NPB 101: Muscular System, Emphasis on Skeletal Muscle
1/85
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
86 Terms
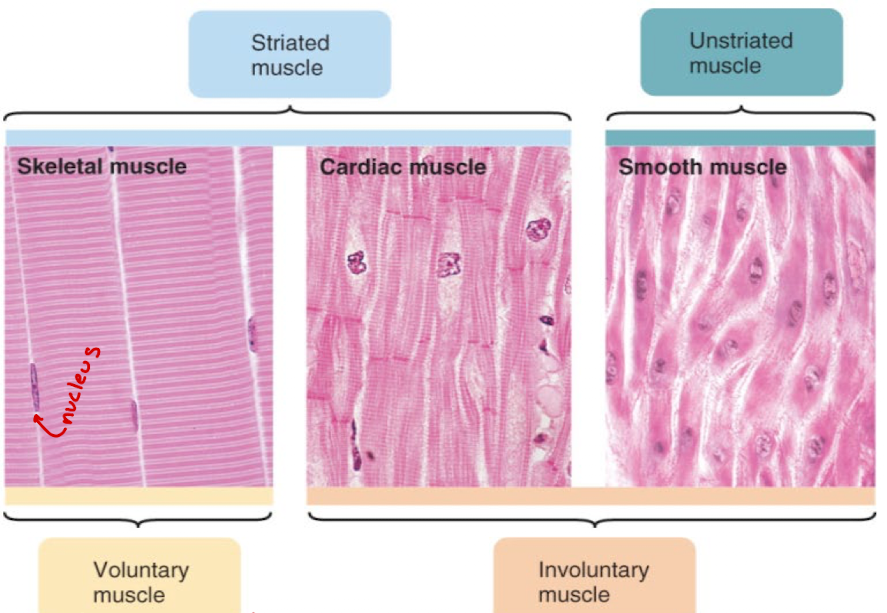
Skeletal muscle
striated and voluntary
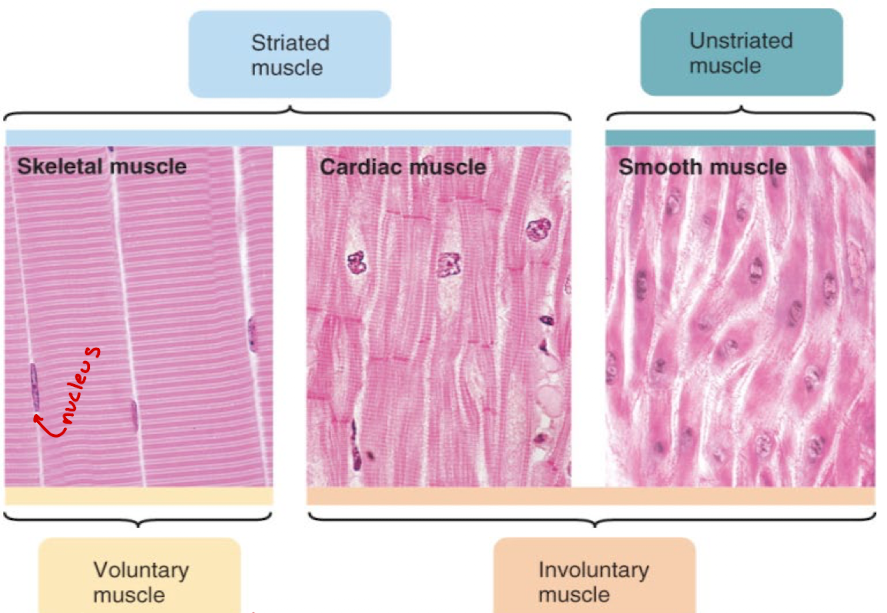
smooth muscle
muscle fibers located in the walls of hollow organs and tubes as blood vessels and intestines. Not Striated, Involuntary
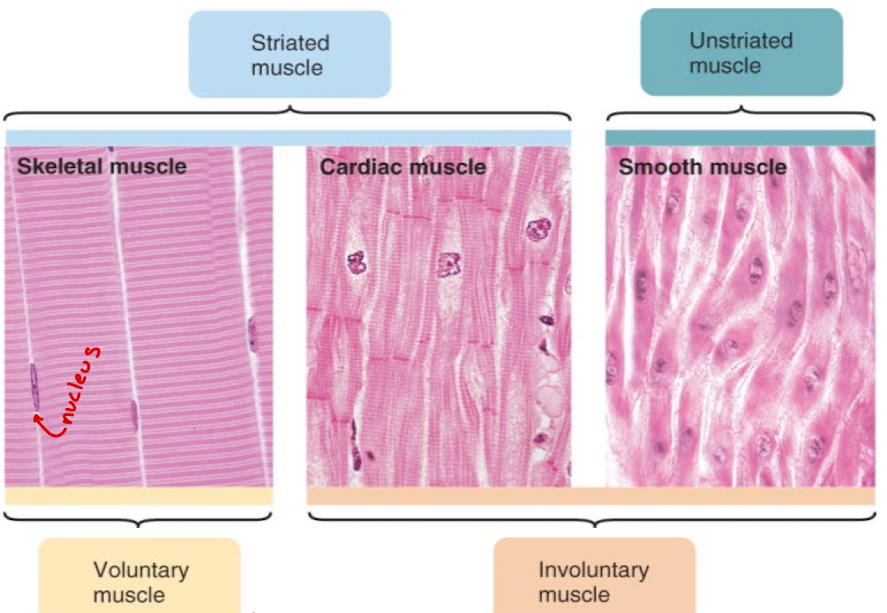
Structure of Smooth Muscle (what does/n’t it contain, shape, size)
Smooth muscle cell is spindle shaped
Smaller than skeletal muscle fibers
Single nucleus, with the capacity to divide throughout life of individual
Thick myosin-containing filaments,
Thin containing filaments, anchored to plasma membrane or cytoplasmic structures (dense bodies)
Thin and thick filaments not organized into myofibrils
No troponin, No sarcomeres
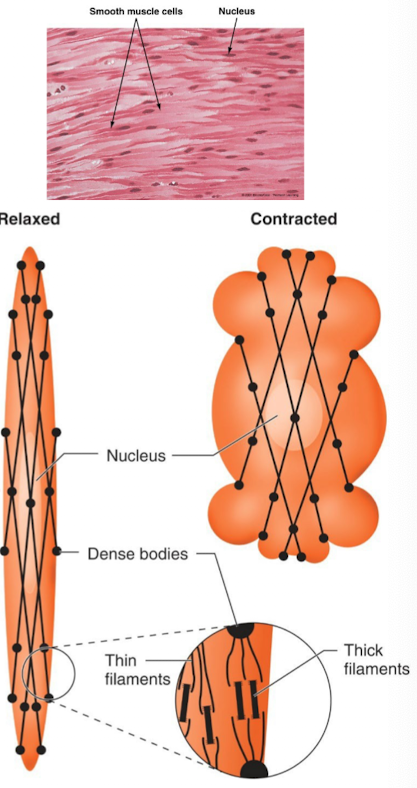
What happens during excitation of smooth muscle contraction?
Ca++ acts as an intracellular messenger that leads to the phosphorylation of myosin
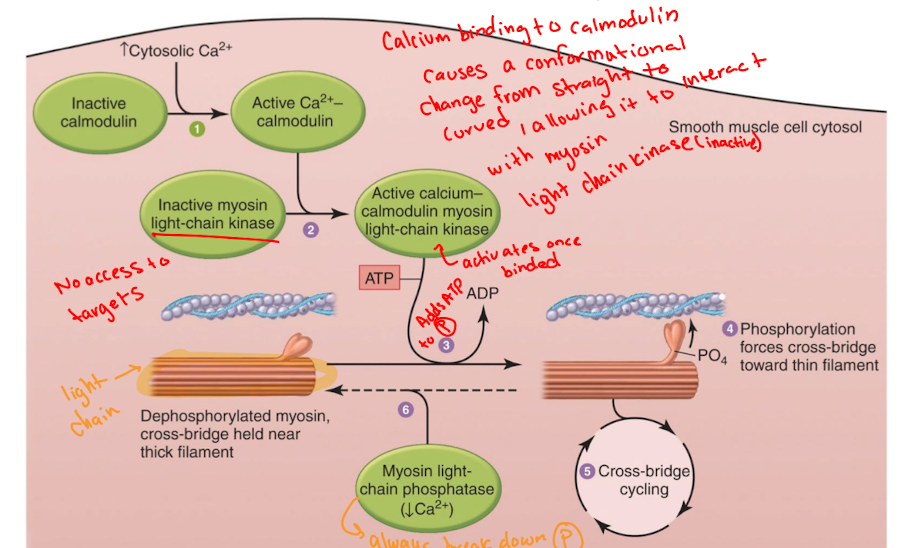
Difference between smooth muscle and skeletal muscle for cross-bridge activation
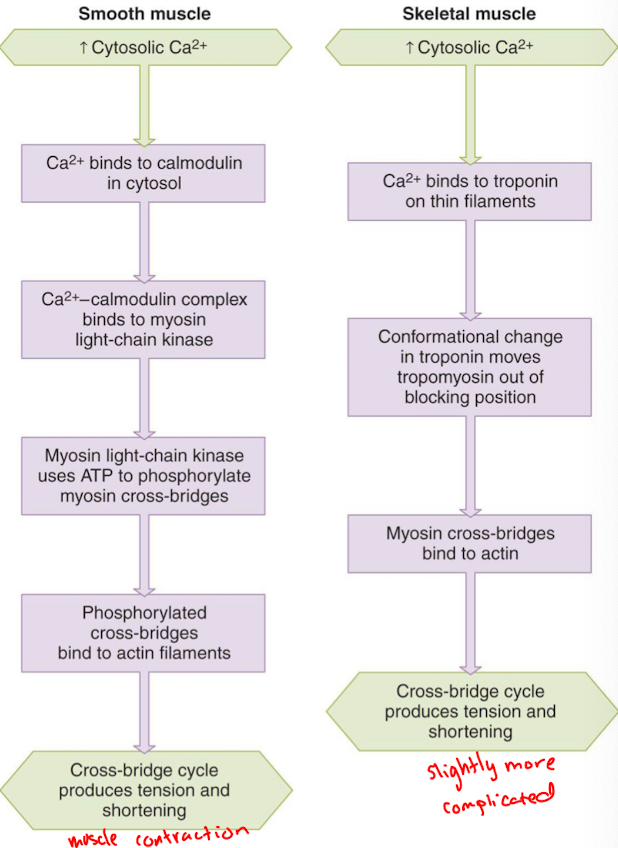
Excitation/contraction coupling in smooth muscle (7)
self or neuronal excitation leads to Ca++ entry from the extracellular space through voltage-gated Ca++ channels
Ca++ entry triggers the internal release of more Ca++ from the sarcoplasmic reticulum
Ca++ -calmodulin complex activities myosin kinase which phosphorylates myosin
phosphorylated myosin binds to actin to form the activated cross-bridges
removal of Ca++ leads to dephosphorylation of myosin and the dissociation of myosin from actin
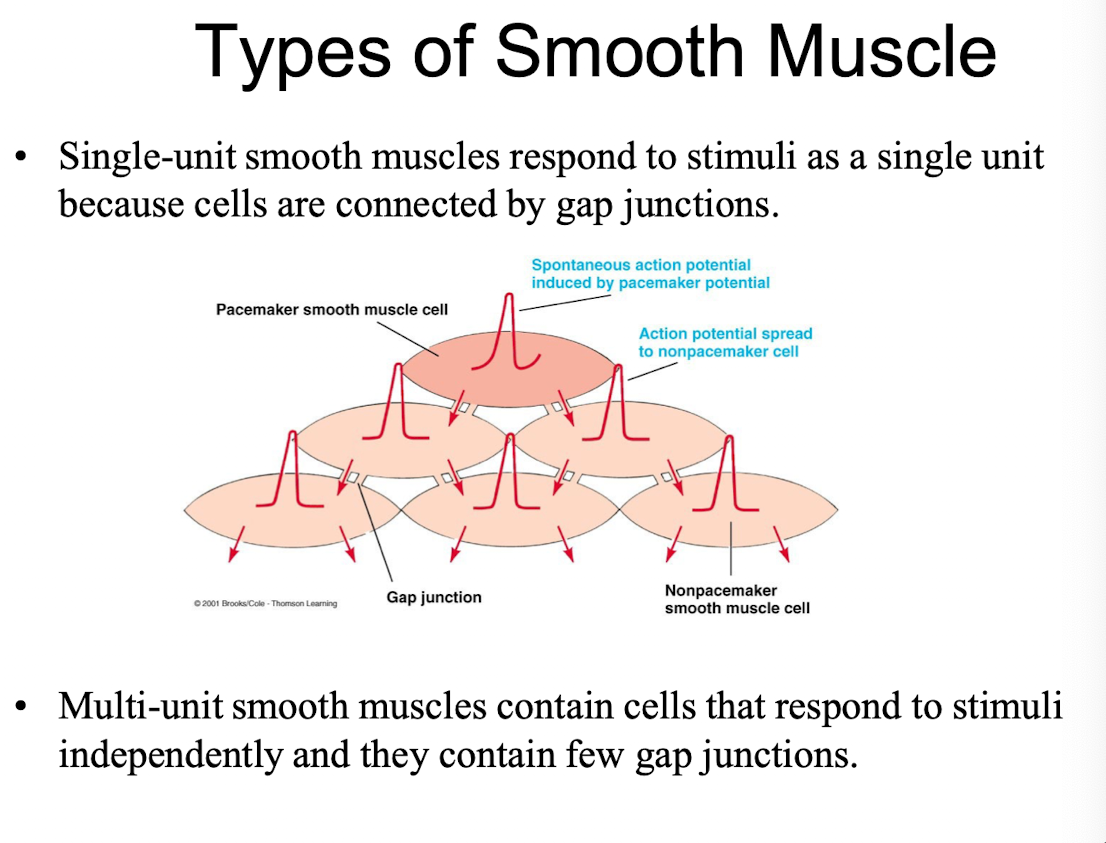
gap-junctions enable excitation of one cell to propagate rapidly to all the couples cells in a network
contraction strength is graded in proportion to the cytosolic Ca++ concentration
T/F: Transverse (T) tubules are present in smooth muscle
false, point of them is to release calcium inside the cell by activating ryanodine receptors
Which one of the following is NOT true about smooth muscle?
A. Both actin and myosin are found in the smooth muscle cell cytoplasm, but these are not arranged in sarcomere units.
B. The needed calcium (Ca2+) for contraction comes primarily from the extracellular fluid.
C. Similar to skeletal muscle cells, smooth muscle cells are capable of only all-or-nothing twitches.
D. Unlike the myosin molecules of skeletal muscle cells, the myosin found in smooth muscle cells is quite long, with its entire length covered with myosin head groups.
C. Similar to skeletal muscle cells, smooth muscle cells are capable of only all-or-nothing twitches.
T/F: In smooth muscle contraction, the majority of calcium (Ca++) needed for contraction enters the cell from the extracellular fluid.
True bc they don’t have well-developed SR, so they need Ca from outside
What are the two functionally distinct types of smooth muscle
Multi-unit smooth muscle
Single-uint smooth muscle
Multi-unit smooth muscle definition and examples
smooth muscle cells that are activated by neuronal input (neurogenic)
Examples:
walls of large blood vessels
large airways to the lungs
muscles of the eye that adjust the lens
iris of the eye
at the base of hair follicles (“goosebumps”)
Single Unit Smooth Muscle definition and examples
smooth muscle cells capable of generating pacemaker activity that are coupled into a functional syncytium by gap-junctions
Examples:
walls of the digestive tract
walls of the reproductive tract
walls of the urinary tract
walls of small blood vessels
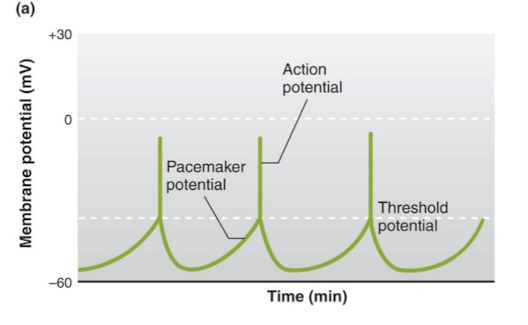
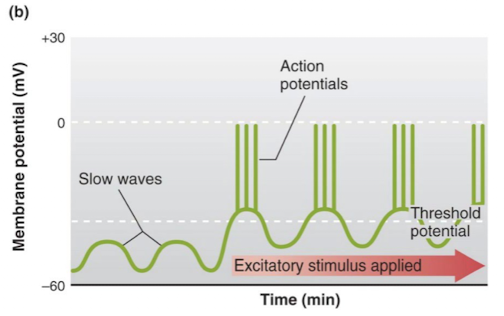
2 Forms of Spontaneous Electrical Activity
Pacemaker potential, Slow wave potential
Pacemaker potential
gradual depolarization until threshold is reached
slow wave potential
alternating depolarizing and hyper-polarizing swings in membrane potential (way of being ready with action potential without making action potential)
What does controlled contraction of muscle allow?
Purposeful movement of the whole body or parts of the body
Manipulation of external objects
Propulsion of contents through various hollow internal organs
Emptying contents of certain organs to the external environment
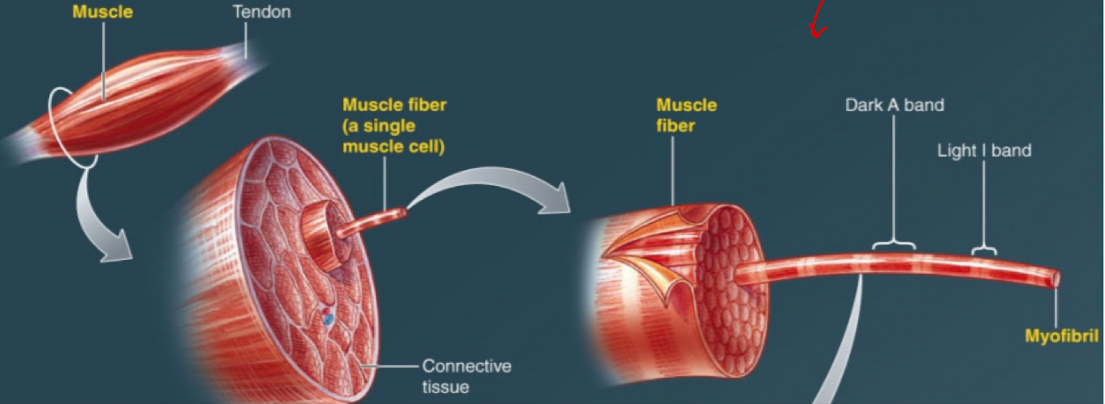
Muscle Definition
population of elongated muscle fibers held together by connective tissue and connected at either end by tendons
Skeletal muscle (“fiber”) structure
many mitochondria
multi-nucleated
Special structures called Transverse tubules (T tubules)
elongated myofibrils
A bands and I bands
sarcomeres
Z-lines, M-lines, H-zone
Thick (myosin) filaments
Thin (actin) filaments
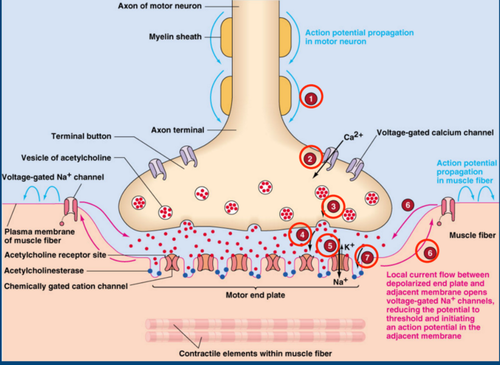
Neuromuscular Junction (NMJ); 7 Sequence of Events
Action potential propagates into the terminal bouton
Depolarization of the terminal “bouton” opens voltage-gated Ca++ channels
Ca++ ions trigger vesicles of ACh to fuse with the plasma membrane
ACh diffuses across the synaptic cleft and binds with receptors in the motor endplate
ACh binding with the receptor leads to the opening of cation channels. Na ++ enters and depolarizes the end plate (EPP)
Depolarizing current flows to adjacent membrane that contains voltage-gated Na++ channels (action potential)
ACh is degraded by ACh-esterase, terminating the action of ACh
Myofibril
elongated, cylindrically-shaped contractile elements composed of a population of sarcomeres connected end-to-end
Muscle fibers
long, slender cells that make up muscles. Each muscle consists of a group of fibers that are bound together by connective tissue.
- muscle fibers have myofibrils
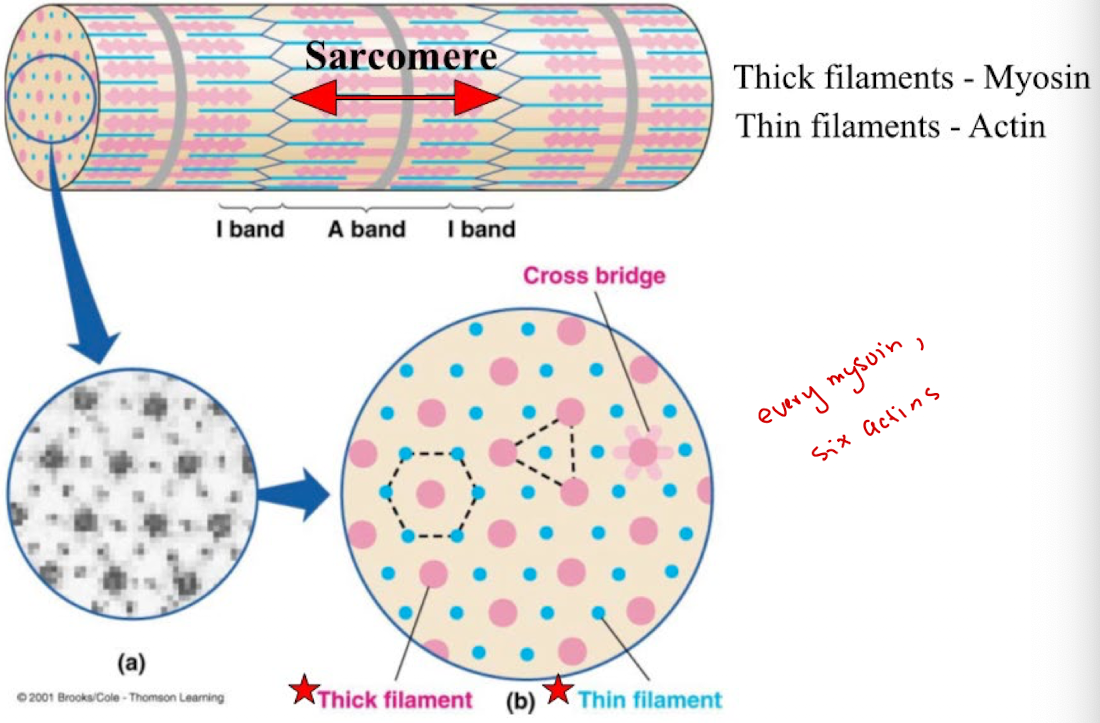
How many actin molecules are there per myosin?
6 actin per myosin; hexagonal
How many myosin are there per 1 actin?
Three myosin proteins surround 1 actin protein (triangular shape)
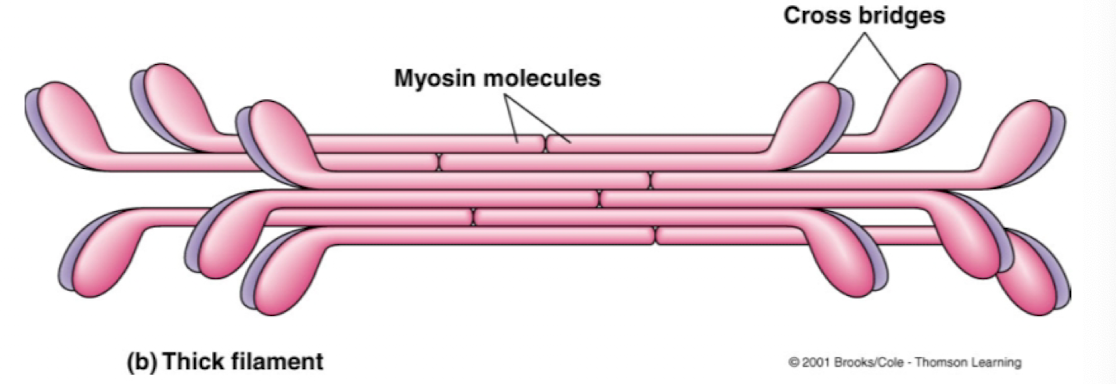
Thick filaments are composed of
special assemblies of hundreds of myosin protein molecules organized into elongated fibers
More efficient for muscle contraction
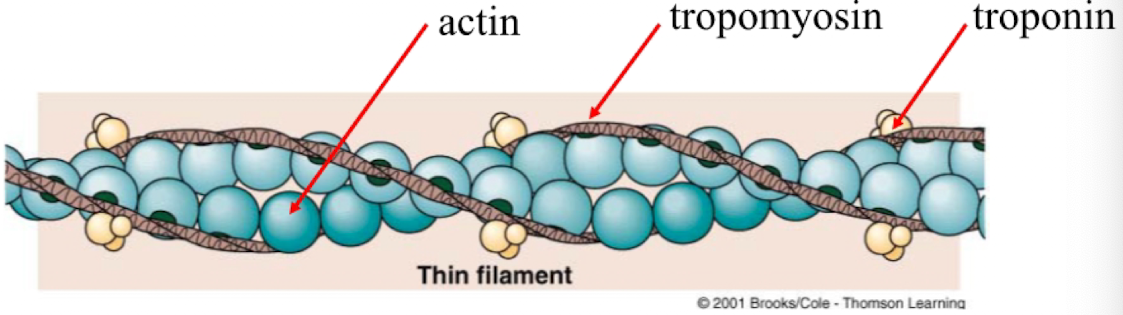
Thin filaments are composed of
specialized assemblies of three proteins
actin
tropomysoin
troponin
arranged to form an elongated double helical strand
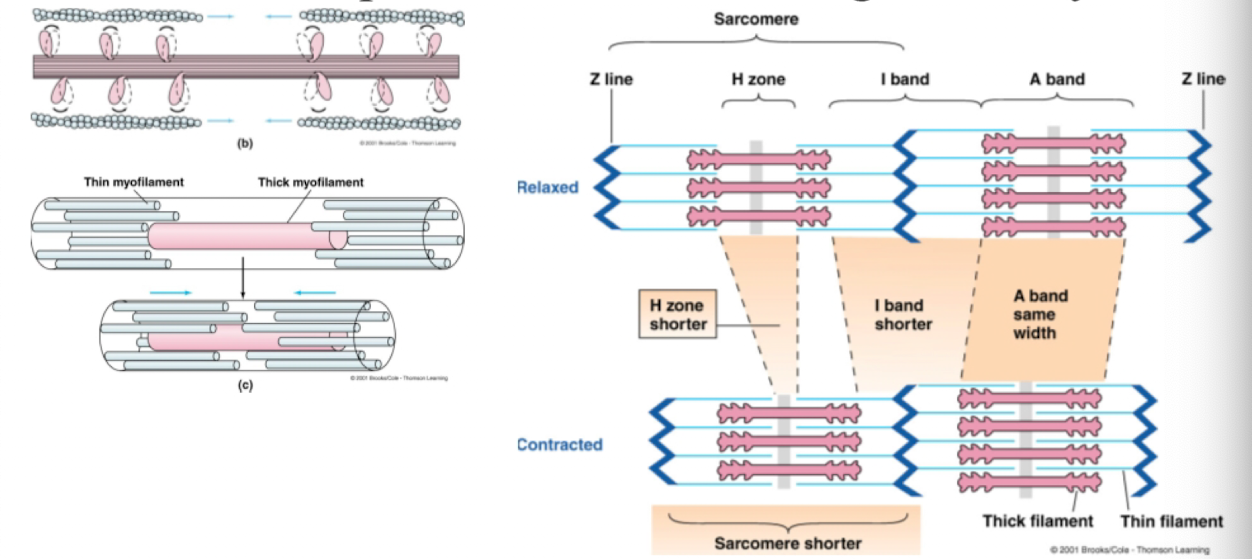
Sarcomere
the smallest unit of a muscle cell containing all of the elements necessary for contraction
composed of interdigitating and partially-overlapping thick and thin filaments
functional unit of the contractile system in straited muscle
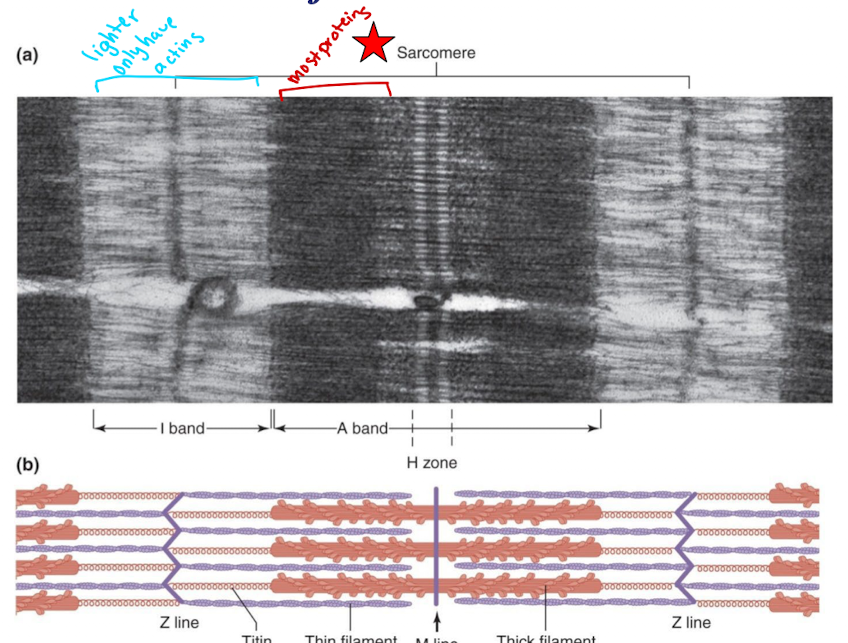
The light band of the sarcomere has which of the following filament protein?
Actin
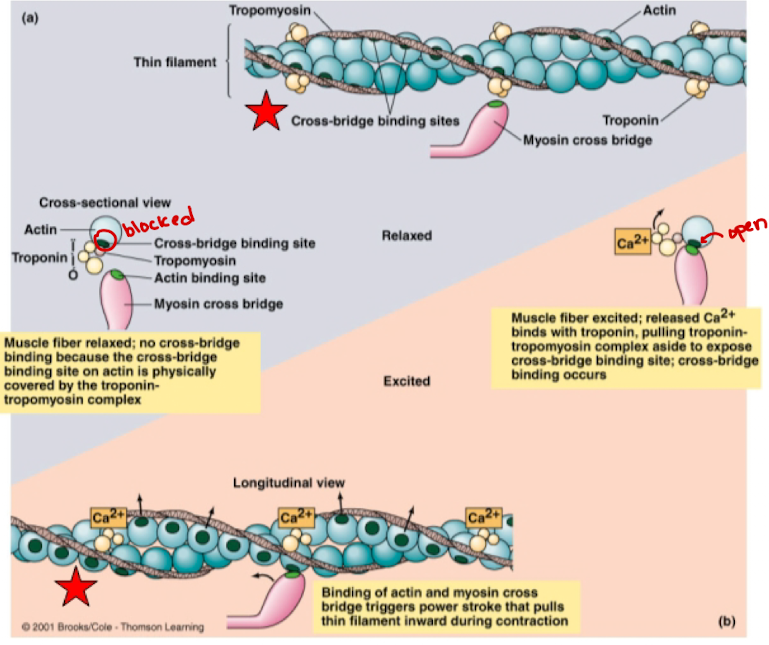
Three types of troponin
Troponin I: Inhibitory subunit
Troponin T: Tropomyosin binding subunit
Troponin C: Calcium (Ca++) binding subunit
If we remove I and T, C wouldn’t work and you will have residual muscle contraction throughout life
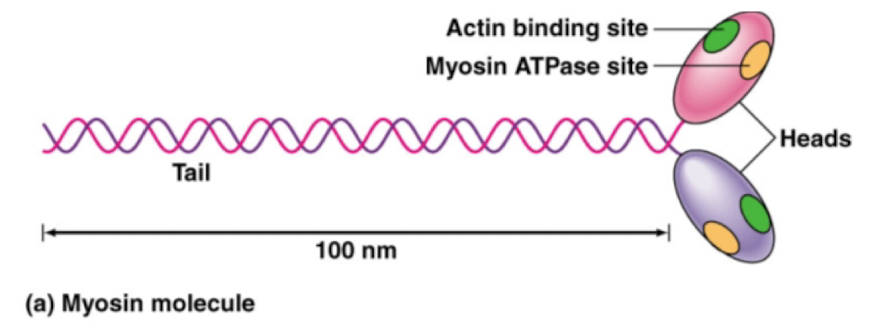
Myosin
Cytoskeletal protein composed of 2 interwoven subunits, each with a long tail and globular head region
actin
globular cytoskeletal protein linked to form two long chains arranged in a double helical strand
2 heads of myosin that help with cross-bridge
Actin binding site & myosin ATPase (ATP hydrolysis)
tropomyosin
pairs of threadlike filamentous proteins that lie alongside the groove formed by the actin helix
Cross-Bridge Activity
Binding: Myosin cross bridge binds to actin molecules
Power Stroke: Cross bridge bends, pulling thin myofilament inward
Detachment: Cross bridge detaches at end of power stroke and returns to original conformation (requires ATP)
Binding: Cross bridge binds to more distal actin molecule; cycle repeats
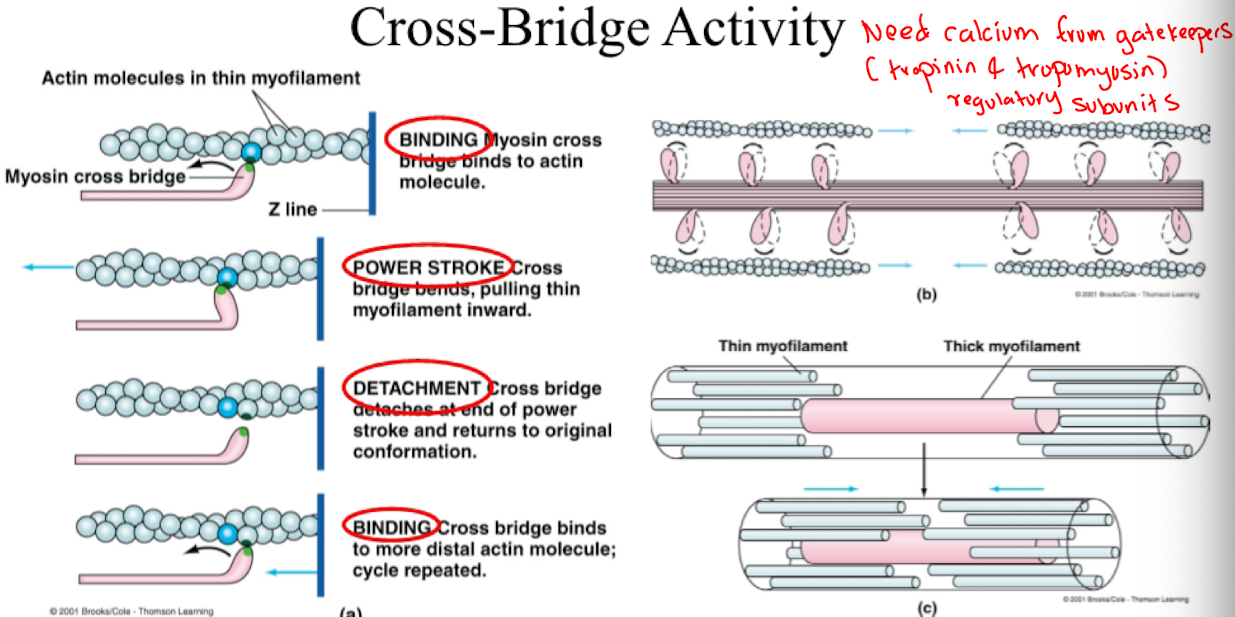
Consequences of cross- bridge activity (5)
1) Sarcomere shortens
2) H zone becomes shorter
3) I band becomes shorter
4) A bands maintains the same width
5) Individual actin and myosin fibers maintain a constant length
Role of Ca++ in turning on cross bridges
When muscle fiber relaxed, cross-bridge binding site is covered by the troponin-tropomyosin complex
When muscle fiber is excited, Ca++ binds to troponin, pulling the troponin-tropomyosin complex aside to expose cross-bridge binding sites
The contractile protein of skeletal muscle involving ATPase activity is
myosin
Calcium ions trigger the start of muscle contraction by
binding to troponin
Muscle Functions
Purposeful movement of the whole body or parts of the body
Manipulation of external objects
Propulsion of contents through various hollow internal organs
Emptying of contents of certain organs to external environments
Z-line
defines boundary of sarcomere; site where thin filaments attach
A band
made up of thick filaments along with portions of thin filaments that overlap
H zone
lighter area within middle of A band where thing filaments do not reach
M line
extends vertically down middle of A band within center of H zone
I band
consists of remaining portion of thin filaments that do not project into A band
Which of the following regulates smooth muscle but not striated muscle contraction?
Calmodulin
Transverse (T) Tubule (skeletal muscle)
Invagination of the plasma membrane at each sarcomere
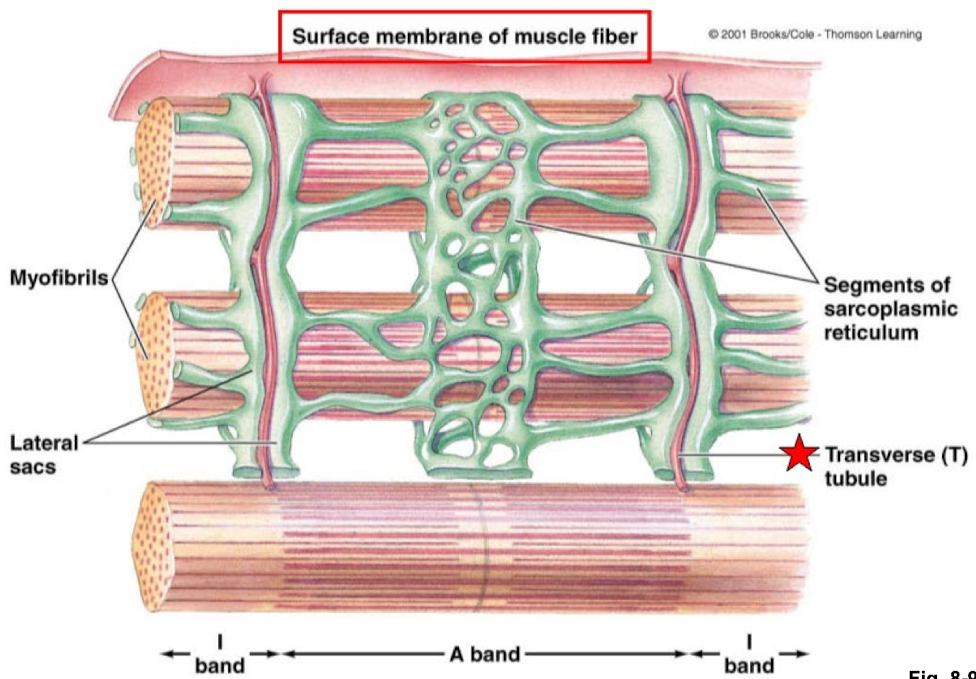
Sarcoplasmic Reticulum (skeletal muscle)
modified endoplasmic reticulum composed of a fine network of interconnected tubules into which Ca++ is actively transported and stored

Lateral Sacs (skeletal muscle)
Enlarged regions of the sarcoplasmic reticulum that come into close contact
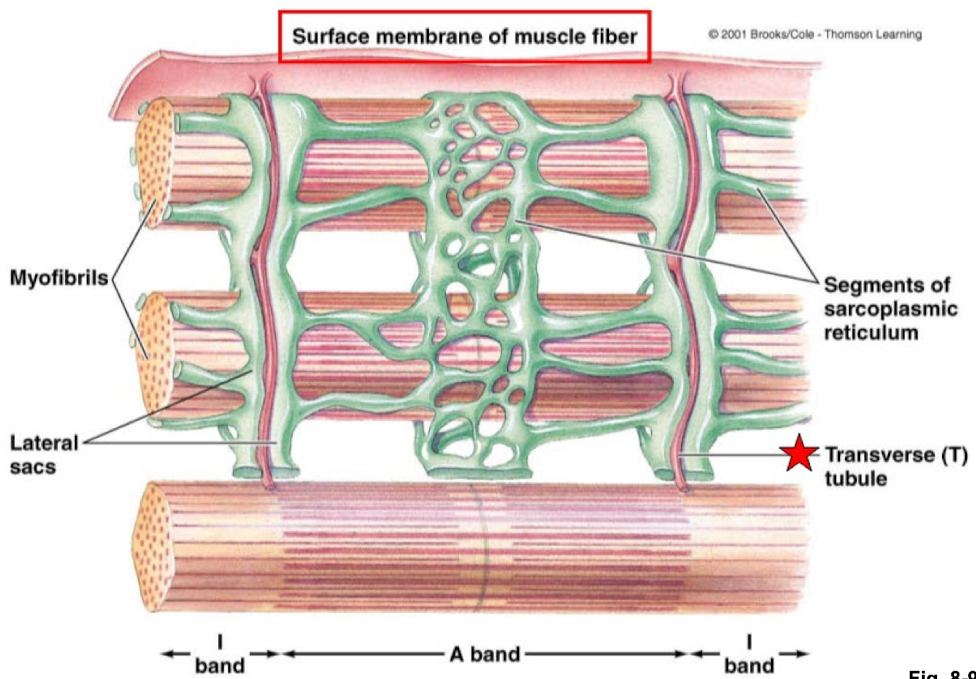
Foot Proteins (skeletal muscle)
proteins that span the gap between the lateral sacs and the transverse tubules and mediate a change in permeability to Ca++ by the lateral sacs. Also known as ryanodine receptors because they are locked open by the plant chemical ryanodine
Located in the membrane of the S.R.
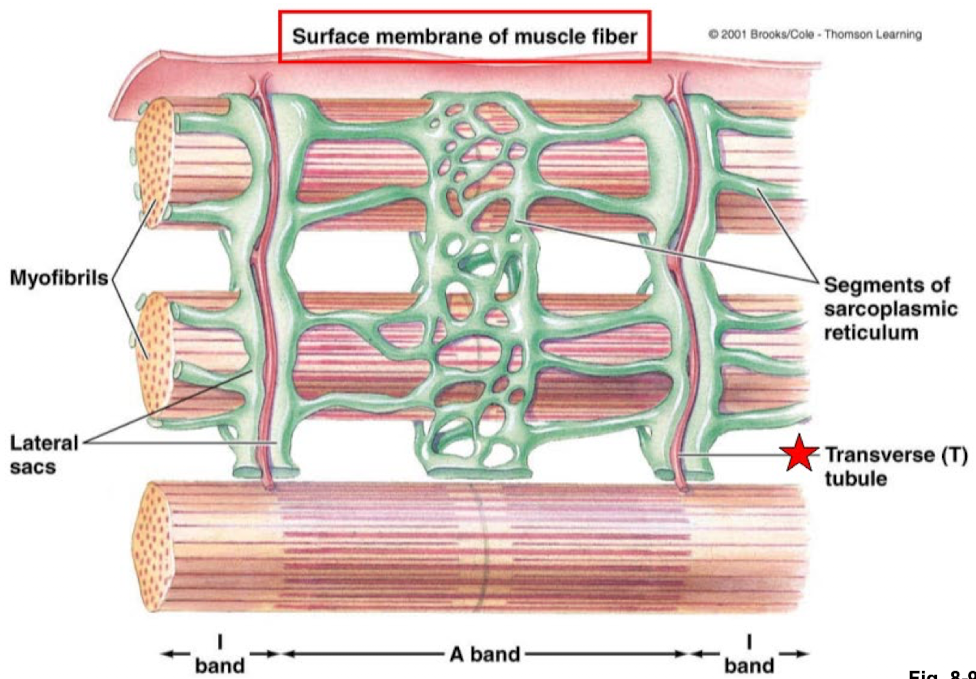
Dihydropyridine Receptor (skeletal muscle)
receptor proteins in the transverse tubule membrane that come into contact with the foot proteins. They are voltage dependent and gate the change in permeability of foot proteins to Ca++
Located in the membrane of the T tubule
Excitation-Contraction Coupling
Muscular contraction occurs when the thick and thin filaments within a sarcomere slide past one another
How is the sliding action mediated in excitation-contraction coupling in skeletal muscle?
By a complex sequence of chemical reactions called the power stroke that utilizes the hydrolysis of ATP as an energy source and is dependent on the release of intracellular stores of Ca++ from the sarcoplasmic reticulum
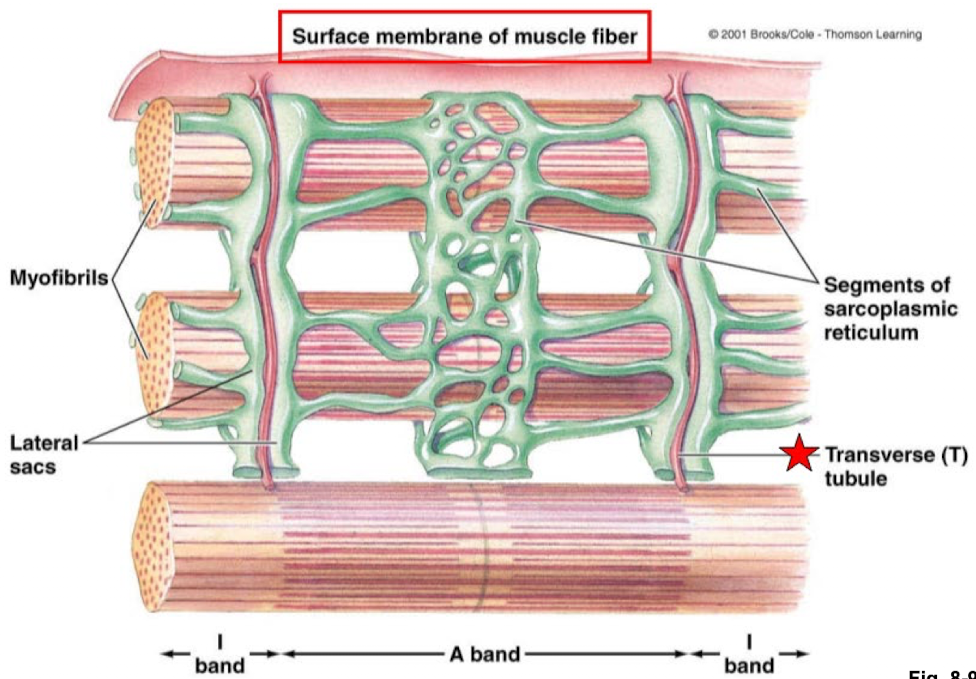
7 Steps to Excitation/Contraction Coupling in Skeletal Muscle
ACh released by axon of motor neuron binds to receptors on the motor end plate
Action potentials generated in response to binding of ACh and subsequent end plate potential is propagated across surface of membrane and down T tubule of muscle cell
Action potential triggers Ca++ release from sarcoplasmic reticulum
Ca++ ions released from lateral sacs bind to troponin on actin filaments; tropomyosin physically moved aside to uncover cross-bridge binding sites on actin
Myosin cross bridges attach to actin and bend, pulling actin filaments towards center of sarcomere powered by energy provided by ATP
Ca++ actively taken up by sarcoplasmic reticulum when there is no longer local action potentials
With Ca++ no longer bound to troponin, tropomyosin slips back to its blocking position over the binding sites on actin; contraction ends; actin slides back to original resting position
Role of ATP in Muscle Contraction
ATP is split by myosin ATPase; energy stored in cross bridge
Ca++ released upon excitation moves the inhibitory influence on actin
Power stroke of cross bridge; ADP and Pi released
Linkage between actin and myosin broken as fresh ATP binds to myosin
In excitation-contraction coupling, the transverse tubules function to…
conduct an action potential into the sarcoplasmic reticulum
Acetylcholine in muscles
is the primary neurotransmitter at the NMJ, responsible for the hyper-polarization of the post synaptic sarcolemma
Diffuses across the NMJ to activate Na+/K+ channels on a post-synaptic dendrite, initiating end plate potential
Binds to voltage gated channels in the junctional folds, initiating end plate potential
Is degraded by ACherase to prevent continuous muscle stimulation
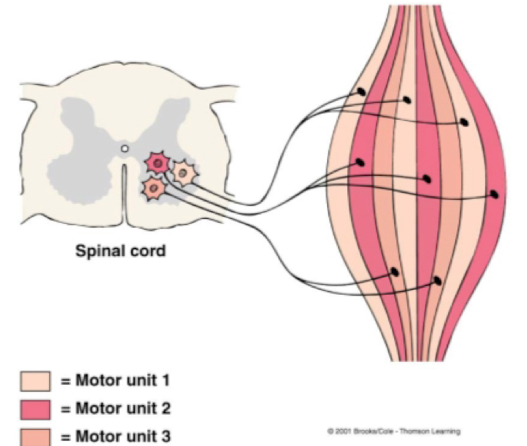
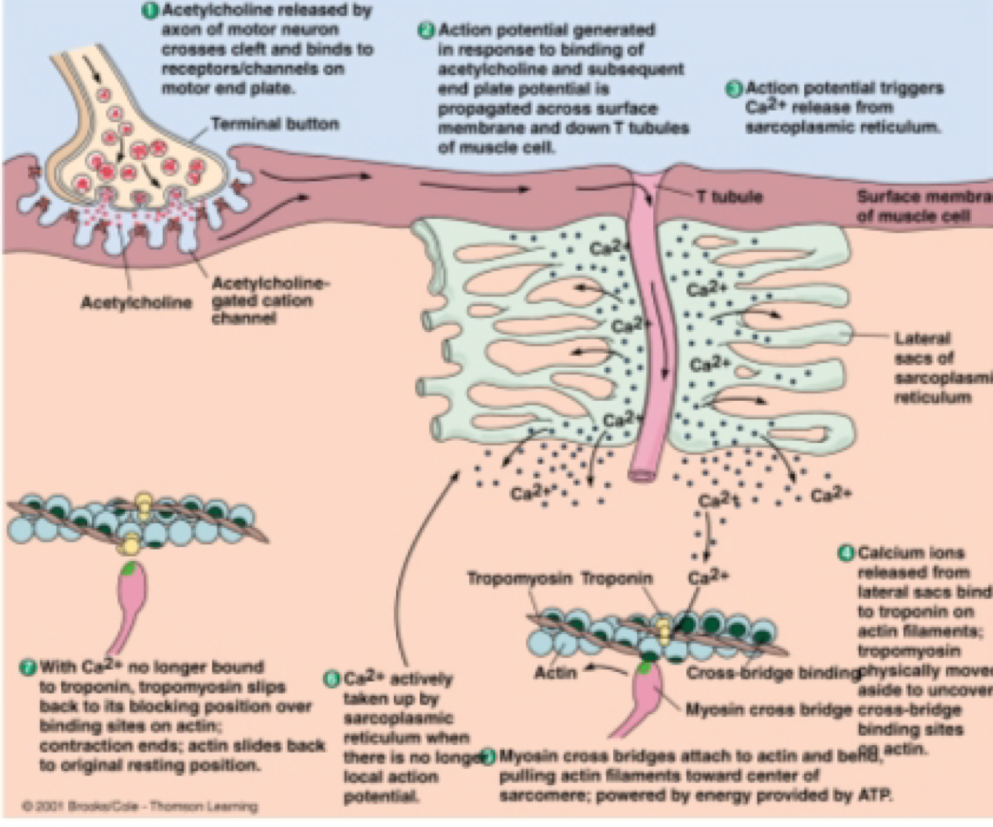
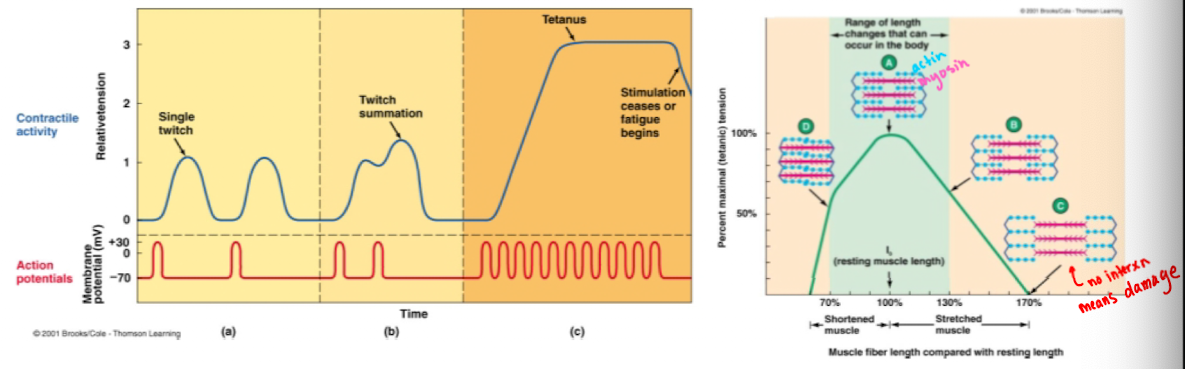
Motor Unit
A motor neuron and all the muscle fibers it innervates
One motor neuron innervates multiple muscle fibersm but each muscle fiber is supplied by only one motor neuron
When a motor neuron is activated, all of the muscle fibers it innervates are stimulated to contract simultaneously
The muscle fibers innervated by a given motor neuron are distributed throughout the muscle; thus, their simultaneous contraction results in an evenly distributed (although weak) contraction of the whole muscle
Fewer fibers per motor unit mean muscles
produce precise, delicate movements (weak contractions)
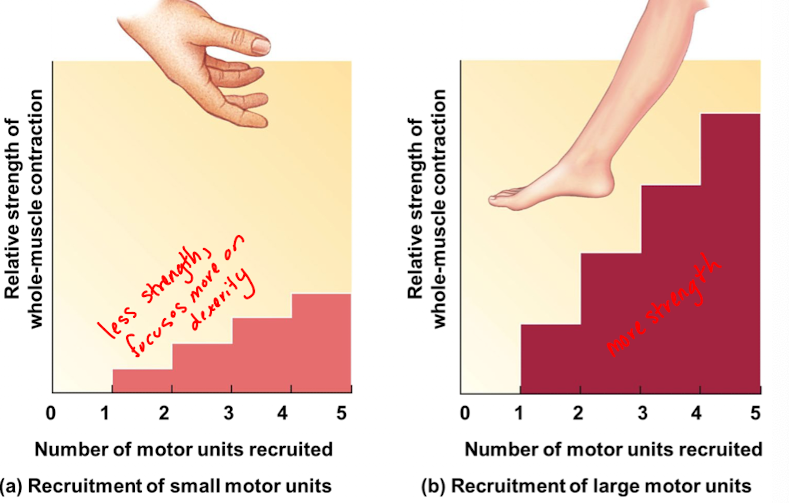
More fibers per motor unit mean muscles
perform powerful, coarsely controlled movement (stronger contractions)
4 factors that influence the extent to which tension can be developed in a fiber
the frequency of stimulation
the length of the fiber at the onset of contraction
the extent of fatigue
the thickness of the fiber
muscle generates force called ____ in order to oppose a force called the ___, which is exerted on the muscle by an object.
tension; load
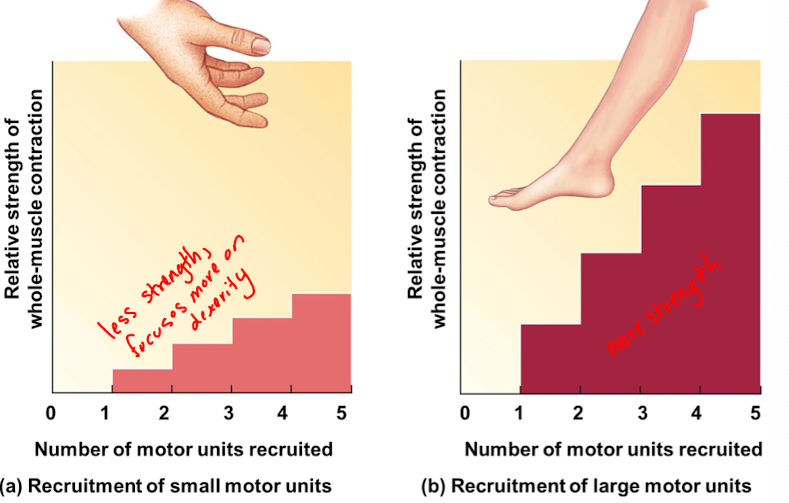
The mechanical response of a muscle fiber to a ___ action potential is known as a ____.
single; twitch
Excitation-contraction coupling involves
A. hyper-polarization of the sarcolemma
B.an increase in the sarcomere's actin-myosin overlap
C.sliding of acting and myosin filaments past each other
D.attachment of actin heads to myosin
E.attachment of Calcium to troponin in order to free
actin binding sites
E. Attachment of calcium to troponin in order to free actin binding sites
Motor unit recruitment
increasing number of motor units contracting
Asynchronous recruitment of motor units
to delay or prevent fatigue
Twitch summation: what it is and how is it possible and resulted from
The increase in tension accompanying repetitive stimulation of a muscle fiber.
Possible bc the duration of the action potential is much shorter than the duration of the resulting twitch
Results from sustained elevation of cytosolic calcium upon repetitive stimulation
Tetanus: what is it and when is it stimulated
Smooth, sustained contraction of maximal strength (3x-4x stronger than a single twitch)
occurs if muscle fiber is stimulated so rapidly that tit does not have a chance to relax btwn stimuli
What is the length-tension relationship in muscle fibers?
Muscle fiber tension depends on its length at the start of contraction. Maximum tension is developed at an optimal length (lo) and less tension is produced at shorter or longer lengths
What limits how much muscles can shorten or lengthen?
The attachment of muscles to bones
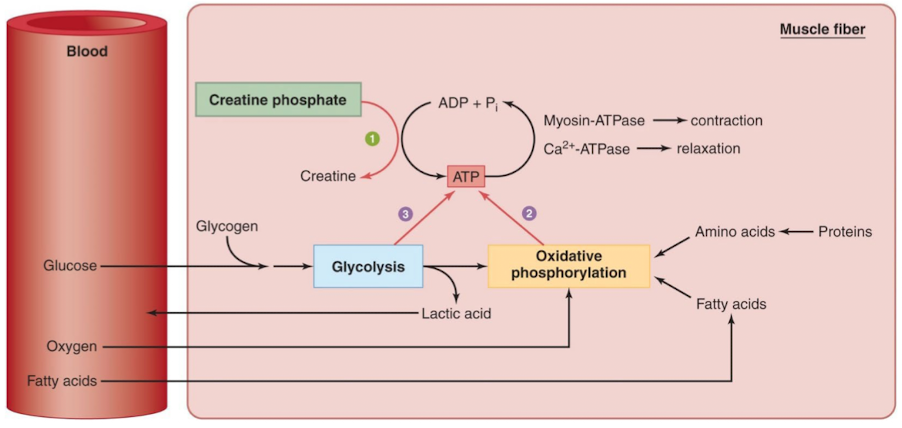
Muscle metabolism: ATP provides energy source for what and where is ATP derived from?
ATP provides the sole energy source for muscular activity: the power stroke and the active transport of Ca++.
The ATP is derived from 3 metabolic sources: Creatine phosphate, Oxidative Phosphorylation, Glycolysis
1.Creatine Phosphate
Provides a reserve of high energy phosphate for synthesis of ATP
During rest, excess ATP generated by glycolysis and oxidative phosphorylation is converted to creatine phosphate that is stored by muscle cells as an energy reserve
2.Oxidative Phosphorylation
Aerobic metabolism of glucose and fatty acids. Makes use of the high myoglobin content of muscle
3.Glycolysis
Anaerobic metabolism of glucose. The byproduct, excess pyruvic acid, is converted to lactiv acid that is removed by the bloodstream
Skeletal Muscle Energy Metabolism: 3 ways a muscle fiber can form ATP
Phosphorylation of ADP by creatine phosphate
Oxidative phosphorylation of ADP in the mitochondria
Phosphorylation of ADP by the glycolytic pathway in the cytosol
Fatigue; results from…
inability of muscle to maintain tension. Can result from muscle fatigue or neuromuscular fatigue
Muscle fatigue
occurs when an exercising muscle can no longer respond to stimulation with the same degree of contractile activity
primary factors of muscle fatigue
depletion of glycogen reserves (energy substrates)
local increases of metabolic byproducts
lactic acid
H+
inorganic phosphate
Impaired calcium release or uptake, neural fatigue
recovery in muscle fatigue
replenishment of muscle glycogen and creatine phosphate following intense activity
Neuromuscular fatigue
inability of the NMJ to synthesize ACh rapidly enough to sustain chemical transmission of AP’s from the motor axon to the muscle cell
Central fatigue
occurs when the CNS no longer adequately activates motor neurons
Excess post-exercise oxygen consumption (EPOC)
is the need for elevated O2 uptake during recovery from exercise
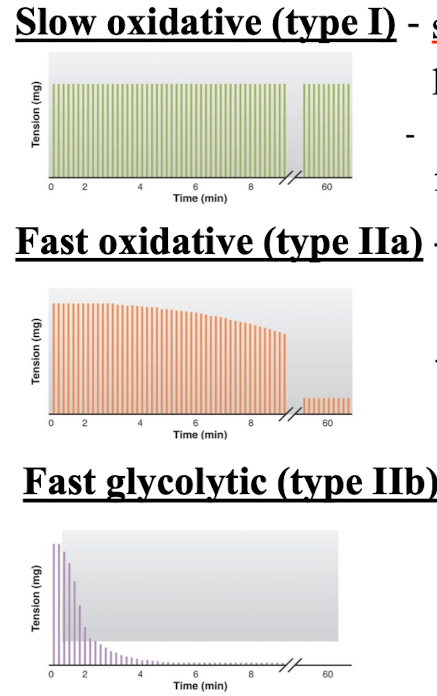
Skeletal Muscle Types: Slow oxidative (type I)
slow contraction and reliance on oxidative phosphorylation for ATP
High in mitochondria, blood supply, and myoglobin
some glycogen storage
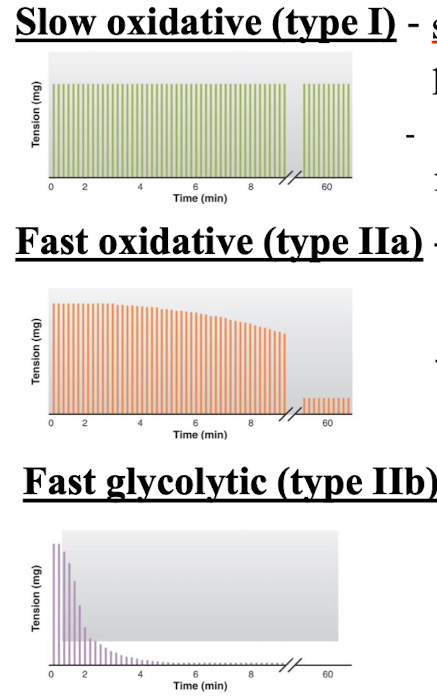
Skeletal Muscle Types: Fast oxidative (type IIa)
fast contraction and reliance on oxidative phosphorylation for ATP
high in mitochondria, blood supply, and myoglobin
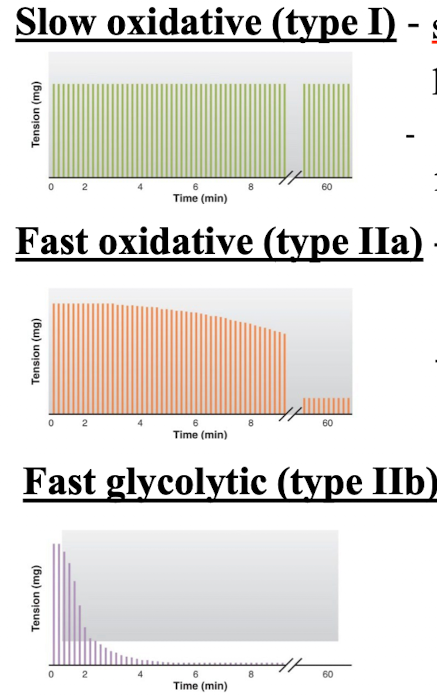
Skeletal Muscle Types: Fast glycolytic (type IIb)
very fast contraction and reliance on glycolysis for ATP
low in mitochondria, blood supply and myoglobin
high in muscle glycogen
3 skeletal muscle types
slow oxidative (type I)
Fast Oxidative (type IIa)
Fast glycolytic (type IIb)
Cardiac muscle
Striated, involuntary found only in the heart and shares characteristics of both skeletal and smooth muscle
Cardiac muscle structure and features
striated
thin filaments contain tropomyosin and troponin
contains an abundacen of mitochondria and myoglobin
possess T-tubules and sarcoplasmic reticulum
Ca++ enters the cytosol from voltage-gated Ca++ channels in the plasma membrane and triggers internal release of Ca++
Displays pacemaker activity initiating its own action potentials
connected by gap-junctions
innervated by autonomic neuronal fibers
action potentials are longer in duration than both smooth and skeletal muscles