CH. 29 - Fetal Development
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
Embryo
term has varied meanings
Some say the fertilized egg or the two-cell stage is an embryo
Others say that an individual becomes an embryo when it is 16 days old and consists of three primary germ layers
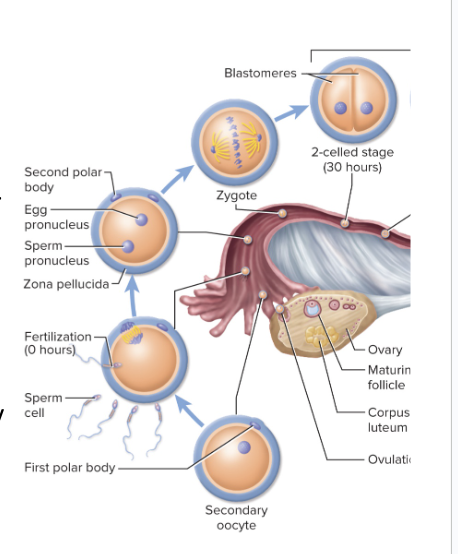
When does the egg have to become fertilized in order to survive?
Egg must be fertilized within 12 to 24 hours of ovulation, if it is to survive
Where must sperm encounter the egg? How many make it the egg and why?
Sperm must encounter the egg somewhere in the distal one-third of the uterine tube
Vast majority of sperm do not make it to egg
Destroyed by vaginal acid or drain out of vagina
Fail to penetrate the mucus of the cervical canal
Destroyed by WBCs in the uterus
Half go up wrong uterine tube
Of the 300 million that were ejaculated, about 200 spermatozoa reach the vicinity of the egg
How long are sperm viable after ejaculation?
Sperm are viable for up to 6 - 7 days after ejaculation
Conception is optimal when sperm are deposited a few days before ovulation to 14 hours after
What happens when the sperm encounters an egg?
When sperm encounters an egg, it releases enzymes needed for one sperm to penetrate the egg
Penetrates granulosa cells, then zona pellucida

Fertilization
Combines the haploid chromosomes from the male and female gamete to form a diploid cell
is synonymous with conception
2 Mechanisms to Prevent Polyspermy
Fast Block
sperm binds to egg which opens up Na+ channels and change the voltage of membrane
This change in polarity electrically repels other sperm from gaining access
Slow Block
involves cortical granules that get exocytsized and form a thick membrane that additional sperm cannot pass through
Meiosis ll
The secondary oocyte begins meiosis II before ovulation, but completes it only once it is fertilized (sperm makes contact with egg)
the final polar body wont be ejected until sperm comes in contact with secondary oocyte
once that final polar body is ejected, it’s an egg for a short time
once the male and female genome mix into one genome, its a zygote
The fertilized egg, now called the zygote, is ready for its first mitotic division
First Trimester
from fertilization through 12 weeks
More than half of all embryos die from natural causes in the first trimester
Conceptus is most vulnerable to stress, drugs and nutritional deficiencies during this time
Second Trimester
weeks 13 through 24
Organs complete most of their development
Fetus looks human
Chance of survival (with intensive care) if born near end of this trimester
Third Trimester
week 25 to birth
Fetus grows rapidly and organs achieve enough cellular differentiation to support life outside of womb
success rate is pretty high
At 35 weeks and 5.5 lb, fetus is considered mature
Pre-embryonic Stage
First 16 days of development (starting at beginning of last menstrual period), ending with the existence of an embryo
Involves 3 major processes
Cleavage
Implantation
Embryogenesis
Cleavage
multiple rounds of divisions that occur in the first 3 days while conceptus migrates down the uterine tube
First cleavage occurs within 30 hours after fertilization
Zygote splits into two daughter cells (blastomeres)
By the time the conceptus arrives in the uterus, it reaches the morula stage
About 72 hours after ovulation
Morula stage—solid ball of 16 cells
Sill no larger than the zygote
Cleavage produces smaller and smaller blastomeres
Morula lies free in uterus for 4 to 5 days
Divides into 100 cells or so
Zona pellucida disintegrates and releases the conceptus, called the blastocyst
Blastocyst
a hollow sphere
made up of the trophoblast and embryoblast
is what actually implants in the lining of endometrium
attaches to uterine wall 6 days after ovulation
Usually on the fundus or posterior wall of the uterus
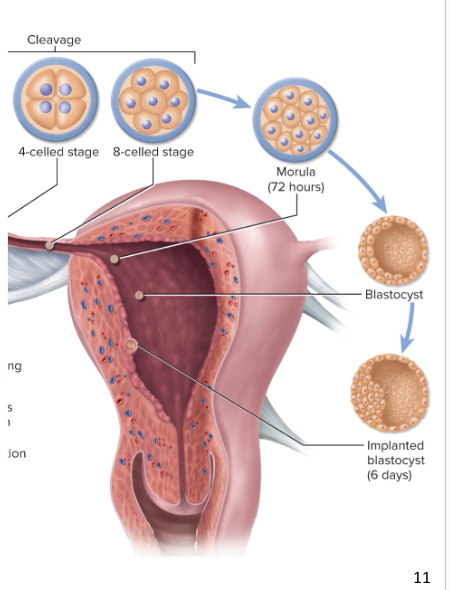
Trophoblast
outer layer of squamous cells
Destined to form the placenta and play a role in nourishment of the embryo
Embryoblast
inner cell mass
Destined to become the embryo
Implantation
process of attachment to uterine wall
Begins when blastocyst adheres to endometrium
cells from blastocyst start to grow into lining of endometrium,
allows for nutritional uptake (endometrium eats up some of the endometrium for nutrients)
Embryogenesis
The arrangement of blastomeres into 3 primary germ layers in the embryoblast
Ectoderm, mesoderm, and endoderm
What do trophoblasts secrete?
they secrete human chorionic gonadotropin (HCG)
HCG stimulates the corpus luteum to secrete estrogen and progesterone
Progesterone suppresses menstruation
keeps endometrium from shedding off by keeping estrogen and progesterone high
HCG levels rise in mother’s blood until end of second month
What does the trophoblast develop into?
Trophoblast develops into membrane called the chorion
chorion takes over the role of the corpus luteum, making HCG unnecessary
Ovaries become inactive for remainder of pregnancy
Estrogen and progesterone levels rise from chorion
Embryonic Stage
begins when all three primary germ layers are present (usually day 16)
placenta starts to grow
forms over the next 6 weeks
Becomes embryo’s primary source of nutrition
organogenesis begins
Organogenesis
germ layers differentiate into organs and organ systems
Organs are present (but not fully functional) at 8 weeks
when the embryo becomes a fetus
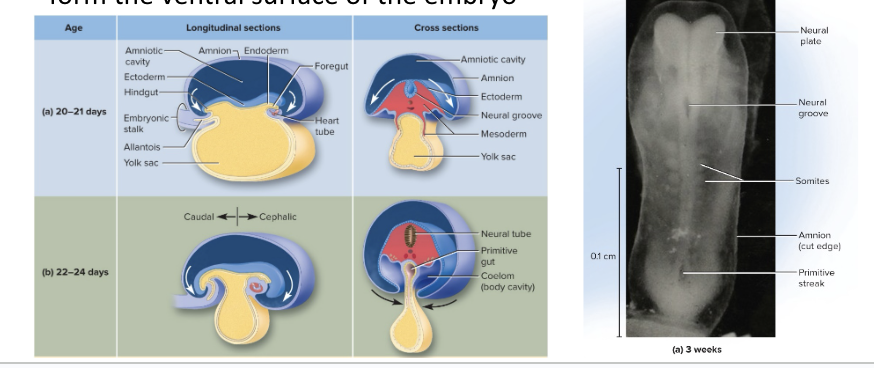
Embryonic Folding
In embryonic stage, the flat embryonic disc is converted into a more cylindrical form
Occurs during week 4
Embryo grows rapidly and folds around a membrane called a yolk sac
yolk sac serves as early blood
Embryo becomes C-shaped, with head and tail almost touching
Lateral margins of the disc fold around the sides of the yolk sac to form the front surface of the embryo
Neural groove forms in the center of this C shaped embryo - is the CNS
As a result of the embryonic folding, the entire surface is covered with ectoderm, and the mesoderm splits into 2 layers
When are all organs present in the fetus?
At 8 weeks
Ectoderm
Outer layer of embryo
Gives rise to epidermis, nervous system, lens and cornea, integumentary glands, internal ear
basically the integumentary and nervous systems
Mesoderm
Middle layer of embryo
2 layers of the mesoderm
One adheres to the ectoderm
The other to the endoderm
Coelom exists in-between
is a cavity between the two layers
gives rise to the skeleton, muscle, cartilage, blood, dermis, lymphoid tissue, gonads and ducts, kidneys and ureters
Endoderm
inner most portion of embryo
forms the tissues and structures that line the tubes that go through our body
Gut and respiratory epithelium and glands, bladder, and urethra
Accessory organs that develop with embryo:
placenta
umbilical cord
4 embryonic membranes:
amnion
yolk sac
allantois
chorion
Amnion
transparent sac that completely enclose the embryo
Penetrated only by the umbilical cord
Fills with amniotic fluid
amniotic fluid is generated by the amnion in the first part of pregnancy
in late pregnancy, it’s produced by the baby’s urinary system
Amniotic Fluid
Protects embryo from trauma, infections, and temperature fluctuations
Allows freedom of movement important to muscle development
Enables embryo to develop symmetrically
Prevents body parts from attaching to each other
Stimulates lung development as fetus “breathes” fluid
At first, amniotic fluid formed from filtration of mother’s blood plasma
Fetus contributes to fluid volume by urinating into amniotic cavity (but fetus also swallows amniotic fluid)
During gestation, the conceptus is nourished in 3 different, overlapping ways:
Uterine milk
Trophoblastic nutrition
Placental nutrition
Uterine Milk
glycogen-rich secretion of the uterine tubes and endometrial glands
Conceptus absorbs this fluid as it travels down the tube and lies free in the uterine cavity before implantation
primary source of nutrition during pre embryonic and embryonic stage
Trophoblastic Nutrition
Conceptus consumes decidual cells of the endometrium
Progesterone from corpus luteum stimulates decidual cells to grow
The cells accumulate a store of glycogen, proteins, lipids
As conceptus burrows into the endometrium, the decidual cells are digested
Is the only mode of nutrition for first week after implantation
Remains dominant source through the end of 8 weeks
Decreases as placental nutrition increases
Placental Nutrition
nutrients diffuse from the mother’s blood through the placenta into the fetal blood
Placenta
disc-shaped organ attached to the uterine wall on one side
on the other side, it is attached to the fetus by the umbilical cord
placenta previa - when the placenta covers the external os, so C-section is needed
Placental Phase
the period beginning at week 9
Sole mode of nutrition from end of week 12 until birth
What is developed by the end of 8 weeks?
All organ systems are present
Now considered a fetus
Bones have begun to calcify
Skeletal muscles exhibit spontaneous contractions
Too weak to be felt by the mother
Heart, beating since week 4, now circulates/pumps blood
Heart and liver are very large, forming the prominent ventral bulge
Head is nearly half the total body length
Fetal Development
The fetus is the final stage of prenatal development
From the start of week 9 until birth
Organs mature to support life outside the mother
Unique aspects of fetal circulation:
Umbilical-placental circuit
arteries carry deoxygenated blood to placenta
vein carry oxygenated blood to fetus
Presence of three circulatory shortcuts: shunts
blood bypasses lungs by flowing from right atrium to left atrium
blood also bypasses lungs by flowing from pulmonary trunk to aorta
blood also bypasses the liver
How is blood oxygenated in utero?
blood is oxygenated by the placenta NOT the lungs
placenta serves as a temporary pulmonary circuit
Two Semester Summary
Anatomy is the study of structure
Physiology is the study of function
structure determines function
We maintain internal balance (homeostasis) with negative feedback loops
Too much, or too little of anything is harmful. Moderation is important
Kindness is of lasting value.