Neurology
1/135
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
136 Terms
Common causes of damage to FCP
Trauma e.g. surgery or facial injury
Acoustic neuroma (non cancerous tuma)
Motor Neurons Disease (most common for SLTs)
- Mixed damage of lower motor neurons and upper motor neurons
Cranial nerves associated with speech and swallowing
V Trigeminal
VII Facial
IX Glossopharyngeal
X Vagus
XII Hypoglossal
Other cranial nerves, significant but not vital, for eating and drinking
I Olfactory (smell)
II Optics (food looking attractive)
XI Accessory (Keeping head upright)
V Trigeminal
Sensory and Motor -
S= Facial, nasal and oral mucosa M= muscles of mastication
VII Facial
sensory and motor,
S=Anterior 2/3rd of tongue (taste)
M= lip and buccal tension, muscles of the lower face (lower branch)
IX Glossopharyngeal
Sensory and Motor.
S= Posterior 1/3rd of tongue
M= swallow reflex, elevation of pharynx, gag reflex
X Vagus
Sensory and Motor.
S= Airway protection and coughing
M= Soft palate, palatoglossus (extrinsic tongue muscle), velum elevation, closure of VFs, oesophagus
XII Hypoglossal
Just Motor - All intrinsic muscles of the tongue, and all extrinsic (beside palatoglossus)
V, VII IX, X, XII Cranial nerves have there origin in ...
the pons (V-VII) or medulla (IX-XII)
All part of the hindbrain
"Swallow centre" in the brain stem
nucleus tractus solitarius
AND
Nucleus ambiguous
Primary motor cortex and primary somatosensory cortex located at...
Precentral gyrus (motor)
Postcentral gyrus (somatosensory)
V, VII (upper), IX, X are innervated:
VII lower and XII are innervated
Bilaterally
VII Facial lower branch and XII Hypglossal are contralaterally innervated
If there is unilateral cortical damage, CN V, VII (upper), IX, X will be...
Okay - The non effected side of the cortex will need a bit of time, but will eventually be able to pick up the slack for the other side.
If there is cortical damage to VII (lower) or XII there would be...
Hemiplegia, contralateral to the side of the lesion as these cranial nerves are unilateral.
Strokes will effect these CN the most. Hence stroke victims often have drooped faces, swallowing and tongue difficulties.
Damage to final common pathway/lower motor neurons (LMNs)
Flaccidity/reduced tone
Flaccid Dysarthria
Fasciculations (twitching)
Atrophy
LMN damage
hypotonia/flaccidity/atrophy
UMN damage
hypertonia/spasticity
Speech motor system:
1) final common pathway
2) direct activation pathway,
3) indirect activation pathway,
4) control circuits
5) Motor programmer
1. Oral Preparatory Phase
when food is manipulated in the mouth and masticated if necessary, reducing it to a consistency ready for swallow
CN I/II prepare for eating. Smell, look.
Afferent nerves send information about consistency of food (V, VII, IX) to sensory cortex. Tongue muscle send taste (VII, IX) information. Salivation triggered (IX)
Efferent nerves control lip seal (VII), mastication (V)
2. Oral phase
Lip seal. Buccal engagement. Anterior to posterior "stripping".
Afferent informs brain of location of bolus (V, VII, IX, XII)
Efferent buccal musculature (VII) engaged. Anterior-posterior stripping (X, XII) of bolus to pharynx.
3. Pharyngeal stage
Swallow triggered when bolus reaches faucial arches. Velum elevates. Larynx elevates. VF and epiglottis close. Cricopharyngeal sphincter opens. Pharyngeal constrictors innervated.
Afferent - all relay somatosensory information which dictates autonomic and motor controls.
Efferent - Velum elevates (X), larynx elevated by complex movements (V, VII, XII), VF/Epiglottis close (X).
4. Oesophageal phase
Stage begins once bolus has gone through the cricopharyngeal sphincter.
Pushed down sequentially through contractions of oesophagus. Innervated by Glossopharyngeal and Vagus (IX, X)
Faucial arches
opening of oropharynx by soft palate and base of tongue. Triggers swallow when bolus reaches.
Four stages of swallowing
1. oral preparatory,
2. oral,
3. pharyngeal,
4. oesophageal
1. Final Common Pathway
Lower motor neurons. Part of the PNS, comprises lower motor neuron system in the form of cranial nerves
2. Direct activation pathway
Upper motor neurons.
Sometimes referred to as pyramidal tract.
Part of the descending tract (Brain-Spinal cord)
Damage to direct activation pathway...
Increased tone/spasticity
Weakness
Dysarthria
Bilateral damage = spastic dysarthria
Unilateral damage = upper motor neuron dysarthria (milder form)
3. Indirect activation pathway
Upper motor neurons.
Sometimes called extra-pyramidal tract.
Functions for speech poorly understood.
Damage to indirect activation pathway...
Spasticity and hyperreflexia.
Bilateral damage = spastic dysarthria
Unilateral damage= upper motor neuron dysarthria (milder form)
4. Subcortical structures
basal ganglia, cerebellum (important to SLTs)
Others less important to us:
thalamus, hypothalamus, hippocampus, amygdala
Basal ganglia and speech
Exact function of individual components of BG not understood well.
As a group they help regulate posture, muscle tone, static muscle contraction, velocity, amplitude and initiation of movement.
Damage to basal ganglia
Presentation:
- Hypokinesia
- Hyperkinesia
- Dysarthria
Causes
- Parkinson's Disease PD (Hypokinetic Dysarthria)
- Huntington's Disease HD (Hyperkinetic Dysarthria)
hypokinetic vs hyperkinetic
damage to basal ganglia effecting movement.
Hypokinetic = reduced movement
Hyperkinetic = involuntary excess movement
Cerebellum and speech
Posture and movement. Interacts with direct and indirect activation pathway to coordinate muscle groups for motor speech.
nystagmus
Involuntary rapid eye movements
intention tremor
involuntary trembling when an individual attempts a voluntary movement
Dysmetria
inability to control the distance, power, and speed of a muscular action
hypotonia
reduced muscle tone or tension
Damage to cerebellum
Coordination issues.
Dysmetria - Inability to control distance, speed and range of motion necessary to perform coordinated movements Nystagmus - Repetitive and involuntary movement of eyes
Intention tremor - Tremor during intense activities such as handwriting or speaking
Hypotonia - Decreased muscle tone
Ataxic dysarthria - distinctive motor speech disorder associated with damage to the cerebellar control circuit
Ataxic Dysarthria
Results from damage to cerebellar system. Articulatory & prosodic (rhythm) problems
5. Motor programming
Developing a plan to organise and coordinate speech movements.
Localisation - language dominant hemisphere, sensory and motor cortices, premotor cortex
Damage to motor programming stage
Apraxia of Speech (AOS) - As the main Motor Speech Disorder MSD
- Left/dominant hemisphere, near Brocas area.
- Someone with Brocas Type Aphasia may also have an companying MSD in form of AOS
perisylvian fissure
Peri=about or around
Therefore around the sylvian fissure.
Divides Broca's and Wernicke's areas
Dysarthria
neuromuscular speech disorder upper/lower MN.
Consistent errors, weakness, spasticity, or involuntary movements.
apraxia of speech
impairment in the ability to program movements caused by CNS damage.
Not necessarily weak, flaccid or spastic.
Inconsistent errors
May be able to produce spontaneous speech, but struggle when planned.
Groping for a sound they cant make.
Aphasia
impairment of language, not just articulation. usually caused by left hemisphere damage.
middle cerebral artery (especially left)- importance for speech and language?
supplies the left middle brain where language and speech areas are.
Strokes involving the MCA - likely impact communication
progressive neurological disorders
Deteriorates over time e.g. MND, Alzheimer's, Parkinson's
Non-progressive neurological disorder
Will either improve slightly/completely, or remain static in effect.
cerebrovascular accident CVA
stroke, lack of blood supply to the brain causing brain damage.
Occupy 20% of acute hospitral beds.
4th largest cause of death in the UK.
Risk factors for cerebrovascular accident
Hypertension (high BP)
Heart disease (including myocardial infarction - heart attacks) and atrial fibrillation (irregular and abnormally fast heart rate)
Family history
Cholesterol
infarct
Area of dead tissue after a lack of blood supply
myocardial infarction
heart attack
atrial fibrillation
irregular and abnormally fast heart rate
Ischaemic CVA
Most common CVA - 85%.
blood vessel occlusion from atherosclerotic thrombus or embolus
haemorrhagic CVA
Less common CVA - 15%.
bursting of blood vessels
embolism
the sudden blockage of a blood vessel by an embolus. Forms elsewhere then travels to the brain
thrombosis
abnormal condition of a blood clot - forms inside the brain and blocks there
Circle of Willis
A circle of arteries at the base of the brain that supply blood to the brain
Provide a fail safe for ischaemic strokes, if one part blocks it can be reached by other wys.
Circle of Willis inflowing arteries...
Internal Carotid Artery
Vertebral Artery
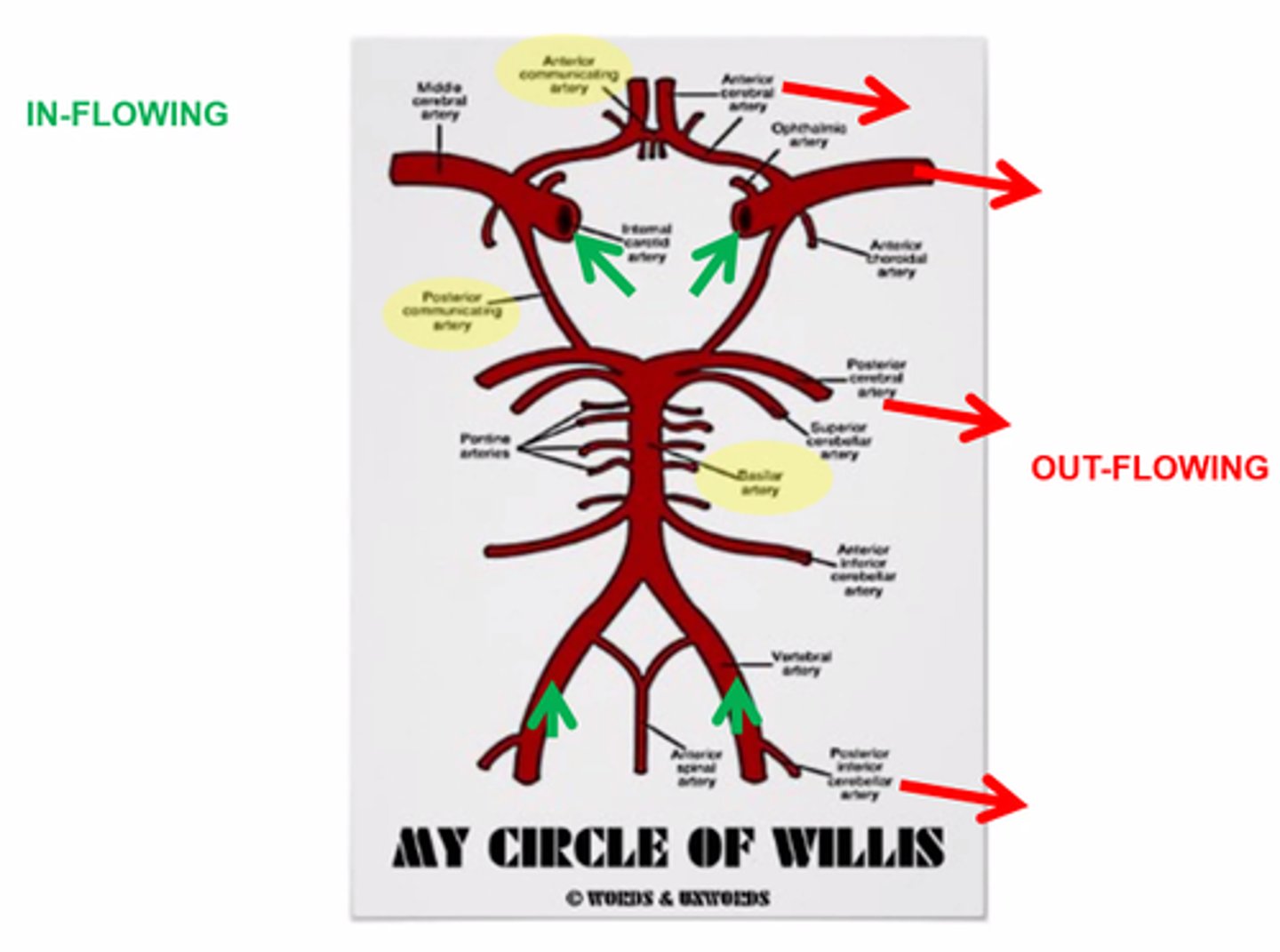
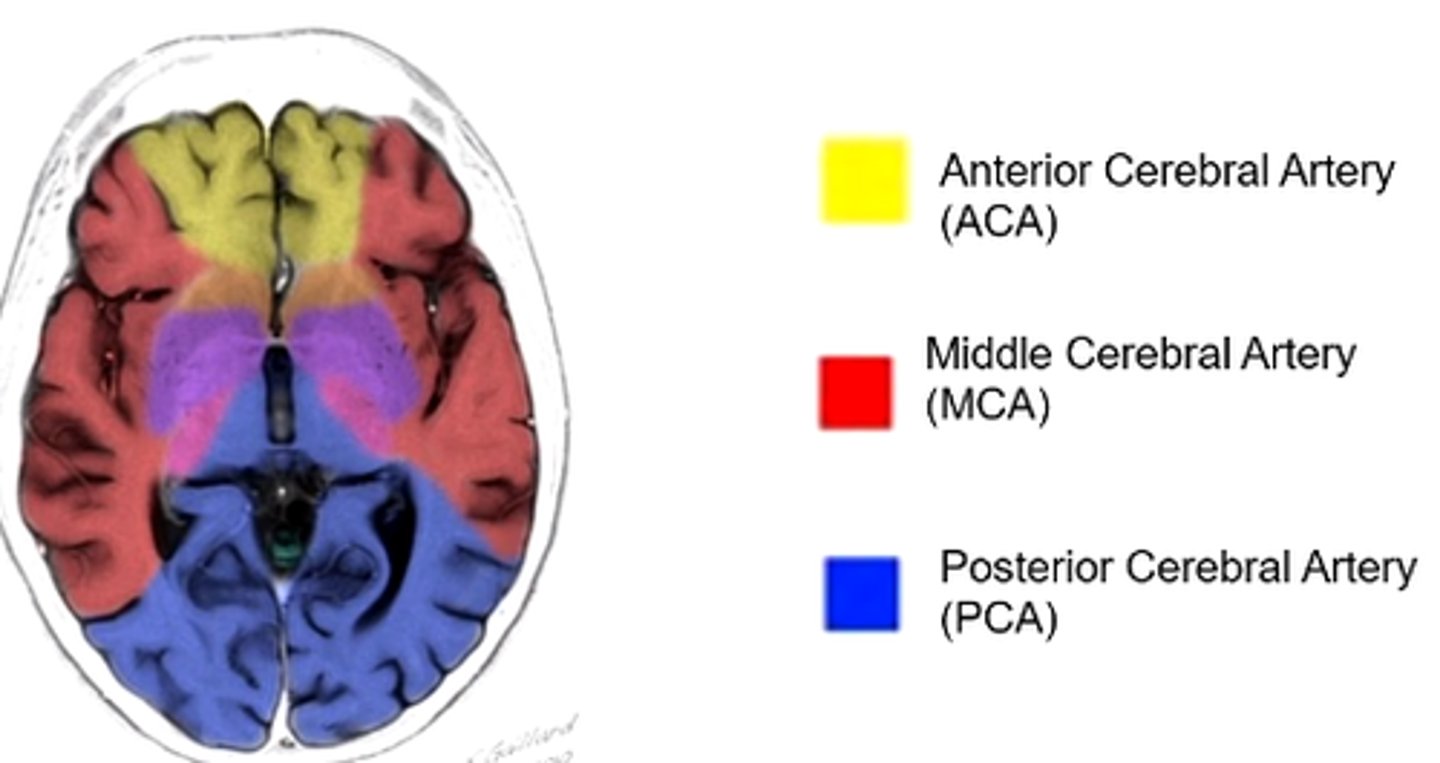
Circle of Willis outflowing arteries...
Anterior Cerebral Artery (ACA)
Middle Cerebral Artery (MCA)
Posterior Cerebral Artery (PCA)
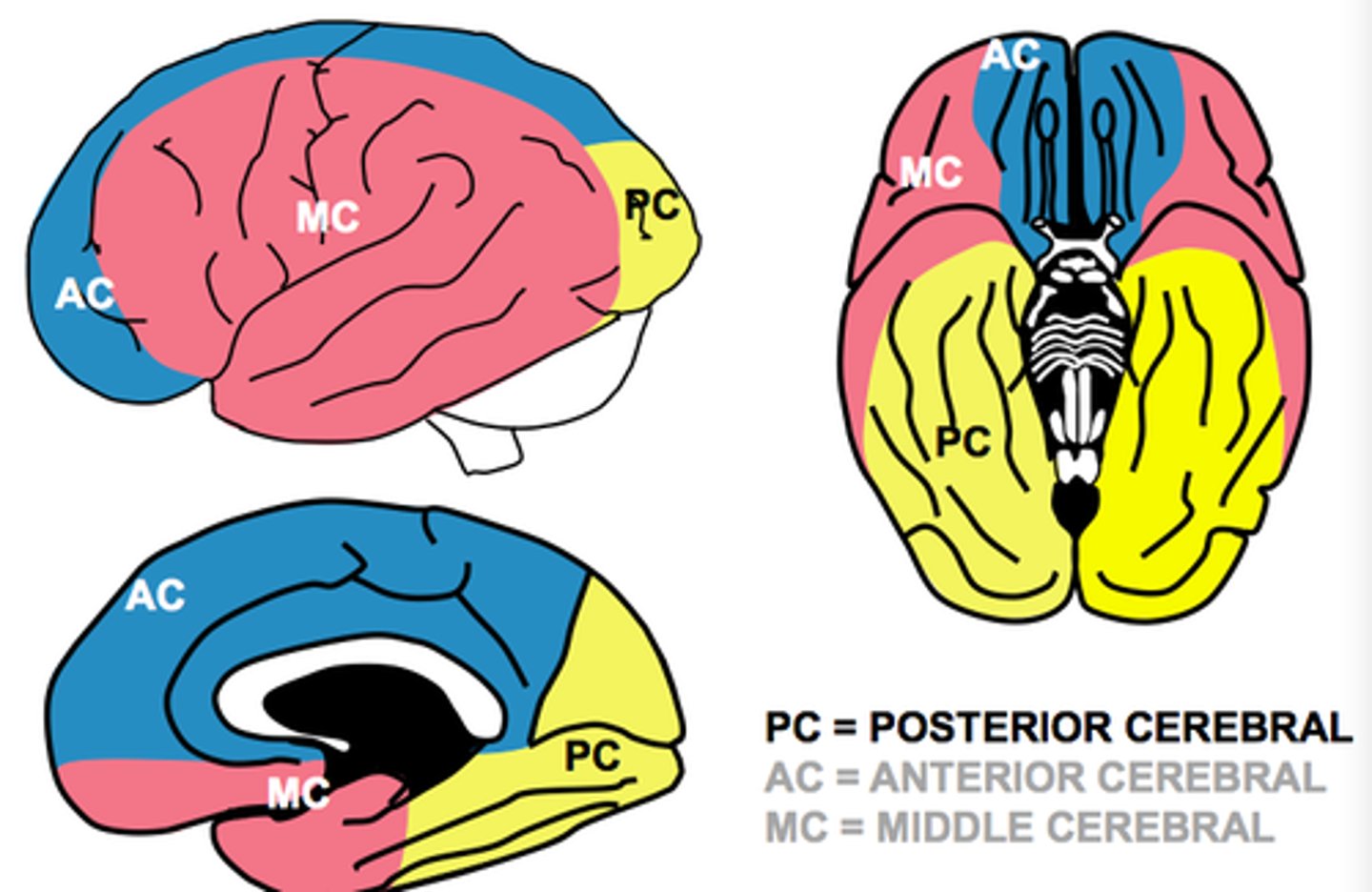
Blood supply to lateral surface of brain
Mostly middle cerebral artery, with ACA to the anterior and PCA to the posterior
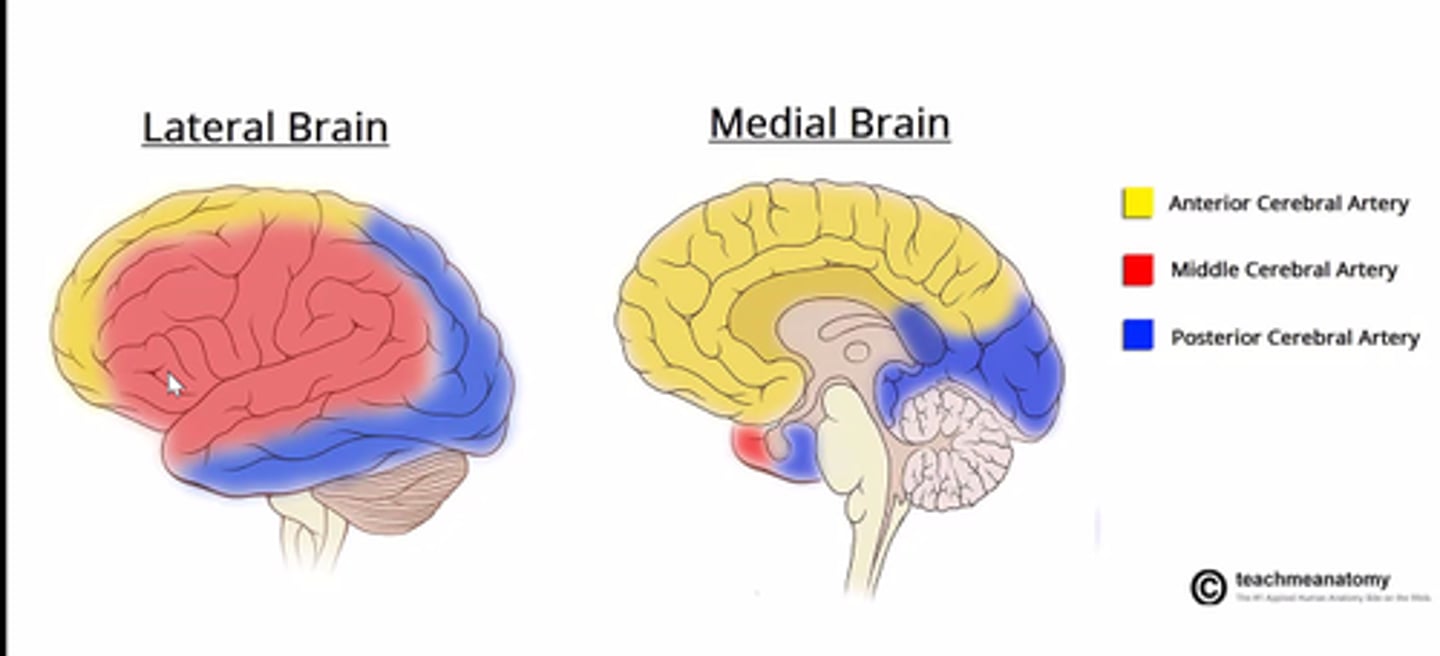
Blood supply to medial part of brain
mostly ACA, with PCA to posterior
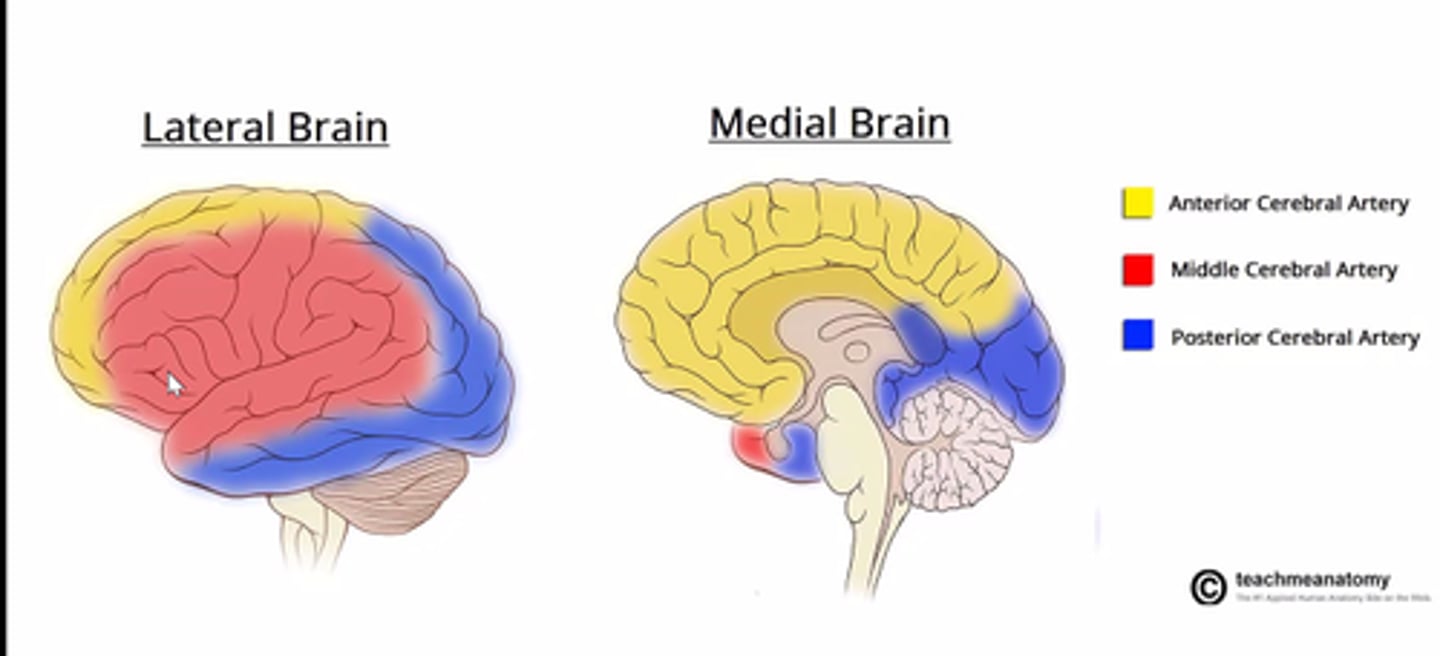
Blood supply to brain when looking axially
ACA to anterior, MCA to sides, PCA to posterior
Four types of Oxford Classification System strokes and why is it used
1- Total Anterior Circulation Syndrome (TACS)
2- Partial Anterior Circulation Syndrome (PACS)
3- Posterior Circulation Syndrome (POCS)
4- Lacunar Stroke (LACS)
Intends to classify strokes without jargon. Accessible to pts and clinicians.
Based on idea that site and size of lesion will influence presentation and prognosis.
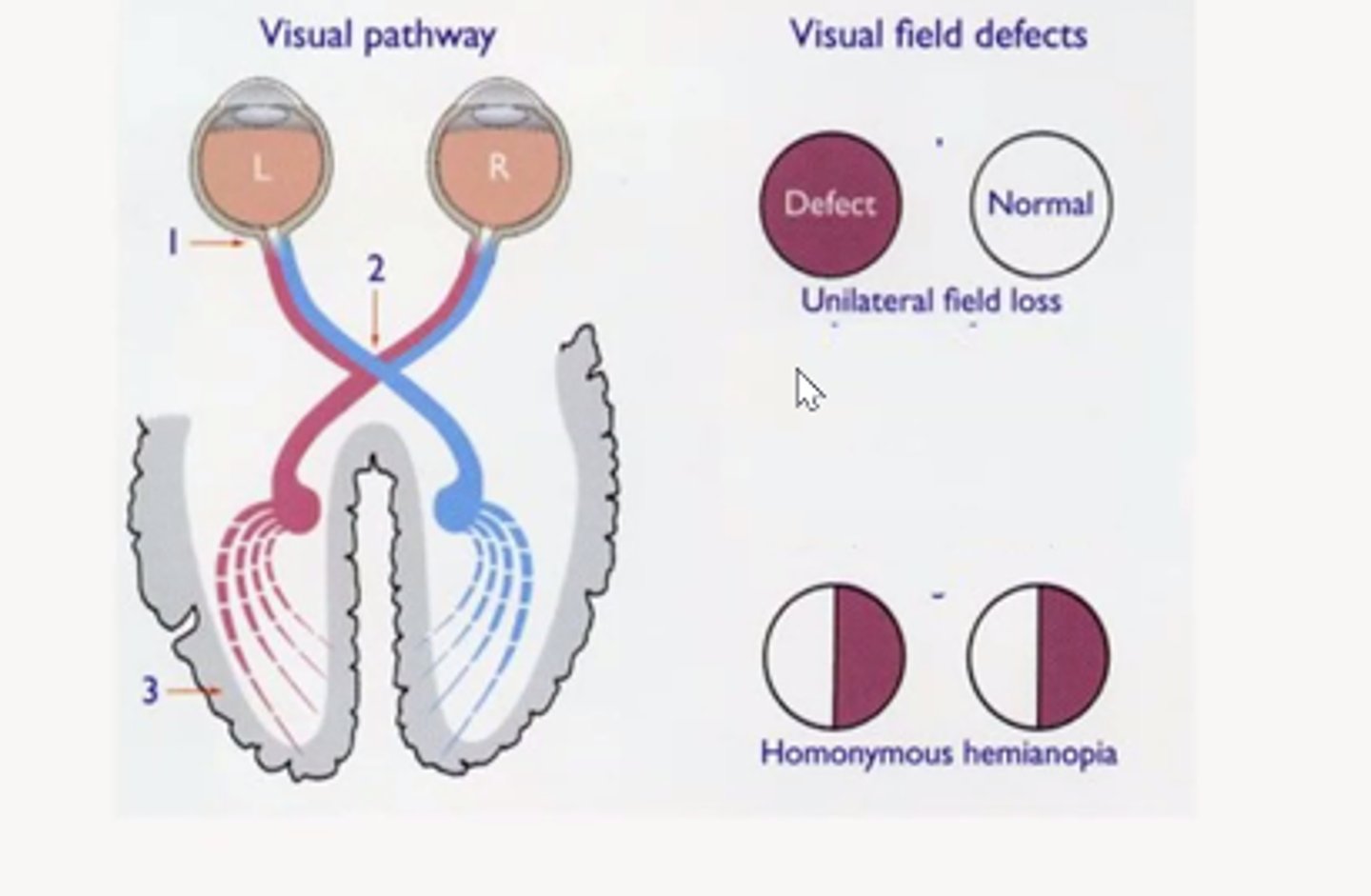
anopia
blindness
homonymous hemianopia
The loss of the right or left half of the field of vision in both eyes. Due to leision at the optic tract/visual cortex of the brain (as left hemisphere of brain controls visual hemfield for right of both eyes and visa versa)
1- Total Anterior Circulatory Stroke (TACS)
Has to present with all 3:
1- Unilateral weakness and/or sensory impairment of face arm and leg
2- Homonymous hemianopia
3- Higher cerebral dysfunction (e.g. aphasia)
MCA and ACA arteries effected.
Prognosis:
- 56% die
- 39% dependent
-4% independent
2- Partial Anterior Circulatory Stroke (PACS)
Has to present with 2 of the 3 features:
1- Unilateral weakness and/or sensory impairment of face arm and leg
2- Homonymous hemianopia
3- Higher cerebral dysfunction (e.g. aphasia)
Only part of ACA effected
Prognosis - 10% don't survive
34% dependent
55% independent
3. Posterior Circulation Stroke (POCS)
One of the following:
1- Cranial nerve palsy and a contralateral motor/sensory deficit
2- Bilateral motor/sensory deficit
3- Conjugate eye movement disorder (e.g. horizontal gaze palsy)
3- Cerebellar dysfunction (e.g. vertigo, nystagmus, ataxia)
5- Isolated homonymous hemianopia
Damage to posterior circulation e.g. cerebellum and brainstem
Prognosis:
14% die
18% dependent
68% independent
4. Lacunar Stroke (LACS)
One of the following:
1- Pure sensory stroke
2- Pure motor stroke
3- Sensori-motor stroke
4- Ataxic hemiparesis
Subcortical stroke that occurs secondary to small vessel disease. No higher cerebral dysfunciton (e.g. aphasia)
Prognosis:
7% die
26% dependent
66% independent
computed tomography (CT)
brain-imaging method using computer-controlled X-rays of the brain
- Easily available
- Quick to complete
- Good for bone and fresh blood
magentic resonance imaging (MRI)
magnetic waves produce images of organs and tissues in all three planes of the body
- More expensive (less availability)
- Takes longer
- Better for brain tissues
- 3 planes
Symptoms for stroke
Hemiplegia, dysarthria, dysphasia, hemianopia, aphasia
anxiety
neglect
agnosia
balance impairments
anticoagulant
prevents blood clotting prior to a stroke e.g. aspirin (not to be used during a stroke)
Used for haemorrhagic strokes
thrombolysis
destruction of a blood clot by breaking it down and dispersing
thrombectomy
surgical physical removal of a blood clot
Traumatic Brain Injury (TBI)
a blow to the head or a penetrating head injury that damages the brain
Half of all deaths in under 40s are caused by TBI
TBI- first injury
- Initial damage to the brain that occurs at the time of damage
Closed
- Skull intact
- Brain not exposed
Open
- Skull integrity
- Brain exposed
Crush
- Head crushed
TBI second injury
- Can occur at dif times after minutes or days/weeks/months
- Lack of oxygen
- Bruising
- Raised intracranial pressure
- Infection
- Formation of blood clots
contusions
bruises
Haematoma
Localised congealed bleeding outside of blood vessels
haemorrhage
excessive bleeding involving blood vessels
Focal Damage (TBI)
- Contusions (may occur opposite side of brain - ricochet)
- intracranial haematoma
- sub dural/extra dural haematomas
- intra-ventricular haemorrhages
intra-ventricular haemorrhages
bleeding into the ventricles of the brain
Brain meniges
layers of protection over the brain
Different layers of meninges
Skin -- > Cranium --> Dura Mater --> Arachnoid Mater --> Pia mater --> Brain
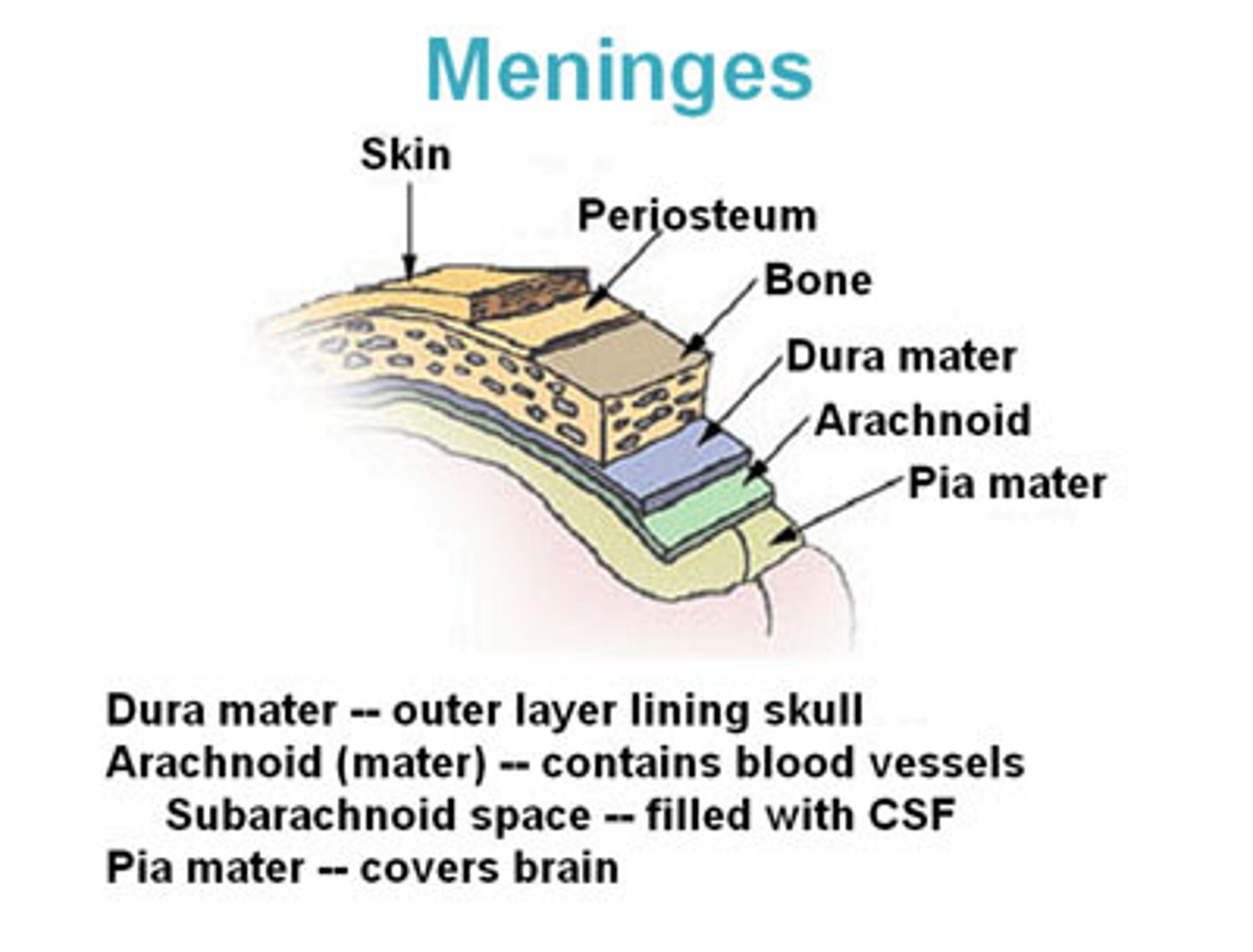
dura mater (hard mother)
thick, outermost layer of the meninges surrounding and protecting the brain and spinal cord
arachnoid mater
weblike middle layer of the three meninges. No blood vessels or nerves.
pia mater
thin, delicate inner most membrane of the meninges with many tiny blood vessels.
TBI symptoms
aphasia, AOS, dysarthria, initial mutism, confused language, naming difficulties, difficulty initiating conversation, reduced word fluency, lack of turn taking, imprecise language, reading and writing problems, comprehension auditory deficits
Treating TBI
reducing secondary complications, airway patent, oxygen therapy, ventilation, surgery, anticonvulsants for epilepsy, monitor closely, treating intercranial pressure, rehabiliation
cerbrovascular accident CVA
aka stroke; ischemic or hemorrhagic; brain tissue dies
neurodegenrative disease
progressive decline in the structure, activity and function of CNS or PNS.
idiopathic
unknown cause
Parkinson's disease aetiology
-Progressive disease of the CNS, mostly effecting basal ganglia
- Loss of dopamine producing neurons in the midbrain
- Idiopathic
basal ganglia
a set of subcortical structures that work together to regulate motor function.
Requires neurotransmitter dopamine
PD characteristics
-Resting tremor - sometimes "Pill rolling"
- Rigidity/hypertonia
-Hypokinesia - leads to reduced facial expressions
- Hypokinetic dysarthria
- Dysphagia
- Language/cognitive issues
- PDD/DLB
Neuropsychiatric symptoms of PD
-Dementia (Parkinson's Disease Dementia/DLB)
- 30% of PD will progress to dementia
- Memory/cognitive changes
- Depression
- Anxiety
- Hallucinations
Hypokinetic Dysarthria
Results from damage to basal ganglia (e.g. PD)
- Imprecise consonants
- Monopitch/monoloudness
- Neurogenic dysfluency (repetition of utterances/words)
- Reduced vital capacity of lungs