ch 23 pt 2 (digestive)
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
small intestine
-major organ of digestion and absorption!!!
is 2-4m long; from pyloric sphincter to ileocecal valve
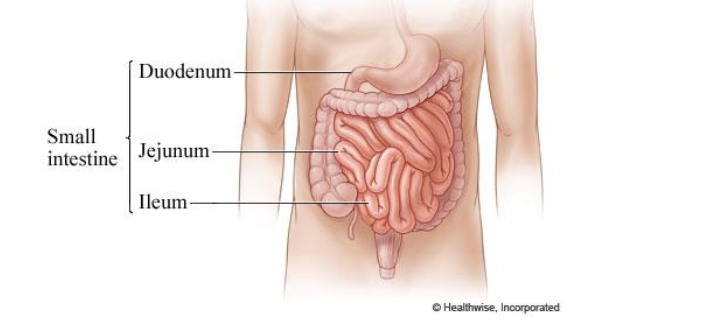
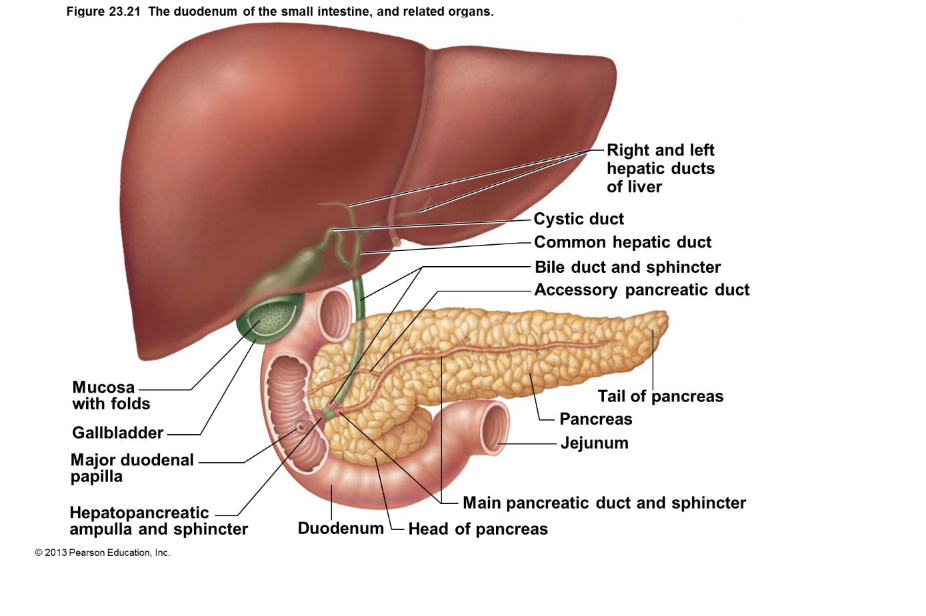
duodenum
Curves around head of pancreas; shortest part – 25 cm
• Bile duct (from liver) and main pancreatic duct (from pancreas)
– Join at hepatopancreatic ampulla
– Enter duodenum at major duodenal papilla
– Entry controlled by hepatopancreatic sphincter
duodenum of small intestines and related organs
Liver: The liver produces bile, which is transported thru the right and left hepatic ducts.
Gallbladder: The gallbladder stores and concentrates bile. The bile duct from the gallbladder is the cystic duct.
Common Hepatic Duct: The right and left hepatic ducts from the liver merge to form the common hepatic duct.
Common Bile Duct: This duct is formed by the union of the cystic duct and the common hepatic duct. It carries bile to the duodenum.
Pancreas: The pancreas is a gland that produces digestive enzymes. The main pancreatic duct carries these enzymes to the duodenum.
Duodenum: This is the first part of the small intestine. The hepatopancreatic ampulla and sphincter is the point where the common bile duct and the main pancreatic duct join and enter the duodenum.
structural modifications of SI that increase SA for digestion & absorption
* Villi: These are finger-like projections lining the small intestine. They increase the surface area to help absorb nutrients.
* Microvilli: These are tiny, hair-like structures on the surface of the villi. They further increase the surface area for absorption.
* Epithelial Cells: These cells cover the villi and absorb nutrients from digested food.
* Capillaries: Tiny blood vessels that absorb nutrients and transport them to the bloodstream.
* Lacteal: A lymphatic vessel within the villus that absorbs fats and fat-soluble vitamins.
* Goblet Cells: Cells that secrete mucus to protect the lining of the intestine.
* Muscle Layers: Layers of muscle tissue that help move food through the intestine.
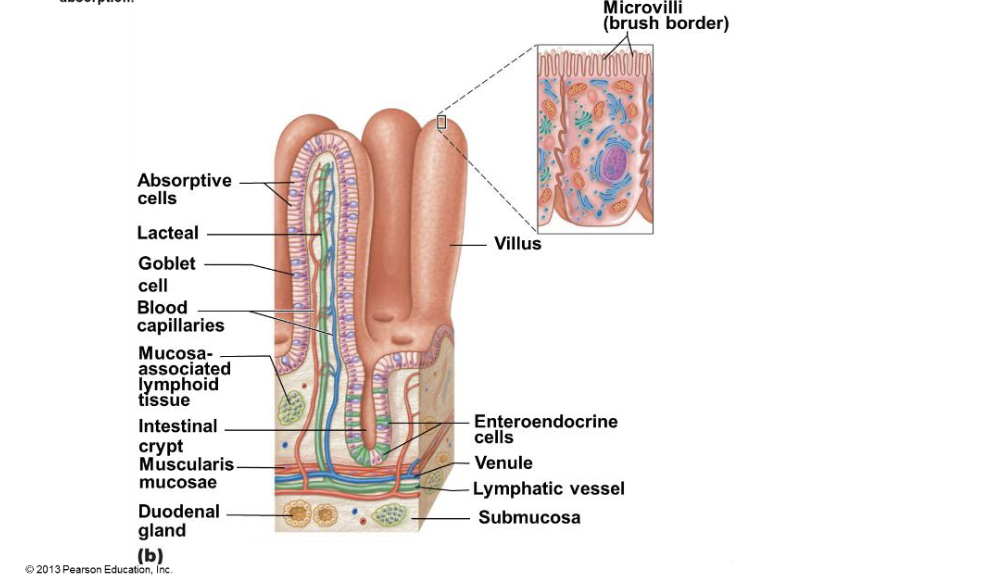
circular folds
-permanent folds (~1 cm deep) that force chyme to slowly spiral thru lumen→ more ↑ nutrient absorption
vili
extensions (~1 mm high) of mucosa with capillary bed and lacteal for absorption
*increase surface area for absorption
microvilli
aka brush boarder
-contains enzymes for carbohydrate and protein digestions
*increase surface area for absorption
Intestinal crypt epithelium
renewed every 2-4 days
– Most - secretory cells that produce intestinal juice
– Enteroendocrine cells enterogastrones
– Stem cells divide to produce crypt cells
– Chemotherapy and radiation therapy targets rapidly dividing cells
– Kills cancer cells but…
– Kills rapidly dividing GI tract epithelium
– So…. Many patients undergoing chemotherapy or radiation therapy often suffer from
nausea, vomiting, diarrhea
liver
many functions: only digestive function→ bile production
liver has bile which is a fat emulsifier
gallbladder
-chief function→ bile storage
bile
Yellow-green, alkaline solution containing
– Bile salts - cholesterol derivatives that function in fat emulsification and absorption
– Bilirubin - pigment formed from heme
• Bacteria break down in intestine to stercobilin → brown color of feces
Homeostatic imbalance
Hepatitis
– Usually viral infection, drug toxicity, wild mushroom poisoning
• Cirrhosis
– Progressive, chronic inflammation from chronic hepatitis or alcoholism
– Liver → fatty, fibrous → portal hypertension
• Liver transplants successful, but livers scarce
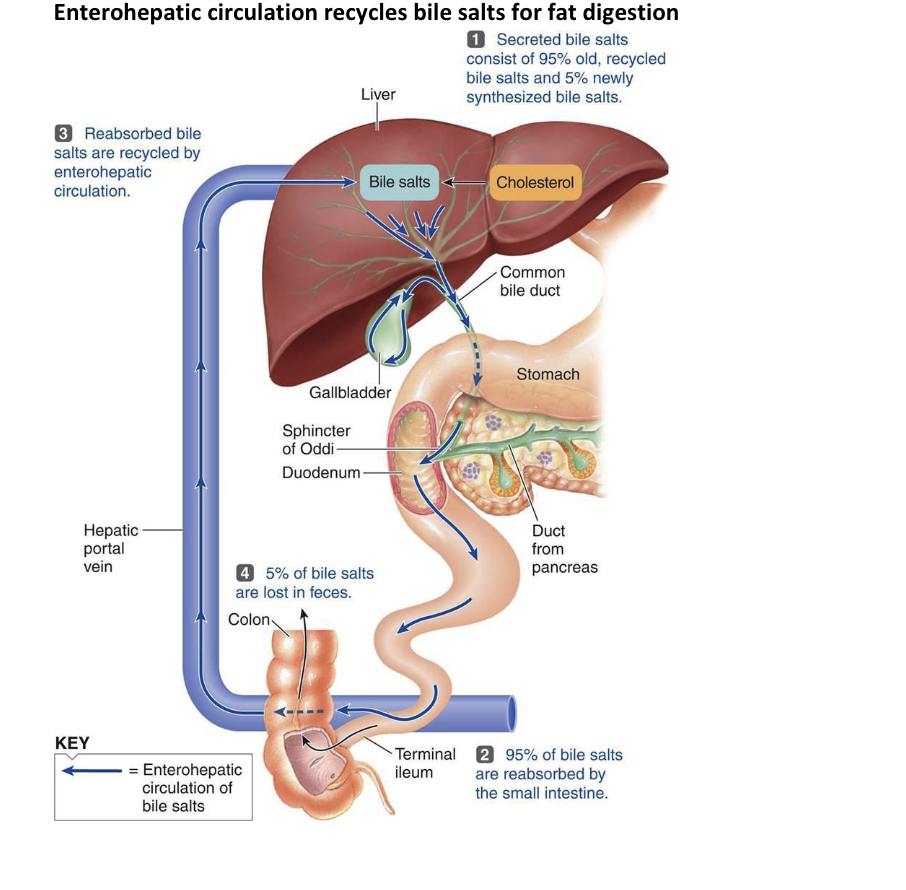
enterohepatic circulation
what recycles bile salts for fat digestion?
chart on how bile salts are recycled in the body to help digest fats.
The image illustrates the enterohepatic circulation, which is how bile salts are recycled in the body to help digest fats.
1. The liver makes bile salts.
2. Bile salts are used in the small intestine to digest fats.
3. Most (95%) of the bile salts are reabsorbed in the small intestine.
4. The reabsorbed bile salts go back to the liver.
5. A small amount (5%) of bile salts are lost in feces.
This cycle helps the body efficiently use bile salts for fat digestion.
gallstones
High cholesterol; too few bile salts gallstones (biliary calculi)
– Obstruct flow of bile from gallbladder
• May cause obstructive jaundice
– Gallbladder contracts against sharp crystals → pain
– Treated with drugs, ultrasound vibrations (lithotripsy), laser vaporization, surgery
gallstones
High cholesterol; too few bile salts → gallstones (biliary calculi)
– Obstruct flow of bile from gallbladder
• May cause obstructive jaundice
– Gallbladder contracts against sharp crystals pain
– Treated with drugs, ultrasound vibrations (lithotripsy), laser vaporization, surgery
pancreas
Endocrine function:
– Pancreatic islets secrete insulin and glucagon to control blood sugar
• Exocrine function:
– Acini (clusters of secretory cells) secrete pancreatic juice
• To duodenum via main pancreatic duct
• Zymogen granules of acini cells contain proenzymes
Pancreatic Juice
• Watery alkaline solution (pH 8) neutralizes chyme
• Electrolytes (primarily HCO3–)
• Enzyme rich!!
– Amylase, lipases, nucleases secreted in active form but require ions or bile for optimal
activity
– Proteases secreted in inactive form…why?? To prevent digestion of the pancreas and
ducts
• Protease activation in duodenum
• Trypsinogen activated to trypsin by brush border enzyme enteropeptidase
• Procarboxypeptidase and chymotrypsinogen activated by trypsin
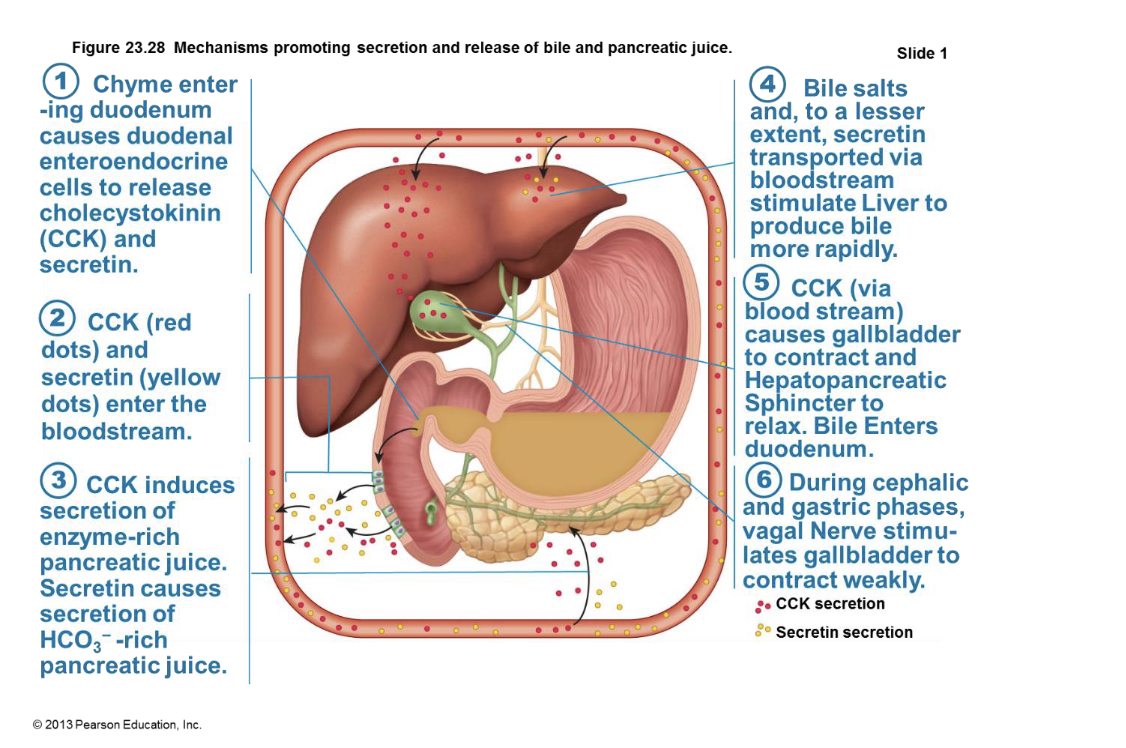
mechanisms promoting secretion and release of bile and pancreatic juice
The image illustrates how the body regulates the secretion and release of bile and pancreatic juice.
1. Chyme enters the duodenum, triggering the release of cholecystokinin (CCK) and secretin.
2. CCK and secretin enter the bloodstream.
3. CCK stimulates the pancreas to secrete enzyme-rich juice, while secretin causes the pancreas to secrete bicarbonate-rich juice.
4. Bile salts and secretin stimulate the liver to produce bile.
5. CCK causes the gallbladder to contract, releasing bile into the duodenum.
6. During cephalic and gastric phases, the vagal nerve stimulates the gallbladder to contract weakly.
large intestine (colon)
Residue remains in large intestine 12–24 hours
• No food breakdown except by enteric bacteria!!
• Vitamins (made by bacterial flora), water, and electrolytes (especially Na+ and Cl–) reclaimed
(although less than small int.)
• This essentially converts diarrhea to normal feces
• Major functions - propulsion of feces to anus; defecation
• Colon not essential for life!!
• Most contractions of colon
• Haustral contractions
• Slow segmenting movements
• Haustra sequentially contract in response to distenvsion
• Gastrocolic reflex (stomach>>colon)…make some room!!
• Initiated by presence of food in stomach
• Activates three to four slow powerful peristaltic waves per day in colon (mass
movements)
Homeostatic Imbalance: Diverticula split card
• Low fiber diet → narrowed colon → strong contractions → increased pressure on walls → diverticula (herniations of mucosa)
• Diverticulosis commonly in sigmoid colon
– Affects ½ people > 70 years
• Diverticulitis
– Inflamed diverticula; may rupture and leak into peritoneal cavity; may be life
threatening
Homeostatic Imbalance: Irritable bowel syndrome
– Symptoms: Recurring abdominal pain, stool changes, bloating, flatulence, nausea,
depression
– Stress common precipitating factor
• Stress management important in treatment
– doesn't cause permanent damage to your colon
defecation reflex chart
1. Feces enter the rectum, stretching its walls.
2. Stretch receptors send signals to the spinal cord.
3. The spinal cord initiates a reflex: the rectum and sigmoid colon contract, and the internal anal sphincter relaxes.
4. If it's a good time to go, the brain allows the external anal sphincter to relax, and feces are eliminated.
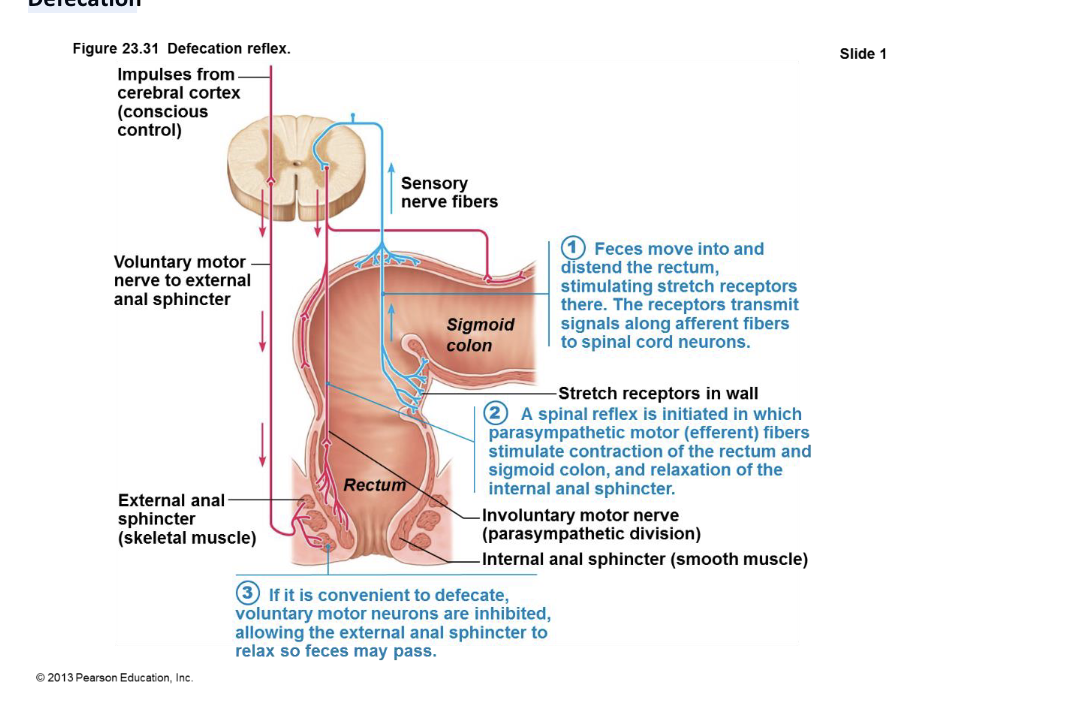
defecation
Muscles of rectum contract to expel feces
• Assisted by Valsalva maneuver
– Closing of glottis, contraction of diaphragm and abdominal wall muscles → increased
intra-abdominal pressure
– Levator ani muscle contracts → anal canal lifted superiorly → feces leave body
chemical digestion
What is chemical digestion?
– Catabolic
– macromolecules → monomers small enough for absorption
• What is involved??
– Enzymes
• Intrinsic and accessory gland enzymes break down food
– Hydrolysis
• Water is added to break bond
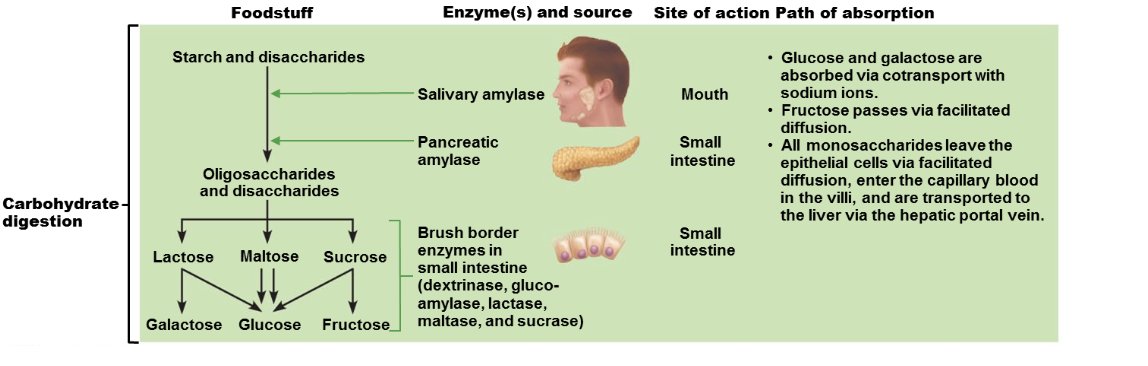
digestion of carbohydrates
Only monosaccharides can be absorbed!!
Monosaccharides absorbed as ingested
– Glucose, fructose, galactose
• Digestive enzymes:
– Salivary amylase & pancreatic amylase break down starch
– brush border enzymes (dextrinase, glucoamylase, lactase, maltase, and sucrase) Break
down disaccharides sucrose, lactose, maltose; polysaccharides glycogen and starch
carbohydrate digestion chart
1. Starts in the Mouth: Salivary amylase begins breaking down starch.
2. Continues in the Small Intestine: Pancreatic amylase and brush border enzymes further break down carbohydrates.
3. Absorption: Glucose and galactose are absorbed with sodium. Fructose uses facilitated diffusion.
4. Transport: Monosaccharides enter blood capillaries and go to the liver.
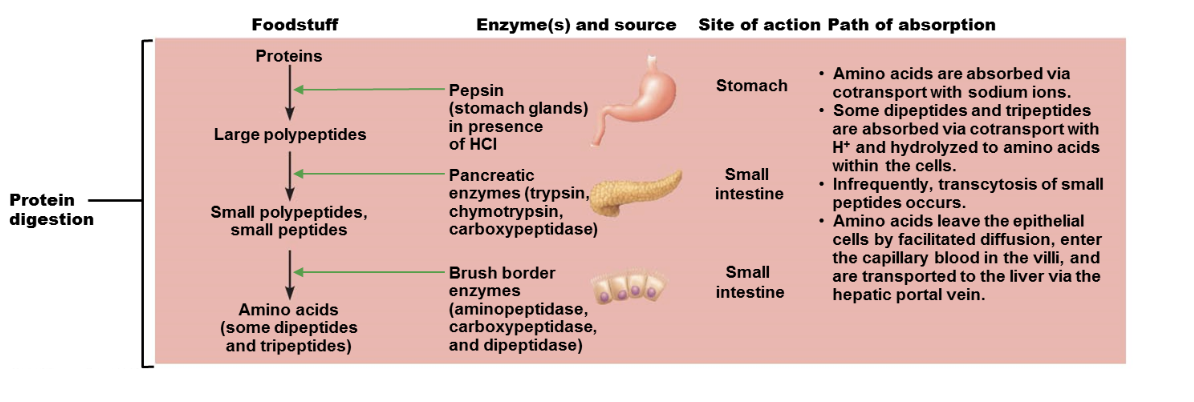
Digestion of Proteins
• Begins with pepsin in stomach at pH 1.5 – 2.5
– Inactive in high pH of duodenum
• Pancreatic proteases
– Trypsin, chymotrypsin, and carboxypeptidase
• Brush border enzymes
– Aminopeptidases, carboxypeptidases, and dipeptidases
• Trypsin &Chymotrypsin chop up proteins >> fragments
• Aminopeptidases and carboxypeptidases pull one amino acid at a time off the ends of proteins
protein digestion chart
1. Foodstuff: Proteins are the starting point.
2. Stomach: In the stomach, proteins are broken down into large polypeptides by pepsin in the presence of HCl.
3. Small Intestine:
* Pancreatic enzymes (trypsin, chymotrypsin, carboxypeptidase) further break down polypeptides into smaller peptides.
* Brush border enzymes (aminopeptidase, carboxypeptidase, and dipeptidase) break down peptides into amino acids, dipeptides, and tripeptides.
4. Absorption:
* Amino acids are absorbed into the cells with sodium ions.
* Dipeptides and tripeptides are absorbed with H+ and converted to amino acids inside the cells.
* Amino acids move from the cells into the blood vessels and are transported to the liver.
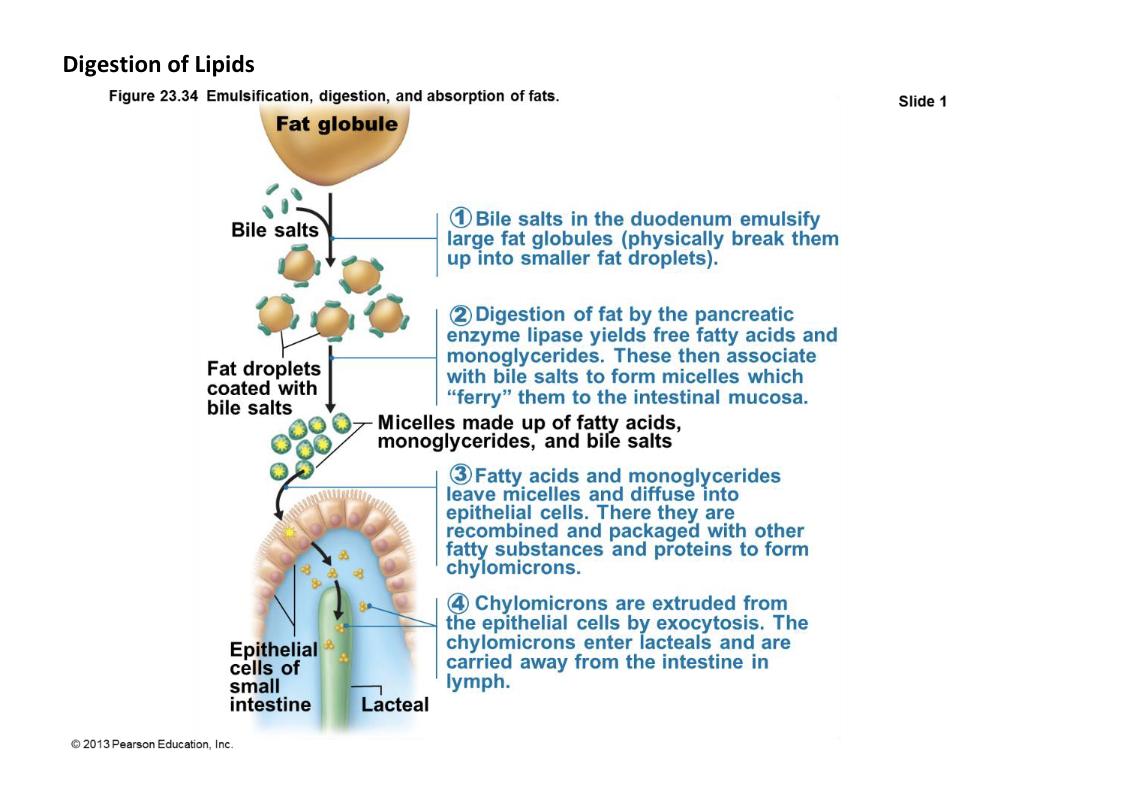
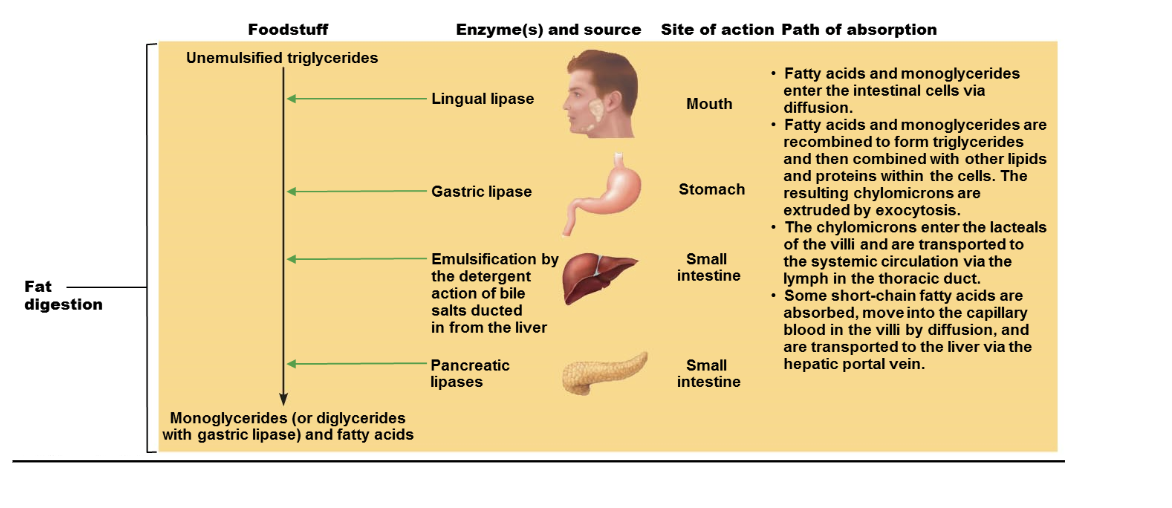
digestion of lipids
1. Emulsification: Bile salts in duodenum break down large fat globules into smaller droplets.
2. Digestion: Pancreatic enzymes break down fats into fatty acids and monoglycerides.
3. Absorption: Fatty acids and monoglycerides enter epithelial cells.
4. Chylomicron Formation: Fatty substances and proteins combine to form chylomicrons.
5. Transport: Chylomicrons are released and transported in lymph.
fat digestion chart
1. Mouth and Stomach: Fat digestion begins with lingual and gastric lipases.
2. Emulsification: Bile salts from the liver break down large fat globules into smaller ones.
3. Small Intestine: Pancreatic lipases break down triglycerides into fatty acids and monoglycerides.
4. Absorption: Fatty acids and monoglycerides are absorbed into intestinal cells.
5. Chylomicron Formation: They are then reassembled into triglycerides and combined with other lipids and proteins to form chylomicrons.
6. Transport: Chylomicrons enter the lymphatic system and are transported to the bloodstream. Short-chain fatty acids go directly to the liver.
absorption
All food; 80% electrolytes; most water absorbed in small intestine
– Most sugars and amino acids absorbed coupled to active transport of Na+ (ie.
secondary active transport!!)
– This is the basis for “Gatorade” to improve absorption of both Na+ and glucose
– Absorption of fats is described above
– 9L water, most from GI tract secretions, enter small intestine
– 95% absorbed in the small intestine by osmosis
– Most of rest absorbed in large intestine
– Water uptake coupled with solute uptake
malabsorption of nutrients
Causes
– Anything that interferes with delivery of bile or pancreatic juice
– Damaged intestinal mucosa (e.g., bacterial infection; some antibiotics)
– Gluten-sensitive enteropathy (celiac disease)
– Immune reaction to gluten
– Gluten causes immune cell damage to intestinal villi and brush border
– Treated by eliminating gluten from diet (all grains but rice and corn)
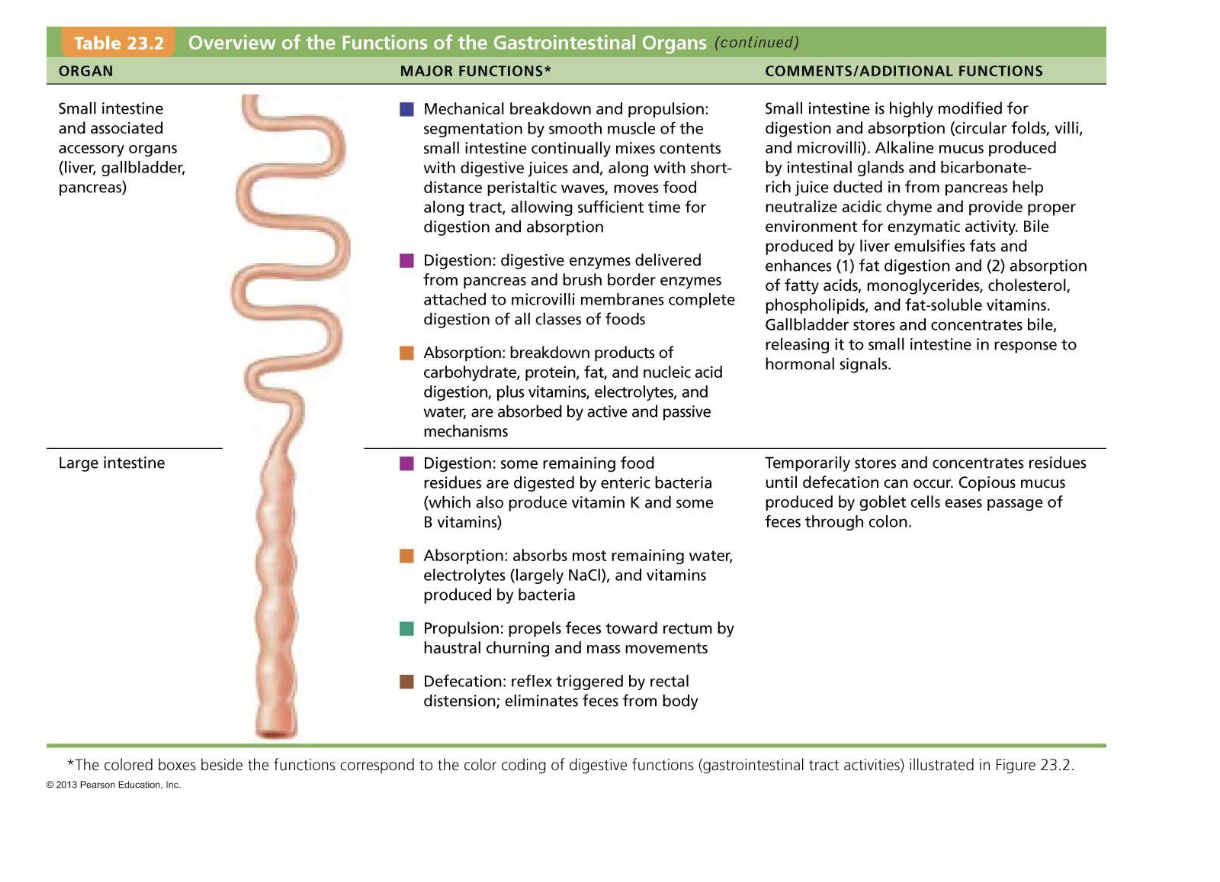
overview of the function of the gi organs
1. Small Intestine:
*mechanical
* Digestion: Breaks down food with enzymes from the pancreas and small intestine.
* Absorption: Absorbs nutrients like carbohydrates, proteins, fats, vitamins, electrolytes, and water.
2. Large Intestine:
* Digestion: Bacteria digest remaining food.
* Absorption: Absorbs water, electrolytes, and vitamins.
* Propulsion: Moves waste towards the rectum thru peristalsis.
* Defecation: Eliminates waste from body