NURS 473: online modules
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
What are the vaccine-preventable diseases?
Chickenpox (Varicella), COVID-19 (Coronavirus), Diphtheria, Flu (Influenza), Hepatitis A & Hepatitis B, Hib (Haemophilus influenzae type b), HPV (Human Papillomavirus), Measles (Rubeola), Meningococcal Disease, Mumps, Mpox (Monkeypox), Pertussis (Whooping Cough), Pneumococcal Disease (Streptococcus pneumoniae), Polio (Poliomyelitis), RSV (Respiratory Syncytial Virus), Rotavirus, Rubella (German Measles), Shingles (Herpes Zoster), Tetanus (Lockjaw)
What is a notifiable diseases?
In Arizona, nurses must report to the County Health Department who then reports to the CDC. Failure to report a notifiable disease could result in being reported to the State Board of Nursing.
Reportable diseases: Anthrax, Hantavirus infection, Respiratory disease, Botulism, Hemolytic uremic syndrome, Rubella (German measles), Brucellosis, HIV infection and related disease in an infant, Rubella syndrome congenital, Candida auris, Influenza-associated mortality in a child, Severe acute respiratory syndrome (SARS), Chancroid, Leptospirosis, Smallpox, Chikungunya, Listeriosis, Spotted fever rickettsiosis (e.g., Rocky Mountain spotted fever), Cholera, Lymphocytic choriomeningitis, Syphilis, Creutzfeldt-Jakob disease, Measles (rubeola), Taeniasis, Cronobacter infection in an infant, Melioidosis, Tetanus, Cysticercosis, Meningococcal invasive disease, Toxic shock syndrome, Dengue, Middle East respiratory syndrome (MERS), Trichinosis, Diarrhea, nausea, or vomiting, Mpox, Tuberculosis active disease, Diphtheria, Mumps, Tuberculosis latent infection in a child 5 years of age or younger, Emerging or exotic disease, Novel coronavirus infection, Tularemia, Encephalitis parasitic, Pertussis (whooping cough), Typhoid fever, Encephalitis viral, Plague, Typhus fever, Glanders, Poliomyelitis (paralytic or non-paralytic), Vaccinia-related adverse event, Gonorrhea, Q fever, Varicella (chickenpox), Haemophilus influenzae invasive disease, Rabies in a human, Viral hemorrhagic fever, Hansen's disease (Leprosy), Relapsing fever (borreliosis), Yellow fever, Zika virus infection
Contagion movie
The outbreak begins: The pandemic starts when Beth Emhoff travels from Hong Kong to her husband's home in Minneapolis, spreading the virus to her son and others along the way. She and her son die shortly after. Her husband, Mitch, is revealed to be immune, providing a rare case of survival.
Medical response: A team of medical professionals, led by figures like CDC's Dr. Ellis Cheever (Laurence Fishburne) and Dr. Erin Mears (Kate Winslet) and WHO's Dr. Leonora Orantes (Marion Cotillard), struggles to contain the MEV-1 virus. They work to identify the virus, its origins, and develop a vaccine, while also dealing with political pressure and the breakdown of social order.
Societal collapse: As the death toll rises, fear and misinformation spread, leading to panic, riots, and a collapse of social structures. A conspiracy theorist blogger, Alan Krum (Jude Law), exacerbates the situation by spreading false information and fear about the pandemic.
The cure: A vaccine is eventually developed by a researcher at the CDC, Dr. Ally Hextall (Jennifer Ehle). She tests the vaccine on herself to prove its effectiveness, leading to a public health victory and the gradual recovery of society.
The end: On day 135, life slowly returns to normal, though the experience leaves a lasting impact on society. The final scene shows Dr. Hextall storing a sample of the vaccine, reflecting on the continuous struggle against disease.
How to break the chain of infection?
isolation (separate the sick from the healthy), treatment, hand washing, PPE, sterilizing/disinfecting, quarantine (separate the exposed during the incubation stage)
Epidemiology
Study of the distribution and determinants of states of health and illness in human populations; used both as a research methodology to study states of health and illness and as a body of knowledge that results from the study of a specific state of health or illness.
When is a disease is considered an endemic, an outbreak, an epidemic or a pandemic and what distinguishes those labels?
Pick a disease and imagine how it might appear across this spectrum. For example, when we first became aware of COVID, cases were initially being noted in a limited geographic area, which would make it an outbreak in those early days. When COVID spread regionally to other areas of China and Asia, it was categorized as an epidemic. Worldwide spread led to it being labeled a pandemic. Now, it seems like COVID is something humanity is going to live with, albeit at lower levels, for the next several generations. When a disease remains in the population like that, it's called endemic.
Endemic: occur at consistent and expected levels in a defined and often limited geographic area
Outbreak: Epidemic usually limited to a localized increase in the incidence of the illness.
Epidemic: An outbreak that occurs when there is an increased incidence of a disease beyond that which is normally found in the population.
Pandemic: epidemic that has spread across the globe
Eradication vs. elimination
Eradication: irreversible elimination of all transmission of infection worldwide (ex: smallpox)
Elimination: reduction to 0 or very low new cases of disease in a defined geographic area (This was the case with polio, but as you may know, new cases have been appearing in the U.S. and Europe, so we can no longer categorized polio as eliminated)
Discuss the role of genomics and the ecological model in modern epidemiological studies.
Genomics refers to the interaction between genetics and the environment.
Genomics can offer insights into what treatments might be most effective for the disease
Person-place-time model
questions that give epidemiologists data to guide containment and treatment of these diseases
Epidemiology Triangle**
Epidemiologic triad: Model based on the belief that health status is determined by the interaction of the characteristics of the host, agent, and environment.
Host: pregnancy increases susceptibility, sickle cell etc.
Agent: pathogen like Malaria
Environment: travelers, immigrants
Vector: ex: mosquito
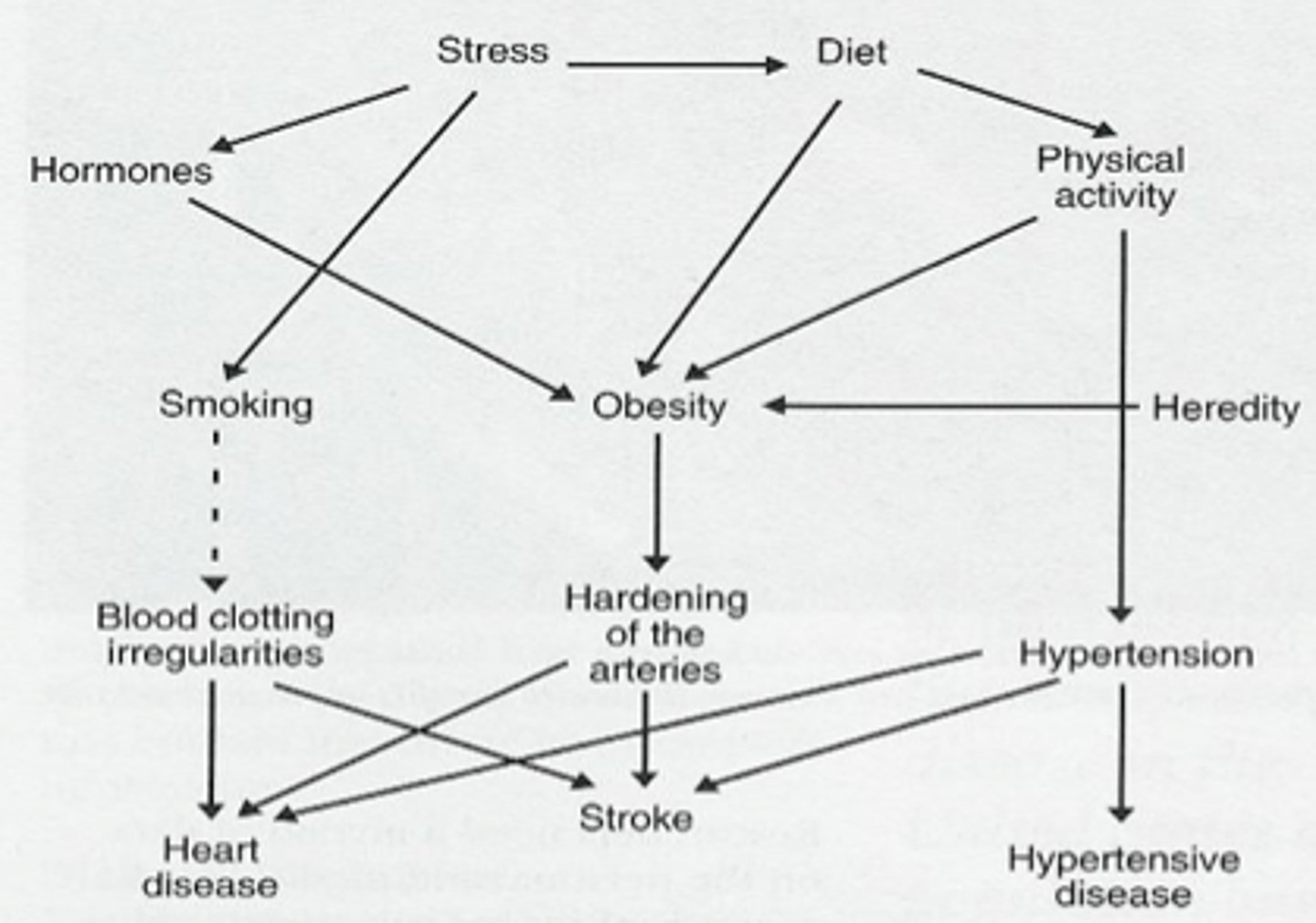
Web of causation
Uses an ecological approach to disease development by acknowledging that there are multiple factors involved
John Snow
"Father of Epidemiology", studied the London Cholera epidemics of 1848 & 1854, suspected it was from the water, as most cases were found close to the Broad Street pump
Sanitary movement
Concern with environment, living conditions, hygiene, access to clean water and food
- built the sewer systems that are still in London today
- prevented SO many deaths
Germ theory
the theory that infectious diseases are caused by certain microbes
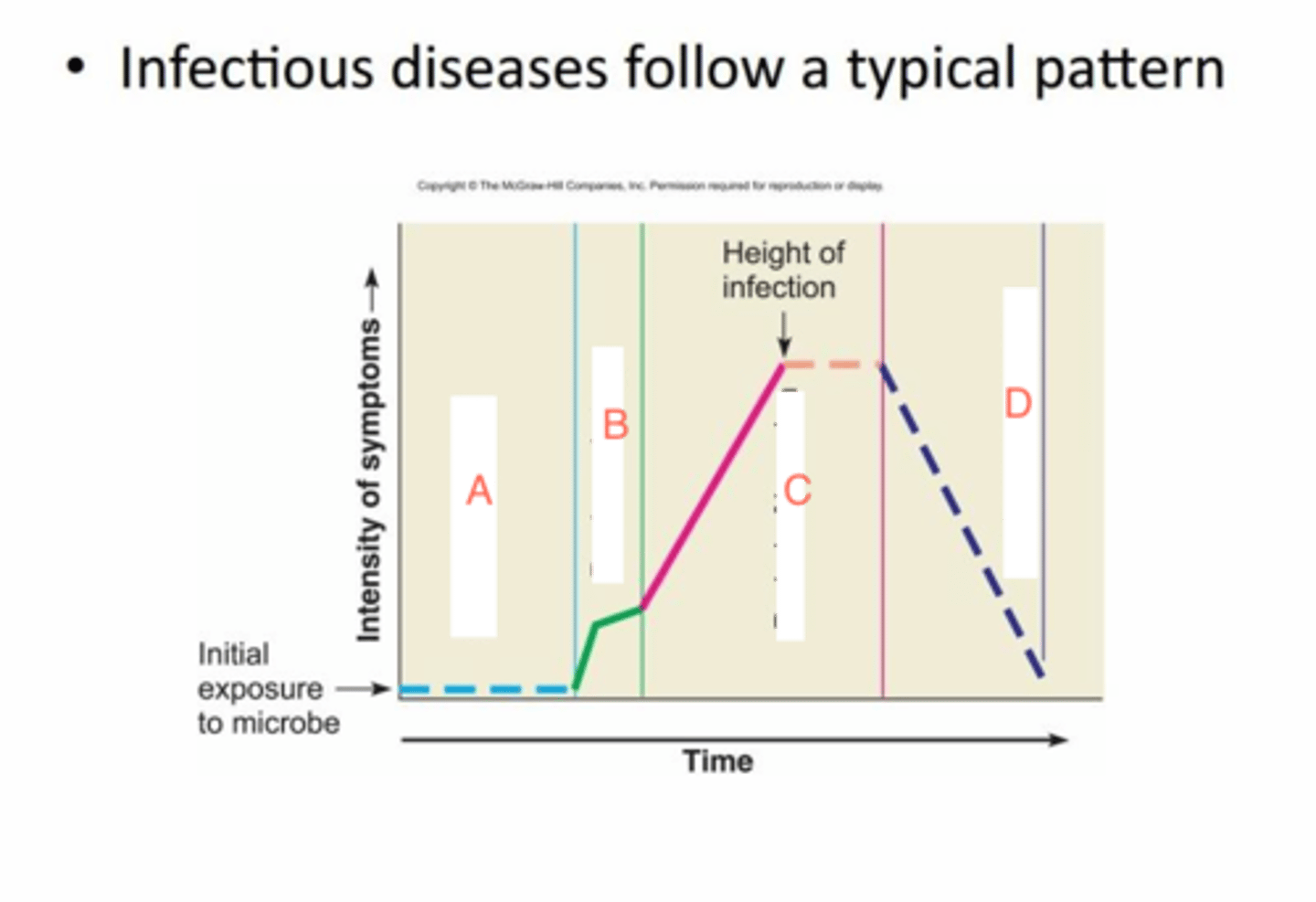
Stages of infection
Incubation period: the time before symptoms begin. (the period of disease follows the incubation period)
Latent period: the time when the individual is not yet contagious. (the period of communicability follows the latent period)
Communicable: infectious regardless of symptoms
**Depending on the disease, the end of the incubation period might align with the end of the latent period, but sometimes the incubation period might overlap the latent period, meaning that someone might have a condition, but not yet display any symptoms.
Incidence
Incidence: number of cases diagnosed for a condition during a specified time period (new cases/diagnoses, events)
- incident rates compare the incidents to the population at risk
- incidence and incident rates can track the effectiveness of prevention efforts
Prevalence
Prevalence: total number of people in the population who have or are living with a condition at a particular point in time
- influenced by rates of new cases, number of existing cases, new treatments, and deaths
- prevalence and Prevalence Rates can be used to describe the scope of an issue
What is the difference between incidence and prevalence?
Incidence: For example, in Arizona in 2008 (during the 2008 calendar year) the incidence of HIV/AIDS was 700 (700 newly diagnosed cases infection-either HIV or as full blown AIDS) and the incidence rate was 10.77 per 100,000.
*period of time*
=> Researchers use incidence rates to determine the effectiveness of primary and secondary prevention. If primary prevention efforts are effective, the incidence and incidence rate should go down in a population. If secondary prevention is effective and more cases are identified, the incidence is likely to rise.
Prevalence: For example, in 2008 (probably a mid year estimate) there were 4,142 persons known to be living with HIV or AIDS (prevalence) and based on a calculation using Arizona's 2008 population, Arizona's HIV prevalence rate is 217.6 per 100,000 persons.
*single point in time*
=> Prevalence cannot be used to determine effectiveness of programs as there are too many variables that impact the number. Prevalence is often used to describe the scope of the public health problem and to plan for services and resources.
Human rights vs civil rights
Human rights: universal, inherent, non-negotiable, not given by the government (ex: right to health, dignity, freedom from discrimination etc.)
Civil rights: legal protections tied to a specific country's national law (ex: equal access, nondiscrimination, etc.)
Health Care in Danger Video
- the right of healthcare workers to not be targeted is not actually upheld in many places
- healthcare workers can show discrimination in who they treat first
- healthcare facilities may be targets
- obstruction/barriers to healthcare is another strategy used to discriminate (ex: permits, checkpoints)
Discuss human rights and civil rights as applied to nursing.
Human rights in nursing: advocate for safe/equitable care, uphold pt autonomy (consent), protect pt confidentiality (dignity)
Civil rights in nursing: compliance with legal protections (ADA, title VI, etc.), ensure nondiscrimination in care delivery
Differentiate between Human Rights Law and International Humanitarian Law.
Human Rights Law: APPLIES AT ALL TIMES; right to health/freedom/education, meant to apply universally across all nations
- emerged after WWII as part of the emergence of the United Nations
International Humanitarian Law: CONFLICT SPECIFIC, applies in armed conflict/emergencies, protects civilians/prisoners of war/medical workers
- rooted in Geneva Conventions
Also know which populations are most at risk of experiencing violations of either human rights law or international humanitarian law.
Human Rights Laws: vulnerable people?
International Humanitarian Law: healthcare personnel?
Analyze the ethical principles and human rights violated in the Tuskegee Syphilis Study. Explain what happened.
Discuss how nurses can incorporate rights-based care in their practice.
Rights-based care: care grounded in universal rights (ex: ensuring informed consent)
Discuss how nurses can incorporate a human needs framework (Maslow's Hierarchy of Needs) in their practice.
Maslow's hierarchy of needs: in light of the Universal declaration of Human rights everyone is entitled to have their physiological needs met (food, water, healthcare, shelter, freedom from torture) as an active right.
Give an example of discrimination in healthcare
- unfair treatment based on race, gender, class, etc.
- impacts quality and access to care
What are the 4 etiologies of discrimination in healthcare
1) individual => person to person
2) institutional => hospital policy
3) structural => geographic barriers
4) cultural => stereotyping/stigmatization
define social justice in the context of nursing
Social justice in nursing: addressing health disparities, advocating for vulnerable patients
sometimes in public health, this is considered an ethical principle
be familiar with the Crisis Prevention Intervention tips
Explain lateral violence in nursing
Be familiar with different roles and responsibilities in occupational health
Articulate the role of OSHA
Be familiar with school nursing's impact in the community
Analyze common health issues encountered by school nurses
Be familiar with the role of school nursing in disease outbreaks
Identify how environmental issues associated with climate change impact health
Impact of climate change on human health:
- air pollution => asthma, cardiovascular disease
- changes in vector ecology => malaria, dengue, encephalitis, hantavirus, Rift valley fever, lyme disease, chikungunya, west nile virus
- increasing allergens => respiratory allergies, asthma
- water quality impacts => cholera, crytospoidiosis, campylobacter, leptospirosis, harmful algal blooms
- water/food supply impacts => malnutrition, diarrheal disease
- environmental degredation => forced migration, civil conflict, mental health impacts
- extreme heat => heat- related illness/death, cardiovascular failure
- severe weather => injuries, fatalities, mental health impacts
Be familiar with the major physical, biologic, chemical, and climate-related hazards to human health, particularity lead poisoning, drought, air pollution, radon, medications, vectors etc . Pg.468, 472, 470 & Climate Change and Heat Related Deaths PPT by Prof Straub
healthy home: lead paint, radon, indoor air quality, mold mitigation, green cleaning techniques, integrated pest management
???
Be familiar with the responsibilities of PHNs in Disaster Management
- Assess the needs of the community as the events unfold.
- Conduct surveillance for communicable disease and unmet needs.
- Prevent and control the spread of disease.
- Maintain communication channels to ensure accurate dissemination of information to colleagues and the public.
- Organize and manage points of distribution centers and mass immunization sites as required.
- Provide on-site triage as needed.
- Manage behavioral responses to stress.
- Ensure the health and safety of self, colleagues, and the public.
- Document events and interventions.
Identify the advantages of using biologic agents as weapons
The incubation periods of live agents afford the terrorist time to leave the scene of the crime before detection, whereas releases of chemicals are evident almost immediately, regardless of the circumstances.
Advantages:
- Infectious via aerosol
- Organisms fairly stable in the environment
- Civilian populations are susceptible
- High morbidity and mortality rates
- Person-to-person transmission (smallpox, plague, viral hemorrhagic fever)
- Difficult to diagnose and/or treat
- Easy to obtain
- Inexpensive to produce
- Potential for dissemination over large geographic area
- Creates panic
- Can overwhelm medical services
- Perpetrators escape easily
- Previous development of organisms for biologic weapons
Definition of a disaster?
Definition: Disasters are often unforeseen, serious, and unique events that disrupt essential community services and cause human morbidity and mortality that cannot be alleviated unless assistance is received from others outside the community. Disasters vary by (1) the type of onset (they often occur without warning), (2) the duration of the crisis, (3) the magnitude or scope of the incident, and (4) the extent to which the event affects the community.
Types of disasters
- Pandemic
- Natural
- Human-made (accidental)
- Terrorist attacks
Be familiar with the 5 phases of emergency management response during a disaster
Preparedness: identify all hazards, proactive planning, evaluate possible damage
Mitigation: take measures to limit damage/disability/loss of life
Response: implementation of disaster plan, provide emergency care, restore communication/transportation
Recovery: stabilization, return to normal status
Evaluation: learn from the past, prepare for the future
Be familiar with when to shelter in place and when to evacuate
Shelter in place: short-duration incidents when moving would result in greater hazard or its impractical to evacuate
Evacuation: occurs when there is potential for massive explosions and fire or flooding, as well as for long-duration events. The loss of significant infrastructure such as potable water or electricity may also require evacuation. Ex: forest fires, hurricanes
18 natural hazards included in the National Risk Index (NRI)
avalanche, coastal flooding, cold wave, drought, earthquake, hail, heat wave, hurricane, ice, storm, landslide, lightning, riverine flooding, strong wind, tornado, tsunami, volcanic activity wildfire, winter weather
**note extreme heat is not accounted for as a natural NRI hazard
Extreme Heat
often results in the highest number of deaths each year among all weather-related hazards.
Urban Heat Island effect
Understand how extreme heat affects individuals who use illicit drugs or take certain psychiatric medications
methamphetamine, fentanyl, and psychiatric medications can make people more vulnerable to extreme heat because they affect the body's ability to regulate temperature
- methamphetamine: stimulant, increases body temp, impairs brain's ability to cool down, hard for heart to compensate
- fentanyl/opioids: slow breathing, reduce body's ability to respond to heat stress, causes excessive sweating => dehydration
- psychiatric meds: some antidepressants and anstipsychotics interfere with the body's ability to sweat and regualte temp
Be familiar with the strategies taken to reduce the impact of extreme heat in Arizona
- Maricopa county has expanded emergency homeless shelters
- Phx/Tuc plans to increase tree canopy by 2030
- Phx/Tuc offer cooling centers
- Red cross mobile home canvassing and beat the heat campaign
Identify aggregates at greatest risk due to climate change.
deaths outdoors: usually male, often homeless, and often using substances like meth
deaths indoors: A/C doesnt work, victims tend to be older, low-income, skew more female, and are much less likely to have used substances
*both groups die because of social isolation
Identify what should be included in a personal emergency supply "to go kit". Be able to list at least 10
- Water (1 gallon per person per day for at least 3 days)
- Food (3 day supply)
- Battery-powered or hand crank radio
- Flashlight
- Extra batteries
- First aid kit
- Medications
- Multi-purpose tool
- sanitation and personal hygiene items
- copies of personal documents (medication list and pertinent medical information, proof of address, deed/lease to home, passports, birth certificates, insurance policies)
- cell phone with chargers
- family and emergency contact information
- extra cash
- emergency blanket
- matches
- Whistle to signal for help
- Dust mask (to help filter contaminated air)
- Plastic sheeting and duct tape (shelter in place)
- Moist towelettes, garbage bags, plastic ties (personal sanitation)
- Wrench of pliers (turn off utilities)
- Can opener for food
- Local map
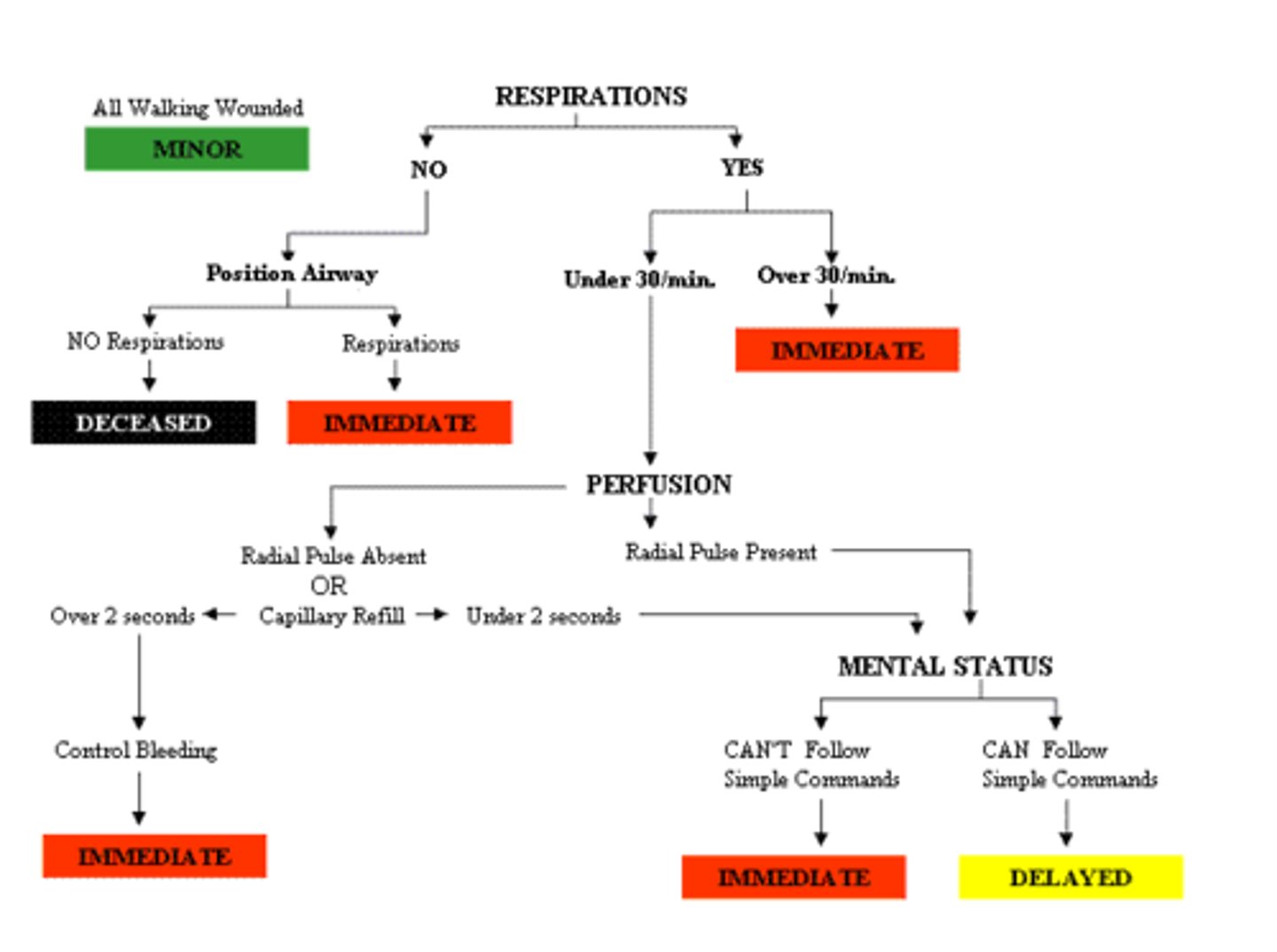
START triage system
Red (Critical): Unstable, requiring immediate intervention
Yellow (Urgent): Stable, but may deteriorate
Green (Delayed): Injured or ill but stable and not likely to deteriorate "walking wounded"
Black (Expectant): Dead or nonsalvageable given available resources
What is PVH?
Pediatric Vehicular Heat Stroke: consequence of a child succumbing to heat inside of a car
- heat stroke occurs when child's body temp rises > 104 F
* a child's body temp rises 3-5 times faster than an adult's
- 107 F => cells are damaged, organs shut down, death/permanent disability
What are the three categories of PVH?
1) gained access (MOM): hiding, exploring, quiet place, locked in by child locks, usually occurs on the weekend, 4 years old
2) forgotten (DAD)
3) knowingly left (MOM): left at bars/race-tracks/casinos, most cases <2 years old
What are the s/s of heat stroke?
s/s: flushed dry skin, perspiration, strong and rapid pulse, possible coma
What are the safety recommendations to prevent PVH?
- call 911 if you see a child or pet left unattended in a car
- cars are not babysitters, never leave a child unattended in a car
- put a toy on the front seat as a reminder a child is in the backseat
- teach children (the car is not a play place, honk the horn if trapped, keep keys out of child's reach, how to get out of car safely)
- if a child is missing, check pool first then all vehicles in the area
What are the primary factors contributing to a car's interior heat?
color of a car's interior, contact with car seat
An adult victim is crying out for help and when asked to move, he is unable to get up. He has an open fracture of the left lower leg and many bloody abrasions on his face and arm. He has respiration rate of 36/m, a cap refill time of 3 seconds, and is able to squeeze your hand and nod appropriately. Using START, how should the triage nurse tag this man?
A - Red
B - Yellow
C - Green
D - Gray
E - Black
A) Red
In this instance, A is the correct answer, due to the individual's respiratory rate, which is over 36 breaths per minutes.
Definition of Nursing Ethics (PPT #5)
The main principles of bioethics (PPT #6)
The seven principles of ethical decision-making (PPT #6)
Identify the different between clinical nursing ethics and public health ethics (PPT #13)