Cardiovascular Drugs #4: Anti-Arrhythmics
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
Why does the heart contract?
Specialized cells in the Sinoatrial (SA) node in the RA and the Atrioventricular (AV) node generate spontaneous action potentials that result in the stimulation and contraction of cardiac muscle cells
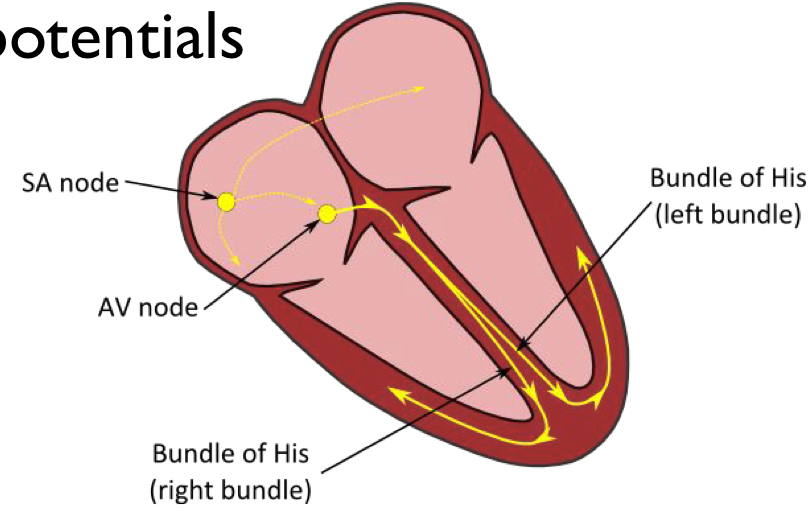
Which node generates impulses faster? Why is this important?
The SA node generates impulses faster than the AV node
This is important because the atria need to contract before the ventricles, which allows for that to happen
The SA node has an inherent rate that is modified by sympathetic (__) and parasympathetic (__). What effect do each of these receptors have on the rate of the SA node?
Sympathetic (Beta-1)
β1 activation stimulates Na+ and Ca++ influx enhancing signal generation and increasing the rate of depolarization and impulse generation
Sympathetic = Faster HR
Parasympathetic (M2 (Muscarinic))
M2 stimulation increases the K + efflux and decreases the Na+ influx which decreases the rate of signal generation.
Parasympathetic = Slower HR
When the signal travels from the atrium to the ventricle, it passes through the AV node, what is something important that happens here that facilitates the proper function of the heart?
It pauses briefly (fraction of a second), this allows for the atria to contract and fill the ventricle before the ventricle contracts
What are Arrhythmias?
Disruptions of the normal HR or Rhythm
What causes Arrhythmias?
Abnormal impulse formation, conduction, or both
Describe the difference between Bradycardia and Tachycardia, how is C.O affected during each of these scenarios?
Tachycardia
HR is increased
The C.O is decreased because there is less time for the ventricle to fill between the beats
Bradycardia
HR is slowed/blocked
Decreased C.O due to a decreased number of BPM
Why are anti-arrhythmic drugs only used seriously?
They can cause arrhythmias and potentially may increase the chance of death
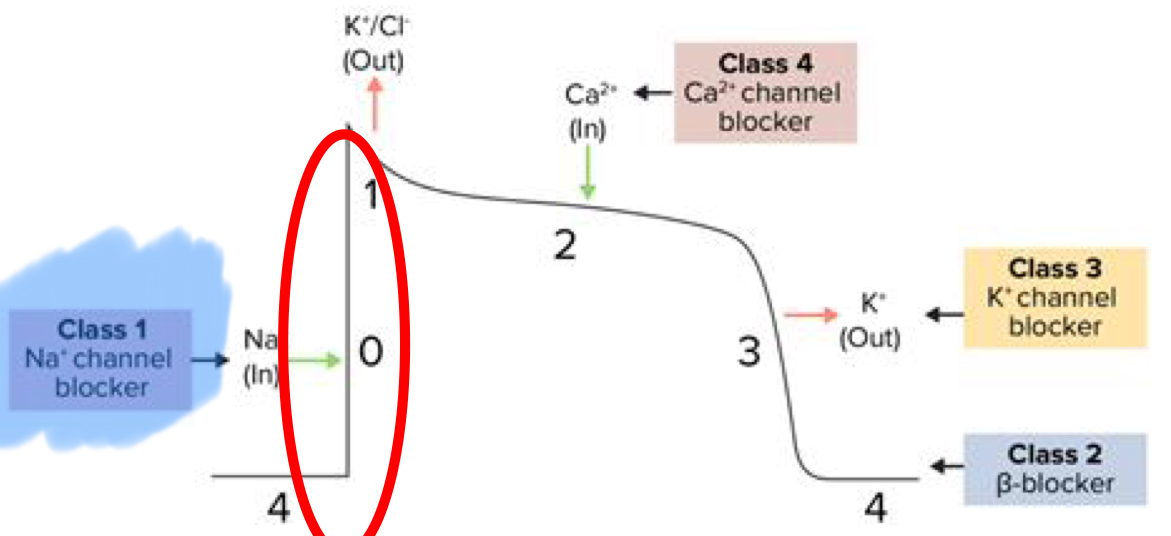
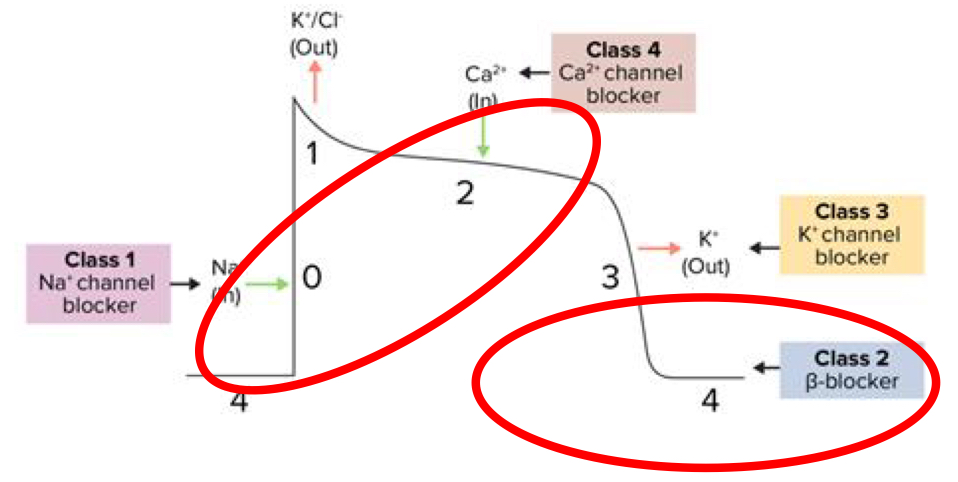
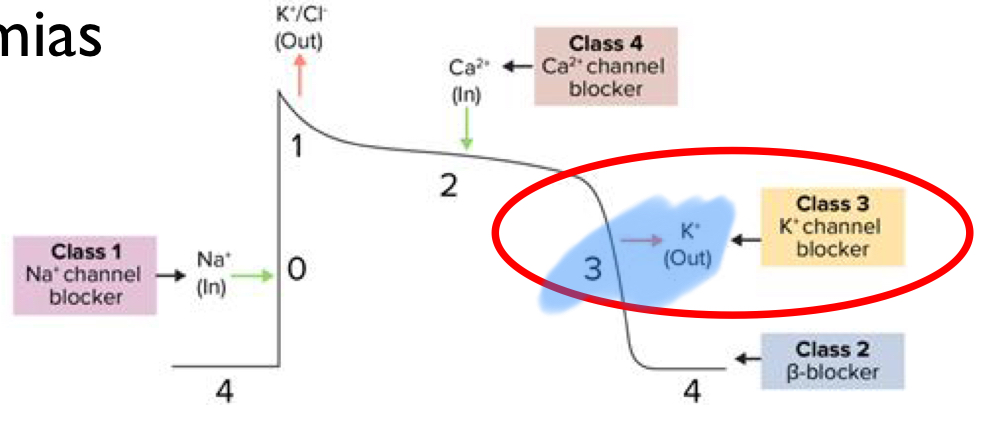
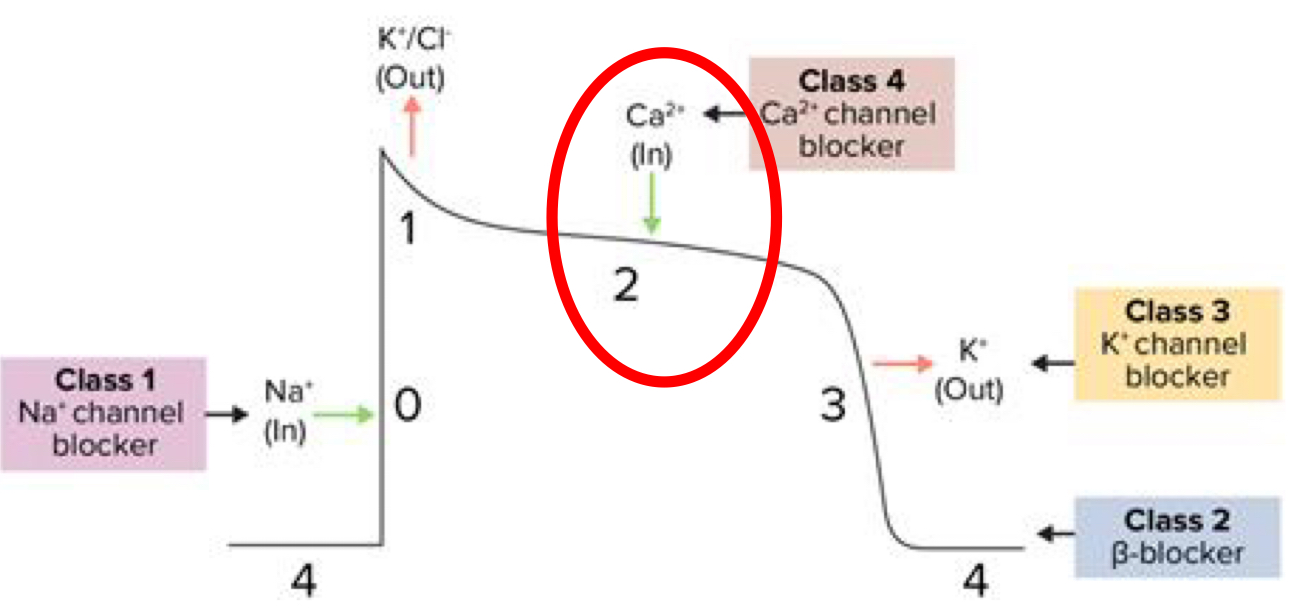
What are the 4 classes of Anti-Arrhythmic drugs?
Class I: Na channel blockers
Class 2: Beta-blockers
Class 3: K channel blockers
Class 4: Ca channel blockers
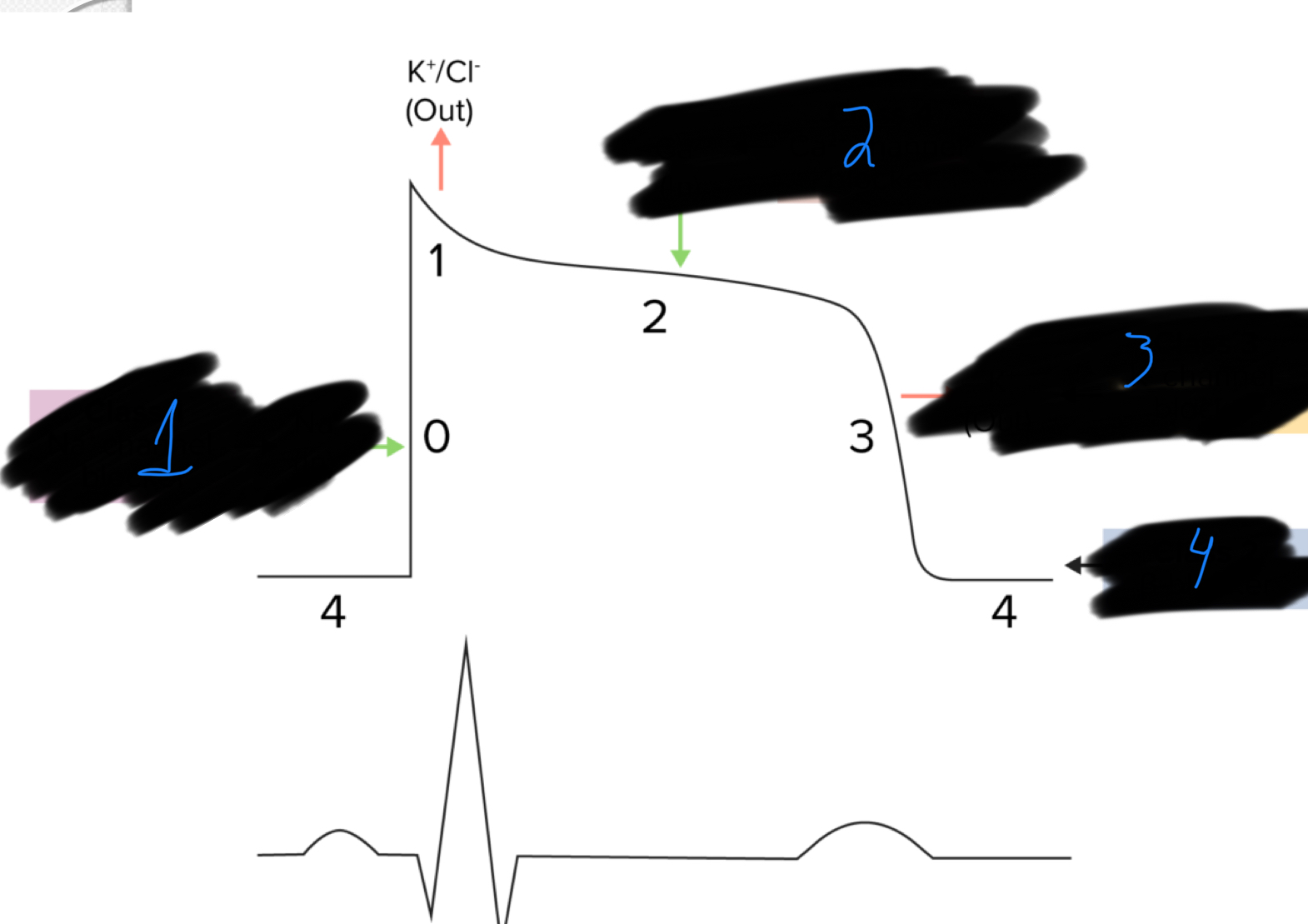
Which class of anti-arrhythmic drug acts at each point of the graph?
Class 1: Na Channel Blockers
Class 4: Ca2+ channel blockers
Class 3: Potassium channel blockers
Class 4: Beta blockers
Class 1 chemicals are similar to _____ _______
Local Anesthetics
How do class 1 anti-arrhythmics work?
They are Na+ channel blockers
They decrease rapid Na influx → slows rate of depolarization in phase 0
Class 1 Anti-Arrhythmics have how many subclasses? What are they?
3
1a
1b
1c
A major benefit of Class 1 Anti-Arrhythmics is that they only target what?
Block excitable cells discharging at abnormally high rates in the heart
What does “Use-Dependence“ mean in terms of Class I Anti-Arrhythmics?
Anti-Arrhythmics that bind more strongly to sodium channels at faster heart rates (They bind to open Na channels not resting ones)
What specific type of Arrhythmias are Class 1 Anti-Arrhythmics used to treat?
Ventricular Arrhythmias
Supraventricular Arrhythmias
How does Class 1 Anti-Arrhythmics affect the heart (what effect does their decreasing the influx of Na have)?
Decreases HR
Decreases conduction velocity through the atria, ventricles, and HIS purkinje fibers
What is the best drug for ventricular Arrhythmias?
Lidocaine (1B)
T/F: Lidocaine is effective in treating atrial arrhythmias
False, it is a class 1 Anti-Arrhythmic, it is effective on the ventricles
_______ is commonly used to revert ventricular arrhythmias that develop during surgery or anesthetisia
Lidocaine (In a normal heart rate, it dissociates before the next beat (safe), but in tachycardia, it stays bound to block the channel.)
What are the adverse effects associated with Lidocaine? What should be done if these signs show up?
Nausea, vomiting, skeletal muscle fasciculation, CNS (excitement, seizures)
Stop the CRI, Lidocaine has a very short half-life, by stopping administration you will end the adverse effects
What is known as the “Oral Lidocaine“? Why is it regarded this way?
Mexiletine (1B)
It works very similar to lidocaine and they are both Class 1 Anti-Arrhythmics
Unlike lidocaine, _______ can be used as a long-term oral treatment for ventricular arrhythmias
Mexiletine
Procainamide (1A) is in the same class as Lidocaine/Mexiletine but functions differently than them, what is its function/MOA?
Inhibits Na (primary), K, and Alpha-1 receptors
Vagolytic
a substance that blocks the action of the vagus nerve, which slows the heart rate
T/F: Procainamide is a good first option for treating ventricular arrhythmias
False, it is a backup to Lidocaine
How is Procainamide normally administered?
Oral (long-term)
Class II Anti-Arryhthmics are ____-Blockers
Beta-Blockers (Antagonists at Beta-1/Beta-2)
By what 3 mechanisms do Beta-Blockers (Class II) act as Anti-Arrhythmics?
Decrease Na and Ca influx
Depresses SA node
Slows AV conduction
Decreases the ventricular response to atria
Increases the refractory period in conducting tissues (4)
Beta Blockers (Class II) treat arrhythmias by decreasing ________ input
Sympathetic
What are the clinical uses of Beta-Blockers?
Arrhythmias caused by excess sympathetic stimulation
Decreasing the ventricular rate in supraventricular or ventricular arrhythmias
Decrease Tachycardia in hyperthyroid cats
Feline hypertrophic cardiomyopathy
T/F: Class I and Class II Anti-Arrhythmics cannot be combined for any reason
False, they can be combined if single drug therapy is ineffective
What are the adverse effects of Beta-Blockers?
Bradycardia
Decreased contractility and CO
Extracardiac effects
Beta-2 Bronchoconstriction
Which of these isn’t a Class II Beta Blocker?
Sotolol
What is Sotolol?
A class III Anti-Arrhythmic
Which Class II beta blocker does this describe?
Original Non-selective product
Short half-life (TID dosing)
Hepatic metabolism
Propanolol
Which Class II beta blocker does this describe?
Relatively Beta-1 selective
Excreted unchanged by the kidneys (good for liver patients)
Dosed q12-24h
Atenolol
Which Class II beta blocker does this describe?
Beta-1 specific
Liver metabolized
High first pass effect → High inter-patient variability
Can cause cardiovascular depression or and AV-block
Metoprolol
How do III Anti-Arrhythmics work?
They are K+ channel blockers
They function during phase 3
They inhibit K+ efflux (leaving)
What is the MOA of Class II Anti-Arrhythmics?
Inhibit K+ efflux → delays repolarization → prolongs the AP → delays conduction → Increase effective refractory period → decreases ectopic activity of ventricular arrhythmias
What does ectopic activity mean?
Ectopic activity refers to premature, extra heartbeats (ectopic beats)

What type of Anti-Arrhythmic is Amiodarone? Why is it known as a “dirty drug“?
Class III (K)
It also has Class I (Na), Class II (Beta), and Class IV (Ca) effects
What are the dangers of Amiodarone use?
Long half-life (3.2 days) + serious Adverse effects (hepatopathy, keratopathy, dermatopathy) make for a bad combination
What are the clinical indications of Amiodarone?
Refractory ventricular tachycardia (Amiodarone is the main treatment for)
a persistent, life-threatening rapid heart rhythm that resists standard treatments
Prevent recurrence of atrial fibrillation
Which of these is a Class III Anti-Arrhythmic?
Sotolol
What is the MOA of Sotolol?
It is a combination of
Class II (Beta-blocker)
Class III (K)
Answer the following about Sotolol
_____ blocker at low concentrations and _______ blocker at high concentrations
____ administration
____ bioavailability
_____ excretion
Short-term/Long-term?
Beta-1/2 blocker at low conditions and K channel blocker at high concentrations
Oral
High bioavailability
Renal Excretion
Can be used long-term
What are the clinical indications of Sotolol?
Longterm for refractory ventricular tachyarrhythmias (eg boxer)
Refractory atrial fibrillation
What are the adverse effects of Sotolol?
Bradycardia
Hypotension
Arrhythmias
GI irritation
Class IV Anti-Arrhythmics are _____ channel blockers
Calcium
What is the MOA of Class IV Anti-Arrhythmics?
Block slow Ca influx in cardiac myocytes and vascular smooth muscle
T/F: Class IV Anti-Arrhythmics are +ve Inotropes
False, they are -ve inotropes (they reduce the contractility of the heart)
What are the clinical indications of Class IV Anti-Arrhythmics?
Supraventricular tachycardia
Vasodilation
Class IV Anti-Arrhythmics should be avoided in patients that have what condition? Why?
CHF
Because Class IV Anti-Arrhythmics reduce contractility (-ve inotrope)
Decreasing the influx of Ca into the cell by Class IV Anti-Arrhythmics has what effect on the heart?
Slows SA firing
Slows AV conduction
Causes peripheral vasodilation
You should avoid using Class IV Anti-Arrhythmics with __________ in order to avoid causing bradycardia
Beta-Blockers
Diltiazem and Verapamil are both class __ Anti-Arrhytmics
IV
What is the major differences between Diltiazem and Verapamil?
Both are Class IV (Ca) Anti-Arrhythmics
Diltiazem
More Popular, less myocardial depression
Indications
Used for canine A-fib and feline HCM
Verapamil
More potent -ve inotrope, -ve chronotrope (agents that decrease heart rate by affecting the electrical conduction system (specifically the SA node)), and vasodilator.
Higher risk of hypotension, cardiac depression, and bradycardia
Not a first choice
What type of Anti-Arrhythmic drug is Digoxin?
Mechanism: Increases parasympathetic (vagal) tone to the heart.
Use: Atrial arrhythmias (slows AV conduction).
What type of Anti-Arrhythmic drug is Isoproterenol?
Mechanism: Non-specific beta-agonist (sympathomimetic).
Use: Medical treatment for AV block or bradycardia that doesn't respond to atropine.
ADR: Hypotension (Beta-2)
Anticholinergic drugs antagonize _____ receptors, what effect does this have on the heart? What is this conditional on?
Muscarinic
Effects of Anticholinergic drugs of heart
Inc sinus rate and AV conduction
ANTICHOLINERGIC DRUG CAN’T TREAT ARRHYTHMIAS UNLESS THEY ARE CAUSED BY EXCESSIVE VAGAL TONE
What are the clinical indications of Anticholinergic drugs?
Sinus bradycardia
AV blocks during anesthesia
What type of Anti-Arrhythmic is Atropine Sulphate?
Antimuscarinic
What type of Anti-Arrhythmic is Glycopyrolate?
Antimuscarinic
Compare and Contrast the main functions of Glycopyrrolate and Atropine Sulphate
Atropine Sulphate
Crosses the BBB
Mechanism: Affects the SA node and increases conduction through the AV node.
Indications: Good for treating bradycardia, specifically when there is a vagal component.
Vascular Effect: Has no significant effect on vasculature.
Adverse Effects (ADR):
CNS excitation.
Decreased GI contractions and urinary bladder tone.
Bronchodilation, mydriasis (pupil dilation), and cycloplegia (paralysis of the ciliary muscle).
Dry mouth.
Glycopyrrolate
Doesn’t cross the BBB
Indications: Often used as a preanesthetic to treat sinus bradycardia, SA arrest, or incomplete AV block.
Adverse Effects (ADR):
Dry mouth.
Decreased bronchial secretions.
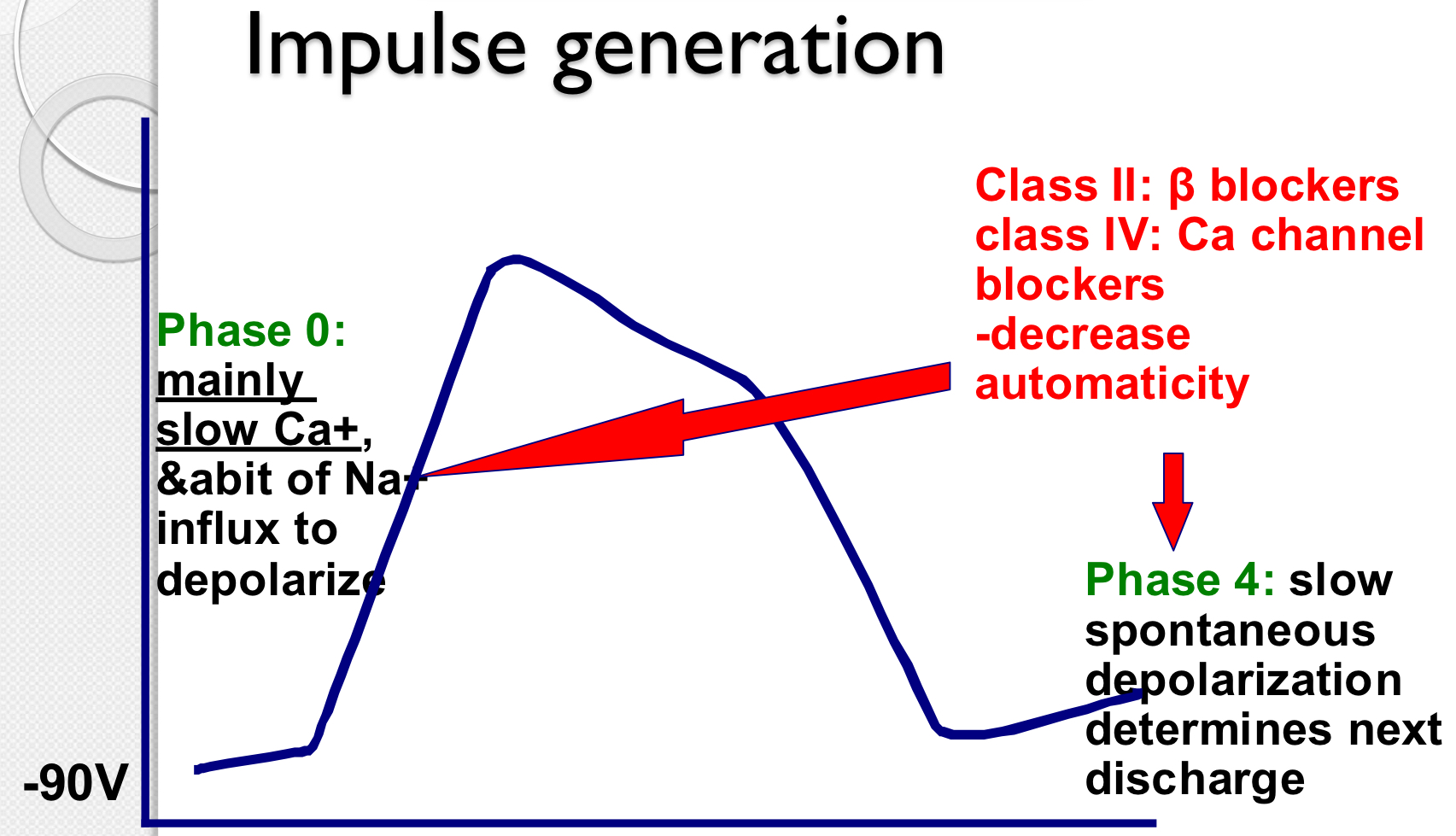
Which Anti-Arrhythmics affect Impulse generation (Phase 0 and Phase 4)?
Class II (Beta-Blockers)
Class IV (Ca Blockers)
What drugs are effective at treating ventricular arrhythmias short and long term?
Short
Lidocain
Long
Procainamide
Mexiletine
Sotalol
What drugs are effective at treating Atrial Tachycardias?
Calcium channel blockers (Type IV)
Beta-Blockers (Type II)
Digoxin
Decreasing sympathetic input to the heart may be the key to prolonged survivability, what type of drugs do this?
Beta-Blockers
ACE inhibitors
Spironolactone