6.4 - Homeostasis is the maintenance of a stable internal environment
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
What is homeostasis?
Internal environment is maintained within
set limits around an optimum.
Why is it important that core temperature
remains stable?
Maintain stable rate of enzyme-controlled
reactions & prevent damage to membranes.
Temperature too low = enzyme & substrate
molecules have insufficient kinetic energy.
Temperature too high = enzymes denature.
Why is is important that blood pH
remains stable?
Maintain stable rate of enzyme-controlled
reactions (& optimum conditions for other
proteins).
Acidic pH = H + ions interact with H-bonds & ionic
bonds in tertiary structure of enzymes → shape
of active site changes so no ES complexes form.
Why is it important that blood glucose
concentration remains stable?
● Maintain constant blood water potential:
prevent osmotic lysis / crenation of cells.
● Maintain constant concentration of respiratory
substrate: organism maintains constant level of
activity regardless of environmental conditions.
Define negative and positive feedback.
Negative feedback: self-regulatory mechanisms
return internal environment to optimum when
there is a fluctuation.
Positive feedback: a fluctuation triggers
changes that result in an even greater deviation
from the normal level.
Outline the general stages involved in
negative feedback
Receptors detect deviation →
coordinator → corrective mechanism by
effector → receptors detect that
conditions have returned to normal.
Suggest why separate negative
feedback mechanisms control
fluctuations in different directions.
Provides more control, especially in case
of ‘overcorrection’, which would lead to a
deviation in the opposite direction from
the original one.
Suggest why coordinators analyse inputs
from several receptors before sending an
impulse to effectors.
● Receptors may send conflicting
information.
● Optimum response may require
multiple types of effector.
Why is there a time lag between
hormone production and response by an
effector?
It takes time to:
● produce hormone
● transport hormone in the blood
● cause required change to the target
protein
Name the factors that affect blood
glucose concentration.
● Amount of carbohydrate digested from
diet.
● Rate of glycogenolysis.
● Rate of gluconeogenesis.
Define glycogenesis, glycogenolysis and
gluconeogenesis
Glycogenesis: liver converts glucose into the storage
polymer glycogen.
Glycogenolysis: liver hydrolyses glycogen into glucose
which can diffuse into blood.
Gluconeogenesis: liver converts glycerol & amino acids into
glucose.
Outline the role of glucagon when blood
glucose concentration decreases.
1. 𝞪 cells in Islets of Langerhans in pancreas detect
decrease & secrete glucagon into bloodstream.
2. Glucagon binds to surface receptors on liver cells &
activates enzymes for glycogenolysis &
gluconeogenesis.
3. Glucose diffuses from liver into bloodstream.
Outline the role of adrenaline when blood
glucose concentration decreases.
1. Adrenal glands produce adrenaline. It
binds to surface receptors on liver cells &
activates enzymes for glycogenolysis.
2. Glucose diffuses from liver into
bloodstream.
Outline what happens when blood
glucose concentration increases.
1. 𝝱 cells in Islets of Langerhans in pancreas detect
increase & secrete insulin into bloodstream.
2. Insulin binds to surface receptors on target cells to:
a) increase cellular glucose uptake
b) activate enzymes for glycogenesis (liver & muscles)
c) stimulate adipose tissue to synthesise fat
Describe how insulin leads to a decrease
in blood glucose concentration
● Increases permeability of cells to glucose.
● Increases glucose concentration gradient.
● Triggers inhibition of enzymes for
glycogenolysis.
How does insulin increase permeability
of cells to glucose?
● Increases number of glucose carrier
proteins.
● Triggers conformational change which
opens glucose carrier proteins.
How does insulin increase the glucose
concentration gradient?
● Activates enzymes for glycogenesis in
liver & muscles.
● Stimulates fat synthesis in adipose
tissue.
Use the secondary messenger model to
explain how glucagon and adrenaline
work.
1. Hormone-receptor complex forms.
2. Conformational change to receptor activates G-protein.
3. Activates adenylate cyclase, which converts ATP to
cyclic AMP (cAMP).
4. cAMP activates protein kinase A pathway.
5. Results in glycogenolysis.
Explain the causes of Type 1 diabetes
and how it can be controlled.
Body cannot produce insulin e.g. due to
autoimmune response which attacks 𝝱
cells of Islets of Langerhans.
Treat by injecting insulin.
Explain the causes of Type 2 diabetes
and how it can be controlled.
Glycoprotein receptors are damaged or become
less responsive to insulin.
Strong positive correlation with poor diet / obesity.
Treat by controlling diet and exercise regime.
Name some signs and symptoms of
diabetes.
High blood glucose concentration
● Glucose in urine
● Polyuria
● Polyphagia
● Polydipsia
● Blurred vision
● Sudden weight loss
● Blurred vision
Suggest how a student could produce a
desired concentration of glucose solution
from a stock solution.
Volume of stock solution = required concentration x
final volume needed / concentration of stock solution.
Volume of distilled water = final volume needed -
volume of stock solution.
Outline how colorimetry could be used to
identify the glucose concentration in a
sample.
1. Benedict’s test on solutions of known glucose
concentration. Use colorimeter to record absorbance.
2. Plot calibration curve: absorbance (y-axis), glucose
concentration (x-axis).
3. Benedict’s test on unknown sample. Use calibration curve
to read glucose concentration at its absorbance value.
Define osmoregulation
Control of blood water potential via
homeostatic mechanisms.
Describe the gross structure of a
mammalian kidney.
Fibrous capsule: protects kidney.
Cortex: outer region consists of Bowman’s capsules, convoluted
tubules, blood vessels.
Medulla: inner region consists of collecting ducts, loops of Henle,
blood vessels.
Renal pelvis: cavity collects urine into ureter.
Ureter: tube carries urine to bladder.
Renal artery: supplies kidney with oxygenated blood.
Renal vein: returns deoxygenated blood from kidney to heart.
Describe the structure of a nephron.
Bowman’s capsule at start of nephron: cup-shaped, surrounds
glomerulus, inner layer of podocytes.
Proximal convoluted tubule (PCT): series of loops surrounded
by capillaries, walls made of epithelial cells with microvilli.
Loop of Henle: hairpin loop extends from cortex into medulla.
Distal convoluted tubule : similar to PCT but fewer capillaries.
Collecting duct: DCT from several nephrons empty into
collecting duct, which leads into pelvis of kidney.
Describe the blood vessels associated
with a nephron
Wide afferent arteriole from renal artery enters renal
capsule & forms glomerulus: branched knot of
capillaries which combine to form narrow efferent
arteriole.
Efferent arteriole branches to form capillary network
that surrounds tubules.
Explain how glomerular filtrate is formed.
Ultrafiltration in Bowman’s capsule.
High hydrostatic pressure in glomerulus forces small
molecules (urea, water, glucose, mineral ions) out of
capillary fenestrations AGAINST osmotic gradient.
Basement membrane acts as filter. Blood cells & large
molecules e.g. proteins remain in capillary.
How are cells of the Bowman’s capsule
adapted for ultrafiltration?
● Fenestrations between epithelial cells
of capillaries.
● Fluid can pass between & under
folded membrane of podocytes.
State what happens during selective
reabsorption and where it occurs.
Useful molecules from glomerular filtrate
e.g. glucose are reabsorbed into the
blood.
Occurs in proximal convoluted tubule.
Outline the transport processes involved
in selective reabsorption.
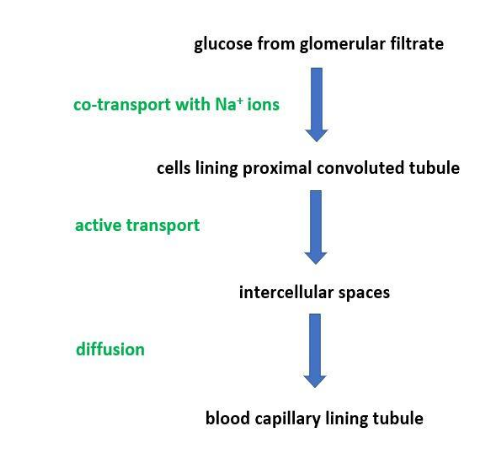
How are cells in the proximal convoluted
tubule adapted for selective
reabsorption?
● Microvilli: large surface area for co-transporter
proteins.
● Many mitochondria: ATP for active transport
of glucose into intercellular spaces.
● folded basal membrane: large surface area.
What happens in the loop of Henle?
1. Active transport of Na + & Cl - out of ascending limb.
2. Water potential of interstitial fluid decreases.
3. Osmosis of water out of descending limb
(ascending limb is impermeable to water).
4. Water potential of filtrate decreases going down
descending limb: lowest in medullary region,
highest at top of ascending limb.
Explain the role of the distal convoluted
tubule.
Reabsorption:
a) of water via osmosis
b) of ions via active transport
permeability of walls is determined by
action of hormones.
Explain the role of the collecting duct.
Reabsorption of water from filtrate into
interstitial fluid via osmosis through
aquaporins.
Explain why it is important to maintain an
Na + gradient.
Countercurrent multiplier: filtrate in collecting
ducts is always beside an area of interstitial fluid
that has a lower water potential.
Maintains water potential gradient for maximum
reabsorption of water.
What might cause blood water potential
to change?
● level of water intake
● level of ion intake in diet
● level of ions used in metabolic
processes or excreted
● sweating
Explain the role of the hypothalamus in
osmoregulation.
1. Osmosis of water out of osmoreceptors
in hypothalamus causes them to shrink.
2. This triggers hypothalamus to produce
more antidiuretic hormone (ADH).
Explain the role of the posterior pituitary
gland in osmoregulation.
Stores and secretes the ADH produced
by the hypothalamus.
Explain the role of ADH in
osmoregulation.
1. Makes cells lining collecting duct more permeable to water:
● Binds to receptor → activates phosphorylase → vesicles
with aquaporins on membrane fuse with cell-surface
membrane.
2. Makes cells lining collecting duct more permeable to urea:
● water potential in interstitial fluid decreases.
● more water reabsorbed = more concentrated urine.