GI E2- GI bleed
1/91
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
92 Terms
Hgb in upper GI tract is cleaved to ________ by gastric pepsin or pancreatic proteases in proximal SI.
Heme & globin
What is the intestinal converted fraction of heme?
Portion of heme that isn’t absorbed in the SI is converted to porphyrins & iron (detected by heme-porphyrin assay, not guaiac FOB)
What measures both heme and porphyrins, and is therefore a highly accurate indicate of bleeding, regardless of its level?
Heme porphyrin assay
Is globin in the upper GI tract detected by immunochemical FOB tests?
No because it is digested by pepsin and pancreatic/intestinal proteases
sites of bleeding & likelihood of + FOBT
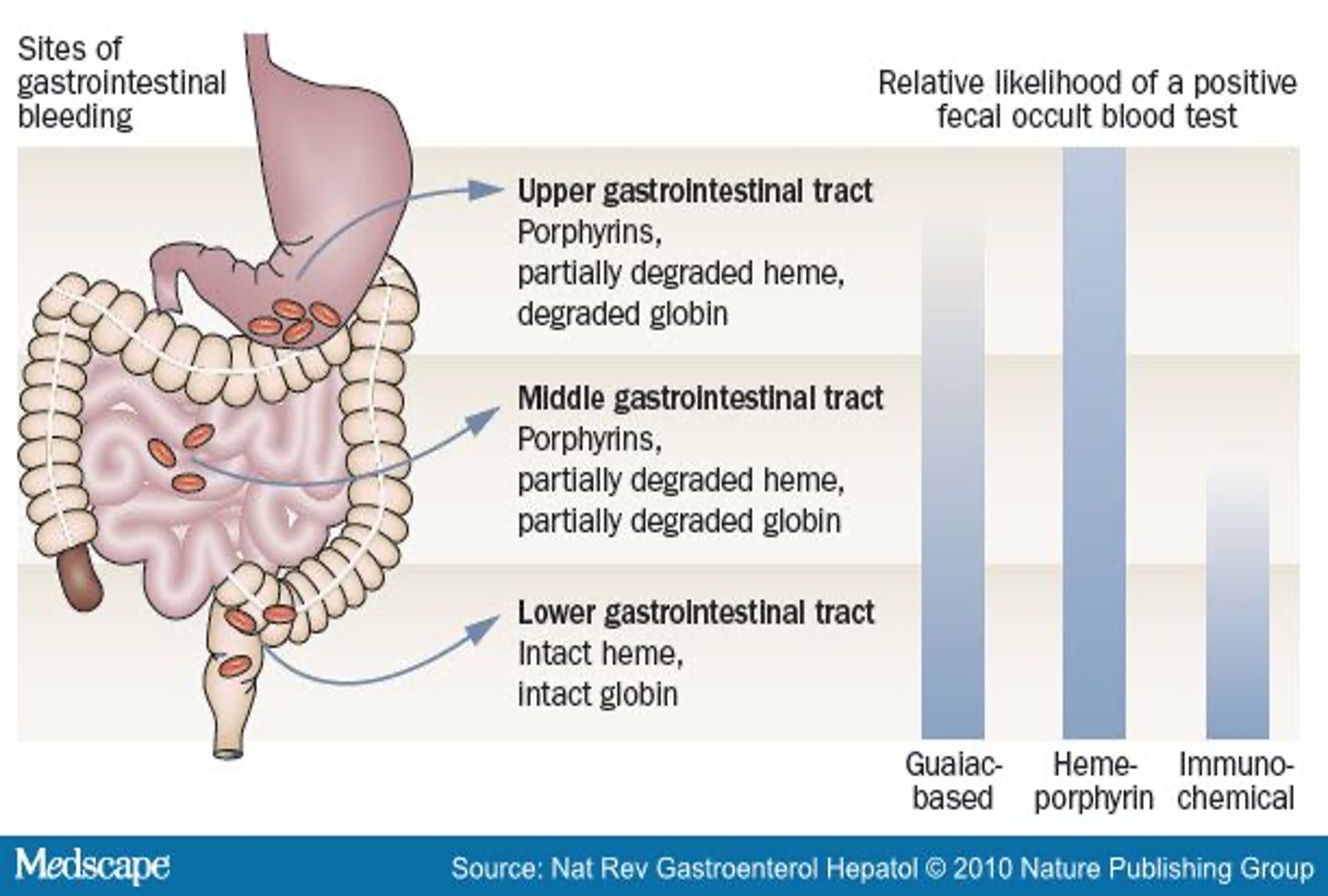
What is the most sensitive test for detecting lower bowel bleeding?
Guaiac FOBT (hemoccult)
What kind of fecal occult blood test (FOBT)?
reaction based on presence of Hgb in sample, requires addition of hydrogen peroxide
Hgb contains pseudoperoxidase which turns guaiac blue
Guaiac / hemoccult
What foods are associated with a false positive guaiac test?
Red meat, cantaloupe, melons, grapefruit, figs, turnips, radishes, horseradish, cauliflower
What meds are associated with a false positive guaiac test?
Vitamin C, NSAIDs, high dose ASA
What kind of fecal occult blood test (FOBT) identifies only intact human hemoglobin?
Immunochemical (hemeselect, feca/eia, fit)
What are advantages to immunochemical FOBT?
red meat & food based peroxidases do NOTt give false positives; specific for lower GI tract bleeding
What are disadvantages to immunochemical FOBT?
requires inc lab staff time; detects only lower GI tract bleeding
What type of fecal occult blood test (FOBT)?
quantifies blood loss
sensitive for both upper and lower GI bleed
not affected by medications or dietary peroxidase (except red meat)
Heme-porphyrin assay (HemoQuant)
Which of the following has the highest sensitivity for a UGI - guaiac, immunochemical, or heme-porphyrin assay?
Heme-porphyrin assay
Which FOBT should be used for CRC screening?
Guaiac & immunochemical
Which FOBT should be used for anemia?
Heme-porphyrin assay
What is vomitus of red blood or “coffee ground” material?
Hematemesis
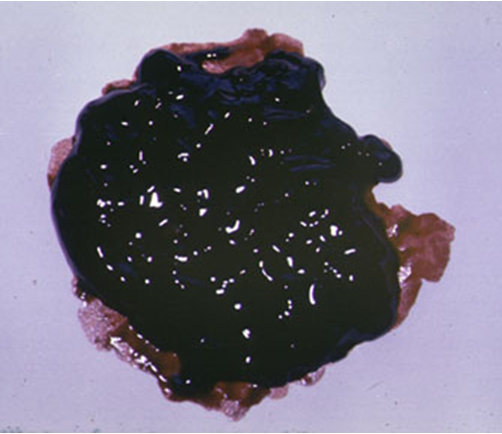
What is black, tarry, shiny, foul smelling stool?
Melena
What is an expulsion of bright red / maroon blood from the rectum?
Hematochezia

What is bleeding that is not visible and is therefore identified by special stool testing, and can arise from anywhere in GI tract?
Occult bleeding
How is anemia detected?
Routine bloodwork or bloodwork performed secondary to sx of blood loss
What are symptoms of blood loss?
Lightheadedness, syncope, angina, tachycardia, dyspnea
What are the 5 ways in which GI bleeding (GIB) can present?
Hematemesis, melena, hematochezia, occult bleeding, anemia
What refers to any blood loss within the GI tract form upper esophagus to duodenum, above the ligament of Treitz, and is considered a medical emergency?
Acute UGIB
Where does bleeding from the small bowel occur?
Ligament of Treitz to ileocecal valve
How can acute UGIB onset?
Can be from intermittent to abrupt
What can the severity of acute UGIB range?
Low grade occult bleeding (+FOBT, anemia) to massive blood loss (hematemesis, hypovolemic shock)
What connects the fourth portion of the duodenum to the diaphragm near the splenic flexure of the colon, and is the anatomic cut off for UGIB?
Ligament of treitz
What would cause death in an acute UGIB?
Decompensation or underlying issue (pts rarely exsanguinate)
What are the 3 clinical predictors of death in pts hospitalized with UGIB?
Older age, comorbidities, hemodynamic compromise
What are RF for acute UGIB?
Long term low dose ASA, combo ASA & clopidogrel, hx peptic ulcers & prior GI bleed, males, age > 70
When can pts with an acute UGIB restart ASA?
Restart if risk for CV complications outweighs the risk for bleeding
What are the 2 categorizations of acute UGIBs?
*(acute mgmt and resuscitation remains the same regardless of origin**)
Variceal and nonvariceal
What is a nonvariceal acute UGIB?
From ulcer or erosion of GI mucosa into underlying vessel (mallory Weiss tears, ulcers, tumors)
What is the MCC of acute UGIB?
PUD
What are possible causes of acute UGIB?
Ulcerative, erosive, inflammatory: PUD, ASA, NSAIDs, ZE, stress/pill induced ulcer
Trauma: mallory weiss tear, FB aspiration
Vascular lesions: varices, angiomas, portal HTN, AVM
Tumors: polyp, carcinoid, metastatic, adenocarcinoma
The following ssx are associated with what condition?
Dizzy, lightheaded, weak, pallor
palpitations, tachycardia, hypotension
normochromic, normocytic anemia
hematemesis / rectal bleeding
Acute/brisk UGIB
What is the treatment for acute UGIB?
Medical emergency requires hospital admission → resuscitation, stabilization, prep for emergent EGD, control bleeding/lesions, prevent and treat episodes of re-bleeding
The following treatment is for what condition?
Assess hemodynamic status: 0.9% NS or LR soln, type & screen for possible transfusion
NG tube insertion to identify source
*can produce false neg
Meds: High dose PPI IV x 72 hrs, Octreotide (somatostatin) for variceal bleeding
Endoscopy w/in 2-24 hrs & repeat in 24 hrs
Surgery for rebleeding
Bleeding PUD
When can Octreotide (Somatostatin) be used for nonvariceal bleeding?
Persistent bleeding despite optimal medical mgmt (PPIs) and those who have multiple comorbidities (poor surgical risks)
What on an NG tube insertion would confirm an upper GI bleed?
Red or coffee ground aspirate
What is the MOA of octreotide (somatostatin)?
Provides splanchnic vasoconstrictive effects, enhances plt aggregation and gastric acid suppression
Stress ulcers only occur in what kind of patients?
Extremely sick → serious trauma, major surgery, burns > 1/3 BSA, major intracranial dz, ventilator dependent, coagulopathies
What is the pharmacologic prophylaxis for stress ulcers?
IV H2RA or PPI; sucralfate
What drug adheres to ulcer sites in the stomach and duodenum to protect and promote healing, and decreases bleeding but not mortality rate?
Sucralfate (Carafate)
What is a tear in the lower esophagus at the GE junction (usually on gastric side) caused by violent vomiting, retching, or coughing?
Mallory weiss tear
What is the treatment for a mallory Weiss tear?
Usually stops spontaneously;
Active bleeding only → endoscopic therapy (injection, thermal coagulation)
What are dilated submucosal veins (weak walls) that develop in the esophagus or stomach in patients with portal HTN, and can cause serious massive UGI bleeding?
Esophageal varices (single venous collateral = varix)
What patients should be screened for varices and treated prophylactically via endoscopy & ligation?
Pts w/ hx chronic liver disease & cirrhosis
The following ssx are associated with what condition?
usually asx
hematemesis, melena, hematochezia (large bleed)
Stigmata of liver dz
Jaundice, spider telangiectasias, palmar erythema
ascites, dupuytren contractures
rhinophyma in pts w/ rosacea
Esophageal varices
What do patients with esophageal varices have a high risk of?
Recurrent bleeding w/in 6 weeks (greatest risk in first 48-72 hrs)
What are possible vascular malformations of the UGI tract (can be arterial or venous in origin)?
Angioma, AVM, telangiectasias, vascular ectasia, angiodysplasia
What is a frequent source of GI bleeding of obscure origin that is typically intermittent and low grade but can be acute, overt, and cease spontaneously?
Vascular malformations
How are vascular ectasias diagnosed?
EGD, capsule endoscopy, CT enterography, angiography
What is the treatment for vascular ectasias?
Laparoscopic small bowel resection, endoscopic therapy w/ thermal coagulation (argon plasma coagulation APC), PPIs IV or PO, octreotide
What stops acute bleeding in vascular ectasias and prevents rebleeding after endoscopy?
PPIs
What is given to all vascular ectasia patients with GI bleed and liver disease OR portal HTN?
Octreotide
What is defined as bleeding arising below the ligament of Treitz?
Acute lower GIB
Where do most acute lower GIBs arise from?
Colon
Upper or lower GIB?
less likely to have hypovolemia or require transfusions
mortality < 3%
usually acute and self limited
Lower
How can acute LGIBs present?
Hematochezia, maroon stools, melena
What is the most common presentation of an acute LGIB?
hematochezia - BRBPR
What can hematochezia/BRBPR suggest?
Acute LGIB - left colon source
can also occur with brisk UGI or small bowel bleeding
What do maroon stools suggest?
Lower GI source, typically right colon or distal small intestine
When does melena occur?
When Hgb is converted to hematin and other hemochromes by bacterial degradation over a period of atleast 14 hrs
*usually indicates digestion of blood from UGI or small bowel source
Melena or hematochezia?
sites: esophagus, stomach, duodenum
rarely jejunum, ileum, ascending colon
black, loos, tarry stools
delayed or minimal passage of blood through GI tract
Melena
Melena or hematochezia?
Site: usually distal to or affecting the colon
rapid hemorrhage of ≥1L assoc w esophageal, stomach, or duodenal bleeding
Bright red or dark, mahogany colored stools
blood mixed w/ formed stools or bloody diarrhea
reflects lower GI bleeding or rapid loss and passage of undigested blood through GI tract
Hematochezia
Are all black stools melena?
NO- use guaiac test to differentiate
*false postives- licorice, bismuth, charcoal, iron, vit C
What is the MCC of an acute LGIB?
Diverticulosis
What are causes of an acute LGIB?
Diverticulosis (MC), vascular ectasias, neoplasms, IBD (esp UC), hemorrhoids, ischemic colitis
The following symptoms are associated with what condition?
abrupt onset, painless
bright red or maroon blood
± abd cramping
can be minor or massive
stops spontaneously in most patients, rebleeding occurs in 25% of pts
Diverticulosis
How is diverticulosis diagnosed?
Abd CT, colonoscopy PRN to r/o other causes
What is the treatment for diverticulosis?
Colonoscopy to identify bleeding diverticula; bipolar coagulation, epi injection, angiography, possible surgical resection
What are mucosal & submucosal blood vessels with direct communication bt the arteries and veins w/o intermediary capillaries (often congenital and lesions are usually scattered elsewhere in colon/GI tract)?
Arteriovenous malformations (AVM)
What cause of LGIB?
painless bleeding that ranges from melena to hematochezia to occult blood loos
MC > 70 y/o
flat red lesions radiating from central lesion
Vascular ectasias
What is used to evaluate SI as source of bleeding (usually only investigated after unexplained recurrent bleeds)?
Capsule imaging/endoscopy
The following is associated with what condition?
usually presents well advanced in disease
usually cause chronic, occult blood loss
Sx: change in bowel pattern & stool shape, rectal bleeding (painless and occult or overt)
Dx: colonoscopy (TOC), flex sig w/ ACBE
Tx: surgical resection
Colonic neoplasms / bleeding cancers
What are characteristics of R sided colonic neoplasms?
Occult blood, unexplained weakness or anemia, palpable abd mass, dull abd pain
What are characteristics of L sided colonic neoplasms?
Gross rectal bleeding, obstructive sx, change in bowel pattern → pencil like or ribbon stools
What symptoms are often present in LGIB caused by IBD?
Abd pain, tenesmus, urgency, variable amounts of hematochezia
What does pain with a BM suggest?
Anal fissure
Internal hemorrhoids cause ________
Painless bleeding
How does LGIB caused by an anorectal disease appear?
Small art of blood on toilet paper or streaking on stool
What condition?
abd pain from mucosal hypoxia due to hypo perfusion of vessels in intestinal wall
pain out of proportion
Ischemic colitis / mesenteric ischemia
Where does ischemic colitis MC affect?
Splenic flexure or rectosigmoid junction due to limited collateral circulation (known as watershed areas)
In what patients is ischemic colitis MC?
Older pts w/ atherosclerotic dz (ASHD) or hyperviscosity syndromes (polycythemia vera)
In what younger patients would ischemic colitis occur?
Vasculitis, coagulation disorders, estrogen use, dehydration and strenuous/vigorous exercise
What imaging modalities can be used to evaluate an acute lower GIB?
Anoscopy and sigmoidoscopy, colonoscopy (study of choice), abd CT, nuclear bleeding scans/angiogrpahy to localize bleed
What amount of blood loss would NOT cause any change in stool?
< 100 mL/day
How is occult bleeding identified?
FOBT, heme-porphyrin assay, IDA
What can cause occult GIB?
Neoplasms, vascular abnormalities, acid peptic lesions, NSAIDs, ASA, IBD, infx (nematodes, TB)
How is occult GI bleeding evaluated?
Colonoscopy and/or EGD depending on presentation (alarm sx, fhx GI cancer, anemia disproportionate to menstrual loss)
Capsule endo, CT enterography, or surgical laparotomy (rare)