Pediatrics Growth and Development
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
77 Terms
Well Child Exam
Main component is assessment of development
Frequent and routine exams allow a view of a child as they grow and develop
Becoming familiar with development and behavioral issues is essential in pediatric practice
Knowledge of normal development and behavior will allow you to address parental concerns, provide reassurance, and enable you yo provide access to early intervention services
What are the 5 Development Areas?
Gross motor (large muscles): walking, crawling, standing
Fine motor (small muscles in the hand): pinch and hold, grasp with entire hand
Cognition
Thinking, learning, memory, object permanence, attention, construction of knowledge about objects and people
Language
Communication and comprehension of words
Social/Emotional
Interacting with people and environment
Screening Tools Recommendations
Screening tools should be used at 3 selected visits during the first 3 years: typically 9 months, 18 months, and 2-3 years
Allows for us to earlier be able to identify developmental concerns and delays
Screening tools provide a much more accurate assessment of development and can pick up 70% of delays that would have been misses
Developmental Screening: Denver II
Common but older
Screens from birth to age 6
Have 125 tasks in four domains: personal/social, fine motor, gross motor, language
Takes 20 additional minutes to perform
Does not assess socio-emotional development or cognitive development
Developmental Screening: PEDS (Parent’s Evaluation of Developmental Status)
10 questions to parents that provider interprets (parent does in waiting room)
Helps to guide concerns during a well child exam
Questions: concerns about
Child’s learning development/behavior
How your child talks and makes speech sounds
How your child understands what you say
How your child uses his hands and fingers
How your child uses his arms and legs
How your child behaves
How your child gets along with others
How your child is learning to do things for themselves
How your child is learning pre-school or school skills
Anything else
Developmental Screening: PEDS DM (Pediatric Evaluation of developmental screening-developmental milestones)
6-8 item survey focused in each developmental domain
Takes 5 minutes to complete and 1 minute to score
Designed for children age birth -8
Screening: Other developmental tests
Age and stages questionnaire: ages 4-48 months, administered by parent
Battelle Developmental Inventory: ages 0-8 years old, administered by psychologist or developmental MD (usually for someone who has failed initial screen: secondary screening tool)
Bayley Scales of Infant Development II: ages 0-8 years old, administered by psychologist or developmental MD (usually for someone who has failed initial screen: secondary screening tool)
Gross Motor Development: Primitive Reflexes
Involuntary reflexes (have at birth): elicited at newborn well child exams
May help to indicate muscle group coordination and neurologic/CNS function
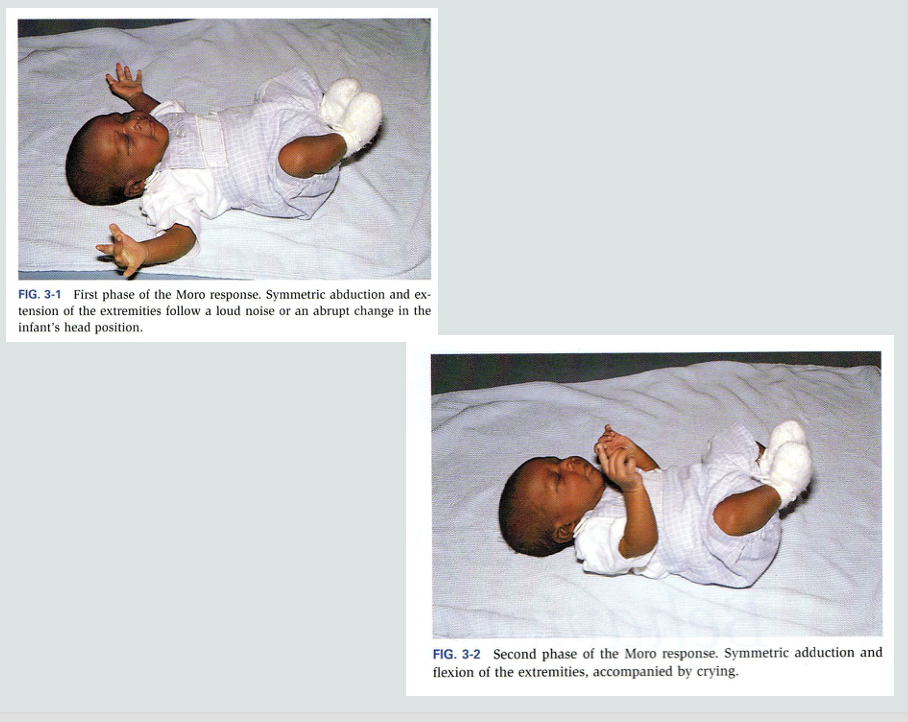
Gross Motor Development: Moro Response
Moro Response:
One of the best known primitive reflexes
Occurs during loud noises or startling
Abrupt extension of a baby’s neck, baby will first abduct and extend their arms then adduct and flex them
Abnormal if only had one arm that elicited reflex
Should disappear by 4 months: if not, can identify congenital/MSK abnormalities/brachial or neuro. plexus injury
Gross Motor Development: Hand grasp
Place finger in palm of newborn → will automatically grip it
Gross Motor Development: Sucking reflex
Can test with gloved finger or pacifier: infant should suckle finger
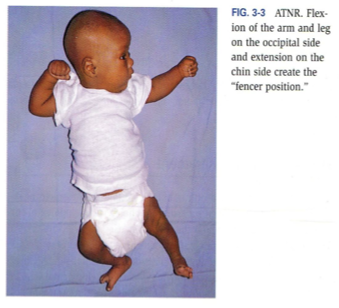
Gross Motor Development: ATNR (asymmetric tonic neck reflex/Fencer position)
The position of a baby’s head will influence the limb motion/position
By turning a baby’s head to one side (passive or active), they will extend the arm they are looking at and the other arm should come up and bend with their hand almost by their head or behind their head
When gaze is redirected, the fencer position is gone
Gross Motor Development: Muscular control
Development of muscle control develops in an organized fashion from head to toe
Prior to 6 months:
When infant is pulled from lying to sitting the head lags after the shoulders
Have good neck control during this time period: spasticity (investigate)
At 4-6 months:
The infant senses movement and should flex the neck before the shoulders lift
Over 4-6 months with no head control: hypotonia
Gross Motor Development: Protective Equilibrium
In a sitting position if the infant is pushed off balance: will outreach their hand and arm away from the force and try to support themselves
Appears around 6 months of age
Gross Motor Development: Parachute Response
When holding an infant or young child horizontally flying and allow them to fall downward → will outstretch both arms and legs to distribute weight for stability
Should have by 10 months
Gross Motor Development: Trunk Control
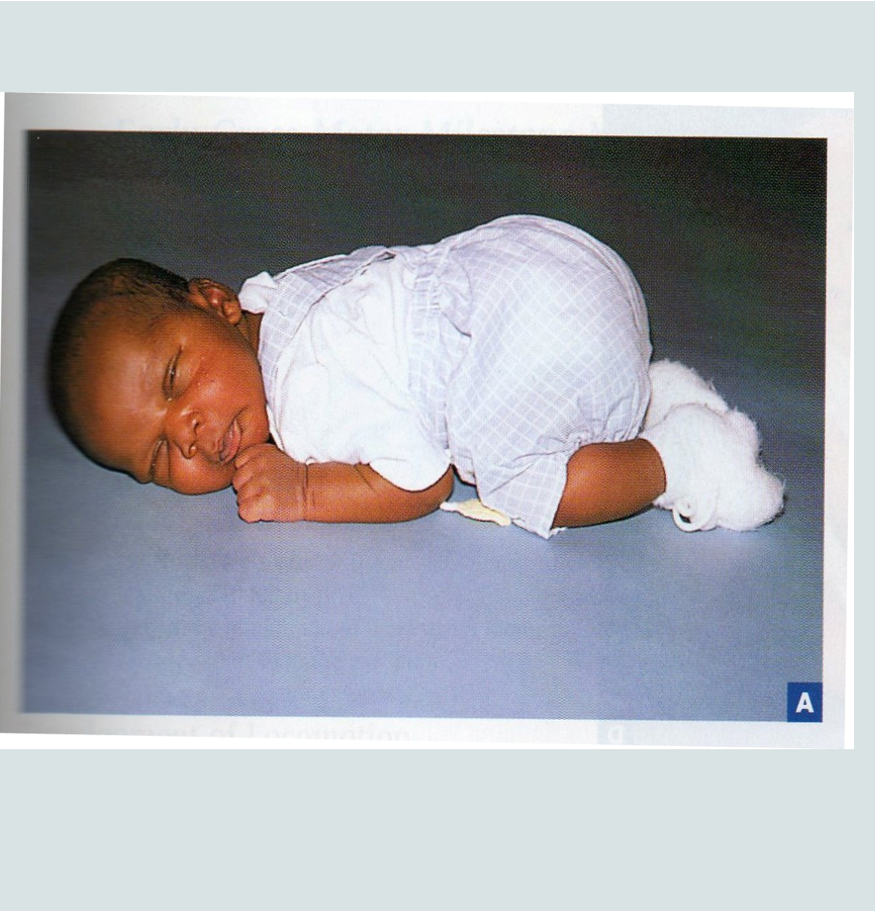
An infant lying prone is tightly flexed
Control of the upper trunk in the first few months develops along with a decrease in flexor tone (head to toe muscle control progression): should be able to control the weight of the upper trunk on their forearms by 4 months
Should not see floppiness or a 4 month old that cannot extend their arms (spasticity)
Gross Motor Development: Rolling
Develops after control of the shoulders and upper trunk develop
Belly to back comes first around 4 months: use arms for this
Back to belly comes at 5-6 months: need to rely on core (abdomen, lumbar spine, hips)
Because we innervate from top down, belly to back comes first and as we gain more control we can roll from back to belly
Gross Motor Development: Commando Crawling
5-6 months
Coordination of upper arms pulling and dragging legs
Some kids will never do this: normal
Gross Motor Development: Creeping/Crawling
6-9 months
Getting up on hands and knees: baby has control over hips and legs
Gross Motor Development: Cruising
9-10 months
Supported standing: stepping/walking while supported on furniture or holding onto a parents hand
Gross Motor Development: Walking
9-17 months
Unassisted walking with 3 or more steps
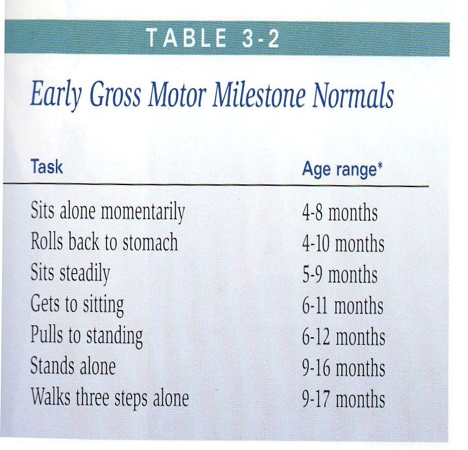
Gross Motor Development: Milestones
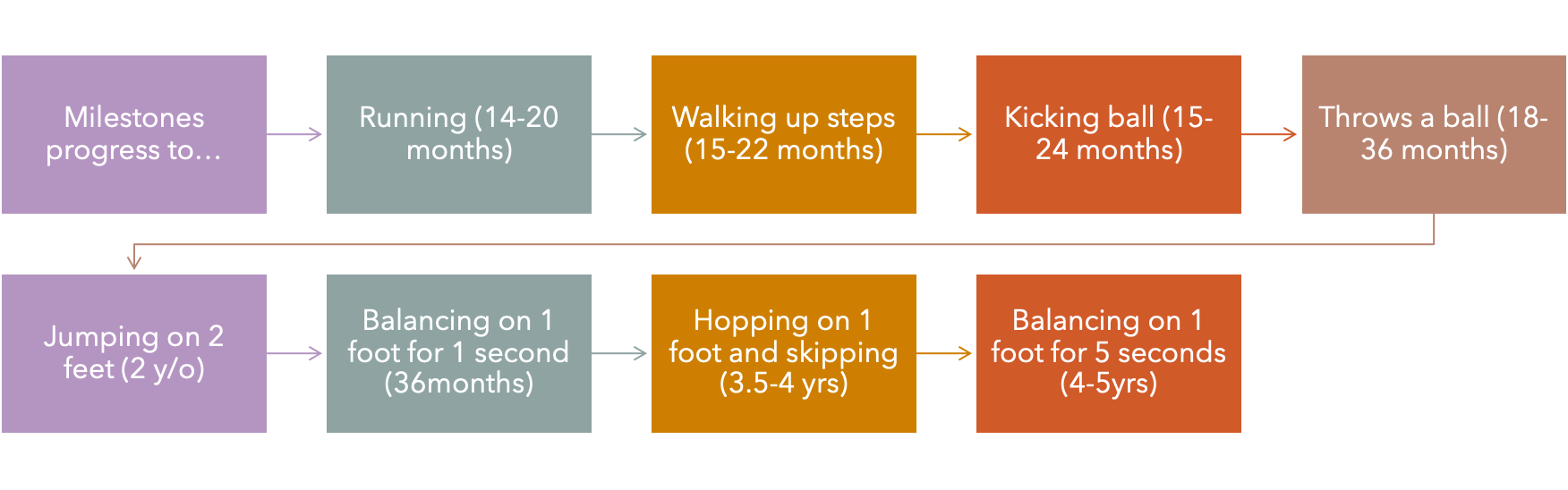
Early Gross Motor Milestones Normal
Potential Causes of Delayed Gross Motor Development
Global Developmental Delay
Genetic syndromes
Chromosomal abnormalities
Endocrine disorders
Intellectual disability
Congenital infection
Neurodegenerative disease
Motor Dysfunction
CNS damage: kernicterus, stroke, trauma, infection, HIE
Spinal cord dysfunction
Peripheral nerve dysfunction (brachial plexus injury, neuropathy)
Muscular disorders
Motor intact but otherwise restricted
Congenital malformation
Decreased energy: malnutrition, chronic illness
Environmental
Sensory deficits
Trauma
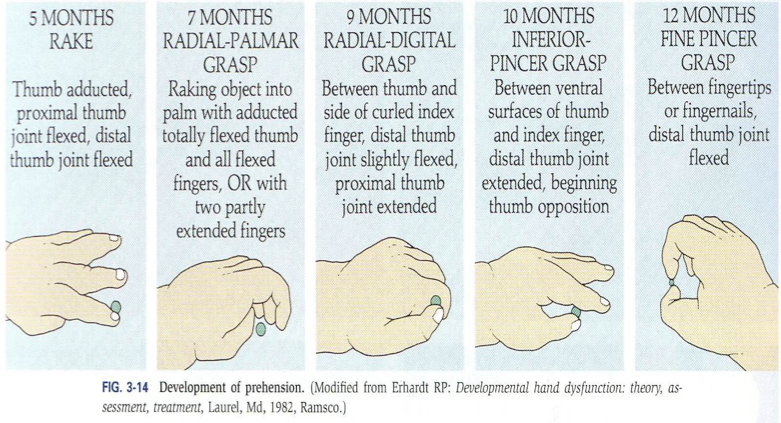
Fine Motor Development:
Control develops in the hand from proximal to distal
Fine Motor Development: Involuntary grasp
Primitive
At birth, an infant is tight fisted
Disappears in a couple of months and infant should develop voluntary grasp
Fine Motor Development: Voluntary grasp 2-3 months
Hands can be brought together in midline
Fine Motor Development: Voluntary grasp 3-4 months
Reaches toward and misses objects (swipes/waves at toys)
Fine Motor Development: Voluntary grasp 4 months
Reaches and grasps objects and brings them to mouth
Fine Motor Development: Voluntary grasp 4-5 months
Entire hand used to bring item near by (claw raking)
Thumb adducted, proximal thumb joint flexed, distal thumb joint flexed
Fine Motor Development: Voluntary grasp 5-7 months
Grasps objects, brings it to midline, and can transfer to other hand
Grasp uses radial palm (not fine pincer fingers)
Fine Motor Development: Voluntary grasp 9-12 months
Pincer grip (thumb and index finger) and baby starts to finger feed themselves
Fine Motor Development: Voluntary grasp 15-18 months
Uses of spoon and fork, scribbles, stacks 2 blocks, makes a line with a crayon
Fine Motor Development: Voluntary grasp 24 months
Stacks 6 blocks, imitates vertical or circular strokes
Fine Motor Development: Voluntary grasp 36 months
Copies circle, builds a bridge with 3 cubes
Fine Motor Development: Voluntary grasp 4 y/o
Copies cross or intersecting lines
Fine Motor Development: Voluntary grasp 5 y/o
Copies squares and draws triangles
Fine Motor Development: Red Flags
A child who does not have pincer grip by age 1
A young child who shows a preference for one hand before age 2 (should use both hands equally)
A child who can’t hold a crayon/pencil and copy a line on paper (age 3), copy a circle (age 4)
Cognitive Development:
The first 2 years: focused on sensory and motor abilities
Cognitive Development: Infant
Fixes and follows a face
Cognitive Development: 4-8 months
Tracks a toy that fell to the floor
Explores toys by touch, mouthing, and shaking to provide sensory input
Cognitive Development: 9-12 months
Object permanence: hide and object and they watch and can find where you put it
Likes to play peek a boo
Waves bye
Cognitive Development: 15 months
Figures out on their own how to make a toy work
Pretend play
Imitates (phone)
Indicates some needs by pointing
Cognitive Development: 15-18 months
Wants to share experience of toys (you do not want to see a child this age isolate themselves or always playing with the same toy)
Able to follow simple 1-2 step directions (take this and throw it out)
Cognitive Development: 18 months-2 years
Completes simple puzzles
Learns body parts/animal noises
Cognitive Development: 2-3 y/o
Learns colors
Learns shapes
Counting numbers
ABCs
Language Development:
Receptive language develops faster then expressive (can understand before we can speak)
Word comprehension starts by 9 months
Understands language and follows instructions by 15 months
Encourage parents to read to their child starting in infancy
Children who are not reaching these language milestones need a hearing evaluation and referral to a speech pathologist (language delays very common)
Language Development: 9 months
Babbles
2 syllables
Language Development: 12 months
1-3 words
Language Development: 15 months
3-6 words
1-2 body parts
Responds to simple commands
Language Development: 18 months
5-20 words
5+ body parts
Points to what they want
Points to 2 pictures
Language Development: 2 y/o
50+ words
2 word phrases
50% intelligible by a stranger
Names a few pictures
Follows 2 part command
Language Development: 3 y/o
900+ words
3-5 word phrases
75% intelligible
Language Development: 4 y/o
Thousands of words
5 word phrases
Social Development: Newborn
Focuses on parent’s face (1ft away)
Social Development: 4-6 week old
Social smile
Calms with comfort
Social Development: 4 month
Laughs at silly faces and sounds
Social Development: 6-8 months
Baby is upset by parent leaving room
Loves to interact with caregiver
Wave by and clap
Social Development: 9-12 months
Stranger anxiety
Plays peek a boo
Social Development: 15 months
Crawling/walking away from parent to toy and returning for encouragement
Social Development: 18 months
Asks for help
Feeds self
Social Development: 2 y/o
Parallel play: I want to be next to you playing but I do not want you touching my stuff (having an experience where someone is allowed to be there but do not share)
Does not want to share
Enjoys asking why, what, that
Helps undress
Listens to stories
Social Development: 3 y/o
Includes other children in play
Tries to cooperate and communicate with friends
Engages in sharing and playing
Doesn’t understand rules in a game
Fantastic imagination
Role playing and fantasy
Do not have these/stuck in parallel play: early sign of autism
Social Development and Sense of Self: 9 months
Wants to feed themselves
Social Development and Sense of Self: 9-12 months
Able to drink from a sippie cup
Social Development and Sense of Self: 12-15 months
Imitates helping at home
Social Development and Sense of Self: 15-18 months
Feeds self with fork and spoon
Social Development and Sense of Self: 18-24 months
Helps to get clothes off
Social Development and Sense of Self: 2-2.5 y/o
Helps to put clothes on
Helps to brush teeth
Social Development and Sense of Self: 3 y/o
Unbuttons clothes
Puts on shoes
Evaluating Social Development
At well child exam observe relationship between parent and child
Notice infant wanting parent for comfort, eye contact, or physical contact
Red flag
Children that have limited eye contact, who may not be affectionate with parent, who don’t participate in relationship exchanges (could be indicative of autism, poor social situation at home, etc…)
Assessment of child with suspected development delays considerations (7)
Remember that following a child across time with regular exams is important: one delay may not be significant
Not all children show consistent age appropriate development
A provider needs to look at multiple skills
Consider factors such as
Health of child
Socioeconomic status
Opportunity for learning
Preterm child or child with chronic health issues may show delays at first but should catch up by age 2
Subtle problems are more common than severe delays but harder to identify (child may not always show problem at visit)
A child that is normal as an infant or toddler may not develop skills expected in pre-school or school age periods
Evaluating for Developmental Delays: History
Medical history
Pregnancy (use of drugs, X-ray exposure, abnormal screens)
Labor and delivery
Newborn infection
Apnea
Elevated bilirubin
Failure to thrive
Chronic illness
Hospitalization
Abuse
Learning and Education
Performance and behavior in classroom
Standardized testing
Psychosocial history
Family/parents/caregivers
Upbringing
Parent language, cultural background, discipline, marriage, drug/alcohol abuse
Family resources
Developmental history
Age that milestones achieved
Family history
Intellectual disability
CNS disorders
Learning disabilities
History of mom’s other pregnancies and health of other children
Evaluating for Developmental Delays: Physical Exam
Dysmorphic features
Abnormal movements
Clumsiness
Vision/hearing exams
Neurological exam
Evaluating for Developmental Delays: Emotional/Social behavior
Often done by psychologist
Evaluating for Developmental Delays: Complete Neuropsychological evaluation
Evaluation of intelligence and achievement
Done by psychologist: very detailed
Referring Suspected Delays
Refer if delays occur in more than 1 area or development of 1 area but lingering
Refer as soon as possible
CT: Birth to 3
State system works on skills
Free of charge
Ages > 3 y/o
Preschool/school system is screening and evaluating
Evaluations by PT, OT, audiologist, speech, psychologist, development pediatrician, etc… may be necessary
Educate parents: anticipatory guidance (what they should expect at the next visit)