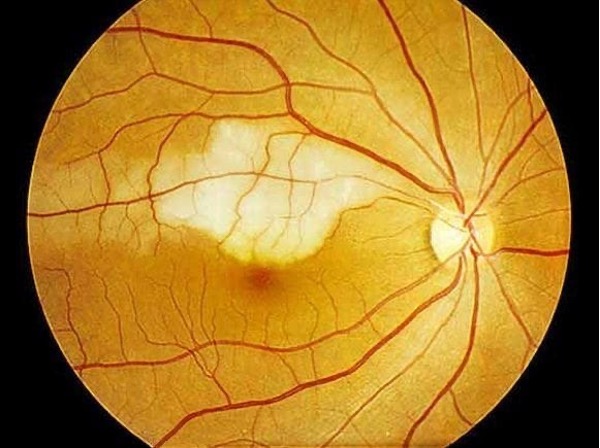
True or false? The fundus image shows a CRVO.
False. This image shows a branch RVO, characterised by the flame haemorrhage and location in a branch vein.
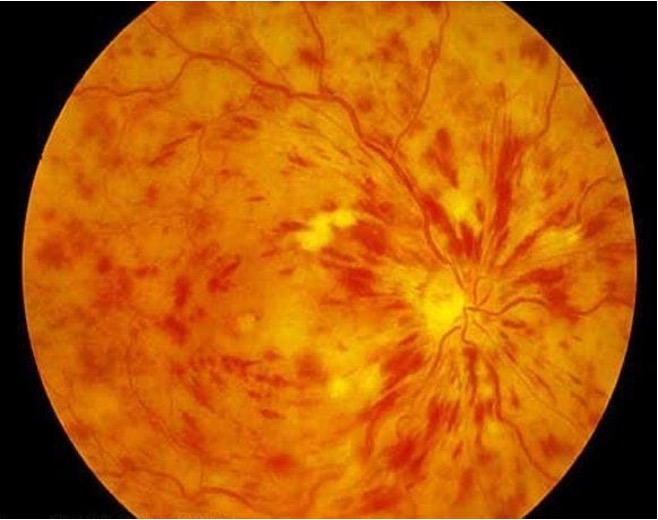
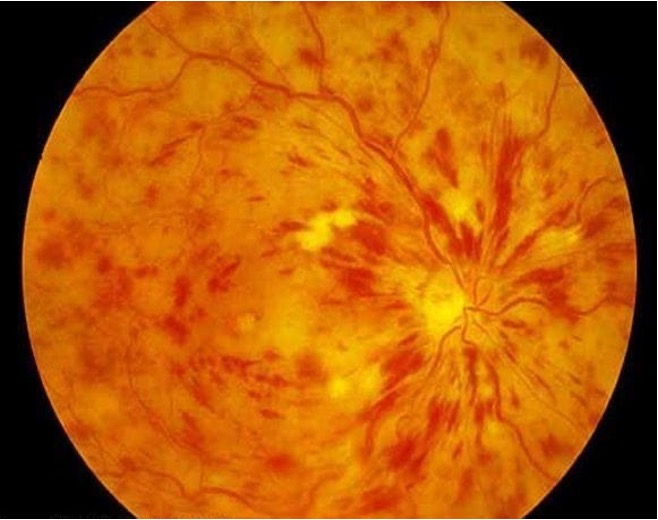
True or false? The image shows a CRAO?
False. The image shows a central retinal vein occlusion, characterised by dot-and-blot haemorrhages and cotton wool spots.
True or false? Both RVO and RAO present with a sudden onset, painless loss of vision in one eye.
True. Both retinal vein occlusion (RVO) and retinal artery occlusion (RAO) can lead to a sudden, painless loss of vision in one eye. Both types of patient may also experience a prior episode of transient visual loss before onset. They can be differentially diagnosed on examination of the fundus.
True or false? RAPD is present in both RVO and RAO?
False. Relative afferent pupillary defect (RAPD) is associated with RAO, but not typically with RVO. Sometimes a minor RAPD is observed in CRVO, but is never associated with BRVO.
How can you differentially diagnose between the four types of vein/artery occlusions?
On fundus exam - CRVO shows dot-and-blot haemorrhage, BRVO shows branch flame haemorrhage, CRAO shows diffuse artery constriction with a cherry red macula and cloudy retinal swelling, and BRAO shows branch artery constriction with a cherry red macula and localised cloudy retinal swelling.
Generally vein occlusions show tortuosity and dilation, whereas artery occlusions show a pale yellow retina, cherry red macula and vessel constriction.
By signs - RAPD is associated with artery occlusions, and artery occlusions typically cause the most significant visual losses with counting fingers or light perception in most cases. RVO usually causes less severe vision loss and can present with varying degrees of visual acuity, with some minor cases of BRVO being asymptomatic.

What is this patient likely experiencing?
Sudden, painless, monocular loss of vision
The patient is 75 and has a history of stroke
The patient thinks they had some black spots in their vision a few days ago, but can’t remember very well
Affected eye has gone totally “black”, i.e. patient cannot see any light
Affected eye demonstrates RAPD
CRAO
The severity of sight loss, presence of RAPD, and appearance of the fundus provide the differentials for diagnosis.
What kind of retinal vascular occlusion is an ocular and life emergency?
RAO - without very swift treatment (<12 hours) there will be significant and irreversible sight loss. The blockage should be swiftly identified and located in case of embolism or aneurysm.
What is this patient likely experiencing?
Sudden, painless, monocular loss of vision
The patient is 89 years of age and has hypertension
The patient thinks they had some black spots in their vision a few days ago, but can’t remember very well
Affected eye has gone blurry, with a VA of 6/18
Affected eye demonstrates a slight RAPD
The patient reports metamorphopsia
CRVO
The presence of blurry vision with reduced VA, and a slight but not significant RAPD, as well as the appearance of the fundus, provide the differential diagnosis. If the patient was experiencing CRAO, they would likely only have counting fingers if they had any light perception at all.
What is the patient likely experiencing?
Sudden, painless, monocular loss of vision
The patient is diabetic and a smoker
Affected eye has gone blurry in the periphery
Affected eye does not demonstrate RAPD
BRVO
The appearance of the fundus, lack of RAPD, and peripheral blur provide the differentials for diagnosis.
What is the patient likely experiencing?
Sudden, painless, monocular loss of vision
The patient has hypertension and a history of stroke
Affected eye has lost all light perception except in the inferior periphery, where the patient can detect hand movements
Affected eye demonstrates a slight RAPD
BRAO
The appearance of the fundus, presence of only a slight RAPD, and ability to detect some light in parts of the visual field provide the differentials for diagnosis. If this was instead a BRVO, the fundus would show a flame haemorrhage in the affected branch, as well as vessel tortuosity and swelling.
True or false? Retinal vein occlusions can be treated.
True - patients are often treated with anti-VEGF or steroid injections to prevent secondary retinal neovascularisation and secondary glaucoma as a result of neovascularisation at the iris. Patients will also likely be referred to the low vision clinic for low vision support.
Retinal artery occlusions are irreversible and must be treated within 12 hours to minimise the amount of visual loss.
What are the major complications of retinal vein occlusion?
Macular oedema and retinal ischaemia, resulting in neovascularisation and possible secondary glaucoma.
What is the prognosis for retinal artery occlusion?
Very poor. Vision loss is likely to be very significant and is irreversible. If a patient receives treatment immediately, they may experience less vision loss.
How are vascular occlusion patients investigated and monitored? (Hint - consider the impact on vision, the retina, the vessels, and any associated complications.)
VA
Visual fields
Fundus photography
OCT
Fluorescein angiogram
IOP
Gonioscopy