Cardiac NREMT PREP with 100% correct answers already graded A+(verified for accuracy)
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
Identify major structures of the heart
Superior and inferior vena cava
Right atrium
Right ventricle
Pulmonary Valve
Right/left pulmonary artery
Septum
Right/left pulmonary veins
Left atrium
Mitral valve
Left ventricle
Aorta
Describe Cardiovascular blood flow
(Describe the path blood takes through the heart/lungs/body)
1) Deoxygenated blood from the body enters heart through the superior and inferior vena cava
2) Moves to right atrium
3) Fills right ventricle then ventricle contracts
4) Blood then moves through pulmonary valve
5) Moves through right/left pulmonary artery
6) Moves to lungs ( the pulmonary circulation in lungs oxygenate blood)
7) Oxygen rich blood returns to heart through pulmonary veins
8) Enters left atrium
9) Passes into left ventricle
10) Pumps into the aorta then the rest of the body
Describe electrical activity in the heart
(Describe the path electricity takes through the heart)
1) An electrical impulse is generated by the SA node
2) Impulse travels across both atria, causing them to contract
3) Impulse travels through the AV node
4) Impulse continues down the conduction pathway via the bundle of His and Purkinje fibers
5) spreads throughout both ventricles and causes them to contract
Acute Coronary Syndrome
A group of symptoms caused by myocardial ischemia; includes angina and myocardial infarction
Angina
Transient chest discomfort caused by partial or temporary blockage of blood flow to the heart muscle; also called angina pectoris.
Myocardial Infarction (MI)
A heart attack; death of heart muscle following obstruction of blood flow to it.
Congestive Heart Failure (CHF)
The failure of the heart to pump efficiently, leading to excessive blood or fluids in the lungs, the body, or both
Aortic Dissection
When blood enters a tear in the inner lining of the aorta and separates the layers of the aortic wall
Renal failure
Loss of the kidneys' ability to filter the blood and remove toxins & excess fluid from the body
End stage renal disease (ESRD)
Irreversible renal failure to the extent that the kidneys can no longer provide adequate filtration & fluid balance to sustain life; survival w/ ESRD usually requires dialysis
Pulmonary edema
Excess fluid in the lungs.
Eclampsia
Seizures resulting from severe hypertension in a pregnant woman.
Preeclampsia/pregnancy-induced hypertension
A condition of late pregnancy that involves headache, visual changes, and swelling of the hands and feet.
Nitroglycerin
A vasodilator. Dilates coronary arteries and veins, improves blood flow. Decreases oxygen demand of the heart.
Nitroglycerin indications
Treatment of angina pain and acute myocardial infarction, must be patient's prescribed dosage and as approved by medical direction.
Nitroglycerin Contraindications
Cerebral hemorrhage, sexual enhancement drugs, hypotension-systolic blood pressure < 100.
Nitroglycerin side effects
Headache, flushing, dizziness, hypotension, and tachycardia.
Aspirin (ASA)
Blood thinner (antiplatelet). Decreases platelet aggregation, decreases clotting.
Aspirin (ASA) Indications
MI and angina as approved by medical direction.
Aspirin (ASA) Contraindications and Precautions
Contraindications: GI bleed, allergy.
Precautions: Anemia, Hodgkin's lymphoma, gastritis
Aspirin (ASA) Side effects
Seizures, coma, GI bleeding, hepatitis and anaphylaxis.
Normal Sinus Rhythm (NSR)
60-100 bpm
all complexes normal and evenly spaced (P, QRS, T)

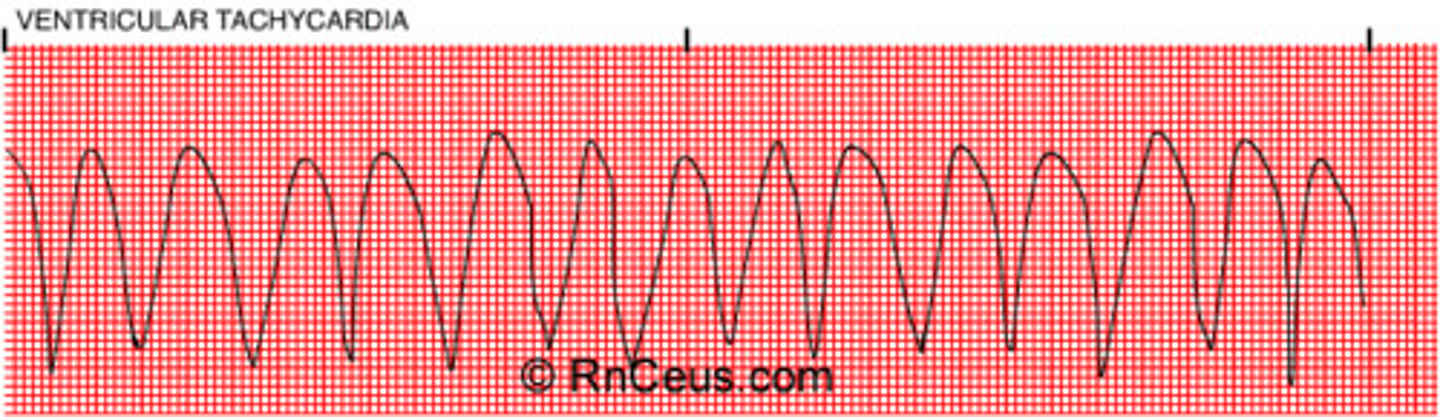
Ventricular tachycardia
A fast heart rhythm, that originates in one of the ventricles of the heart. The ventricles are the main pumping chambers of the heart.
- ventricle irritated and moving fast
- rapid, bizarre, wide QRS complexes
- 1 large QRS after another!
(in vtach pt may not have pulse)
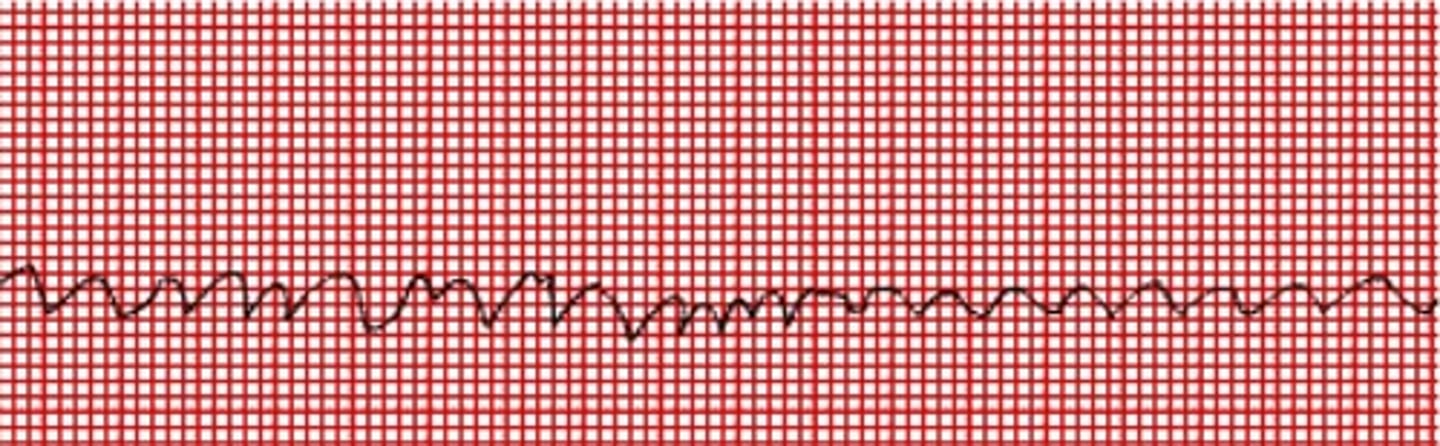
Ventricular Fibrillation
Occurs when the "Heart beats with rapid, erratic electrical impulses." This disordered electrical activity is considered to be the most dangerous of all cardiac arrhythmias because it affects the powerful pumping chambers of the heart - the ventricles. In V-fib, the ventricles ineffectively quiver or flutter and the heart pumps little or no blood which can lead to cardiac arrest.
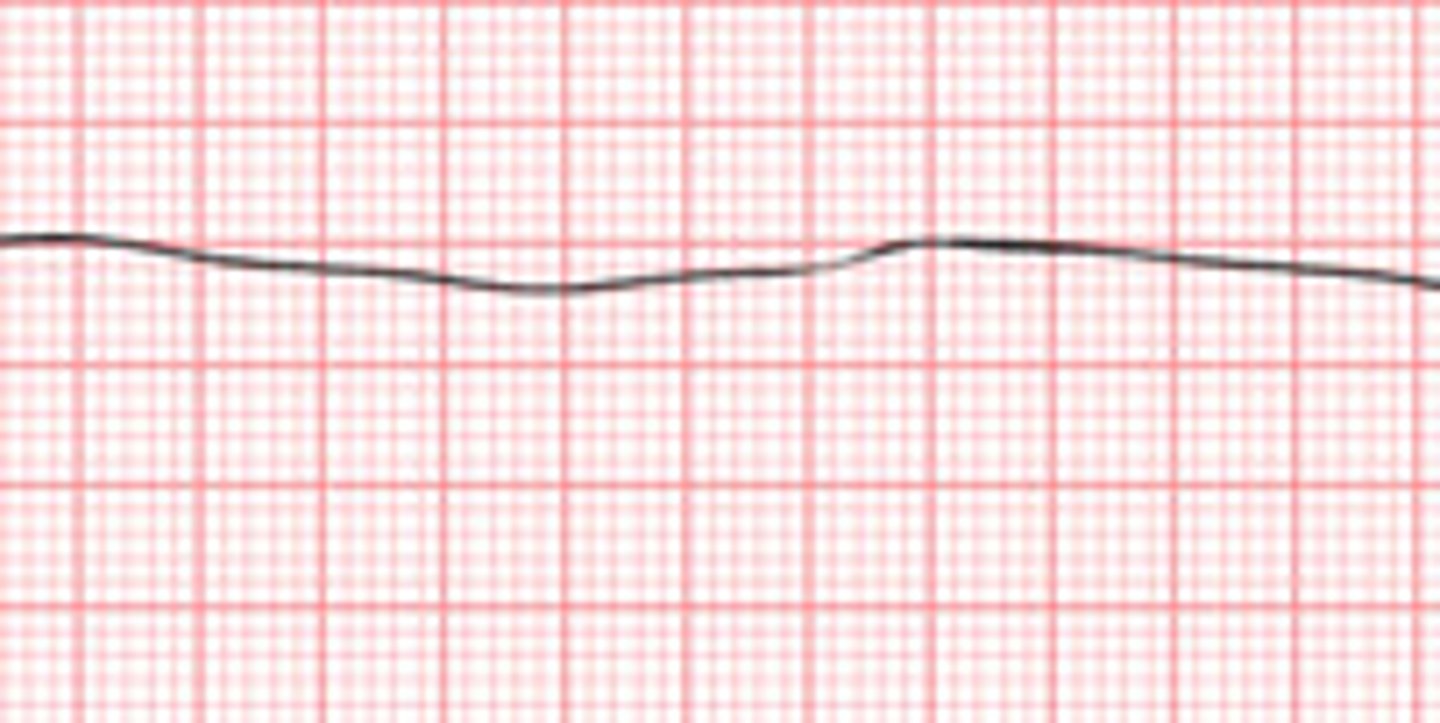
Asystole
- dead (flat-line)
- no electrical activity, only straight line (no rate/pulse)
A dire form of cardiac arrest in which the heart stops beating, there is no systole and there is no electrical activity in the heart. The heart is at a total standstill.
Atrial Fibrillation
Cardiac arrhythmias caused by abnormal impulse formation or conduction
Lacking P-wave
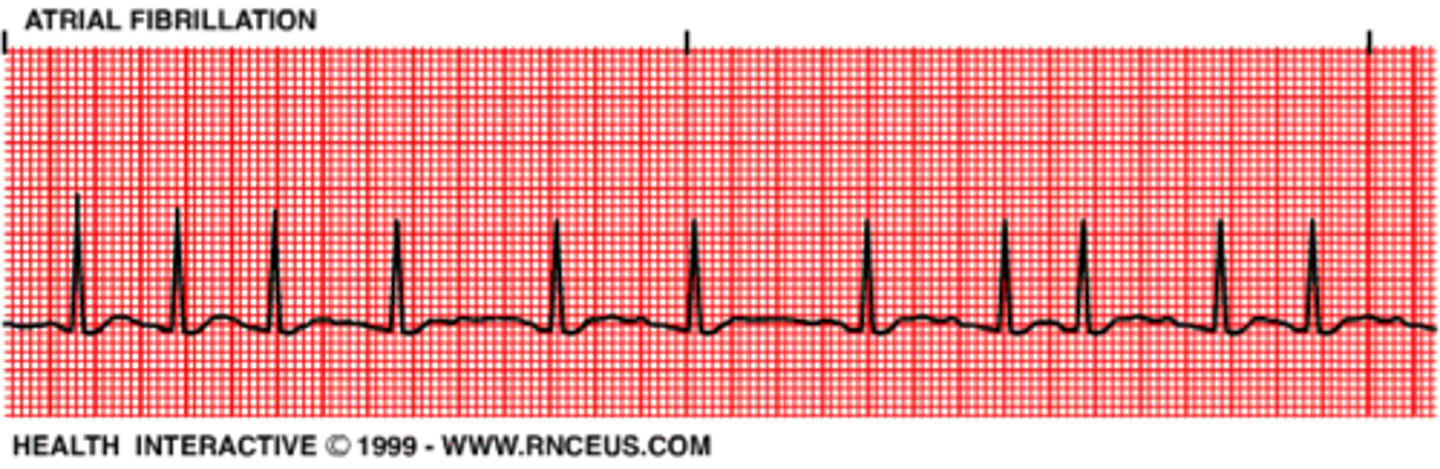
Symptoms of atrial fibrillation
Loss of atrial squeeze
decreased filling time
palpitations, SOB, weakness
Tachycardia
An abnormally rapid heart rate
Bradycardia
An abnormally slow heart rate
Chain of Survival (CPR)
-Recognition of cardiac arrest and activation of the emergency response system
-Early cardiopulmonary resuscitation (CPR) with an emphasis on chest compressions
-Rapid defibrillation
-Basic and advanced emergency medical services
-Advanced life support and post-cardiac arrest care
Where should you place your hands when giving chest compressions during infant CPR?
One hand on the forehead and two or three fingers on the center of the chest
When giving CPR to an infant, about how deep should you compress the chest?
At least one third diameter of chest
About 1½ inches
When giving CPR to a child, about how deep should you compress the chest?
At least one third diameter of chest
About 2 inches
When giving CPR to an adult, about how deep should you compress the chest?
At least 2 inches
The cycle of compressions and breaths in CPR for an infant/pediatric is:
30:2 (Single rescuer)
15:2 (Multi-rescuer)
The cycle of compressions and breaths in CPR for an adult is:
30:2
In pediatric CPR, what is the age range for a child?
Between 1 year and the onset of puberty
When alone, how long should you perform CPR before activating EMS?
2 minutes
The compression and breaths in CPR for a neonate is:
3:1
(rescuers may consider using higher ratios, 15:2, if the arrest is believed to be of cardiac origin)
If CPR is successful and resuscitation is achieved, what care is needed?
Place PT in recovery position:
-With the PT lying on their back, kneel on the floor at their side
-Place the arm nearest you at a right angle to their body with their hand upwards, towards the head
-Tuck their other hand under the side of their head, so that the back of their hand is touching their cheek
-Bend the knee farthest from you to a right angle
-Carefully roll the PT onto their side by pulling on the bent knee
-The top arm should be supporting the head and the bottom arm will stop you rolling them too far
-Open their airway by gently tilting their head back and lifting their chin, and check that nothing is blocking their airway
-Stay with the PT and monitor their condition until help arrives, or if with ambulance transport.
AED use (Steps)
1) place proper pads in correct location on patients bare chest and turn unit on. If two people, rescuer 1 continues compressions during pad placement.
2) clear victim during rhythm analysis
3) if shock advised, clear victim and shock
4) immediately resume compressions after each shock delivery, minimize interruptions in chest compressions before and after shock delivery
What is a stroke?
Inadequate amount of blood being delivered to a portion of the brain caused by a blood clot obstructing a blood vessel in the brain or loss of continuity of the blood vessels.
Types of strokes
Ischemic stroke (Blockage)
Hemorrhagic stroke (Bleeding)
TIA
Ischemic stroke
Occurs when a cerebral artery is blocked by a clot or other foreign matter.
Types of Ischemic strokes
Thrombotic and embolic
Thrombotic stroke
An ischemic stroke resulting from thrombus formation
Embolic stroke
Ischemic stroke resulting from a cerebral embolism.
Hemorrhagic stroke
Results from the rupture of an artery that causes bleeding within the brain or in the space around the outer surface of the brain.
What is TIA?
Transient Ischemic Attacks: Intermittent stroke-like episodes
Primary difference between ischemic and hemorrhagic stroke treatment
-Pt suffering from an ischemic stroke can receive a fibrinolytic drug to break up the clot and restore perfusion to the area of the brain that was not receiving an adequate supply of blood.
-A hemorrhagic stroke PT cannot receive a fibrinolytic drug because it may increase the amount of bleeding within the brain, worsen the stroke, and possibly lead to pt death.
Common sudden onset s/s of a hemorrhagic stroke
Droop in face
Intense headache
Confusion
Nausea or throwing up
Sensitivity to light
Problems with vision
Passing out
Common sudden onset s/s of a ischemic stroke
Droop in face
Sudden numbness or weakness of your face, arm, or leg, often on one side of the body
Confusion
Problems speaking or understanding others
Dizziness, loss of balance or coordination, or trouble walking
Vision loss or double vision
Systolic
The top number in blood pressure. Refers to the amount of pressure in your arteries during the contraction of your heart muscle.
Diastolic
The bottom number in blood pressure. Indicates the pressure in the arteries when the heart rests between beats.
Neonate (0 to 1 m/o)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature:
Pulse Rate: 100 to 180 beats/min
Respiratory Rate: 30 to 60 breaths/min
Systolic Blood Pressure: 50 to 70 mm Hg
Body Temperature: 98 to 100 degrees F
Infant (1 m/o-1 y/o)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature:
Pulse Rate: 100 to 160 beats/min
Respiratory Rate: 25 to 50 breaths/min
Systolic Blood Pressure: 70 to 95 mm Hg
Body Temperature: 96.8 to 99.6 degrees F
Toddler (1 y/o - 3 y/o)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature:
Pulse Rate: 90 to 150 beats/min
Respiratory Rate: 20 to 30 breaths/min
Systolic Blood Pressure: 80 to 100 mm Hg
Body Temperature: 96.8 to 99.6 degrees F
Preschool Age (3 y/o -6 y/o)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature:
Pulse Rate: 80 to 140 beats/min
Respiratory Rate: 20 to 25 breaths/min
Systolic Blood Pressure: 80 to 100 mm Hg
Body Temperature: 98.6 degrees F
School Age (6 to 12 yrs)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature:
Pulse Rate: 70 to 120 beats/min
Respiratory Rate: 15 to 20 breaths/min
Systolic Blood Pressure: 80 to 110 mm Hg
Body Temperature: 98.6 degrees F
Adolescents (12 to 18 yrs)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature
Pulse Rate: 60 to 100 beats/min
Respiratory Rate: 12 to 20 breaths/min
Systolic Blood Pressure: 90 to 110 mm Hg
Body Temperature: 98.6 degrees F
Early Adult (19 to 40 yrs)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature:
Pulse Rate: 60 to 100 beats/min
Respiratory Rate: 12 to 20 breaths/min
Systolic Blood Pressure: 90 to 140 mm Hg
Body Temperature: 98.6 degrees F
Middle Adult (41 to 60 yrs)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature:
Pulse Rate: 60 to 100 beats/min
Respiratory Rate: 12 to 20 breaths/min
Systolic Blood Pressure: 90 to 140 mm Hg
Body Temperature: 98.6 degrees F
Late Adult (61 yrs & older)
Pulse Rate:
Respiratory Rate:
Systolic Blood Pressure:
Body Temperature
Pulse Rate: Depends on health
Respiratory Rate: Depends on health
Systolic Blood Pressure: Depends on health
Body Temperature: 98.6 degrees F
Normal Diastolic Blood Pressure (all ages)
On average 60 - 85. For younger PT it may be 2/3 of systolic
Orthostatic vital signs. (postural)
You take the patients vital signs while lying flat and then you take the vital signs again when the patient is standing.
S/S of hypertensive emergencies
-Pulse that is strong bounding
-Tinnitus (ringing ears)
-headache
-nosebleed
-nausea/vomiting
What are hypertensive emergencies?
Systolic pressure greater than 160 mm Hg
What are hypotensive emergencies?
severe drop in blood pressure
S/S of hypotensive emergencies
Cool, pail, diaphoretic skin
Light headed
Dizziness
Nausea/vomiting