pulmonary physiology
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
Obstructive lung disease
Obstructive -
-something is obstructing the airflow,
- characterized by high airway resistance
must be taught to breathe slowly and quietly (called pursed lip breathing
asthma, emphsema
Restrictive lung disease
something is restricting chest expansion,
characterized by a low compliance
small tidal volume with high RR
stiff lungs
fibrosis, tuberculosis, ARDs, intersitial lung disease
compliance
the change in pressure needed to inflate the lungs to a certain volume
lungs that are more compliant….
are stretchier — it takes a low pressure to inflate them
stiff lungs cause…
restrictive lung disease
emphysema
old stretched out sweater with holes
how does empysema increase compliance and airway resistance?
emphysema destroys the lung matrix, the
airways are very collapsable.
• Especially with forced expiration... the airways flatten out
such that air is hard to get through.
Vital capacity
-total amount of air that can be moved in and out of the lungs
~2.5-4.5 liters
-reduced with any kind of pulmonary disease
-size of vital capacity is indication of person’s pulmonary health
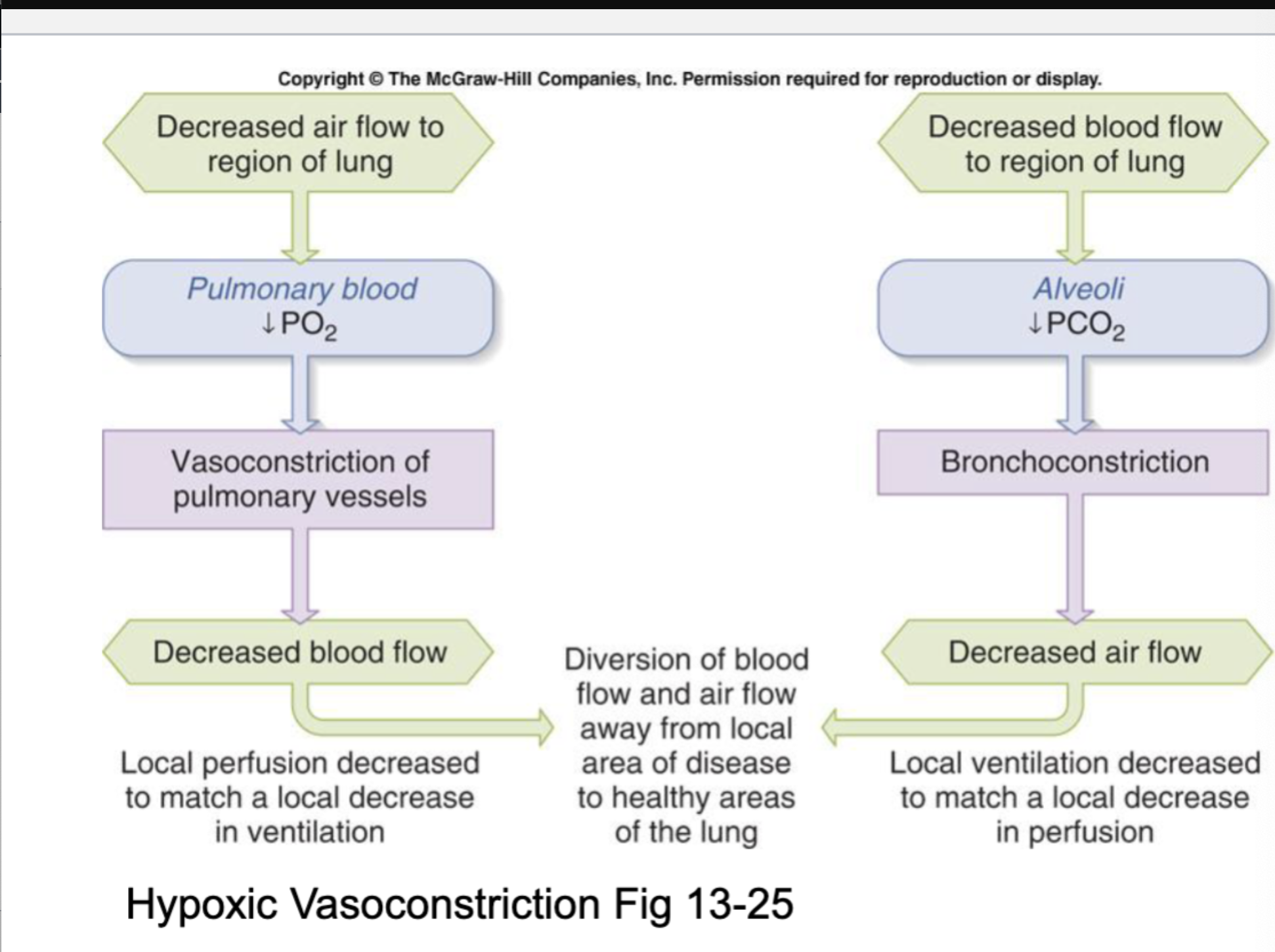
if ventialtion goes down…
↓ PO₂ |
Pulmonary vasoconstriction |
If perfusion goes down///
↓ PCO₂ | Bronchoconstriction |
diffrence between hypoxic vasoconstriction and bronchoconstriction
Hypoxic vasoconstriction shunts blood away from poorly ventilated alveoli, while low CO₂ causes bronchoconstriction to shunt air away from poorly perfused regions—together preserving V/Q matching.
hypoxic vasoconstriction
low oxygen in the airways causes the blood vessels going to that part of the lung to constrict
commonalities between restricitve land obstructive lung disease
Both would have a reduced vital capacity
– R – difficulty expanding to get air in
– O – difficulty recoiling to get the air out
• Both would have a reduced flow rate
– See explanations above
• Both would have an increased work of breathing (WOB)
hypoxic vasoconstriction
Partial pressure (P) is:
The pressure exerted by one specific gas in a mixture of gases
determines direction of diffusion
Partial pressure values in pulmonary vs systemic circulation
Pulmonary circulation (lungs)
Alveolar PO₂ (PAO₂) ≈ 100 mmHg
Pulmonary venous PO₂ (PvO₂) ≈ 40 mmHg
➡ Large gradient (~60 mmHg) drives O₂ into blood
Systemic circulation (tissues)
Arterial PO₂ (PaO₂) ≈ 100 mmHg
Mitochondrial PO₂ ≈ 3 mmHg
➡ Huge gradient drives O₂ from blood → tissues
What are the gradients that permit O2 to diffuse into the blood from the alveoli?
• PAO2 = 100mmHg > PvO2=40 mmHg
What are the gradients that permit O2 to diffusion from the blood to the tissues?
• PaO2 = 100mmHg > Pmito 3mmHg
as blood flows past the alveoli….
O2 rapidly diffuses into blood
Where does blood become fully saturated?
Blood becomes fully saturated within the first 1/3 of the capillary
Remaining 2/3 = diffusion reserve
Oxygen is carried in blood in two forms:
Dissolved O₂ (very small amount)
Bound to hemoglobin (most important)
Why hemoglobin matters:
One Hb molecule binds 4 O₂ molecules
Binding removes dissolved O₂ → maintains diffusion gradient
Allows massive increase in total O₂ carried
📌 Without hemoglobin:
Blood could not carry enough oxygen to meet metabolic demands
Saturation
Percentage of hemoglobin binding sites occupied
Depends only on PO₂
Independent of hemoglobin concentration
Oxygen content
Amount of O₂ in blood (mL O₂ / 100 mL blood)
Depends on:
PO₂
Hemoglobin concentration
sum of bound oxygen and dissolved oxygen.
Mary has 12 gm% of hemoglobin and Frank has 13gm%
• At a pO2 of 100 mmHg of mercury – who is more saturated? - who has a higher content? Who has higher dissolved content? Bound content?
At a pO2 of 100 mmHg
Answer: Mary and Frank are equally saturated, Frank has a higher total content, they have equal dissolved content, and Frank has higher bound content.
Bohr effect
describes how changes in the blood's environment affect hemoglobin's ability to bind and release oxygen.
Right shift of Bohr effect
-promotes oxygen release (right-release)
-Occurs with high temperature,
CO2, and H+(low pH).
-This is beneficial in metabolizing tissues where these conditions are present, allowing oxygen to be released to the cells.
-Result: Hemoglobin releases O₂ more easily to tissues
Left shift of Bohr effect
-promotes oxygen binding (left-bind)
-Occurs with low temperature,
CO2, and H+(high pH).
-This is beneficial in the lungs where these conditions help hemoglobin bind oxygen more readily
CO₂ is transported in three forms:
Dissolved in plasma (small amount)
Bound to hemoglobin (carbaminohemoglobin)
Converted to bicarbonate (MOST IMPORTANT)
Increased CO₂ → increased H⁺ → ↓ pH
location of chemoreceptors
Central chemoreceptors Location:
Medulla
In contact with cerebrospinal fluid (CSF)
Peripheral chemoreceptors Location:
Carotid bodies (at carotid bifurcation)
Aortic bodies (aortic arch)
function of central chemoreceptors
-sense: H⁺ in CSF, Indirectly sense arterial PCO₂
-Function: Major driver of ventilation at rest, Very sensitive to small changes in CO₂
—> Chemoreceptors regulate breathing by sensing chemical changes in blood and CSF.
function of peripheral chemoreceptors
What they sense:
↓ PO₂
↑ PCO₂
↑ H⁺ (metabolic acidosis)
Function:
Rapid response to blood chemistry
Essential during:
Hypoxemia
Metabolic acidosis
Exercise
all chemoreceptors regulate arterial blood gases, not alveolar gas
true
why CO2 is the most important regulator for ventilation:
Why CO₂ matters most:
Small increases in arterial PCO₂ → large increases in ventilation
Acts on both central and peripheral chemoreceptors
A competitive bicyclist takes erythropoietin and experiences an increase in red blood cell count. As a result, this bicyclist would experience which of the following changes?
B. is correct because more hemoglobin means that there will be more bound content.
how does CO2 control ventilation?
Mechanism:
↑ Arterial PCO₂
CO₂ diffuses into:
Blood → ↑ H⁺
CSF → ↑ H⁺
H⁺ stimulates chemoreceptors
Ventilation increases
CO₂ is blown off
📌 PCO₂ is the primary stimulus for breathing at rest
📌 Major contributor to dyspnea (shortness of breath)
O₂ — only important at LOW levels for controlling ventilation
Above 60 mmHg:
Changes in PO₂ have little effect on ventilation
Below 60 mmHg:
Peripheral chemoreceptors strongly stimulate ventilation
how does H⁺ act as metabolic control?
Effect:
Acidosis → ↑ ventilation
Purpose: remove CO₂ to help buffer pH
Detected by:
Peripheral chemoreceptors ONLY
Source of H⁺:
Metabolic acids (lactic acid, ketoacids)
Independent of CO₂
lung tissue matrix
a weave of collagen and elastic fibers
stiff lungs
less stretchy, slow to inflate, small wheezing strengths
-cause restrictive lung disease
empysema
-destroys the lung tissue matrix
-lungs are very compliant
-makes lungs easy to stretch but difficult to recoil
Transpulmonary pressure
alveolar pressure minus the intrapleural pressure
how does alveolar pressure usually relate to intrapleural pressure ?
In physiology, intrapleural pressure (Pip) is always more negative (lower) than alveolar pressure (Palv), creating a pressure gradient (transpulmonary pressure) that keeps the lungs inflated and prevents collapse, even though both pressures change during breathing
what happens to intrapleural pressure during inspiration
During inspiration, Pip becomes even more negative as lungs stretch, causing Palv to drop below atmospheric pressure to draw air in
what happens to intrapleural pressure during expiration
during expiration, Pip becomes less negative (more positive), and Palv rises above atmospheric pressure to push air out, always maintaining Palv > Pip
when is the lowest transpulonary pressure measured
The lowest transpulmonary pressure (PL) is typically measured at the end of expiration (E-E PL), representing the pressure keeping the lungs open (avoiding collapse, or atelectasis), while the highest is at end-inspiration (E-I PL) to prevent overdistension
surface tension
-allows particles to stick together
-high surface tension in lungs makes alveoli more likely to collapse
how does CO2 affect central chemoreceptors
-cross blood brain barrier and reacts with water
-form carbonic acid
-disassociate into H+ and bicarbonate
-increased H+ in CSF stimulates brains respoiratory center
-inc ventilation
build up of CO2 causes…
build up of acid (low pH)
why mgiht a person hypoventilate
-head injury, drug overdose
-a person can stimulate this by holding their breath
why is it important for the membrane to be thing?
it will take less time for O2 to diffuse in and Co2 to diffuse out
dissolved oxygen
-only depends on PO2
-small amount
-responsible for: partial pressure (PaO2) and diffusion gradients
hemoglobin bound oxygen
-depends on hemoglobin concentration and hemoglobin saturation
-makes up 98% of total oxygen concentation
-total oxygen concentration = dissolved O2 and hemoglobin bound O2
total oxygen concentration =
dissolved O2 and hemoglobin bound O2
lowering PCO2 leads to
makes the blood more alkaline (increases pH)
Respiratory alkalosis
increased oxygen-hemoglobin binding
*a lowered partial pressure of carbon dioxide (PCO2) in the blood causes breathing to slow down (hypoventilation) and become shallower
relationship between hemoglobin and oxygen content
increasing hemoglobin directly increases the blood's oxygen carrying capability —> more oxygen can be transported from lungs to tissues
role of hemoglobin
preimary protein responsible for binding and delivering oxygen
-more hemoglobin =means more binding sites for oxygen —> boosting total oxygen content
important in high altitudes or smoking when the body needs more oxygen
increasing PCO2 :
-makes blood more acidic
-triggers brain to increase breathing
-causes blood vessels to dilate
Chemoreceptors detect high PCO2….
…. and go to signal the brainstem to increase ventilation (breathing faster and deeper) to blow off excess CO2.
Respiratory Acidosis:
too much CO2 in the blood leads to the CO2 combines with water to form carbonic acid, increasing hydrogen ions (𝐻+) and lowering pH (making blood acidic).
what does arterial PCO2 tell us?
arterial partial pressure of Carbon dioxide reflects ventilation and how well you brathe out CO2 and its impact on blood pH
*PCO2 is a primary driver of respiratory control, influencing acid-base balance by forming carbonic acid
what does arterial PO2 tell us?
partial pressure of oxygen reflects oxygenation (how well oxygen gets into the blood)
*PO2 indicates lung efficiency in oxygen transfer, with both critical for assessing overall respiratory and metabolic health
Tidal volume (TV) ~500mL
TV: air moves in or out during normal, quiet breathing
TV + IRV = IC
Total Lung capacity (TLC) ~6000 mL
TLC= entire volume of air lungs can hold
*IRV + ERV+ TV+ RV
Inspiratory capacity (IC) ~3500 mL
IC= max amount you can inhale after a normal exhale
TV + IRV = IC
4 lung volumes
Tidal volume, inspiratory reserve volume, expiratory reserve volume, residual volume
Inspiratory Reserve Volume (IRV) ~3000mL
IRV = extra air you can inhale after a normal inhalation
*IRV + TV = IRC
Expiratory Reserve volume (ERV) ~1200mL
ERV = extra air you can exhale after a normal exhalation
*ERV + RV = Functional Residual capacity
Residual volume (RV) ~1200mL
RV= air remaining in your lungs after maximal exhalation
!CANNOT be exhaled!
Which values can a spirometer not measure?
residual volume (RV), and therefore FRC + TLC becasue they contain RV
Vital Capacity (VC) ~4700mL
VC= total amount of air you can move in and out - max inhale and max exhale
*IRV + TV + ERV
!vital capacity: you would use all of the air possible if it was vital!
Functional Residual Capacity (FRC) ~ 2400ml
FRC= air left after normal exhalation (lung’s resting volume
*FRC= ERV + RV
4 lung capacities and equations
Inspiratory capacity(IC) = TV
= IRV
Vital Capacity (VC) = IRV + TV + ERV
Functional Residual Capacity(FRC) = ERV + RV
Total Lung Capacity(TLC) = TV + IRV + ERV + RV
MINUTE VENTILATION
respiratory rate(RR) x tidal volume (TV)
asthma
bronchoconstriction —> airway narrowing —> increased resistance
fibrosis
stiff lungs —> hard to expand —> low compliance
what does alveolar ventilation measure?
measures the fresh air reaching the gas exchange areas (alveoli) per minute
alveolar ventilation equation
𝑉𝐴=(𝑇𝑖𝑑𝑎𝑙𝑉𝑜𝑙𝑢𝑚𝑒(𝑉𝑇)−𝐷𝑒𝑎𝑑𝑆𝑝𝑎𝑐𝑒(𝑉𝐷))
×𝑅𝑒𝑠𝑝𝑖𝑟𝑎𝑡𝑜𝑟𝑦𝑅𝑎𝑡𝑒(𝑓)
NORMAL PARTIAL PRESSURES:
Arterial : PaO2 =~ 100mmHg, PaCO2 = ~40mmHg
Venous: PvO2= ~40 mmHg, PvCO2 = ~46mmHg