Malignant Hyperthermia
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
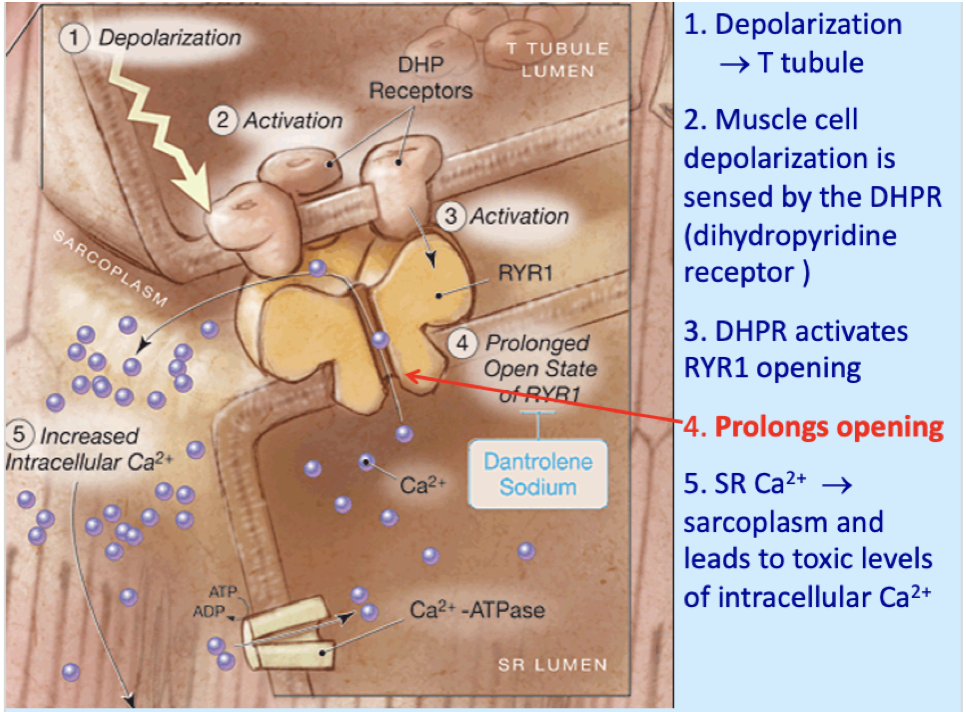
What occurs after depolarization that causes MH to occur?
When does rigidity occur in MH?
when unbound Ca reaches contractile threshold
What causes the fever and acidosis associated with MH?
Oxidative phosphorylation (synthesis of ATP - aerobic metabolism)
But, excess Ca is absorbed into mitochondria ⇢causes toxic concentrations that uncouples oxidative phosphorylation from electron transport chain ⇢leading to decreased ATP production
This causes lactate acid and heat production
anaerobic metabolism accelerated O2 consumption and heat
Once ATP is depleted, what occurs?
the pumping systems fail, so ions/molecules follow their concentration gradients, and cell death can occur
When ATP pumps fail, what moves in and out of the cell and what are some results?
Movement into cells:
Na+ with H2O - swelling
Ca2+ - worsening the intracellular derangement
Movement out of cells:
K+
Phosphorylase
Magnesium
Later: Enzymes and myoglobin
Obstructs renal tubules ®ARF
Cell death
Initial heat production probably is due to increased _____________, and later it is due to___________ production
aerobic metabolism; lactate (anaerobic)
what is Tismus Masseter Spasm or Masseter Muscle Rigidity (MMR)?
a condition that occurs most often with succs or in children after inhalation induction
normally pathologic, but may be benign bc it does occur in non-MHS people
What will a peripheral nerve stimulator show if it is Masseter Muscle Rigidity?
flaccid paralysis (usually)
What are differential diagnoses for Masseter Muscle Rigidity?
Myotonic syndrome
TMJ
Underdosing of SCh (in true MMR, repeat succs will not relieve issue)
Not allowing sufficient time for SCh to work prior to intubation
Treatment options for MMR?
cancel elective surgeries and treat s/s
in a hospital, you can d/c triggers, treat s/s, and consider dantrolene (should NOT be done in surgery centers or where ICU is not available)
Which labs should be checked if MMR occurs?
Obtain creatine kinase levels at 6, 12 and 24 hrs after episode
Levels >20,000 IU → MH is more likely cause
Check myoglobin
Serum (>170 mcg/L)
Urine (>60 mcg/L)
Early signs of MH
hypercarbia, MMR, tachycardia, and fever(fever use to be a later sign, but is now considered an early sign)
Why does hypercarbia occur in MH?
the increased metabolism increases O2 consumption and CO2 production resulting in metabolic acidosis (can lead to tissue hypoxia- increases temp and potassium)
What is a good sign of MH that anesthesia can monitor for?
increase in EtCO2 that is resistant to changes in MV (any unexplained rise in CO2 should be investigated)
What is often the first recognized sing of MH?
tachycardia
Other signs of MH
HTN
Hyperkalemia (>6)
cyanosis
What is the clinical hallmark sign of MH
fever (can climb 1-2C per 5 mins)
How does succs influence muscle rigidity from MH?
Will make rigidity occur faster
Repeat doses will worsen the stiffness
What does muscle rigidity eventually cause?
Rhabdomyolysis / Myoglobin release ®ARF
Monitor for compartment syndrome
Cases exist that this was only sign (postop)
K+ release ®cardiac arrest
CK release
How does MH effect the pulm system
Acidosis and hypoxemia
Tachypnea due to acidosis
Pulmonary edema can result with overzealous fluid administration
how does MH effect the renal system
Low output (oliguria, anuria) secondary to shock
Myoglobinuria will block renal tubules ®ARF
ARF is a problem with hyperkalemia
How does MH effect the CNS
Extreme: coma, areflexia, unresponsiveness
ICP due to systemic manifestation i.e. temp, acidosis, K+, hypoxia, cell membrane dysfunction
How can MH impair coagulation?
DIC due to release of tissue thromboplastin during high temp, acidosis, hypoxia, and hypoperfusion
Impaired coag associated with hemolysis, marked decrease in platelets, fibrinogen, and factor VIII
How can MH result in mortality?
Ventricular arrhythmias (hyperkalemia)
Acute pulmonary edema
Brain death (edema, temp, acidosis)
Acute DIC
ARF
Differential diagnoses from MH
Neuroleptic Malignant Syndrome (NMS)
Hyperkalemic cardiac arrest
Sudden unexpected cardiac arrest, exposed tocertain meds (mainly succs), assume Hyperkalemia
Pheochromocytoma (HR, HTN and fever, but lacks the metabolic changes / response)
Thyroid storm (lacks acid-base abnormality)
Elevated ETCO2
Lap cases, faulty humidifier or CO2 exhausted
Septicemia - fevers
Blood product reactions
Light anesthesia
Cocaine or other drug toxicity
Seizure disorder
CNS bleed
s/s of neuroleptic malignant syndrome
Fever, tachycardia, HTN, rhabdomyolysis, tachypnea, diaphoresis, muscle rigidity and acidosis (extrapyramidal effects, pulmonary congestion, dyspnea, stupor, LOC)
Mortality is about 20%
Which drugs are associaated with NMS?
Virtually all classes of drugs (in therapeutic range) that induce dopamine-2 receptor blockade have been associated with NMS
Haloperidol, phenothiazines, butyrophenones, lithium, and MAO inhibitors
Antiemetics (prochlorperazine), pro-peristaltic agents (metoclopramide), anesthetics (droperidol), and sedatives (promethazine)
Sudden withdrawal from meds treating Parkinson’s also may trigger NMS
treatment for NMS
Bromocriptine, amantadine (dopamine agonists)
Benzodiazepines and dantrolene
How does NMS compare to MH
NMS has slow onset / patient need not be MH susceptible
MH is acute
NMS is not inherited (problem with drugs affecting the brain)
MH is inherited (problem with skeletal muscle receptors & Ca control)
Can relax patient with NDMR
MH patients may have break-through rigidity
Who is most at risk for developing hyperkalemic cardiac arrest post succs?
pts suffering from undiagnosed subclinical myopathy like muscular dystrophy (more common in boys under 10)
How do you treat cardiac arrest due to hyperkalemia?
Rule out hypoxia and ventilatory problems first, then treat hyperkalemia:
CaCl2, bicarb, insulin, glucose, hyperventilate
Resuscitation may be prolonged and difficult
This reaction is usually not MH
However, it is described on MH posters as cautionary
Which non-MH disease can result in life threatening hyperkalemia and rhabdo when triggering agents are given?
Dystrophinopathies
Duchene’s and Becker muscular dystrophies
Genetic mutation is on X chromosome (MH is chromosome 19)
Diseases/conditions associated with or related to MH (Predisposing – from high to low)
Central core disease (CCD) & MultiminiCore disease (MmD) with RYR1 mutation
Rare familial polymyopathyies characterized by hypotonia, delay in walking, muscle weakness
(core: bx is stained and a central area of muscle fiber doesn't stain)
King-Denborough Syndrome (KDS)
Periodic Paralysis
History of unexplained fevers without diagnosis
Previous episode of rhabdomyolysis without diagnosis
History of dark-colored urine
EHI / ER
Which gene mutations have been linked with MH?
Chromosome 19- Ryanodine (RYR1)
over 50% of cases
CACNA13
codes for DHP and is directly coupled with RYR1
CaV1.1
STAC 3 (SH3)
What is CaV1.1?
AKA DHP Receptor that controls voltage gated Ca channel
What does a mutation of CaV1.1 cause?
causes a gain of function that makes RyR1 hypersensitive to caffeine and anesthetics in MHS causing excessive release of Ca into cytosol
Which MH gene mutation has been linked to Native american myopathy?
STAC3
WHat is the gold standard lab test for diagnosis of MH?
a muscle biopsy with Caffeine Halothane Contracture (CHCT) Test
How is a caffeine halothane contracture test performed?
A muscle biopsy is taken from the vastus lateralis muscle. The fiber are suspended in a Kreb’s solution. Halothane is bubbled through, caffeine and Ryanodine are added and contraction is measured
How accurate is the CHCT test?
97% sensitivity and 78% specific (false positives like 20% of the time with other myopathies that are not MH)
Indications for a CHCT test
Patient with known MHS relative (tested positive by muscle biopsy)
Patient with MHS relative (suspicious episode)
Patient with past suspected MH event
Patient with severe MMR
Patient with mild to moderate MMR + rhabdomyolysis
Patient with unexplained rhabdomyolysis during or after surgery or with exercised-induced rhabdo
Signs suggestive of MH, but not definitive
If military service is desired, patients with suspicion of MHS are required to undergo CHCT
What test, other than CHCT, can be done for diagnosis of MH?
creatinine kinase- must be elevated in 3 different occasion and is not specific to MH (>20,000 IU after MMR indicates an ~80% likelihood the patient will have positive contracture test, but CK is often higher if SCH was used)
genetic testing- does not replace the muscle biopsy bc not all mutations are Id’d
How do you prepare dantrolene?
it comes as a lyophilized yellow/orange substance with 20 mg Dantrolene and 3000mg Mannitol/NaOH. it is reconstituted in 60 ml of sterile water w/o bacteriostatic agent. It can be warmed to 37-39C for faster mixing. shake for 20 secs or until solution is clear (20mg/60mL)
Dantrolene dosing
Initial dose of 2.5 mg/kg and a total dose of 10 mg/kg
titrated to HR, PaCO2, and rigidity
if not subsided after 10-30 mg/kg, probs not MH
Post-op: 1mg/kg IV q 6hrs for 24 hrs and PO for 24 hrs or more after
There is a new formulation of Dantrolene called Ryanodex, how does preparation of this formulation differ?
it is reconstituted with 5mL sterile water and is ready in 1 min (250mg/5mL = 50 mg/mL)
requires a LOT less vials and overall fluids than other preparations (3 bottles=35 bottles)
does not contain large doses of mannitol, like other preparations
Why can dantrolene not be reconstituted with NS?
it causes precipitate and results in a hypertonic solution (526mOsm/L) almost double what it is when reconstituted with sterile saline (261 mOsm/L)
MOA of Dantrolene
acts in the SR of skeletal muscle (little efefct on heart and smooth muscle) and acts by reducing Ca release by the SR or inhibiting excitation contractures at the transverse tubules
does NOT effect Ca reuptake, electrical activity, or rate of ACH synthesis
Cons of dantrolene
Drowsiness, nausea, weakness
Potentiates NDMR
Placental transfer
Can cause fetal weakness
Also can cause uterine atony →bleeding
can alter liver function when used long-term
What other conditions can dantrolene be used in?
Management of spasticity resulting from upper motor neuron disorders:
MS, cerebral palsy, spinal cord injury, CVA
Muscle breakdown from
Heat strokes, cocaine & MDMA (ecstasy)
If MH occurs, call for help… then what? (step 1 of the process)
Discontinue triggers
Hyperventilate – lower CO2
100% O2 high flow rates at > 10 L/m
Place charcoal filters (replace each hour in crisis event)
Halt surgery when possible and/or continue with non triggering agents
Do not waste time changing circle system & absorbent
Consider more vascular access
Foley
Switch to core temperature monitoring
What are the steps 1-7 on the Malignant Hyperthermia Card?
1-Callfor help, get dantrolene, notify surgeon, and call MH hotline
2- give dantrolene
3- Treat acidosis
4-cool the pt
5- dysrhythmias
6- hyperkalemia
7- follow
How should acidosis be treated (step 3)?
give 1-2 mEq/kg of bicarb until blood gas is available
How should pt be cooled (step 4)?
cool to 38C (COOL, BUT DON”T OVERCOOL)
give cool IV of Plyte or NS
lavage open cavities with cool saline
ice packs
pharmacological cooling
can use invasive techniques
If dysrhythmias occur (step 5), dantrolene should correct it, but if not uses standard drug therapies, but avoid the following drugs:
Ca channel blockers- can worsen hyperkalemia and cause cardiac arrest in the presence of Dantrolene (do not withhold dantrolene if pts are on these drugs)
lidocaine and procainamide- avoid if hyperkalemic can cause wide QRS
How to treat hyperkalemia (step 6)?
Bicarb 1-2 mEq/kg
Reg insulin 10 units with 50 mL of 50% dextrose – adults
Reg insulin 0.1 units/kg with 2mL/kg of 25% dextrose – peds
CaCl 10 mg/kg IV (Cal gluconate 10-50 mg/kg) - for life-threatening K
Albuterol or B2 agonist nebulized can lower K
Check glucose hourly
What steps are included in step 7: Follow?
ETCO2 & minute vent
Blood work
ABGs, lytes, BG, CK
Venous gases may show hypermetabolism before arterial
Coags
DIC treatment
Heparin, FFP, PLT, and clotting factors
Core temp
Urine – amount and color and prevent rhabdomyolysis
Fluids greater than 2 mL/kg/hr
Diuretics
How long should pt be monitored post-op with MH attack?
at least 24 hrs (continue dantrolene for 24 hrs) and check CK q 6 hrs
Where should pts be referred after an event of MH?
MHAUS- have resources and counseling
call hotline and fill out a adverse metabolic or muskuloskeletal reaction to anesthesia form so it can be documented for pt anaonymously (even if they do not want the referral)
For pts with known MH, where can providers get a thorough history of the pt?
North American MH registry in Fl will have the pt database which contains:
Adverse anesthetic events
Family MH history
Muscle biopsy result
Subsequent anesthesia course
Patient info can be anonymous (will need pt signed consent to receive info and must give th ept’s name, BD, and mom’s maiden name)
If a pt has known MH, how should anesthesia be given?
Avoid triggers
Monitoring and labs
Routine monitoring including temp
Labs: maybe ABGs with electrolytes / coags / CPK / myoglobin
Postop: keep 4-6 hours before discharge
Dantrolene should be accessible within ten minutes of the first signs of MH
Should have the capacity to administer at least 10 mg/kg of dantrolene in the event of an acute MH episode
prepare AGM prior to surgery
How can the GAM be adjusted for an MH case?
use a charcoal filter
Physically disconnect vaporizers from the workstation
Tape message over ones that cannot be removed
Use a new, disposable breathing circuit
Replace absorbent
Follow AGM manufacturer recommendations for flushing
What anesthetic can be used for a muscle biopsy for suspected MH>?
Adults: lateral femoral cutaneous nerve block
Children: GA with safe agents
How is a charcoal filter used?
used to remove unwanted anesthetics from breathing circuit
Setup: flush oxygen 10 L/m for 90 sec - then place filters
they are labeled insp and exp (do not switch them)
Keep gas flow at least greater than 3 L/m during case
Filters are good for up to 12 hours once placed – change q 12 hrs
However, during a crisis change every hour
How much does a charcoal filter improve care?
Without the activated charcoal filters it took
Took 55 min to reach less than 5 ppm of isoflurane
With the activated charcoal filters
Inspired iso concentration was quickly less than 5 ppm
Charcoal filters: elective and during crisis
What can be done to the GAM if charcoal filters are not available?
flush the workstation (may take 10-90mins
during the case, FGF may need to be >10L/m to avoid rebound phenomenon
use a dedicated vapor free machine (unusual to have spare machine)
use an ICU vent that has never been exposed to volatile agents
What is rebound phenomenon?
increased release of residual volatile anesthetic agent when fresh gas flow is reduced after a set period of flushing