asthma
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
what is asthma
Widespread narrowing of the bronchial airways, which changes in severity over short periods of time (either spontaneously or under treatment) and leads to cough, wheezing and difficulty breathing
Characterised by bronchospasm and airway hyper-responsiveness (triggers cause airway to narrow e.g. cold, allergies, exercise)
Significant inter-patient variability in terms of disease severity, course and response to treatment.
Symptoms may resolve in response to medication (or spontaneously), and may sometimes be absent for weeks or months at a time.
Reversibility differentiates asthma from other chronic and/or progressive respiratory disorders (i.e. COPD)
Often provoked by trigger factors e.g. exercise, cold air, allergy, house dust mite
what is acute asthma exacerbation
asthma attack
onset of severe asthma symptoms, which can be life-threatening
what are the risk factors for asthma development
No single cause of asthma, phenotyping may help identify individual risks.
Personal or family history of atopic disease (i.e. family asthma history, eczema, allergic rhinitis, allergic conjunctivitis)
Tobacco / smoking exposure (including prenatal exposure)
Respiratory infections (particularly bronchiolitis) during infancy
Obesity
Prematurity / Low birth weight
Social deprivation
Workplace exposure to floor dust, paint, volatile chemicals (solvents)
what are the prognostic features and complications of asthma
In general, the earlier the onset of asthma symptoms, the more likely a person is to “grow out” of asthma in transition to adulthood.
Male children more likely to develop pre-pubertal asthma, but also more likely to grow out of asthma during transition to adulthood
In significant/severe/uncontrolled disease, possibility of respiratory complications (i.e. pneumonia, pneumothorax, respiratory failure, status asthmaticus)
Significant impact of uncontrolled/suboptimally controlled asthma on quality of life (i.e. through chronic fatigue, time off work/school etc)
In chronic uncontrolled disease, airway remodelling can cause persistent airflow obstruction similar to COPD
what is the pathophysiology of asthma
Typically mediated by immunoglobulin E, and precipitated by response to allergen (animal dander, pollen etc).
Allergen-specific IgE antibodies attach to surface of mast cells
Subsequent exposure causes release of inflammatory mediators that promote bronchospasm, including:
Leukotrienes
Histamine
Prostaglandins
these are targets for drug therapy
If untreated, eosinophils, T-helper cells and mast cells migrate to airways
Excessive mucus production causes further airway narrowing
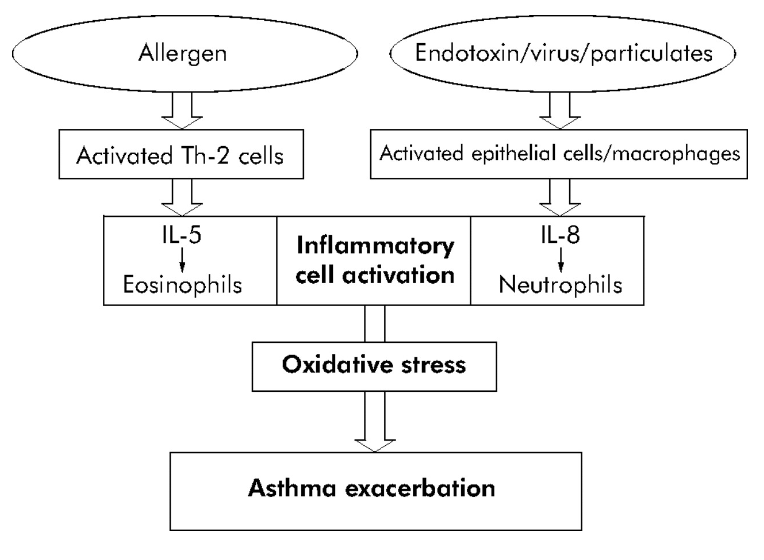
what are the pathways to exacerbation of asthma
both leads to inflammatory cell activation, oxidative stress and asthma exacerbation
however, white cells that are activated are different
what are the key triggers of asthma
Many factors may cause an asthma exacerbation/attack, with triggers being patient-specific and variable.
Allergens, e.g. Pollen, Animal dander, Dust mite and In some cases, ingested allergens
Viral infections
Stress
Exercise
Cold air
Iatrogenic (NSAIDs, beta-blockers (propranolol) → any injury, illness, or adverse condition in a patient caused by medical treatment)
early vs late asthmatic responses
Following an allergen challenge, response may be characterised as “Early” (or “Acute”) and “Late” asthmatic response → effects of FEV1 varies
EAR – typically bronchospasm following exposure to allergen
LAR – inflammatory reaction,comprising bronchospasm, alongside:
Vasodilation
Oedema
Excess mucus secretion
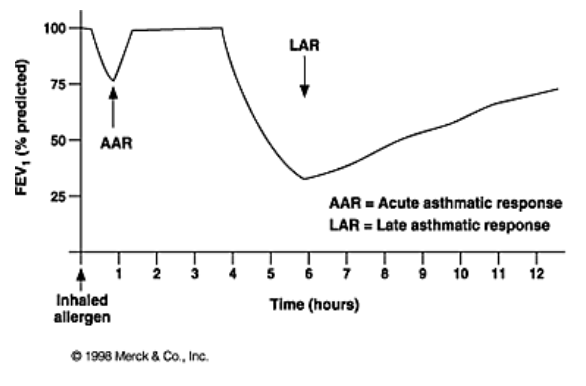
what is a late asthmatic response
thought to be caused by influx of T-helper (Th2) cells & Activated Eosinophils
Release of inflammatory mediators:
Leukotrienes
Cytokines IL-3, IL-4 & IL-5
Chemokine IL-8
‘Toxic’ proteins
Eosinophil cationic proteins
Major basic protein
Eosinophil-derived neurotoxin
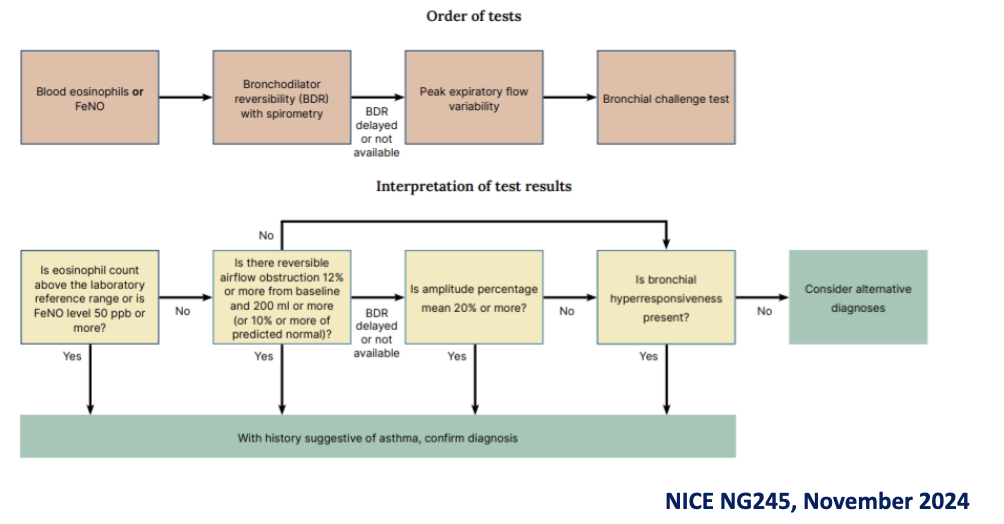
how is asthma diagnosed
No single diagnostic test to prove asthma in previously undiagnosed patients.
Diagnosis of asthma typically based upon combination of structured clinical history and objective tests, including:
Blood eosinophil count
Fractional exhaled Nitric Oxide (FeNO) testing
Bronchodilator reversibility with Spirometry
Peak Flow (PEF) readings
Bronchial challenge
On presentation, ensure patients are not acutely unwell. If acutely unwell (i.e. presentation with acute exacerbation)
what are the key diagnostic tests for asthma
Fractional Exhaled Nitric Oxide (FeNO) → Measures fraction of exhaled Nitric Oxide. Demonstrates/quantifies level of inflammation in the respiratory tract.
Bronchodilator reversibility with Spirometry → Spirometric testing before and after administration of bronchodilator (i.e. short-acting beta2 agonists). Demonstrates reversibility of airway restriction and can help distinguish asthma from other conditions.
Peak flow readings → Diurnal variations in Peak Flow can suggest day-to-day symptom variation characteristic of asthma.
Bronchial Challenge → Administration of challenge (i.e. via methacholine) to provoke bronchoconstriction. Demonstrates airway hyper-responsiveness.
how is diagnosis of asthma confirmed according to NICE
what is the history taking for asthma
Asthma should only be confirmed in patients where a history suggestive of asthma is present, alongside objective tests.
In a structured clinical history, presence of more than one symptom of episodic wheeze, cough, breathlessness and chest tightness suggestive of asthma:
Symptoms typically diurnal, and may be worsened at night (or in early morning)
Triggers may include exercise, recent viral infection, exposure to cold air or allergens. Occupational asthma in adults may be worsened on days whilst working.
Iatrogenic triggers may include beta-blockers and NSAIDs
Emotional triggers may also be present, particularly in children
how are NSAIDs a latrogenic trigger
Inhibition of COX enzymes, reduce prostaglandin synthesis and relieves pain and inflammation.
Inhibition of COX activates lipoxygenase pathway, increasing production of leukotrienes, promoting bronchospasm
how are beta blockers a latrogenic trigger
particularly Non-selective beta-blockers block both beta-1 and beta-2 receptors.
Cardioselective beta-blockers may block beta-2 receptors at high doses.
Blockage of beta-2 receptors can prevent innate pathways for bronchodilation in response to trigger (or affect response to medication use)
Level of cardioselectivity / vasodilatory properties vary between generations (and individual agents)
what are differential diagnosis to asthma
Other conditions which may present with similar symptoms include:
Bronchiectasis / Interstitial lung disease
Chronic Obstructive Pulmonary Disease (COPD)
Cystic fibrosis
GORD
Heart Failure
Pulmonary Embolism
Tuberculosis
Consideration should be given to signs that may suggest another diagnosis (i.e. haemoptysis, persistent symptoms with no diurnal variation, presence of oedema etc)
what is the current guideline for asthma
Tri-partite NICE/BTS/SIGN guidance published in November 2024
what are the key sources of guidance
National Institute for Health and Care Excellence / British Thoracic Society / Scottish Intercollegiate Guidelines Network (NICE/BTS/SIGN) joint guideline
British Thoracic Society / Scottish Intercollegiate Guidelines Network (BTS/SIGN) joint guideline (partially replaced)
what were the traditional asthma treatments (old)
asthma treatments broadly split into two types, “preventers” and “relievers”
Preventers → designed to prevent symptoms, minimise exacerbations of asthma etc
Relievers → designed to be used in the event of shortness of breath etc
what are Short-acting Beta2 agonists
E.g. Salbutamol (Albuterol in US), Terbutaline
Act through activation of beta adrenergic receptors, causing relaxation of smooth muscle in the lung and resultant dilation and opening of the airways.
however, not specific to beta 2 receptors→ can cause tachycardia and palpitations by agonising beta 1 receptors at high doses
Also may cause tremor, excessive sweating, insomnia and agitation.
Some reports of paradoxical aggravation of asthma in large doses although cause unknown.
Traditional “when required” therapy
salbutamol (Brand: Ventolin and others): Available as pMDI, dry powder inhaler, breath actuated pMDI, nebuliser solution
Terbutaline (Brand: Bricanyl) Available as dry powder inhaler, nebuliser solution
what are long-acting beta 2 agonists
E.g. Salmeterol, Formoterol, Indacaterol , Olodaterol
Shares a mechanism of action with short-acting beta2 agonists with a considerably greater duration of action allowing for use as a ‘preventer’
Effect persists despite washing of tissue, so no full agreement on why action persists over long period of time.
Long acting: Generally used twice daily (Salmeterol, Formoterol) → Onset varies. Formoterol quicker onset than Salmeterol, formoterol the most common long acting beta 2 agonist and works quicker than the others
Ultra long acting: Generally used once daily (Indacaterol, Vilanterol)
Variety of formulations available, both as monotherapy and as combination inhalers: pMDI: Formoterol, Salmeterol, Olodaterol AND DPI: Formoterol, Salmeterol, Indacaterol
what are inhaled corticosteroids
E.g. Beclometasone Dipropionate, Budesonide
Thought to act through action at nucleus of epithelial cells promoting transcription of genes that decrease inflammation.
Important to consider equivalence between different corticosteroids when transitioning between products – broadly grouped (for adults) into low dose, medium dose, high dose
Formulation also important with BDP due to microfine particles in some formulations: Clenil Modulite (standatd formulation ) v Qvar (extra fine particles ) (2:1)
was available as either monotherapy, or co-formulated in ICS/LABA or ICS/LABA/LAMA (“triple therapy”) inhaler → adherence is typically poor → not really used as monotherapy, mostly combined in new guideline
inflammation reduced in the long-term
high dose ICS leads to systemic effects
oral thrush most common effect of poor inhaler technique
Variety of formulations available:
pMDI: BDP, Ciclesonide, Fluticasone
Breath actuated pMDI: BDP
DPI: BDP, Budesonide, Mometasone, Fluticasone
Nebuliser Solution: Budesonide, Fluticasone
what are the formulations of inhaled corticosteroids
pMDI: BDP, Ciclesonide, Fluticasone
Breath actuated pMDI: BDP
DPI: BDP, Budesonide, Mometasone, Fluticasone
Nebuliser Solution: Budesonide, Fluticasone
what are leukotriene receptor antagonists
E.g. Montelukast
Typically taken daily at night
Act through inhibition of Leukotrienes, which promote bronchoconstriction, inflammation and mucus secretion.
Zafirlukast withdrawn from UK market, but still available in some countries and may be mentioned in some guidance. Reports of liver dysfunction.
Montelukast (Brand: Singulair) – Available as tablets, granules, chewable tablets → Taken once daily at night.
what is the NEW guideline NICE/BTS/SIGN 2024
For adults (or adolescents >12 years old)
For newly diagnosed asthma, offer a low-dose ICS/formoterol (AIR) for when required use → air anti inflammatory reliver → combination inhaler specifically licensed for symptoms which includes combo inhaler with ICS (usually budesonide) / long-acting beta2-agonist (LABA) (usually formoterol) to be used as reliever → not be used when there are no symptoms e.g. as a preventer
If uncontrolled at stage 1, then offer low-dose maintenance and reliever therapy (MART)
If uncontrolled, then escalate to medium-dose MART regimen
If uncontrolled, then consider adding first a leukotriene receptor antagonist (LTRA) for a trial, followed by a long-acting muscarinic antagonist (LAMA)
what are the new guidelines for combination inhalers
Licensed for asthma, principally combinations containing ICS/LABA E.g Seretide, Fostair, Symbicort
Reduces amount of puffs required to be taken regularly and can improve adherence
Some ICS/LABA/LAMA inhalers licensed for fixed-dose use in asthma (likely specialist introduced/recommended in current guidance).
Some (but not all) licensed for use for use in MART regimens
Not necessarily more effective that individual components in fixed regimens, but certainly more convenient in most cases
what are the new guidelines ICS/LABA combination inhalers
Licensed in one of three ways (some as all three, some just as one/two) → important to check carefully
Some ICS/formoterol inhalers licensed as initial “when required” therapy for patients with mild asthma. (i.e. Symbicort 200/6 Turbohaler), AIR therapy
Some ICS/LABA combination inhalers licensed as MART (either low-dose or medium-dose) (i.e. Fostair, Symbicort etc)
Principally those including formoterol as LABA component due to speed of onset
Same inhaler used as both “preventer and reliever” (i.e. 1 dose BD, 1 dose PRN)
Some ICS/LABA combination inhalers only licensed as fixed dose combination (i.e. Seretide evohalers) → Separate inhalers i.e. 2 puffs BD, with separate reliever inhaler)
what are the new guidelines for Anti-inflammatory reliever (AIR) therapy
Refers to combination inhaler, containing formoterol-ICS
Used as “reliever” inhaler only (i.e. when required for asthma symptoms), with no regular preventer used
Formoterol used with preference to other LABAs due to speed of onset vs other LABAs
Initially only Symbicort 200/6 Turbohaler (budesonide/formoterol) was licensed for this indication.
Increasing number of other budesonide-formoterol combinations now licensed i.e. Fobumix Easyhaler, Duoresp Spiromax, WockAIR Budesonide/formoterol
Likely extension to beclomethasone-formoterol in near future
Current challenges in terms of transition from traditional treatment paradigm (i.e. patient adoption etc)
what are the new guidelines for Maintenance and Reliever Therapy (MART)
Use of same inhaler as both “preventer” and “reliever” therapy.
Patient still only need to carry and use a single inhaler.
Refers to ICS/LABA combination inhalers containing formoterol (due to quick onset of action) vs salmeterol
Wider range of inhaled therapies licensed for this use in comparison to AIR therapy
Examples of inhalers licensed for this use:
Symbicort Turbohaler / DuoResp Spiromax (Budesonide / Formoterol salts)
Fostair/Proxor/Luforbec/Bibecfo/Vivaire pMDI/DPIs (BDP / Formoterol)
what are specialist therapies
In specialist settings, additional interventions may be made that would not typically be employed in primary care settings:
Increase dose of inhaled corticosteroid to high-dose range (i.e. Up to 2000mcg/day BDP maximum (or equivalent) → Increased risk of systemic effects at higher doses
Biological therapies increasingly favoured for certain types of asthma (i.e. omalizumab)
Some ‘old fashioned’ approaches to asthma management, that might still be encountered on occasion:
Trial of modified release theophylline
Modified release oral beta2 agonist (e.g. Salbutamol tablets) may be available/used in very specific circumstances, but very rarely used → Often poorly tolerated in patients also using a LABA due to enhanced risks of adverse effects
Continuous / regular use of oral corticosteroids may be considered as a last resort
what is theophylline
Xanthine - acts through two distinct mechanisms:
Smooth muscle relaxation
Suppression of response of the airways to stimuli
Caution required:
Narrow therapeutic index
Some variability between brands – Brand prescribing needed.
High propensity for toxicity
Huge amounts of drug interactions
Issues around clearance with smokers
Theophylline (Brand – Uniphyllin Continus): Available as M/R tablets. Other brands (Nuelin SA, Slophyllin) discontinued.
Aminophylline: (Theophylline-ethylenediamine): Available as solution for Injection – oral dosage forms discontinued in UK (but available in some international markets) as Phyllocontin
what are considerations for the regular use of corticosteroids
Patients should be under the care of a respiratory specialist before initiation of regular oral corticosteroids is considered.
Introduce regular oral corticosteroids (Prednisolone) at lowest possible dose to provide adequate asthma control.
This is not a replacement for inhaled corticosteroids, which should be continued alongside oral corticosteroids.
Consider long term consequences of use of oral corticosteroids: Calcium supplementation? or Gastro-protection?
Steroid card should be provided
providing review for asthma patients
All asthmatic patients will need to be monitored in primary care with a view to stepping up / stepping down treatment as required.
Monitoring should be individualised to the patient/severity of disease, the following factors should be considered as a part of monitoring plans:
Symptomatic control
Lung function (PEF / Spirometry)
History of asthma attacks, oral corticosteroid use and time off work/school missed since last assessment
Inhaler Technique
Bronchodilator / “reliever” use
Self-management plan – does the patient have one? Have they increased doses?
what is the assessment of symptomatic control
Consider Royal College of Physician’s 3 Questions:
In the last month/week have you had difficulty sleeping due to your asthma (including cough symptoms)
Have you had your usual asthma symptoms (eg, cough, wheeze, chest tightness, shortness of breath) during the day?
Has your asthma interfered with your usual daily activities (eg, school, work, housework)?
Also Asthma Control Test / Mini Asthma Quality of Life Questionnaire
Can be used for patient self-assessment in advance of appointment
what are the causes of treatment failure
Inhaler Technique
Widespread non-adherence to traditionally prescribed regular ‘preventer’ medicines, particularly ICS monotherapies
Intention v Non-intentional
Lack of observed or perceived benefit
Practical factors (capacity, resources, opportunity)
Patient self-reporting simple and useful in most circumstances → May overestimate adherence
Failure to respond to treatment in the absence of non-adherence should be referred to a specialist -> Possibility of incorrect diagnosis