Excretion as an example of Homeostatic Control (2)
1/179
Earn XP
Description and Tags
Done
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
180 Terms
What happens to blood as it passes through the sinusoids?
Hepatocytes convert toxic substances into less harmful molecules.
Kupffer cells break down old red blood cells and remove bacteria from the bloodstream.
Describe the outline of the ornithine cycle (all we need to know. Not whole process)
1) Amino acids are deaminated: the amino group is removed, forming ammonia and organic acids. (not ornithine cycle)
2) The organic acids are respired or stored as glycogen.
3) Ammonia is combined with carbon dioxide, which converts it into urea in a cyclical reaction.
4) Urea is released into the bloodstream.
5) It is then filtered by the kidneys and excreted from the body in the urine.
What is excretion?
The removal of metabolic wastes from the body (eg co2)- would cause tissue damage if allowed to accumulate
Excretion maintains homeostasis by keeping substances within a healthy range.
Enables organisms to maintain pH balance and regulate osmotic pressure
\
* bile pigments
\
* nitrogen-containing compounds such as urea
Why is it important to remove metabolic waste products?
To stop toxic products such as CO2 and ammonia building up
The products interfere with cell processes by altering the pH- prevents normal metabolism
Other metabolic products may act as inhibitors- reduces the activity of essential enzymes
\
* liver
\
* lungs
\
* kidneys
What is the kidneys function in excretion?
Removes the urea from the bloodstream to become a part of the urine
Urine is stored in the bladder before being excreted from the body via the urethra
How is hydrogen carbonate formed?
1) CO2 + H2O = H2CO3 (carbonic acid)
The carbonic acid dissociates to release hydrogen ions
2) H2CO3= H^+ + HCO3^-
\
* Can also occur in the blood plasma
What is the skins function in excretion?
Sweat contains salts, urea, water, uric acid and ammonia which are all excretory products
The loss of water and salts is an important part of homeostasis- maintaining body temperature and water potential of the blood
What affect do hydrogen ions have on red blood cells?
1) They affect the pH of the cytoplasm in RBCs
2) The hydrogen ions interact with bonds within haemoglobin, changing its 3D shape
3) Change of the 3D shape reduces the affinity of haemoglobin for oxygen
4) Hydrogen ions can then combine with haemoglobin to form haemoglobinic acid
What affect do hydrogen ions have on blood plasma?
Reduce the pH
Maintaining pH is essential because
Why is it important to maintain the pH of blood plasma?
Changes could alter the structure of many proteins that help transport a wide range of substances around the body
What can happen to the CO2 that isn’t converted into hydrogen carbonate ions?
Can combine directly with haemoglobin to produce carbaminohaemoglobin
\
* Causes an increase in breathing rate to help remove the excess CO2
What is the effect of both carbaminohaemoglobin and haemoglobinic acid?
They are unable to combine with oxygen as normal
This reduces oxygen transport further
What is the livers function in excretion?
Excretes some metabolites as bile
Converts excess amino acids to urea
How are amino acids converted to urea in the liver?
They are broken down by the process of deamination
The nitrogen-containing part of the molecules is then combined with CO2 to make urea
\
* It is then transported mostly in the form of hydrogen carbonate ions to the lungs
\
* In the lungs CO2 diffuses into the alveoli to be excreted as you breath out
Explain the details of the excretion of bile pigmentation
Formed from the breakdown of haemoglobin in the liver
Excreted in the bile from the liver via the small intestine and gall bladder
Explain the details of the excretion of nitrogenous waste products
Formed from the breakdown of excess amino acids by the liver
All mammals produce urea to remove nitrogenous waste
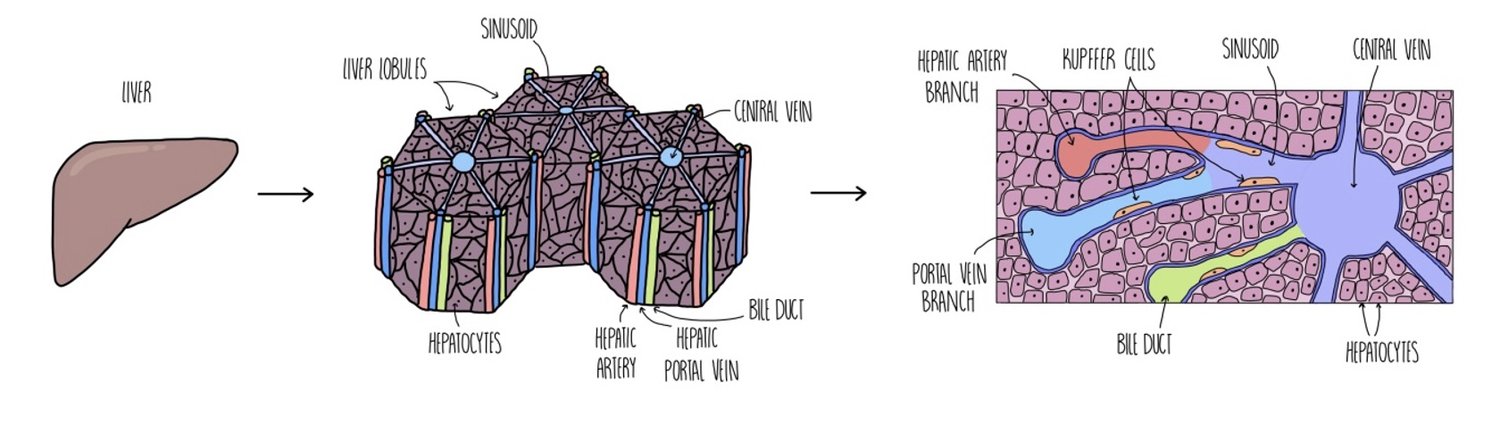
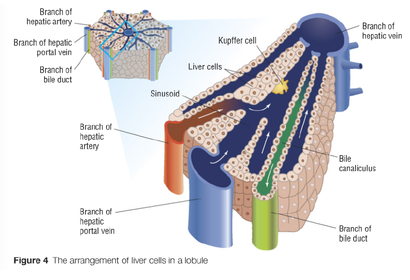
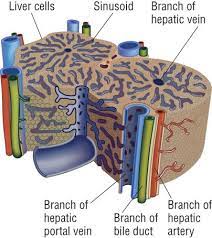
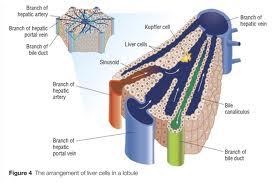
General structure of the liver
Made up of lobes which divide into lobules
Has four vessels
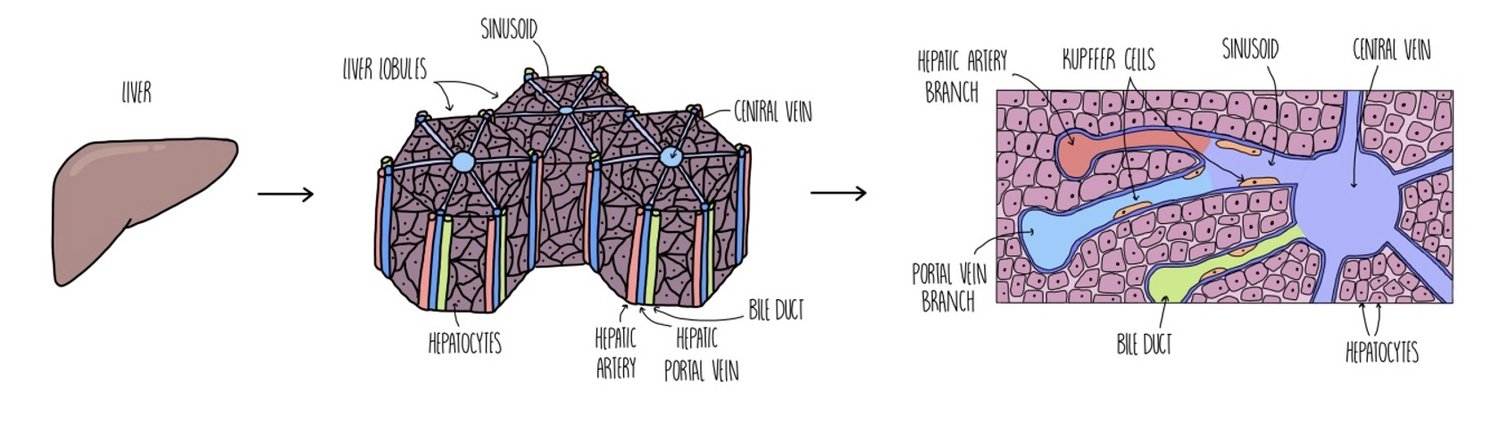
Why are the cells, blood vessels and chambers in the liver arranged the way they are?
To ensure greatest possible contact between the blood and liver cells
\
* hepatic vein
\
* bile duct
\
* hepatic portal vein
Role of the hepatic artery
Supplies the liver with oxygenated blood from the heart- good supply of O2
This supplies O2 that is essential for aerobic respiration
\
* Many of these processes require energy in the form of ATP- Need good supply of O2 for aerobic respiration
What does the Bile duct do?
Carries bile from the liver to the gall bladder
It is stored here until its required to aid the digestion of fats in the small intestine
What is the name for liver cells?
Hepatocytes
Structure of hepatocytes
Large nuclei
Prominent Golgi apparatuses
Lots of mitochondria
Many microvilli on the surface
Dense cytoplasm
What are Inter-lobular vessels?
The smaller vessels that the hepatic artery and hepatic portal vein split into once they enter the liver
They run between and parallel to the lobules
Describe the composition of each liver lobule.
Have a central vein in the middle that connects to the hepatic vein
Many branches of the hepatic artery, hepatic portal vein and bile duct are connected to each lobule
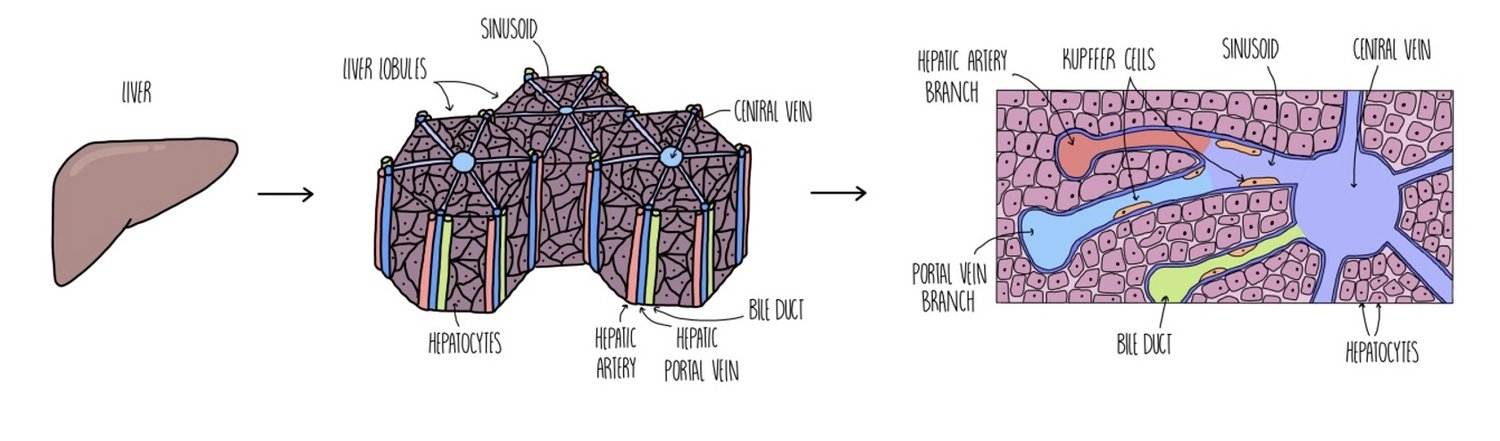
About the Sinusoid
The blood from the hepatic artery and hepatic portal vein is mixed and passes along this chamber
It is lined with liver cells
It contains Kupffer cells
As blood flows along the sinusoid it is in close contact with the liver cells
They have canaliculi
What is the role of liver cells in the liver lobules?
They remove harmful substances and oxygen from the blood that passes past them in the sinusoids
They break down the harmful substances into less harmful substances that then re-enter the blood
Produce and secrete bile into the bile canaliculi
What do the central veins from all the lobules connect up to form?
The hepatic vein
What do the sinusoids connect?
They connect the hepatic artery and the hepatic portal vein to the central vein
Role of Kupffer cells
To breakdown and recycle old RBCs- The haemoglobin of RBC’s is broken down into bilirubin
To ingest foreign particles and help protect against disease
How the vessels are arranged in the lobules
Hepatic artery, portal vein and bile duct are known as interlobular vessels
Interlobular vessels are found on the outside of the lobules
A branch of hepatic veins known as the intra-lobular vessel is found at the centre of each lobule
What are some functions of the liver?
Breaks down amino acids into urea – this involves deamination followed by the ornithine cycle
Detoxifies the blood - alcohol, drugs and hormones in the blood are broken down by the liver - products are excreted in the urine.
Stores glycogen – the liver converts excess glucose into glycogen.
Makes bile – bile aids lipid digestion by emulsifying fats.
Destruction of red blood cells
What is the role of the liver in storing glycogen?
Hepatocytes respond to the binding of insulin to receptors in the cell membrane by converting glucose into glycogen for storage.
Glycogen can then be released when blood glucose levels are low.
\
* Cytochrome P450
The role of catalase in detoxification
Converts hydrogen peroxide to oxygen and water
It has a high turnover* number of 5 million
*the number of molecules of hydrogen peroxide that 1 molecule of catalase can render harmless in 1 second
The role of cytochrome P450 in detoxification
Its a group of enzymes used to break down drugs such as cocaine and medicinal drugs
Their role in metabolising drugs can interfere with other metabolic roles and can cause the unwanted side effects of some medicinal drugs
Where is alcohol broken down?
In the hepatocytes
By the action of the enzyme ethanol dehydrogenase
What is the resulting compound after alcohol is broken down?
Ethanal
This gets broken down further into Ethanoate by the enzyme ethanal dehydrogenase
\
* This is then combined with coenzyme A to form acetyl coenzyme A which enters the process of aerobic respiration
What happens to the hydrogen atoms released from alcohol?
They're combined with a coenzyme called NAD to form reduced NAD
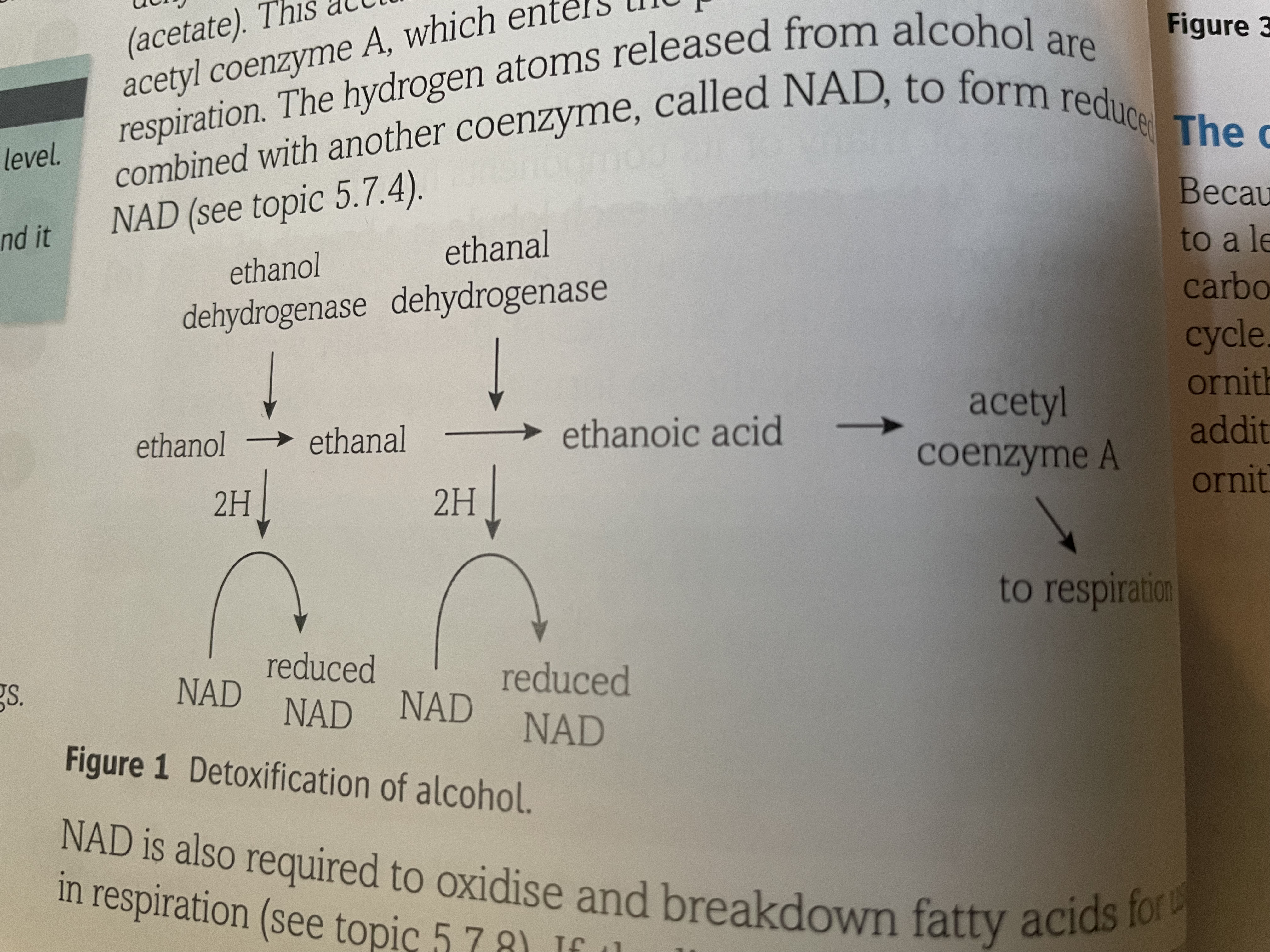
Ethanal -> Ethanoate
Ethanoate + Coenzyme A -> Acetyl coenzyme A
Describe how you get fatty liver
If the liver has to detoxify too much alcohol it uses up its stores of NAD
There are insufficient stores left to deal with fatty acids
The fatty acids are then converted back into lipids and stored as fat in the hepatocytes
This storing causes the liver to become enlarged
Types of reaction that the liver can do to detoxify
Oxidation
Reduction
Methylation
Combination
What 2 processes do amino acids go through to remove and excrete the amino component?
1) Deamination
2) Ornithine cycle
Formation of urea
Amino acid -> ammonia + keto acid
Ammonia+ keto acid → urea
Deamination
Removes the amino group from excess amino acids and produces ammonia
Also produces keto acid which can enter respiration directly to release its energy
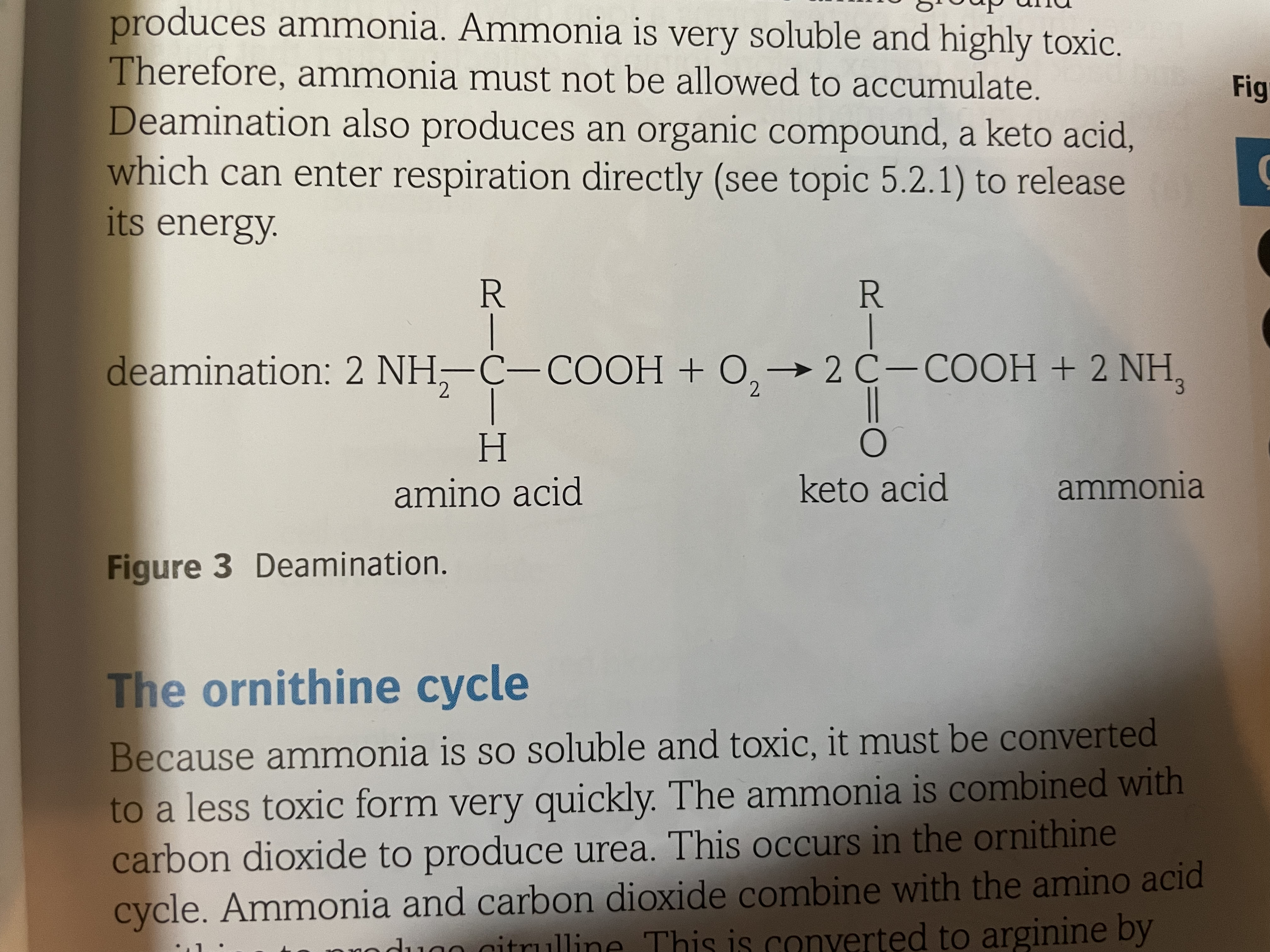
Why do we produce urea instead of leaving it as ammonia?
Its less soluble and toxic
It can be passed back into the blood and transported around the body to the kidneys
What happens to urea in the kidneys?
It is filtered out of the blood and concentrated in the urine
What can keto acids be used for?
Respiration
Lipid storage
Sequence of events in the ornithine cycle (don’t think i need to know this much detail)
1) Ornithine
2) Ammonia in, carbon dioxide in, water out, citrulline is made
3) Ammonia in, water out, arginine is made
4) Water in, urea out, ornithine is made
goes back to the start

Give an overview of how the kidneys excrete waste products
1) Blood enters the kidneys via the renal artery
2) The blood then passes through capillaries in the cortex of the kidneys
3) As it passes through the capillaries, substances are filtered out of the blood -ultrafiltration
4) Useful substances are reabsorbed back into the blood from the tubules in the medulla and cortex- selective reabsorption
5) The remaining unwanted substances pass along the tubules and ureter to the bladder- expelled as urine
6) Filtered blood leaves via the renal vein
What are the roles of the kidneys?
Excretion- they remove waste products(urea) from the blood and produce urine
They also regulate the water potential of the blood (remove excess water, excess ions)
Parts of the structure of the kidney
Capsule (surrounds the 3 regions)
Cortex (outer region)
Medulla (inner region)
Renal vein
Renal artery
Pelvis (centre) which leads into the ureter
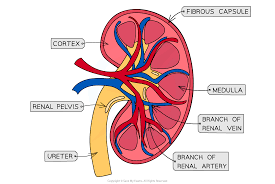
Capsule of the kidney
Hard outer layer of the kidney
Protects against mechanical damage
Medulla of the kidney
Beneath the cortex
Contains the loop of Henle and the collecting duct
Pelvis of the kidney
Where urine is emptied into
Made of connective tissue
Parts of the nephron
Afferent arteriole
Efferent arteriole
Glomerulus
Bowman's capsule
Loop of Henle
Proximal convoluted tubule
Peritubular capillaries
Distal convoluted tubule
Collecting duct
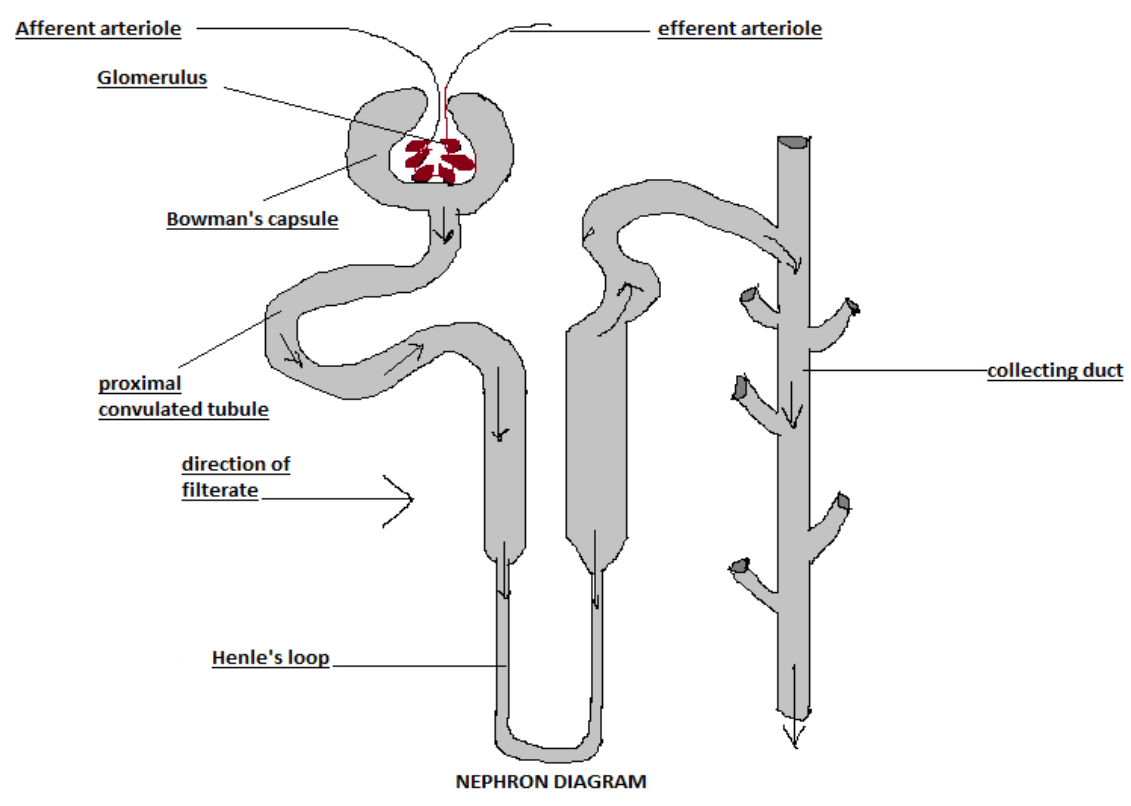
What processes occur in the nephron in order?
1) Ultrafiltration
2) Selective reabsorption
3) Reabsorption of water
About nephrons
Each one starts in the cortex at the Bowmans capsule
The remainder of the nephron is a coiled tubule that passes through the cortex
It then forms a loop down into the medulla and back to the cortex
It then joins a collecting duct that passes back down into the medulla
Which parts of the nephron are in the medulla?
Loop of Henle
Collecting duct
What do the renal arteries split into?
Afferent arterioles- carry blood into the glomerulus
What happens to the blood in the glomerulus?
It continues into an efferent arteriole
The efferent arteriole carries the blood to more capillaries surrounding the rest of the tubule
These capillaries eventually flow into the renal vein
Why might tubules look different sizes down a microscope?
Different planes of cut
Distorted by preparation of the slide
What doesn’t leave the blood during ultrafiltration?
Larger molecules
Proteins
RBC’s
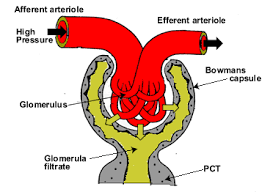
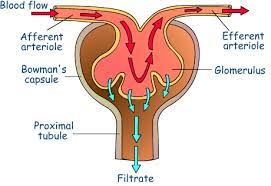
Why is there a high pressure in the glomerulus?
Blood comes in via the afferent arteriole which has a wide lumen
Blood leaves via the efferent arteriole which is narrower
What does the high pressure in the glomerulus lead to?
It forces liquid and small molecules in the blood out of the capillary into the Bowmans capsule
What is the filter?
The barrier between the blood in the capillary and the lumen of the Bowman’s capsule
\
* The basement membrane
\
* Podcytes
Basement membrane
Consists of a fine mesh of collagen fibres and glycoproteins
The mesh acts as a filter to prevent the passage of larger molecules
This means that most proteins and all blood cells are held in the capillaries of the glomerulus
Podocytes
Have many finger-like projections called major processes
On each major process there are minor processes
The minor processes hold the cells away from the endothelium of the capillary
These projections ensure that there are gaps between the cells
Fluid from the blood in the glomerulus can pass between these cells into the lumen of the Bowman’s capsule
What are the 3 parts of the rest of the tubule that the Bowman’s capsule leads to?
Proximal convoluted tubule
Loop of Henle
Distal convoluted tubule
Where does the fluid from the nephrons go?
It enters the collecting ducts which pass through the medulla to the pelvis
The endothelium of the capillary
There are narrow gaps between cells of the endothelium of the capillary
The cells of the endothelium contain pores called fenestrations
The fenestrations allow blood plasma and the substances dissolved in it to pass out of the capillary
Describe the process of ultrafiltration
1) The diameter of the afferent arteriole is wider than that of the efferent arteriole
2) This means the blood in the glomerulus is under high pressure
3) The high pressure forces liquid and small molecules out of the capillary into the Bowmans capsule
4) The fluid is filtered by the 3 layers
5) Filtrate moves into the proximal convoluted tubule
6) Plasma proteins and cells remain in the blood- allows water reabsorption later
What is Ultrafiltration?
Filtration of the blood at a molecular level under pressure