15. Lens metabolsim, oxidation, and catarcts
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
What does lens circulation provide?
Support viability of lens by moving:
Nutrients/glucose
metabolic waste
oxidative repair molecules
ions
water
How does water and ions flow through the lens?
Dependent on NKA, with NKA concentrated in cells near equator.
Facilitated by large numbers of gap junctions and aquaporins
What channels does glucose go through to enter aqueous?
SGLT on pigmented epithelial cell
GLUT on non-pigmented epithelial cell
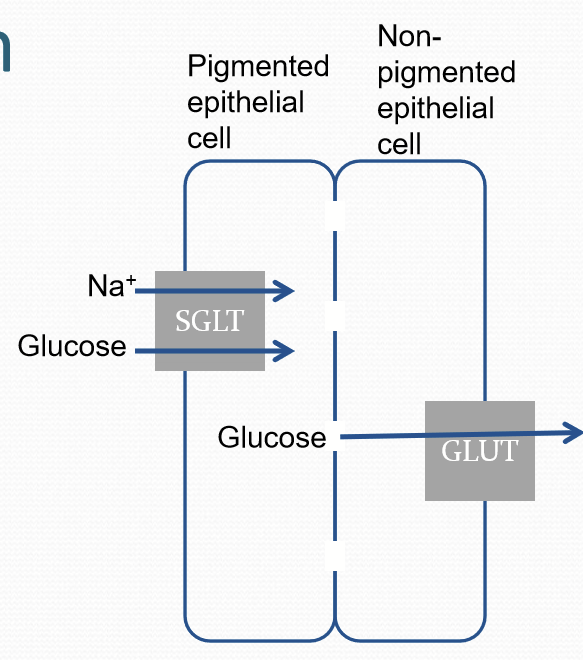
What GLUT transporters are on the lens and where are they?
GLUT1 is primarily in lens epithelium
GLUT3 is primarily in cortical lens fibers and center of the lens
Glucose has higher affinity for GLUT3 than GLUT1
SGLT is found on deeper lens fibers. Uses Na gradient.
What are some lens complications of diabetes?
Lens is damaged by high levels of glucose=facilitates cataract formation
Damage is mediated by aldose reductase: sorbitol may cause osmotic damage and may also create oxidative stress
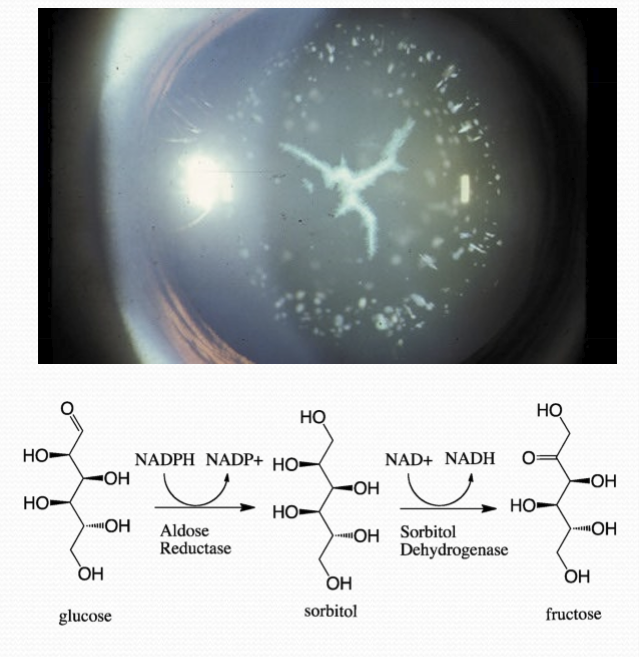
What are long-term issues with the lens from diabetes?
Variable refractive changes and opacities
Increases lens size: thicker lens and increase in curvature
What are short-term issues with the lens from diabetes?
Variable refractive changes:
fluctuations in glucose levels affects osmolarity of lens
changes in osmolarity changes water content
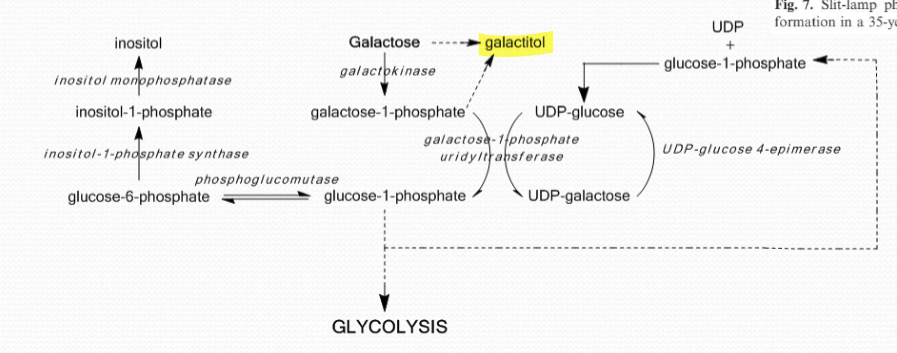
What is galactosemia?
A defect in, or absence of, galactose-metabolizing enzymes. It is rather rare and causes a buildup of galactitol. The osmotic swelling of the lens epithelial cells causes lens opacity/cataracts.
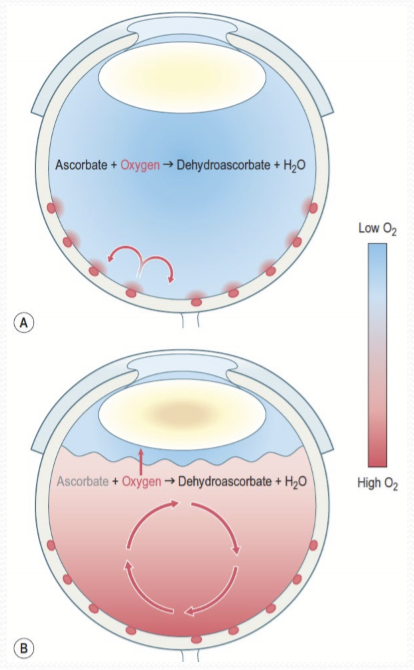
What are the 2 main sources of lenticular oxygen?
Diffusion across the cornea (major)
retinal vascularture
Some contribution of oxygen from ciliary body vasculature, but most of the oxygen is utilized by ciliary body vasculature.
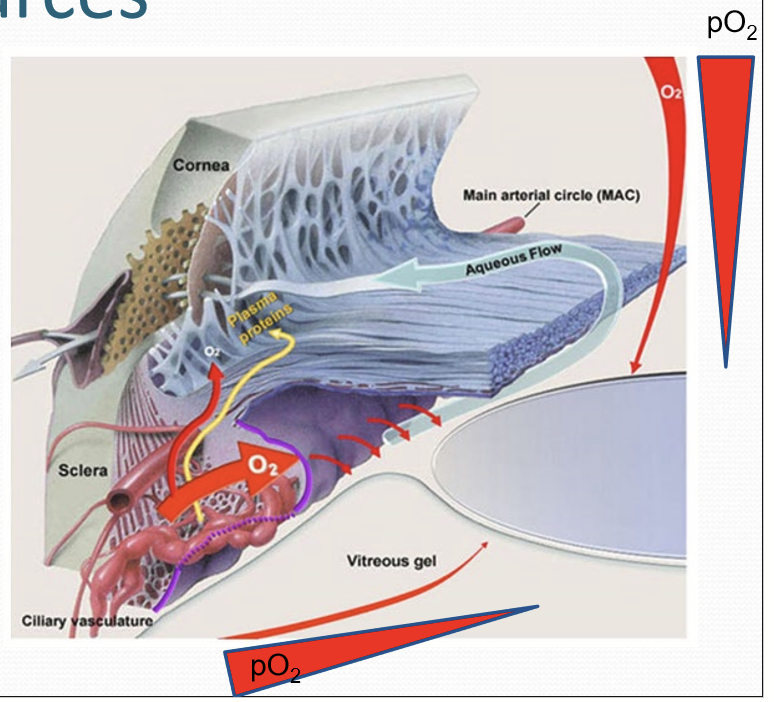
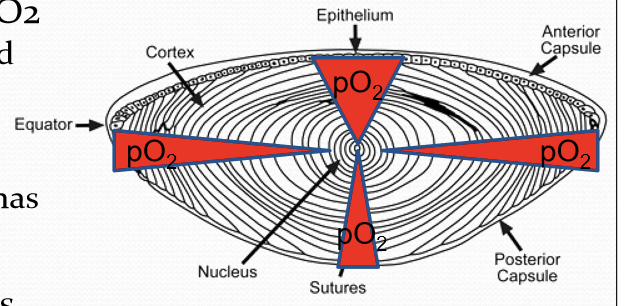
What is the oxygen levels of the lens?
Lens tissue has a gradient, with highest pO2 in lens epithelium and peripheral lens fibers. Lowest in lens nucleus. Low pO2 protects lens proteins and lipids from oxidative damage.
What is linked to oxygen levels?
Growth rate. With more oxygen = more growth.
What determines the type of metabolism that occurs in the lens?
Oxygen content and mitochondria number. So lens epithelium has a high mitochondria number and less in central nuclear fibers.
What cells undergo both aerobic and anaerobic metabolism?
Lens epithelial cells. Glucose utilization: ~50% each.
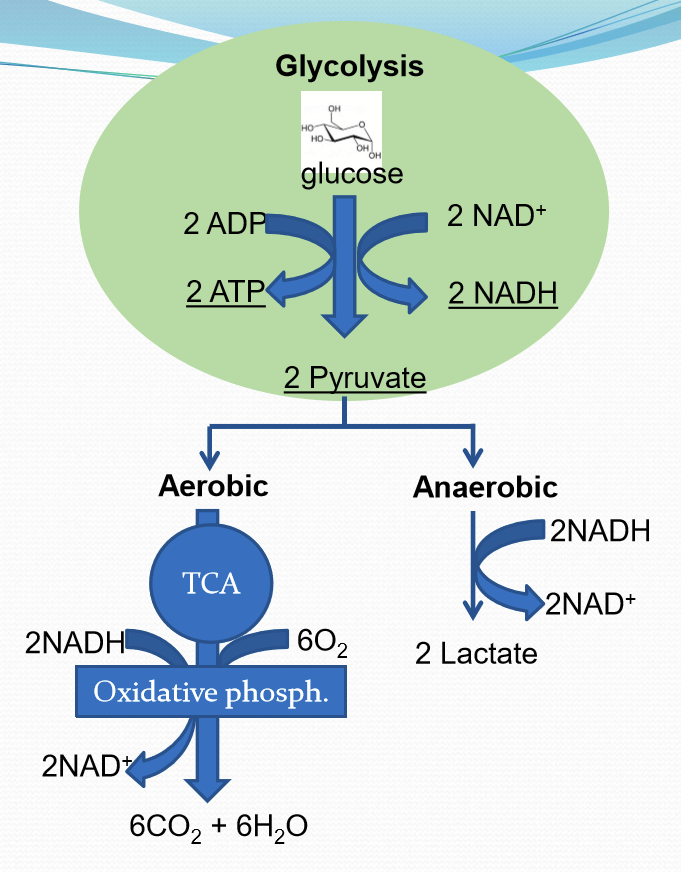
What cells use almost entirely anaerobic metabolism?
Lens fiber cell
Where is the majority of lens ATP derived from?
Anaerobic glycolysis.
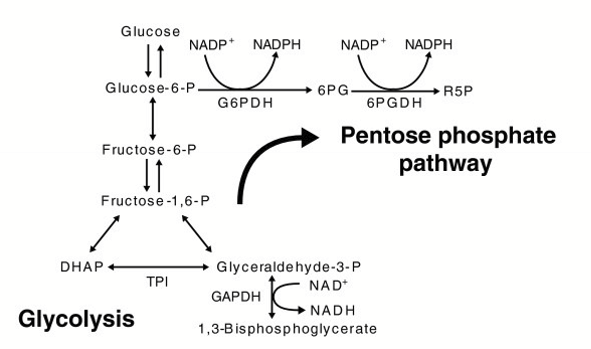
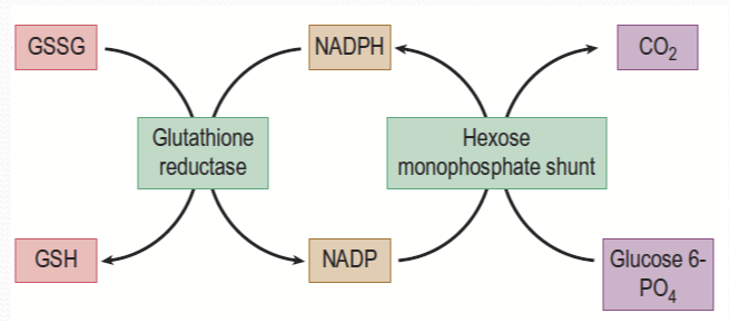
What does the function of hexose monophosphate shunt?
Utilized by corneal epithelium and lens cells to:
Produce NADPH in synthesis of lipids and limit ROS
Produces ribose-phosphate, needed for nucleic acid synthesis
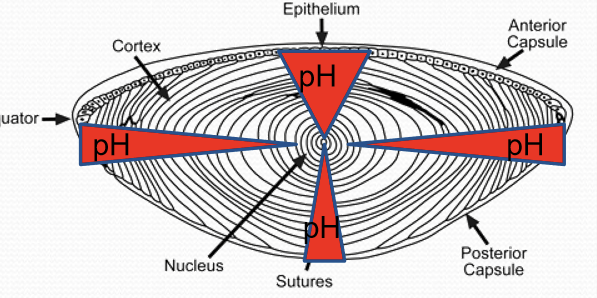
What happens to the lens due to the build up of lactate?
Intracellular pH drops significantly towards deeper fiber cells. Increased degree of anaerobic metabolism=increase lactate levels.
What can happen in an hyperbaric oxygen environment?
Nuclear cataract formation. Effects are reversed upon normal O2 environments. Suggests that the lens has a limited capacity to reverse oxidative damage.
What does nuclear cataract formation due to increased oxygen demonstrate?
Central fibers are more susceptible to oxidative damage.
What role does the vitreous have for protecting the lens?
It reduces the amount of oxygen that reaches the lens. Based on incidence rate of cataracts following vitrectomy = 95% within 2 years.
What are ways free radicals are produced in the lens?
Oxidative phosphorlyation in cortical lens fibers/epithelium
UV light absorbed by lens fiber proteins/DNA
How is H2O2 produced in the lens?
lens mitochondria (minor) via superoxide dismutase actiong on the superoxide anion
Oxidation of ascorbic acid (major)
What protects the lens against the oxidative damage?
Glutathione: Very high conc in lens cells. It is generated by lens epithelial cells, superficial lens fibers. Gap junctions allow passage of glutathione between cells to the lens nucleus.
What is Glutathione made up of?
Glutamine, cysteine, and glycine.
How is amino acid transported into the lens?
High extracellular Na/Cl to bring in precursors into lens epithelial /cortical lens fiber cells.
What enzyme assembles glutathione?
glutathione synthase
How is glutathione transported in the lens fiber cells?
Sodium dependent transporter
Gap junctions
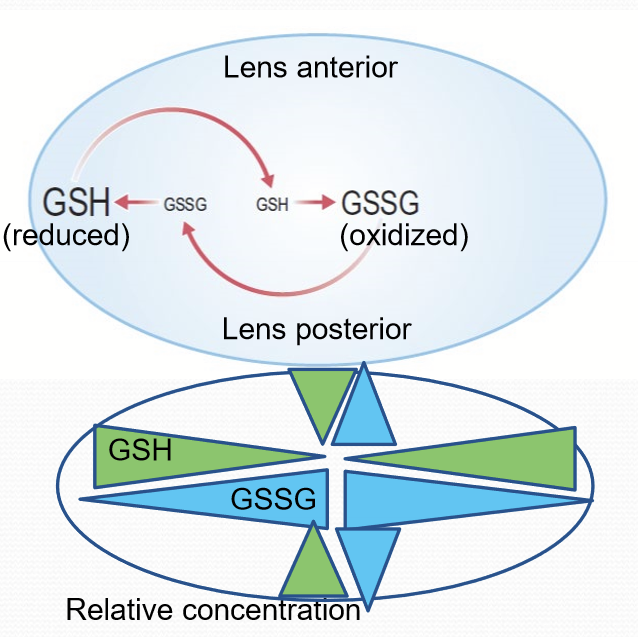
How does glutathione protect the lens?
Forms disulfide bonds with oxidized sulfhydryl group of damaged proteins. Thioltransferase reduces mixed disulfide and produces “fixed” protein and oxidized glutathione (GSSG).
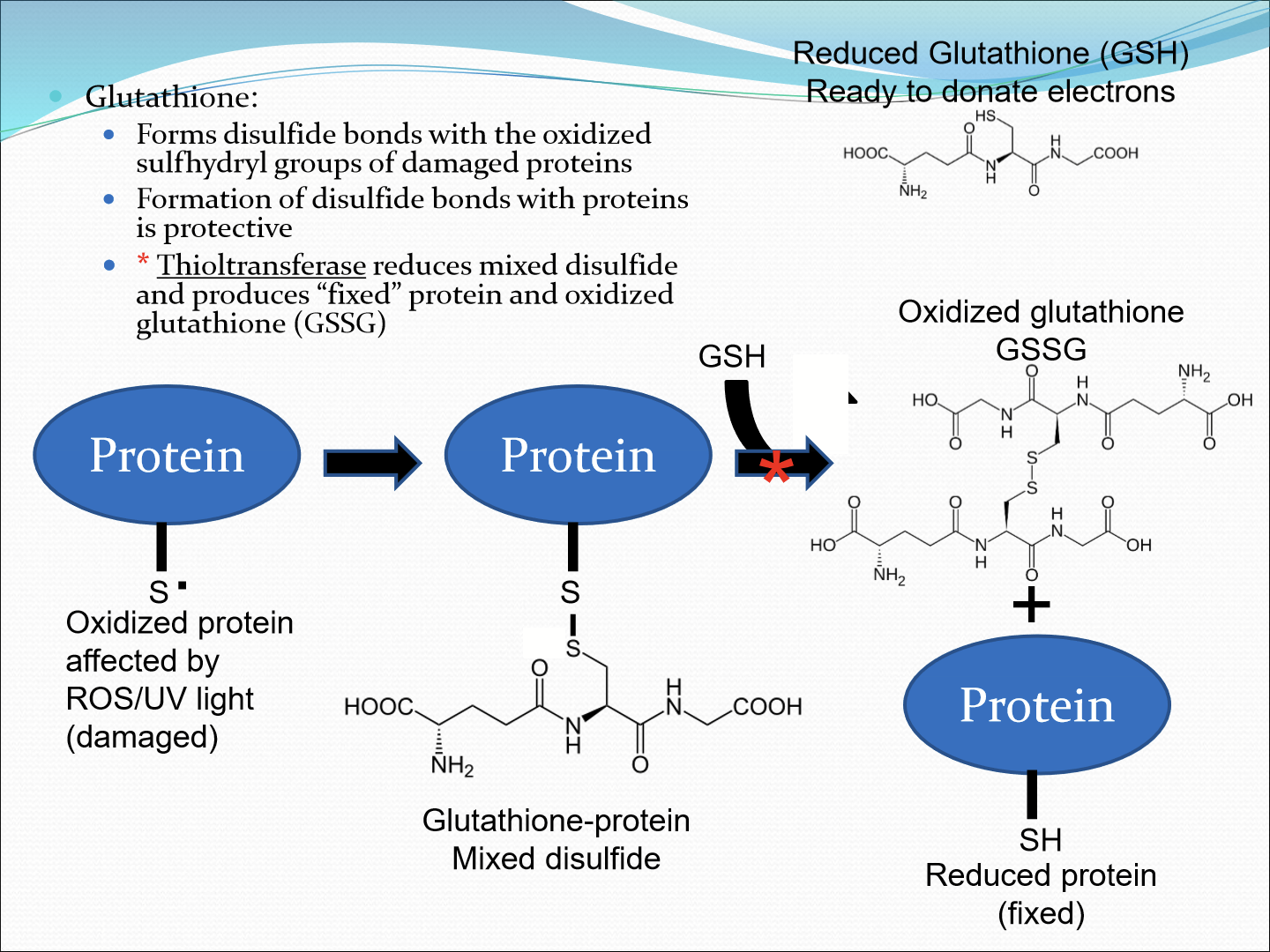
What converts the oxidized glutatione (GSSG) to reduced form (GSH)?
Glutathione reductase, using NADPH. Hexose monophosphate shunt then regenerates NADP back to NADPH.
Where is the concentration of GSH lowest?
Cells deeper in the lens due to limited capacity for synthesizing or reducing glutathione.
What happens to the diffusion rate of glutathione with time?
Rate of diffusion diminshes and therefore older lens are more susceptible to oxidative damage.
What enzyme reduces H2O2 to water?
glutathione peroxidase
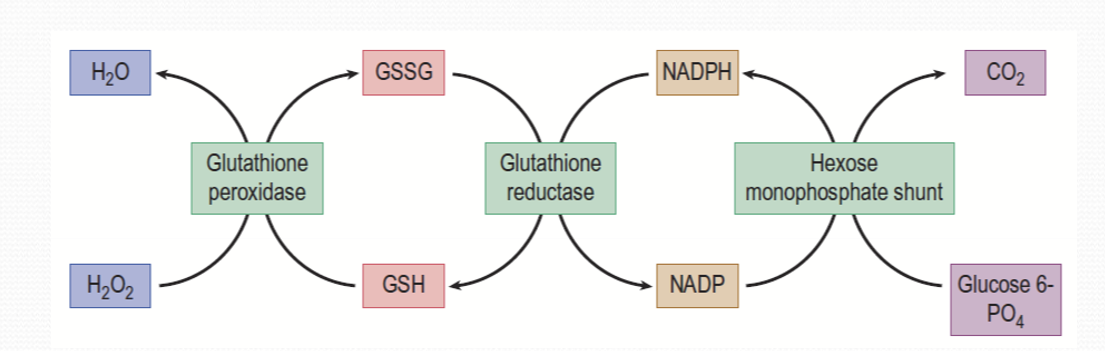
Where is glutathione peroxidase abundant?
In lens epithelial cells
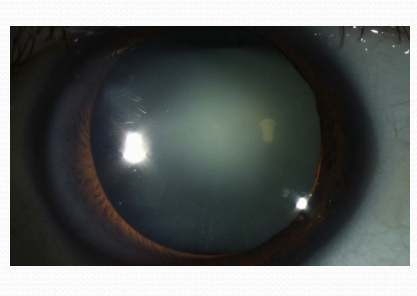
What is cataracts?
An opacification of the lens. It is clinically significant when the opacification interferes with visual function.
How does cataracts interferes with visual function?
Increased light scattering from disruption of lens structure, increase in protein aggregation, cytoplasmic phase separation
Increase in light absorption: brunescent

What does bruescence affect?
Diminishes the perception of violet and blue light. Lens absorbs 300-500 nm range.
What is responsible for the color of brunescence?
Build up of chromophores.
What normally provides UV filtration of UVB and UVA light?
Kynurenine and its derivatives.
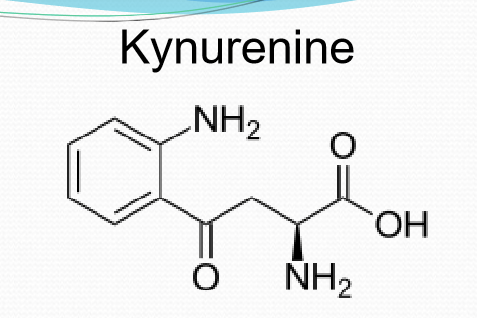
What are the consequences of kynurenine’s tendency to undergo deamination and oxidation?
Becomes a chromophore and can be a precursor to nuclear cataract.
Modification of what chemical can also produce chromophore?
Ascorbate
What can the over expression of kynurenine cause?
Cataracts in transgenic mouse models
How is cataracts classified?
Cause: age, congenital, environment
Region of lens affected: nuclear (C), cortical (B), Posterior subcapsular (D), Mixed
Progressive
Clinically defined by a type and grade
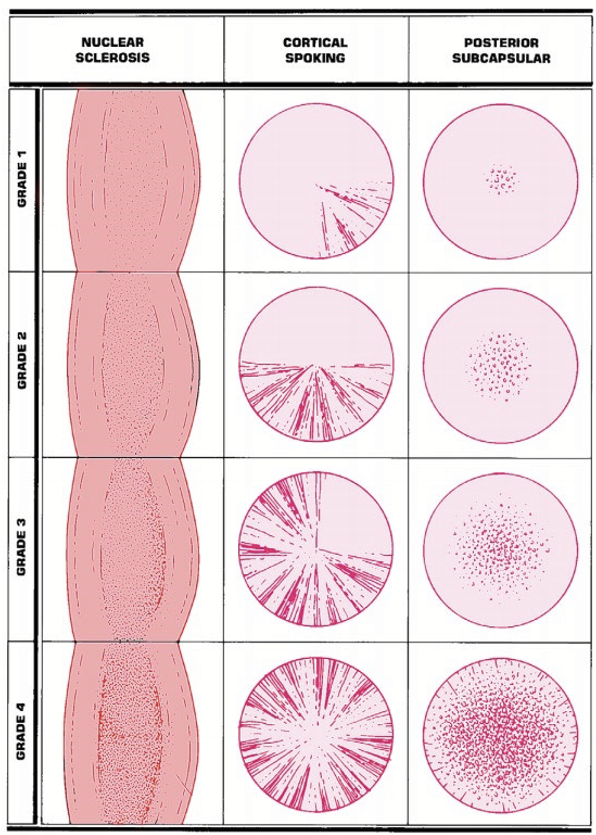
What is the most common type of cataracts?
Nuclear cataracts (60% of surgeries)
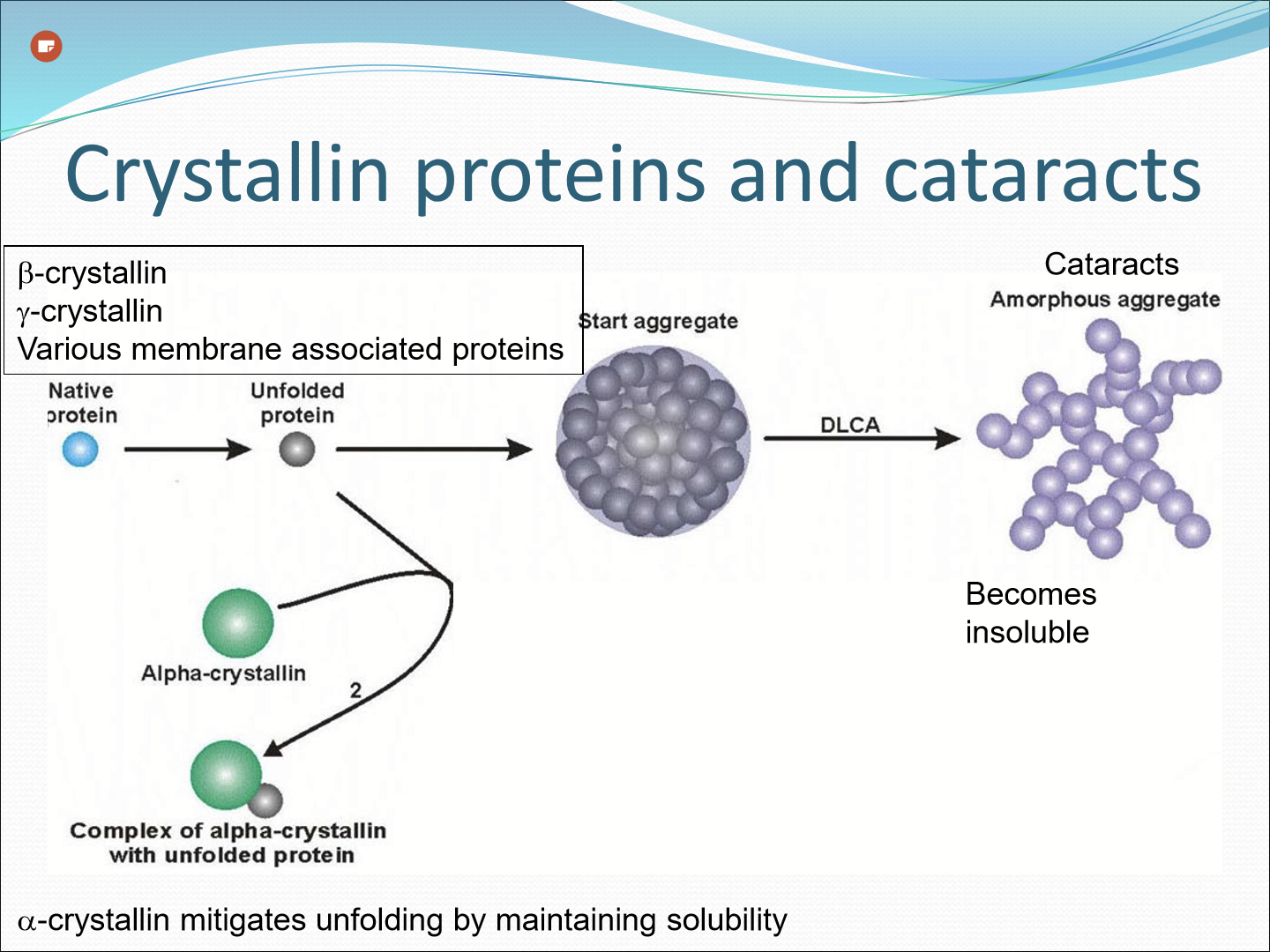
What causes age-related nuclear cataracts
Disulfide bond formation between protein subunits aggregate proteins
Crystallin protein-lipid membrane intractions
Increase in oxidized glutathione in lens nucleus
Progressive failure in glutathione-dependent reduction pathways
proteins losing solubility
What are the 3 major crystallin proteins in the lens?
alpha, beta, and gama crystallins.
What role does alpha-crystallins have?
Chaperone-like activity: prevents protein unfolding and promotes protein solubility to keep lens clear
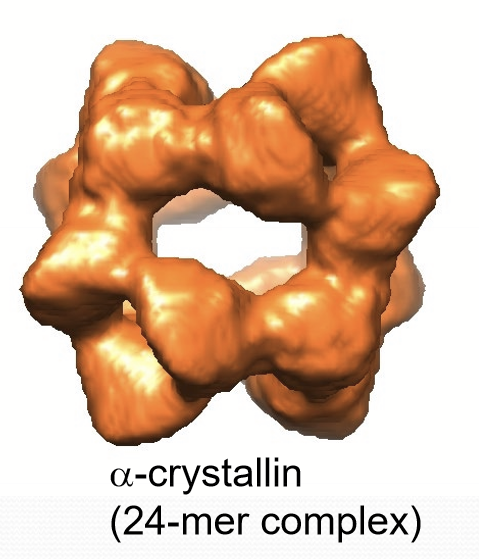
What happens to soluble alpha-crystallin with age?
It creases with age in the lens nucleus, decreasing its ability to maintain the solubility of other proteins.
What happens as the solubility of beta and gama cyrstallin and other proteins become reduced with age?
Alpha-crystallin is overwhelmed and insoluble crystallin and protein aggregates form.
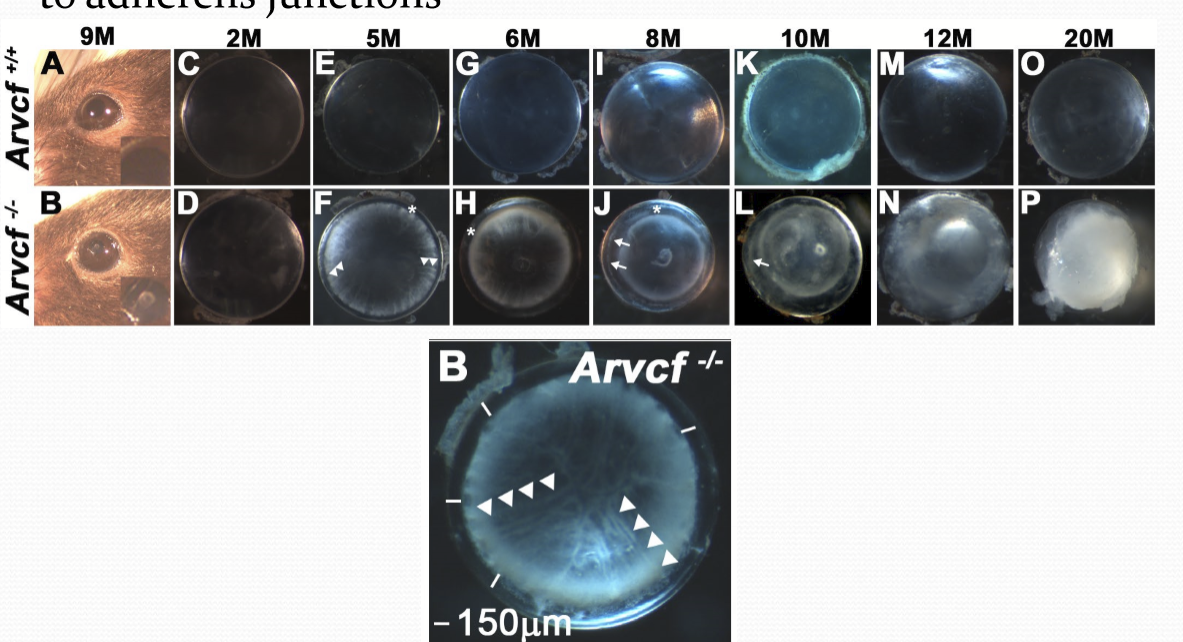
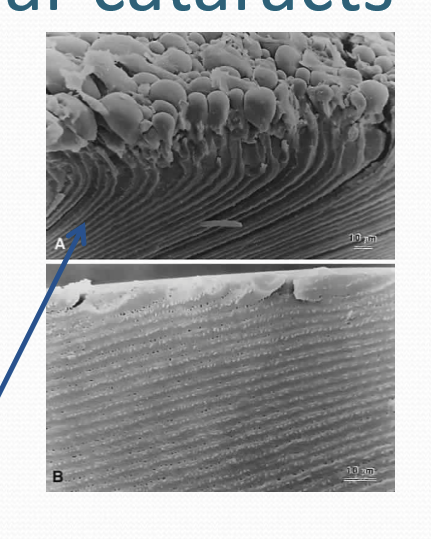
Where does cortical cataracts most often occur?
In the inferior/nasal quadrant of the lens. May spread around the lens circumference over the course of years. opacities tend to occur in the central portion of the affected fiber cells around equator. Extend along fibers as cortical spokes.
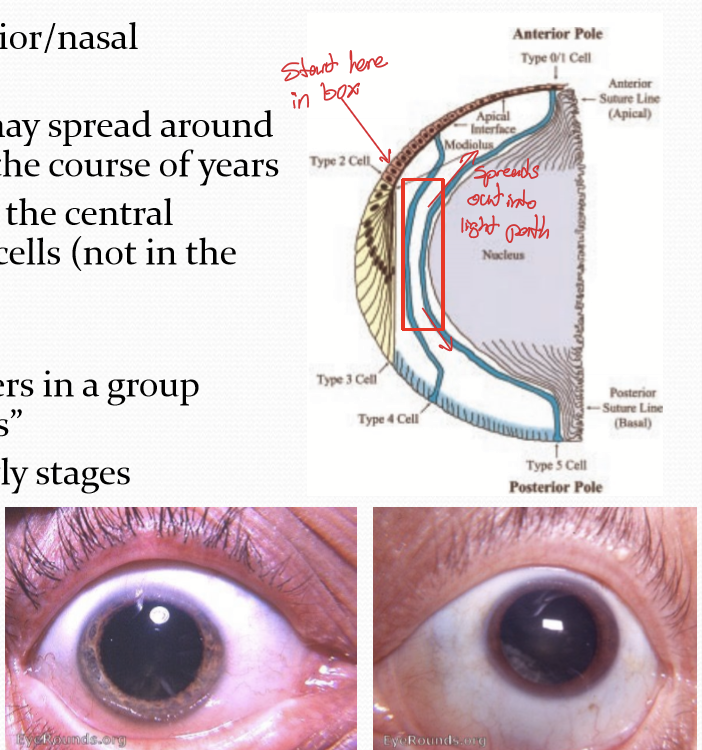
What causes cortical cataracts?
Disruption to adherens junctions.
What is posterior subcapsular cataracts?
Light scattering in cluster of swollen cells at the posterior pole just beneath capsule. It is less common than nuclear or cortical cataracts.
What is the cause of posterior subcapsular cataracts?
Aberrant migration or differentiation of lens epithelial cells
Can be induced by radiation
Use of intravitreal steroids
Swelling of posterior ends of fibers along the suture planes
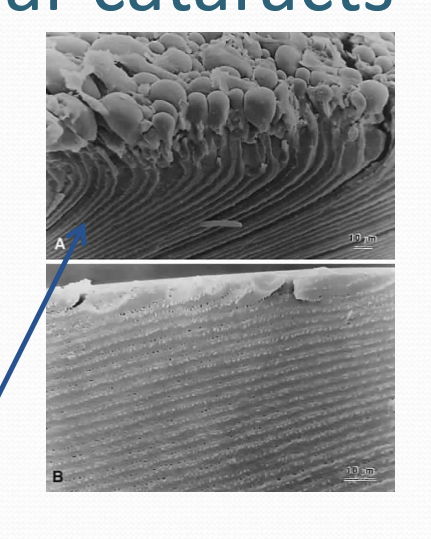
What is anterior polar cataract (APC)?
Formation of an opaque plaque near center of lens epithelium. It is made of spindle-shaped lens epithelial cells embedded in a large amount of extracellular matrix.
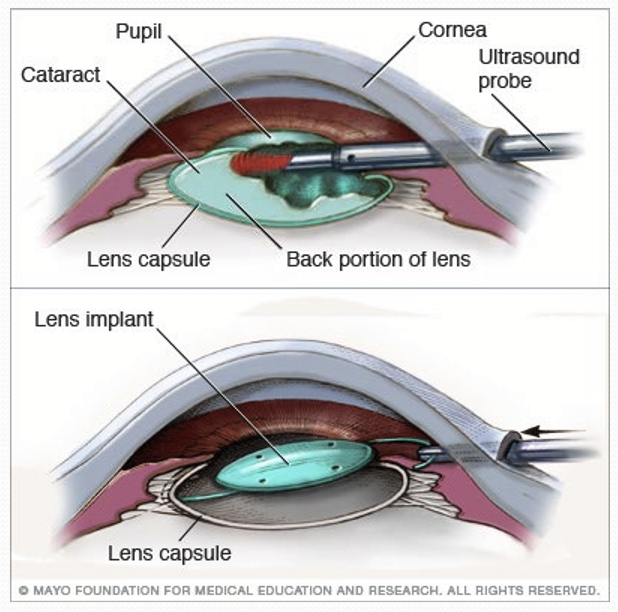
How is cataracts treated?
Surgical intervention. Cataract affected lenses are removed via peripheral corneal incision and a phacoemulsification instrument. Subsequent replacement with an artificial lens.
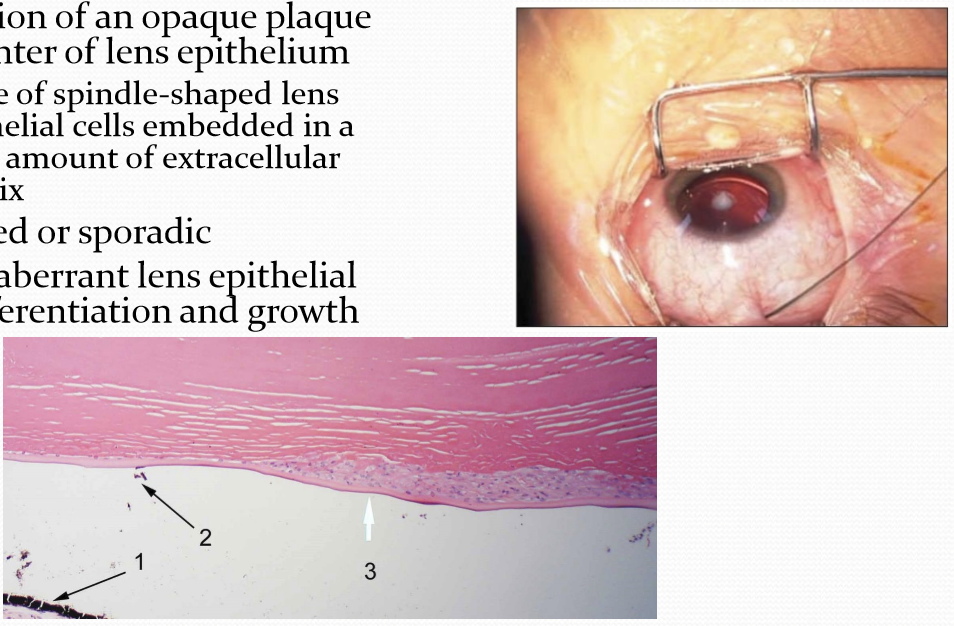
What is secondary cataracts?
Posterior capsular opacification, a frequent complication of extracapsular cataract surgery, where lens epithelial cells remaining after surgery differentiate into a mass of fiber like cells.
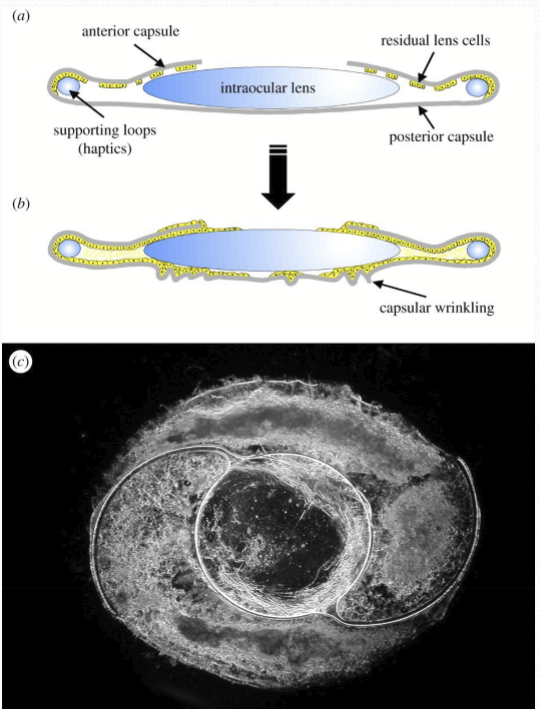
What happens if the cells migrate further onto the posterior capsule?
Formoation of lentiod like bodies: unorganized clumps of cells and scatter light.
What is used to treat secondary cataracts?
YAG laser capsulotomy.