Cardiac AP and conduction system
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
[DSA] What are the three general types of cardiac action potentials
Non-pacemaker action potentials, AKA: fast response action potentials
rapid depolarization,
atrial and ventricular myocytes does this
slow response action potentials
slower rate of depolarization
Found in SA and AV nodes
Specialized conducting cells found within the His-Purkinje system
Similar to fast response action potentials but EXHIBIT SPONTANEOUS DEPOLARIZATION
[DSA] List the Differences between Cardiac Action potentials and neural/skeletal muscle action potentials
APs are much longer in cardiac cells
The Role of Ca2+
Nerve/Muscle: depolarization = opening of fast sodium channels.
Cardiac Pacemaker Cells: Ca2+ are involved in initial depolarization phase
Non-pacemaker cells: Ca2+ influx prolongs duration of AP → plateau phase
[DSA] Describe What happen in each Phase in Non-Pacemaker AP
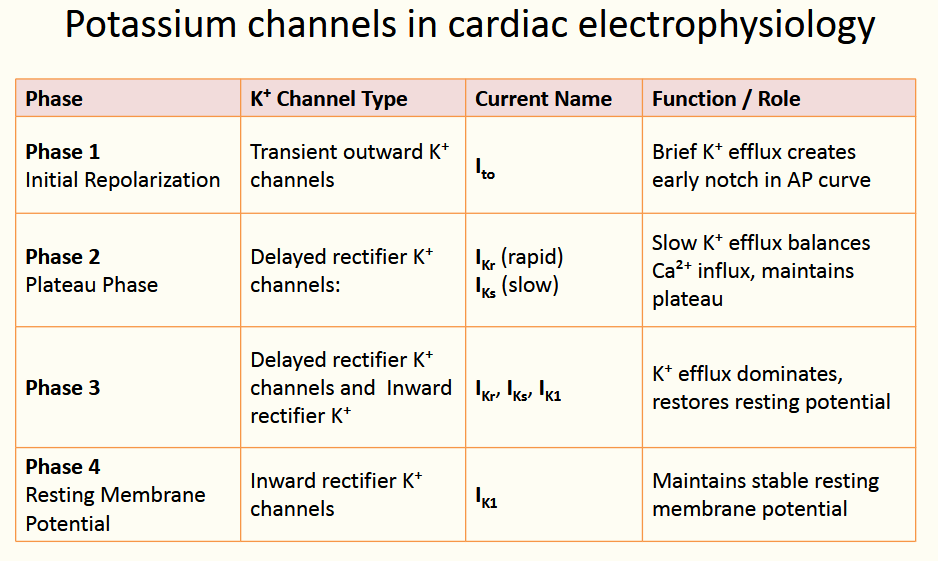
Phase 4: @ resting membrane voltage; K+ is leaking out; Fast-sodium channels/ L-type slow Ca2+ channels = closed → Na/Ca2+ not going in
Phase 0:
Threshold Reached @ -70 → Na+ conductance increases via fast Na channels → Depolarization
K+ conductance decreased due to K+ channels closing
Phase 1:
Short Repolarization due to opening of transient outward K+ channel (Kto)
this is short lived
Phase 2:
@ same time as K+ efflux, Slow Inward Ca2+ influx is occuring via L-type Ca channels
opens @ about -40 mV
Overall → plateau
Phase 3:
Repolarization due to increased K+ efflux coupled w/ inactivation of Ca2+ channels
[DSA] When does the effective refractory period occur in a non-pacemaker cell.
What is the mechanism?
Why is this beneficial?
ERP is during phase: 0,1,2,3 and early 4
Mechanism:
fast Na channels = inactivated following channel closing during phase 1 (see figure).
They are not in their closed, resting (excitable) state until sometime after the membrane potential has fully repolarized
Benefits:
Prevents Multiple APs compounding → affects HR
@ high HRs, heart can’t fill adequately w/ blood → ventricular ejection decreases
[DSA] Describe the Transformation of non-pacemaker into pacemaker cells
In hypoxic events:
membrane depolarizes → closes fast Na+ channels
@ -50mV → slow inward Ca2+ channels open → APs are possible
can display spontaneous depolarization and automaticity
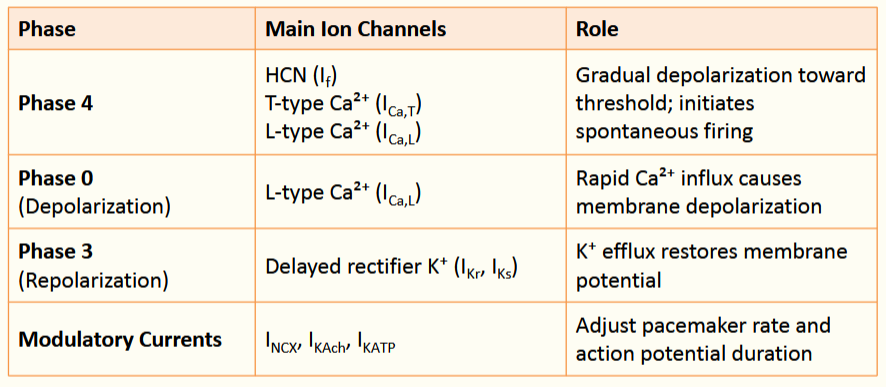
[DSA] Describe the Phases of SA Node Action Potential (pacemaker action potentials)
Phase 4:
slow, inward Na+ currents → Spontaneous depolarization
Called “funny” currents (If)
@ -50mV → T-type Ca++ channel (T=transient) open → Ca2+ Enters
@ -40mV → L-Type Ca2+ channels open (L= long-lasting) → Ca2+ enters
Phase 0:
Depolarization via L-type Ca++ channels
Funny currents + T-type Ca++ channels are closed @ this time
Phase 3:
Repolarization via K+ channels opening
L-type channels Closed
What are the Primary, Secondary, and Tertiary pacemaker cells
Primary: SA Node
Secondary: AV Node
Tertiary: Purkinje Fibers
***If SA Node fails, AV node take over; Purkinje takes over if AV fails***
***As you go from Primary → Tertiary, the intrinsic rate decreases***
Which specialized cardiac myocytes are specialized for rapid
and regulated conduction
Internodal Pathways (Right Atrium)
Conduct impulses from SA → AV
AV Node Cells
Slow conduction → physiological delay between atrial and ventricular activation
Purkinje Cells (AV Bundle, Bundle of His, Purkinje Fibers)
rapid conduction → synchronized ventricular contraction

[REVIEW] Sequence of electrical activation in the heart

List out the phases of fast-response action potential
Phase 0: Rapid depolarization
Phase 1: Early partial repolarization
Phase 2: Plateau phase
Phase 3: Final repolarization
Phase 4: Resting potential
Describe the two refractory periods present in cardiac myocyte
Absolute / Effective Refractory Period (ERP) (Vm > +30mV):
phases 0, 1, 2, and early phase 3
inactivation of voltage-gated Na⁺ channels via inactivation gate → block new APs regardless of strength
Relative Refractory Period (RRP) (+30mV > Vm ≥ -90 mV):
second half of phase 3 and ends before phase 4
Requires stronger stimulation then usual
What is the significance of the Refractory Period?
Significance of the refractory period:
Ensures that APs propagate in a unidirectional and
coordinated manner through cardiac tissue.Prevents premature re-excitation of recently activated cells
maintain synchronized electrical activity
allowing impulses to travel efficiently
avoid chaotic conduction or reentry
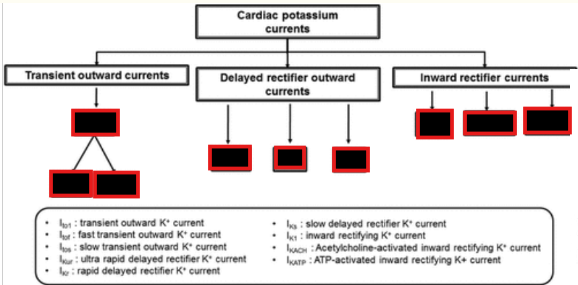
List out the roles of K+ channels in cardiac electrophysiology? Clinical Importance?
K⁺ channels are essential for:
Shaping the action potential waveform
Controlling repolarization and refractory periods
Maintaining resting membrane potential
CLINICAL IMPORTANCE:
K⁺ channels are targets for many cardiac drugs
used to treat arrhythmias and regulate heart rate and rhythm
Describe KAcH and KATP:
Function?
Mechanism?
KAch:
primarily active in atrial myocytes and play a minimal role in ventricular cells
open during late Phase 3 and early Phase 4 → increases K+ conductance → shortens atrial AP and hypolarizes membrane
KATP:
ATP-dependent K⁺ channels that link cellular metabolism to membrane excitability.
Open when Low intracellular ATP levels →K⁺ efflux→ membrane hyperpolarization.
helps protect the heart during metabolic stress by reducing excitability and conserving energy.
List out the phases of pacemaker APs

Describe Funny Currents:
AKA?
Type?
Why is it called funny?
Na+ inward current: Funny Current (If) Channels:
Hyperpolarization-activated cyclic nucleotide-gated (HCN)
are on selective cation channels permeable to Na⁺ and K⁺
Primarily Na
Called Funny because:
activate during hyperpolarization
modulated by cyclic AMP (cAMP)
What are there none of @ SA/AV nodes (hint: channel)
NO fast Na+ channels in the SA and AV nodes
Describe the Refractory period in pacemaker cells as opposed to non-pacemaker cells
Refractory period in pacemaker cells:
Refers to the continuous recovery of excitability during the action potential
around the early part of phase 4
includes the time needed for ion channels to reset after repolarization is complete
recovery of full excitability is a slower process than in "fast-response action potentials, which ensures a steady, regular rhythm
What is a normal HR called?
Define:
Tachycardia
Bradycardia
Normal HR: normal sinus rhythm
Tachycardia: HR > 100 bmp
Bradycardia: HR < 60 bpm
[REVIEW] Regulation of the heart and vasculature via autonomic, hormonal, and local factors

In regards to the heart, what does parasympathetic innervation primarily influence?
What about sympathetic innervation?
Para: vagus nerve primarily innervates the SA and AV nodes, influencing heart rate.
Sympathetic: mainly target cardiac muscle (controlling contractility),
with limited input to pacemaker cells
Describe how NE and AcH affect the heart
How do they interact w/ another?
NE:
via B1-AR
positive chronotropic (↑HR),
positive dromotropic (↑conduction velocity)
positive inotropic (↑contractile forces)
AcH:
via M2 receptors
negative chronotropic,
negative dromotropic,
negative inotropic
How NE and AcH interacts w/ each other:
crosstalk between systems modulates cardiac activity by competing for second messengers (cAMP)
Cardiac myocytes have adrenergic and cholinergic receptors
Describe how Autonomic input influences pacemaker activity
Autonomic input modulates this rhythm:
Vagal input reduces SA node firing
Sympathetic activation raises heart rate, especially during activity
SA Node Also influenced by:
hormones, ion concentrations, hypoxia, drugs, and age
Describe the mechanism on how the parasympathetic system influences pace maker cells
Net Effects?
Parasympathetic regulation: via M₂ receptors
Postganglionic → AcH → M2
Reduces cAMP:
↓ If (funny current) → slower Phase 4 depolarization
↓ ICa,L → reduces Ca²⁺ influx
Both above reduces steepness of Phase 4
↑ IK,ACh → increases K⁺ efflux, hyperpolarizing the membrane
Hyperpolarizing membrane = maxing diastolic potential more negative
Net Effects:
Slower heart rate (SA node)
Reduced conduction velocity (AV node)
More negative maximum diastolic potential
Less steep pacemaker potential slope
Higher threshold for action potential initiation
Describe the mechanism on how the sympathetic system influences pace maker cells
Net Effect?
Sympathetic regulation: via β₁-adrenergic effects:
Activates B1 → increases cAMP
↑ If in SA node → steeper Phase
4 depolarization↑ Ca²⁺ current in myocardial
cellssteeper Phase 4
lower threshold for action
potential initiation
Net Effect:
Increased heart rate (SA node)
Increased conduction velocity through the AV node
More steep pacemaker potential slope
Lower threshold for action potential initiation