Physiology Terminology
Functions of the Skeletal System
Support: Provides a framework that supports the body’s structure and holds it upright. Certain bones give the body its shape and help bear weight.
Protection: Shields vital organs, such as the brain (skull), heart and lungs (rib cage), and spinal cord (vertebrae).
Movement: Works with muscles to facilitate movement by acting as levers. Joints allow bones to move in specific directions, helping with everyday actions
Mineral Storage: Stores minerals such as calcium, phosphorous, magnesium, sodium, and potassium, that are essential for various body functions. When the body needs those minerals, bones release them into the bloodstream.
Blood Cell Production: Inside some bones, especially in the bone marrow, the body produces red and white blood cells (hematopoiesis). Red blood cells carry oxygen and white blood cells fight infections.
Fat Storage: Yellow bone marrow stores fat as an energy reserve.
Main Divisions of the Skeleton
- Axial Skeleton
Description: The central core of the skeleton, consists of 80 bones.
Components: Skull, neck, trunk, hyoid bone, vertebral column, thoracic cage (rib cage) - 12 pairs, and sternum
Function: Provides support and protection for the brain, spinal cord, and vital organs, and serves as the body's central framework.
- Appendicular Skeleton
Description: The part of the skeleton that supports the limbs, consists of 126 bones.
Components: Arms (humerus, ulna, radius), shoulder girdle (scapula and clavicle), legs (femur, tibia, fibula), pelvic girdle (hip bones), phalanges
Function: Facilitates movement by anchoring the limbs to the axial skeleton and providing attachment points for muscles involved in motion.
Types of Bone Shapes
1. Long Bones
Description: Longer than they are wide, with a shaft (diaphysis) and two ends (epiphyses).
Function: Act as levers for movement and support body weight.
Examples: Femur, humerus, tibia.
2. Short Bones
Description: Nearly equal in length, width, and thickness, cube-like shape.
Function: Provide stability and support with little movement.
Examples: Carpals (wrist bones), tarsals (ankle bones).
3. Flat Bones
Description: Thin, flattened, and usually curved.
Function: Protect internal organs and provide surfaces for muscle attachment.
Examples: Skull, ribs, sternum, scapula.
4. Irregular Bones
Description: Complex shapes that don’t fit into other categories.
Function: Provide protection, support, and muscle attachment.
Examples: Vertebrae, pelvic bones.
5. Sesamoid Bones
Description: Small, round bones that are embedded within tendons.
Function: Protect tendons from wear and tear, and improve the mechanical advantage of tendons by modifying pressure.
Examples: Patella (kneecap), and smaller sesamoid bones found in tendons of the hands and feet.
Types of Cartilages
Hyaline Cartilage: The most common type, it is smooth and glassy in appearance. It provides support and reduces friction in joints. Found in the nose, trachea, and at the ends of long bones in joints.
Elastic Cartilage: More flexible than hyaline cartilage due to the presence of elastic fibers. It maintains shape while allowing flexibility. Found in the ear and the epiglottis.
Fibrocartilage: The toughest type, it contains dense collagen fibers. It provides strong support and can withstand heavy pressure. Found in intervertebral discs and the menisci of the knee.
Main Categories of Joints
1. Fibrous Joints (Synarthroses)
Structure: Bones are connected by dense fibrous connective tissue.
Movement: Very little to no movement.
Examples: Sutures in the skull, where bones are tightly fused together.
2. Cartilaginous Joints (Amphiarthroses)
Structure: Bones are connected by cartilage (either hyaline or fibrocartilage).
Movement: Allows limited movement.
Examples: Intervertebral discs (between vertebrae), pubic symphysis.
3. Synovial Joints (Diarthroses)
Structure: Bones are separated by a fluid-filled joint cavity (synovial fluid) enclosed in a synovial membrane.
Movement: Freely movable and the most common type of joint in the body.
Examples: Shoulder, knee, hip, and elbow joints.
Types of Joints
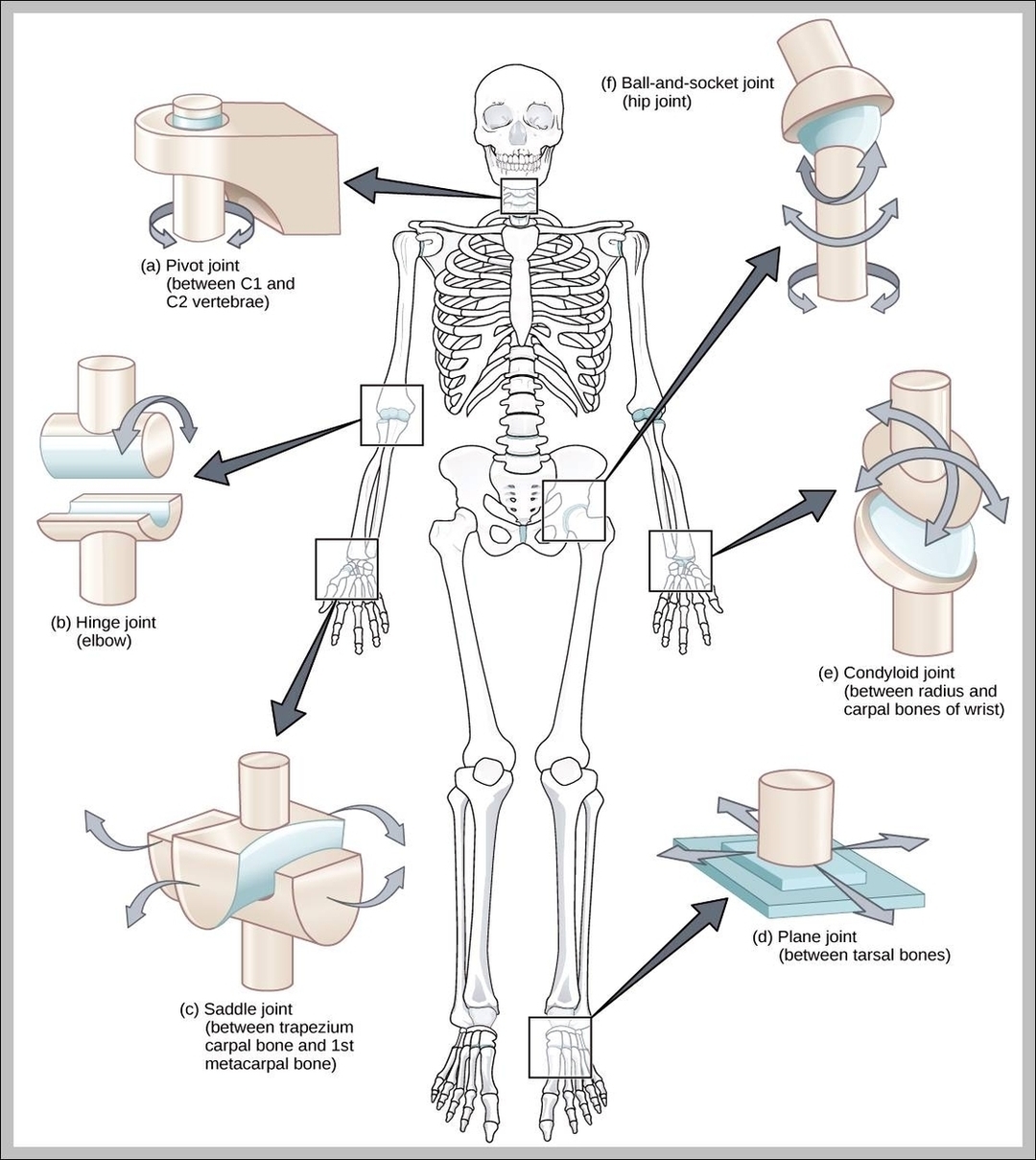
1. Hinge Joint: Allows movement in one direction, like a door hinge. Found in the elbow and knee, allowing flexion and extension.
2. Ball-and-Socket Joint: Provides the widest range of movement, including rotation. Found in the shoulder and hip, allowing movement in all directions (e.g., flexion, extension, rotation).
3. Pivot Joint: Allows rotational movement around a single axis. Found in the neck (between the atlas and axis vertebrae), allowing the head to turn side to side.
4. Condyloid (Ellipsoidal) Joint: Allows movement but no rotation, with a rounded end fitting into a shallow cavity. Found in the wrist and fingers, allowing flexion, extension, and some side-to-side movement.
5. Saddle Joint: Shaped like a saddle, allowing movement back and forth and side to side. Found in the thumb, giving it a wide range of movement.
6. Gliding (Plane) Joint: Allows bones to glide past one another in any direction within the plane of the joint. Found in the small bones of the wrist and ankle.
Anatomy of Long Bone
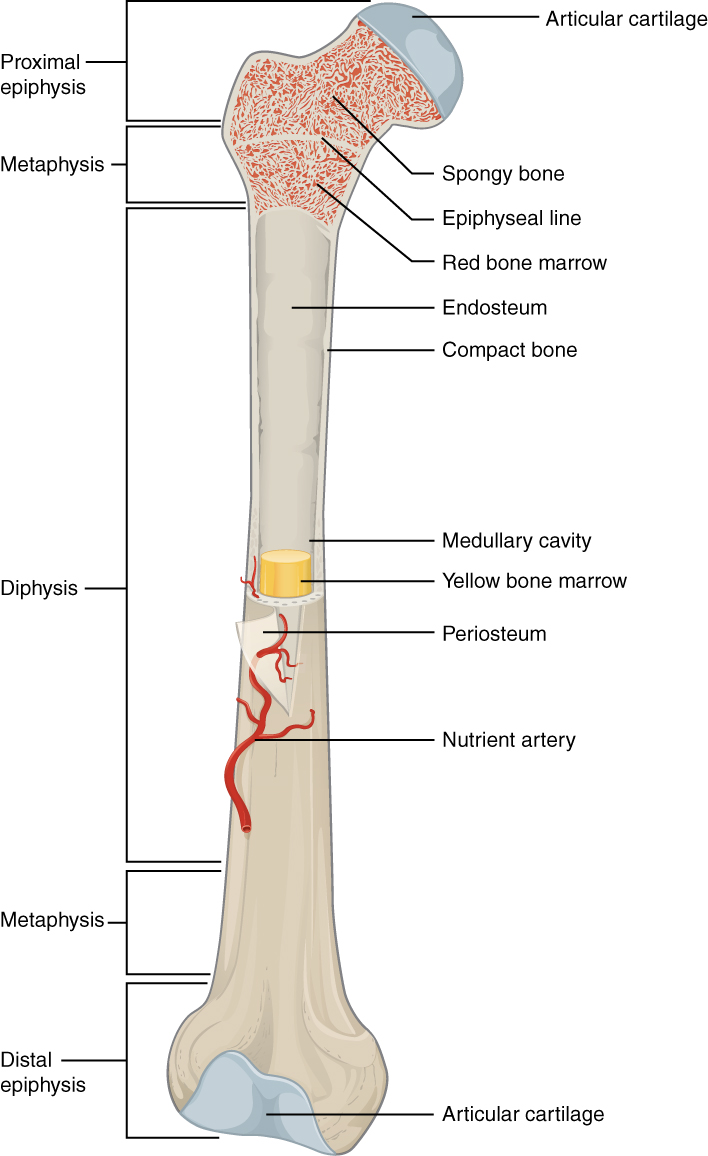
1. Diaphysis (Shaft)
Description: The long, central tubular portion of the bone.
Function: Provides strength and acts as a lever for movement. It is composed mainly of compact bone, which gives the bone its strength.
2. Epiphysis (Ends)
Description: The rounded ends of the bone, located at the proximal and distal ends.
Function: They are mostly made of spongy bone, which contains red bone marrow, and are involved in the formation of joints and articulation with other bones. Covered with articular cartilage to reduce friction in joints.
3. Metaphysis
Description: The narrow region between the diaphysis and epiphysis.
Function: Contains the epiphyseal plate (growth plate) in growing bones, which allows the bone to lengthen during development. In adults, it becomes the epiphyseal line.
4. Periosteum
Description: A tough, fibrous membrane covering the outer surface of the bone, except at joint surfaces.
Function: Contains nerves and blood vessels that nourish the bone. Also involved in bone growth, repair, and providing attachment points for tendons and ligaments.
5. Medullary (Marrow) Cavity
Description: The hollow space inside the diaphysis.
Function: Contains yellow bone marrow in adults, which stores fat. In children, it contains red bone marrow, which is involved in blood cell production.
6. Endosteum
Description: A thin membrane lining the inner surface of the medullary cavity.
Function: Contains cells that help with bone growth, repair, and remodeling.
7. Articular Cartilage
Description: A smooth, white cartilage covering the ends of the epiphyses where they form joints.
Function: Reduces friction and absorbs shock in joints, allowing smooth movement between bones.
8. Compact (Cortical) Bone
Description: Dense, hard outer layer of the bone, primarily found in the diaphysis.
Function: Provides strength and support to the bone, allowing it to withstand weight and forces.
9. Spongy (Cancellous) Bone
Description: Lighter, porous bone tissue located mainly in the epiphysis.
Function: Contains red bone marrow and helps reduce the overall weight of the bone while maintaining structural integrity.
10. Nutrient Artery
Description: A key blood vessel that enters the bone through the nutrient foramen, typically located in the diaphysis. It passes through the compact bone to reach the medullary cavity.
Function: Critical in providing the long bone with essential blood supply and nutrients, promoting bone health, repair, and growth.
11. Epiphyseal Line
Description: A line of bone tissue found in the long bones of adults between the shaft and ends. It forms where the epiphyseal plate (growth plate) used to be during childhood and adolescence, marking the end of bone length growth.
Function: The epiphyseal plate is responsible for bone growth in length. As a person matures, the plate gradually hardens and turns into the epiphyseal line.
Branches of the Nutrient Artery
1. Medullary Branches: These smaller arteries supply the bone marrow and the inner layers of the bone (spongy bone and endosteum).
2. Cortical Branches: These branches extend outward to nourish the compact bone tissue (the hard outer shell of the bone).
Compact vs. Spongy Bones
- Spongy Bone (Cancellous Bone)
Structure: Porous, with a honeycomb-like network of bony plates (trabeculae).
Location: Found mostly in the epiphysis (ends) of long bones and inside flat bones (e.g., pelvis, ribs).
Density: Lighter and less dense than compact bone.
Function: Supports bone marrow, facilitates lightweight support, and absorbs shock.
Blood Supply: Rich blood supply due to proximity to red bone marrow, where blood cells are produced.
- Compact Bone (Cortical Bone)
Structure: Dense and solid, arranged in concentric rings (osteons).
Location: Forms the outer layer of all bones and makes up the diaphysis (shaft) of long bones.
Density: Heavy and very dense, providing strength and protection.
Function: Bears weight and withstands stress, providing structural support.
Blood Supply: Supplied by the nutrient artery, and blood vessels run through small channels (Haversian canals).
Red Bone Marrow vs. Yellow Bone Marrow
- Red Bone Marrow
Function: Produces blood cells (hematopoiesis).
Cell Types Produced: Red blood cells, white blood cells, and platelets.
Location: Found mostly in spongy bone (e.g., in the epiphysis of long bones, pelvis, ribs, vertebrae, and sternum).
Prevalence: More abundant in children; gradually replaced by yellow marrow as we age.
- Yellow Bone Marrow
Function: Stores fat (adipose tissue); can convert to red marrow if the body needs more blood cells.
Production: Does not produce blood cells under normal conditions.
Location: Found in the medullary cavity of long bones, like the diaphysis.
Prevalence: More abundant in adults; replaces red marrow in many bones over time.
Osteoblasts vs. Osteoclasts
- Osteoblasts
Function: Build new bone tissue by producing bone matrix (collagen and minerals).
Role: Involved in bone formation and growth, and help repair bones after injury.
Location: Found on the surface of bones where new bone is being formed.
Outcome: Eventually become osteocytes (mature bone cells) when trapped in the bone matrix.
- Osteoclasts
Function: Break down (resorb) old or damaged bone tissue.
Role: Involved in bone remodeling by removing bone tissue, balancing the work of osteoblasts.
Location: Found on bone surfaces, especially in areas of bone resorption.
Outcome: Release calcium into the blood during bone breakdown.
Role of Osteocytes
Description: Mature bone cells that originate from osteoblasts. Once osteoblasts become trapped within the bone matrix they produce, they differentiate into osteocytes.
Function: Maintain and monitor the bone matrix. They play a role in the exchange of nutrients and waste between the bone and the blood, and they help regulate bone remodeling by signaling to osteoblasts and osteoclasts.
Location: Found embedded within small spaces called lacunae inside the bone tissue.
Significance: They are crucial for maintaining the structural integrity of bone and for bone health over time.
Bone Growth and Repair
- Bone Formation/Ossification (During Development)
1. Lengthwise Growth: Bones grow in length at the epiphyseal plates (growth plates), located between the diaphysis and epiphysis.
Cartilage cells divide and push older cells toward the diaphysis.
These cells then calcify and are replaced by bone tissue, causing the bone to lengthen.
2. Width Growth: Bones grow in width through a process called appositional growth.
Osteoblasts add new bone tissue to the outer surface, while osteoclasts break down bone from the inner surface, maintaining bone strength and shape.
- Bone Repair (After Injury)
1. Fracture Formation: When a bone breaks, blood vessels are damaged, forming a hematoma (blood clot) at the fracture site.
2. Callus Formation: A soft callus made of cartilage forms around the break to provide temporary stability.
3. Hard Callus Formation: Osteoblasts replace the soft callus with a hard callus made of new bone tissue.
4. Bone Remodeling: Over time, osteoclasts break down any excess bone tissue, and osteoblasts continue to reshape and strengthen the repaired bone to restore its original structure.
Body Movements
1. Flexion
Description: Decreasing the angle between two body parts.
Example: Bending the elbow or knee.
2. Extension
Description: Increasing the angle between two body parts, straightening them.
Example: Straightening the arm or leg after flexion.
3. Abduction
Description: Moving a limb away from the midline of the body.
Example: Lifting the arm or leg sideways, away from the body.
4. Adduction
Description: Moving a limb toward the midline of the body.
Example: Bringing the arm or leg back toward the body.
5. Rotation
Description: Movement around a central axis.
Example: Turning the head from side to side or rotating the shoulder joint.
6. Circumduction
Description: A circular movement combining flexion, extension, abduction, and adduction.
Example: Moving the arm in a circular motion (like drawing a circle with your hand).
7. Pronation
Description: Rotating the forearm so the palm faces downward or backward.
Example: Turning the hand so the palm faces the floor.
8. Supination
Description: Rotating the forearm so the palm faces upward or forward.
Example: Turning the hand so the palm faces the ceiling.
9. Dorsiflexion
Description: Lifting the foot upward toward the shin.
Example: Flexing the ankle to point the toes upward.
10. Plantarflexion
Description: Pointing the foot downward away from the shin.
Example: Standing on tiptoes.
11. Inversion
Description: Turning the sole of the foot inward.
Example: Twisting the foot so the sole faces the other foot.
12. Eversion
Description: Turning the sole of the foot outward.
Example: Twisting the foot so the sole faces away from the other foot.
13. Protraction
Description: Moving a body part forward.
Example: Pushing the jaw forward or moving the shoulders forward.
14. Retraction
Description: Moving a body part backward.
Example: Pulling the jaw or shoulders back.
15. Elevation
Description: Lifting a body part upward.
Example: Shrugging the shoulders or closing the mouth.
16. Depression
Description: Lowering a body part.
Example: Dropping the shoulders or opening the mouth.
17. Hyperextension
Description: Movement of a joint past its normal limit of extension.
Example: Tilting the head backward excessively.
Fracture Classification
- Three “either/or” fracture classifications
1. Position of bone ends after fracture
Nondisplaced: ends retain normal position
Displaced: ends are out of normal alignment
2. Completeness of break
Complete: broken all the way through
Incomplete: not broken all the way through
3. Whether skin is penetrated
Open (compound): skin is penetrated
Closed (simple): skin is not penetrated
- Can also be described by location of fracture, external appearance, and nature of break
Fracture Type
Comminuted: bone fragments into three or more pieces
Particularly common in the aged, whose bones are more brittle
Compression: bone is crushes
Common in porous bones, subjected to extreme trauma like a fall
Spiral: ragged break occurs when excessive twisting forces are applied to a bone
Common sport fracture
Epiphyseal: epiphysis separates from the diaphysis along the epiphyseal plate
Tends to occur when cartilage cells are dying and calcification of the matrix is occurring
Depression: broken bone portion is pressed inward
Typical of skull fracture
Greenstick: bone breaks incompletely, much in the way a twig breaks, only one side of the shaft breaks while the other side bends
Common in children, whose bones have relatively more organic matrix and are more flexible than those of adults
Fracture Treatment and Repair (In-Depth)
- Treatment involves reduction, the realignment of broken bone ends, which involves 4 major stages
Closed Reduction: physician manipulates to correct position
Open Reduction: surgical pins or wires secure ends
Immobilization of bone by cast or traction is needed for healing
Time needed for repair depends on break severity, bone broken, and age of patient
Hematoma Formation and Inflammatory Phase
Inflammatory Phase
Various chemical inflammatory mediators are released which recruit inflammatory cells to the fracture site
Mediators attract MSCs (mesenchymal stem cells) to the site and the next stage of healing is initiated
Phagocytic cells (neutrophils and macrophages) are called in to clean up debris and initiate tissue repair
Hematoma Formation
Hematoma (mass of clotted blood) forms at the site of the fracture due to disruption of blood vessels and hemorrhage (blood loss from damaged vessel)
This stage usually lasts for a few days
Soft Callus Formation and Granulation Tissue Formation
Soft Callus Formation
MSCs differentiate into chondroblasts (form cartilage) and osteoblasts (form bone)
A soft callus composed of fibrocartilage and collagen is formed and the fracture gap is bridged by this matrix
Fibroblasts secrete collagen fibers to span break and connect broken ends while chondroblasts produce cartilage
Fibroblasts, chondroblasts, and osteogenic cells begin reconstruction of bone
Create cartilage matrix of repair tissue
Osteoblasts form spongy bone within the matrix
Granulation Tissue Formation
Granulation tissue which is rich in fibroblasts (component of connective tissues) and blood vessels, helps nourish the area and fill the broken gap
These capillaries grow into the hematoma, bringing oxygen and nutrients necessary for bone healing
The soft callus temporarily stablilizes the fracture and allow for the deposition of bone tissue
This stage lasts for a few weeks
Hard Callus Formation and Endochronal Ossification
Hard Callus Formation
Osteoblasts (responsible for bone formation) enter the soft callus and deposit new bone tissue.
New trabeculae (small, bony structures usually in spongy bone) appear in fibrocartilaginous (soft) callus
Soft callus undergoes mineralization and transforms into hard callus, composed of woven immature bone
Endochronal Ossification
A process that involves the transformation of cartilage into bone
Hard callus provides structural stability and bridges the fracture gap
This stage can last several months
Remodeling Phase
Bone Remodeling
Newly formed woven bone is reshaped into its mature and functional structure
Osteoclast resorb excess bone, osteoblasts deposit new bone tissue (bone modeling)
Excess material on diaphysis exterior and within medullary cavity is removed
Compact bone is laid down to reconstruct shaft walls
This stage can take several years with the bone gradually adapting to its mechanical stressors
Factors Affecting Bone Healing
1. Age: Younger people generally heal faster because their bones regenerate more quickly, while older adults may experience slower healing due to reduced cell activity.
2. Blood Supply: Adequate blood flow to the fracture site is essential for delivering oxygen and nutrients needed for healing. Poor blood supply can delay the process.
3. Type of Bone: Larger, denser bones (like the femur) take longer to heal compared to smaller bones (like the wrist).
4. Severity and Location of the Fracture: Complex fractures or fractures in areas with less blood flow (e.g., the hip) may heal more slowly than simple, clean breaks.
5. Infection: If the fracture site becomes infected, it can significantly slow or even stop the healing process.
6. Nutrition: Nutrients like calcium, vitamin D, and protein are critical for bone healing. Poor nutrition can impair the healing process.
7. Smoking and Alcohol: Smoking reduces blood flow and oxygen to the bone, while excessive alcohol consumption weakens bone structure and delays healing.
8. Medical Conditions: Diseases like diabetes, osteoporosis, or vascular disorders can interfere with bone healing.
9. Medications: Some medications, like corticosteroids, can slow down the bone repair process.