Midterm 1
0.0(0)
Card Sorting
1/123
There's no tags or description
Looks like no tags are added yet.
Last updated 2:16 AM on 9/17/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
124 Terms
1
New cards
Understand the history of Immunology and the concepts which shaped it
* Edward Jenner's observations that milkmaids exposed to cowpox were protected against smallpox led to his experiments vaccinating people with cowpox to prevent smallpox infection. This pioneering work introduced the concept of acquired immunity through exposure/vaccination.
* Louis Pasteur provided evidence supporting the germ theory of disease - that microorganisms cause infectious disease. This was a key foundation for understanding immune responses to pathogens.
* In the late 19th century, concepts emerged of humoral immunity mediated by antibodies in serum and cellular immunity mediated by direct killing by cells. This formed the basis of adaptive immunity.
\
* Louis Pasteur provided evidence supporting the germ theory of disease - that microorganisms cause infectious disease. This was a key foundation for understanding immune responses to pathogens.
* In the late 19th century, concepts emerged of humoral immunity mediated by antibodies in serum and cellular immunity mediated by direct killing by cells. This formed the basis of adaptive immunity.
\
2
New cards
Describe “The Immune problem” and how it relates to our body's defenses
In summary, the "immune problem" involves inducing targeted, rapid responses that clear pathogens without excessive inflammation or autoimmunity, while also developing specific, long-lasting immunological memory. The immune system has evolved various mechanisms to achieve this delicate balancing act of protection without self-reactivity.
3
New cards
Explain the origins of the immune systems and cells
The cells of the immune system originate in the bone marrow, where many of them also mature. They then migrate to guard the peripheral tissues, circulating in the blood and in a specialized system of vessels called the lymphatic system.
4
New cards
Compare the differences between Innate and Adaptive immunity
* Innate immunity is the body's first line of defence against pathogens. It is general and non-specific, which means it does not differentiate between types of pathogens. Adaptive immunity is a type of immunity that is built up as we are exposed to diseases or get vaccinated
5
New cards
Understand the phases of an infection and reinfection.
The immune response to an infection follows distinct phases:
__**Initial infection:**__
* Innate immunity activated immediately
* Inflammation, phagocytosis, nonspecific killing
* Signals to recruit and activate adaptive cells
__**Lag phase:**__
* Adaptive immune cells proliferate and differentiate
* Antigen-specific receptors generated
* Immunological memory established
__**Elimination phase:**__
* Pathogen rapidly cleared by expanded adaptive cells
* Antibodies neutralize and mark pathogens for destruction
* Cytotoxic T cells kill infected host cells
__**Resolution phase:**__
* Inflammation resolves, tissue healing begins
* Some memory cells remain for future response
__**Reinfection:**__
* On second exposure, memory cells mount faster, stronger response
* Pathogen-specific antibodies rapidly induced to control infection
* Greatly reduced lag phase due to immunological memory
* Infection cleared before extensive infection/symptoms occur
__**Initial infection:**__
* Innate immunity activated immediately
* Inflammation, phagocytosis, nonspecific killing
* Signals to recruit and activate adaptive cells
__**Lag phase:**__
* Adaptive immune cells proliferate and differentiate
* Antigen-specific receptors generated
* Immunological memory established
__**Elimination phase:**__
* Pathogen rapidly cleared by expanded adaptive cells
* Antibodies neutralize and mark pathogens for destruction
* Cytotoxic T cells kill infected host cells
__**Resolution phase:**__
* Inflammation resolves, tissue healing begins
* Some memory cells remain for future response
__**Reinfection:**__
* On second exposure, memory cells mount faster, stronger response
* Pathogen-specific antibodies rapidly induced to control infection
* Greatly reduced lag phase due to immunological memory
* Infection cleared before extensive infection/symptoms occur
6
New cards
Describe the cells of the innate immune system and their function.
* **Neutrophils:** Phagocytic cells that engulf and destroy bacteria and fungi. Also release antimicrobial proteins and reactive oxygen species. Short-lived cells that quickly recruit to sites of infection.
* **Monocytes:** Circulate in blood and tissues. Differentiate into macrophages and dendritic cells. Can phagocytose pathogens.
* **Macrophages:** Phagocytic cells residing in tissues. Engulf and digest pathogens, dead cells, and debris through phagocytosis. Present antigen on MHC to activate adaptive responses. Secrete inflammatory cytokines.
* **Dendritic cells:** Antigen presenting cells that activate T cell responses. Capture and process antigen, migrate to lymphoid tissues, and present antigen on MHC to T cells.
* **Mast cells:** Release inflammatory mediators like histamine. Involved in allergic responses and anti-parasitic immunity. Help recruit other innate cells like eosinophils.
* **Eosinophils:** Modulate inflammation and fight parasites. Release enzymes toxic to parasites. Help regulate immune responses.
* **Basophils:** Secrete inflammatory mediators during immune responses. Play a role in allergic inflammation and anti-parasitic immunity.
* **Natural killer (NK) cells:** Cytotoxic cells that induce apoptosis of infected or abnormal cells. Important for containing viral infections. Also secrete cytokines like IFN-gamma.
* **Innate lymphoid cells (ILCs):** Rapidly secrete cytokines to stimulate inflammation, fight extracellular parasites, and regulate tissue remodeling. Do not phagocytose.
* **Monocytes:** Circulate in blood and tissues. Differentiate into macrophages and dendritic cells. Can phagocytose pathogens.
* **Macrophages:** Phagocytic cells residing in tissues. Engulf and digest pathogens, dead cells, and debris through phagocytosis. Present antigen on MHC to activate adaptive responses. Secrete inflammatory cytokines.
* **Dendritic cells:** Antigen presenting cells that activate T cell responses. Capture and process antigen, migrate to lymphoid tissues, and present antigen on MHC to T cells.
* **Mast cells:** Release inflammatory mediators like histamine. Involved in allergic responses and anti-parasitic immunity. Help recruit other innate cells like eosinophils.
* **Eosinophils:** Modulate inflammation and fight parasites. Release enzymes toxic to parasites. Help regulate immune responses.
* **Basophils:** Secrete inflammatory mediators during immune responses. Play a role in allergic inflammation and anti-parasitic immunity.
* **Natural killer (NK) cells:** Cytotoxic cells that induce apoptosis of infected or abnormal cells. Important for containing viral infections. Also secrete cytokines like IFN-gamma.
* **Innate lymphoid cells (ILCs):** Rapidly secrete cytokines to stimulate inflammation, fight extracellular parasites, and regulate tissue remodeling. Do not phagocytose.
7
New cards
Describe the barriers to infection and which are covered by the innate arm
* **Anatomic barriers**
* Skin - forms a physical barrier preventing pathogen entry
* Mucosal membranes - epithelial layers protect respiratory, digestive, urogenital tracts
* **Physiologic barriers**
* Temperature - fever responses inhibit microbial growth
* pH - stomach acidity kills ingested microbes
* Normal flora - compete with pathogens for attachment sites
* **Cellular barriers**
* Phagocytes - macrophages, neutrophils, dendritic cells engulf and destroy pathogens
* Natural killer cells - induce apoptosis of infected or abnormal cells
* **Soluble barriers**
* Antimicrobial peptides - defensins, cathelicidins disrupt microbial membranes
* Complement proteins - opsonize pathogens, induce inflammatory responses, directly kill some bacteria
* **Inflammation**
* Vasodilation, increased permeability, immune cell recruitment
* Induced by cytokines, histamine, leukotrienes
* Contains infection and recruits additional innate and adaptive cells
In summary, innate barriers include physical barriers, chemical conditions, cellular components, and soluble factors that provide immediate, nonspecific protection against pathogens.
\
OR
\
The innate immune system includes physical and anatomical barriers as well as effector cells, antimicrobial peptides, soluble mediators, and cell receptors (Table 1). Skin and mucosa provide an effective immune barrier between the internal and external environment.
* Skin - forms a physical barrier preventing pathogen entry
* Mucosal membranes - epithelial layers protect respiratory, digestive, urogenital tracts
* **Physiologic barriers**
* Temperature - fever responses inhibit microbial growth
* pH - stomach acidity kills ingested microbes
* Normal flora - compete with pathogens for attachment sites
* **Cellular barriers**
* Phagocytes - macrophages, neutrophils, dendritic cells engulf and destroy pathogens
* Natural killer cells - induce apoptosis of infected or abnormal cells
* **Soluble barriers**
* Antimicrobial peptides - defensins, cathelicidins disrupt microbial membranes
* Complement proteins - opsonize pathogens, induce inflammatory responses, directly kill some bacteria
* **Inflammation**
* Vasodilation, increased permeability, immune cell recruitment
* Induced by cytokines, histamine, leukotrienes
* Contains infection and recruits additional innate and adaptive cells
In summary, innate barriers include physical barriers, chemical conditions, cellular components, and soluble factors that provide immediate, nonspecific protection against pathogens.
\
OR
\
The innate immune system includes physical and anatomical barriers as well as effector cells, antimicrobial peptides, soluble mediators, and cell receptors (Table 1). Skin and mucosa provide an effective immune barrier between the internal and external environment.
8
New cards
Know the basic principals for sensory cells use to determine if a foreign object is an invader.
* Pattern recognition receptors - Cells express receptors like Toll-like receptors and NOD-like receptors that recognize conserved molecular patterns associated with broad classes of pathogens. Binding to these pathogen-associated molecular patterns (PAMPs) indicates a potential threat.
* Missing self recognition - Natural killer cells detect downregulation of MHC class I molecules on cell surfaces, which can occur when cells are infected by viruses or transformed. Lack of MHC-I flags a cell as abnormal.
* Detection of cell stress and damage - Cells undergoing stress, damage, or necrosis release danger-associated molecular patterns (DAMPs) like ATP and uric acid crystals. DAMPs signal a potential threat or inflammation.
* Opsonization - Complement, antimicrobial peptides, and antibodies coat pathogens and mark them for destruction by phagocytes and other cells. This distinguishes foreign material.
* Physical characteristics - Size, shape, motility, and other morphological characteristics can indicate if an object is likely a pathogen. For example, motile bacteria exhibit different behaviors than host cells.
In summary, innate immune cells rely on recognition of foreign molecular patterns, missing self signals, cell stress markers, opsonization tags, and physical traits to detect and respond to invaders.
* Missing self recognition - Natural killer cells detect downregulation of MHC class I molecules on cell surfaces, which can occur when cells are infected by viruses or transformed. Lack of MHC-I flags a cell as abnormal.
* Detection of cell stress and damage - Cells undergoing stress, damage, or necrosis release danger-associated molecular patterns (DAMPs) like ATP and uric acid crystals. DAMPs signal a potential threat or inflammation.
* Opsonization - Complement, antimicrobial peptides, and antibodies coat pathogens and mark them for destruction by phagocytes and other cells. This distinguishes foreign material.
* Physical characteristics - Size, shape, motility, and other morphological characteristics can indicate if an object is likely a pathogen. For example, motile bacteria exhibit different behaviors than host cells.
In summary, innate immune cells rely on recognition of foreign molecular patterns, missing self signals, cell stress markers, opsonization tags, and physical traits to detect and respond to invaders.
9
New cards
Understand the process that innate cells use for causing inflammation
* Pathogen recognition: Cells like macrophages and dendritic cells express pattern recognition receptors like Toll-like receptors that detect pathogen-associated molecular patterns (PAMPs). This recognition triggers cell activation.
* Cytokine and chemokine secretion: Activated innate cells release pro-inflammatory cytokines like TNF, IL-1, IL-6 and chemokines like CCL2, CXCL8.
* Vasodilation and increased permeability: Cytokines alter endothelial cells of local blood vessels to relax and loosen cell junctions. This allows plasma and leukocytes to enter inflamed tissue.
* Leukocyte recruitment: Chemokines attract neutrophils and monocytes from circulation into inflamed tissue. Signals like complement also recruit cells.
* Cardinal signs of inflammation: Vasodilation and increased blood flow causes redness and heat. Leakage of fluid into tissue leads to swelling. Mediators like histamine stimulate nerve endings causing pain.
* Contain infection: Inflammation provides innate cells access to infected tissue to eliminate pathogens, remove debris, and initiate tissue repair. It also helps activate and recruit adaptive immune cells.
In summary, innate cells recognize pathogens and release inflammatory mediators that induce vascular changes, fluid leakage, and leukocyte infiltration to promote pathogen clearance and activate adaptive immunity.
* Cytokine and chemokine secretion: Activated innate cells release pro-inflammatory cytokines like TNF, IL-1, IL-6 and chemokines like CCL2, CXCL8.
* Vasodilation and increased permeability: Cytokines alter endothelial cells of local blood vessels to relax and loosen cell junctions. This allows plasma and leukocytes to enter inflamed tissue.
* Leukocyte recruitment: Chemokines attract neutrophils and monocytes from circulation into inflamed tissue. Signals like complement also recruit cells.
* Cardinal signs of inflammation: Vasodilation and increased blood flow causes redness and heat. Leakage of fluid into tissue leads to swelling. Mediators like histamine stimulate nerve endings causing pain.
* Contain infection: Inflammation provides innate cells access to infected tissue to eliminate pathogens, remove debris, and initiate tissue repair. It also helps activate and recruit adaptive immune cells.
In summary, innate cells recognize pathogens and release inflammatory mediators that induce vascular changes, fluid leakage, and leukocyte infiltration to promote pathogen clearance and activate adaptive immunity.
10
New cards
Describe the cells of the adaptive immune system and their function.
1. **T Cells:** Helper T cells (CD4+) coordinate immune responses, while cytotoxic T cells (CD8+) directly eliminate infected cells.
2. **B Cells:** These produce antibodies that neutralize pathogens.
3. **APCs**: Dendritic cells and macrophages present antigens to activate T cells.
4. **NK Cells:** They detect and destroy infected or cancerous cells.
11
New cards
Explain how the adaptive immune system adapts to a pathogen.
1. **Recognition:** When the body encounters a new pathogen, antigen-presenting cells (APCs) such as dendritic cells capture and present fragments of the pathogen's antigens to helper T cells. This interaction activates the helper T cells.
2. **Activation of B and T Cells:** Helper T cells release cytokines that stimulate B cells to produce antibodies and cytotoxic T cells to become active. B cells produce antibodies that can bind to the antigens on the pathogen's surface, marking it for destruction. Cytotoxic T cells become capable of directly attacking infected cells.
3. **Clonal Expansion:** Once activated, B cells and cytotoxic T cells undergo clonal expansion, producing a large number of identical cells that are specific to the antigen. This amplifies the immune response.
4. **Effector Phase:** Effector B cells (plasma cells) secrete antibodies, which neutralize pathogens and mark them for removal. Cytotoxic T cells recognize and eliminate infected cells directly.
5. **Memory Formation:** Some of the activated B and T cells differentiate into memory cells. These memory cells "remember" the specific pathogen's antigens. They remain in the body for a long time, providing a rapid and robust response if the same pathogen reappears.
6. **Secondary Response:** In case of re-infection with the same pathogen, memory B and T cells are quickly activated. This results in a faster and more efficient immune response. The pathogen is eliminated before it can cause significant harm.
12
New cards
13
New cards
What are the differences between T-Cell Receptors and Antibodies?
T-cell receptors (TCRs) and antibodies are both crucial components of the adaptive immune system, but they have distinct roles and structures. Here are the key differences between T-cell receptors and antibodies:
%%__1. Structure and Composition:__%%
* **T-Cell Receptors (TCRs):** TCRs are membrane-bound proteins found on the surface of T cells. They consist of two protein chains: alpha and beta chains (in most cases). TCRs have a variable region that can bind to specific antigens.
* **Antibodies:** Antibodies, also known as immunoglobulins, are Y-shaped proteins secreted by B cells and plasma cells. Each antibody has four protein chains: two heavy chains and two light chains. Antibodies have antigen-binding regions that can recognize specific antigens.
%%__2. Binding Targets:__%%
* **TCRs:** TCRs recognize antigens that are presented by major histocompatibility complex (MHC) molecules on the surface of antigen-presenting cells (APCs) or infected cells. TCRs bind to peptide fragments of antigens in the context of MHC molecules.
* **Antibodies:** Antibodies can directly bind to free antigens in the bloodstream or on the surface of pathogens. They can neutralize pathogens, mark them for destruction, and trigger complement activation.
%%*3. Cell Association:*%%
* **TCRs:** TCRs are expressed on the surface of T cells. They play a critical role in T cell activation and response to specific antigens.
* **Antibodies:** Antibodies can be secreted by B cells as soluble proteins or remain anchored to the surface of B cells. They are essential for humoral immune responses.
%%__**4. Effector Functions:**__%%
* **TCRs:** TCRs on cytotoxic T cells (CD8+ T cells) recognize antigens on infected cells and trigger their destruction through direct cell-to-cell contact.
* **Antibodies:** Antibodies can neutralize pathogens, enhance phagocytosis by macrophages, activate complement proteins to destroy pathogens, and facilitate antibody-dependent cellular cytotoxicity (ADCC).
%%__**5. Diversity Generation:**__%%
* **TCRs:** TCR diversity is generated through gene rearrangement of the TCR genes in T cells. This generates a diverse repertoire of T cells, each capable of recognizing a specific antigen.
* **Antibodies:** Antibody diversity is created through gene rearrangement of antibody genes during B cell development, resulting in a vast array of B cells, each producing antibodies with unique antigen-binding sites.
%%__**6. Role in Immune Response:**__%%
* **TCRs:** TCRs play a central role in cell-mediated immunity, coordinating responses against intracellular pathogens and abnormal cells.
* **Antibodies:** Antibodies are a key component of humoral immunity, defending against extracellular pathogens and toxins.
%%__1. Structure and Composition:__%%
* **T-Cell Receptors (TCRs):** TCRs are membrane-bound proteins found on the surface of T cells. They consist of two protein chains: alpha and beta chains (in most cases). TCRs have a variable region that can bind to specific antigens.
* **Antibodies:** Antibodies, also known as immunoglobulins, are Y-shaped proteins secreted by B cells and plasma cells. Each antibody has four protein chains: two heavy chains and two light chains. Antibodies have antigen-binding regions that can recognize specific antigens.
%%__2. Binding Targets:__%%
* **TCRs:** TCRs recognize antigens that are presented by major histocompatibility complex (MHC) molecules on the surface of antigen-presenting cells (APCs) or infected cells. TCRs bind to peptide fragments of antigens in the context of MHC molecules.
* **Antibodies:** Antibodies can directly bind to free antigens in the bloodstream or on the surface of pathogens. They can neutralize pathogens, mark them for destruction, and trigger complement activation.
%%*3. Cell Association:*%%
* **TCRs:** TCRs are expressed on the surface of T cells. They play a critical role in T cell activation and response to specific antigens.
* **Antibodies:** Antibodies can be secreted by B cells as soluble proteins or remain anchored to the surface of B cells. They are essential for humoral immune responses.
%%__**4. Effector Functions:**__%%
* **TCRs:** TCRs on cytotoxic T cells (CD8+ T cells) recognize antigens on infected cells and trigger their destruction through direct cell-to-cell contact.
* **Antibodies:** Antibodies can neutralize pathogens, enhance phagocytosis by macrophages, activate complement proteins to destroy pathogens, and facilitate antibody-dependent cellular cytotoxicity (ADCC).
%%__**5. Diversity Generation:**__%%
* **TCRs:** TCR diversity is generated through gene rearrangement of the TCR genes in T cells. This generates a diverse repertoire of T cells, each capable of recognizing a specific antigen.
* **Antibodies:** Antibody diversity is created through gene rearrangement of antibody genes during B cell development, resulting in a vast array of B cells, each producing antibodies with unique antigen-binding sites.
%%__**6. Role in Immune Response:**__%%
* **TCRs:** TCRs play a central role in cell-mediated immunity, coordinating responses against intracellular pathogens and abnormal cells.
* **Antibodies:** Antibodies are a key component of humoral immunity, defending against extracellular pathogens and toxins.
14
New cards
Describe the five classes of antibodies and their different functions
\
1. %%__IgM (Immunoglobulin M):__%%
* **Structure:** IgM is the largest antibody, existing primarily as a pentamer (five units) held together by a "J chain."
* **Function:** IgM is the first antibody produced during an initial immune response to a new antigen. It is efficient at agglutinating (clumping together) pathogens and activating complement proteins. It is particularly effective against pathogens in the bloodstream.
2. %%__IgG (Immunoglobulin G):__%%
* **Structure:** IgG is the most abundant antibody in the blood and tissues. It has a Y-shaped structure with two heavy chains and two light chains.
* **Function:** IgG provides long-term protection against infections. It can neutralize pathogens, enhance phagocytosis by macrophages, activate complement, and cross the placenta to provide passive immunity to the fetus.
3. %%__**IgA (Immunoglobulin A):**__%%
* **Structure:** IgA exists in two main forms: secretory IgA (sIgA) found in bodily secretions like saliva, tears, and mucous membranes, and serum IgA found in the bloodstream.
* **Function:** IgA is primarily associated with mucosal immunity. sIgA helps prevent pathogens from attaching to mucosal surfaces and entering the body. It's particularly important in protecting areas exposed to the external environment.
4. %%__**IgE (Immunoglobulin E):**__%%
* **Structure:** IgE has a unique structure with high affinity for certain receptors on mast cells and basophils.
* **Function:** IgE is involved in allergic responses and defense against parasitic infections. When bound to mast cells and basophils, IgE triggers the release of histamines and other chemicals during allergic reactions.
5. %%__**IgD (Immunoglobulin D):**__%%
* **Structure:** IgD is found in small amounts on the surface of B cells.
* **Function:** The precise function of IgD is still being studied, but it's believed to play a role in the activation and regulation of B cells.
1. %%__IgM (Immunoglobulin M):__%%
* **Structure:** IgM is the largest antibody, existing primarily as a pentamer (five units) held together by a "J chain."
* **Function:** IgM is the first antibody produced during an initial immune response to a new antigen. It is efficient at agglutinating (clumping together) pathogens and activating complement proteins. It is particularly effective against pathogens in the bloodstream.
2. %%__IgG (Immunoglobulin G):__%%
* **Structure:** IgG is the most abundant antibody in the blood and tissues. It has a Y-shaped structure with two heavy chains and two light chains.
* **Function:** IgG provides long-term protection against infections. It can neutralize pathogens, enhance phagocytosis by macrophages, activate complement, and cross the placenta to provide passive immunity to the fetus.
3. %%__**IgA (Immunoglobulin A):**__%%
* **Structure:** IgA exists in two main forms: secretory IgA (sIgA) found in bodily secretions like saliva, tears, and mucous membranes, and serum IgA found in the bloodstream.
* **Function:** IgA is primarily associated with mucosal immunity. sIgA helps prevent pathogens from attaching to mucosal surfaces and entering the body. It's particularly important in protecting areas exposed to the external environment.
4. %%__**IgE (Immunoglobulin E):**__%%
* **Structure:** IgE has a unique structure with high affinity for certain receptors on mast cells and basophils.
* **Function:** IgE is involved in allergic responses and defense against parasitic infections. When bound to mast cells and basophils, IgE triggers the release of histamines and other chemicals during allergic reactions.
5. %%__**IgD (Immunoglobulin D):**__%%
* **Structure:** IgD is found in small amounts on the surface of B cells.
* **Function:** The precise function of IgD is still being studied, but it's believed to play a role in the activation and regulation of B cells.
15
New cards
Know the primary and secondary organs of the Immune system.
\n The immune system consists of various primary and secondary organs that work together to defend the body against infections and maintain overall health. These organs play distinct roles in immune cell development, maturation, activation, and coordination of immune responses. Here's a breakdown of the primary and secondary organs of the immune system:
%%__**Primary Organs:**__%%
1. Bone Marrow:
* **Function:** Bone marrow is the site of hematopoiesis, where all blood cells, including immune cells like B cells, mature. It is crucial for the production and maturation of immune cells.
2. Thymus:
* **Function:** The thymus is essential for the development and maturation of T cells. Immature T cells produced in the bone marrow migrate to the thymus to undergo selection processes that ensure they recognize antigens without attacking the body's own tissues.
%%**Secondary Organs:**%%
1. Spleen:
* **Function:** The spleen filters blood, removing damaged red blood cells and pathogens. It is also a site of immune cell interactions. B cells and T cells can encounter antigens here, leading to immune responses.
2. Lymph Nodes:
* **Function:** Lymph nodes are distributed throughout the body and serve as hubs for immune cell communication. They filter lymph (a fluid containing immune cells and antigens) and facilitate interactions between immune cells, promoting effective immune responses.
3. Tonsils and Adenoids:
* **Function:** Tonsils and adenoids are clusters of lymphoid tissue in the throat. They help trap pathogens entering the body through the mouth and nose, initiating immune responses.
4. Peyer's Patches and Appendix:
* **Function:** Peyer's patches are found in the lining of the small intestine, and the appendix is an extension of the large intestine. Both contain lymphoid tissue and contribute to the surveillance of the digestive system for pathogens.
5. Mucosa-Associated Lymphoid Tissue (MALT):
* **Function:** MALT is a collection of immune cells and tissues found in mucous membranes throughout the body, such as the respiratory and gastrointestinal tracts. MALT defends against pathogens entering through these surfaces.
6. GALT (Gut-Associated Lymphoid Tissue):
* **Function:** GALT is a type of MALT specifically located in the intestines. It monitors and responds to antigens from ingested food and pathogens.
7. Bronchus-Associated Lymphoid Tissue (BALT):
* **Function:** BALT is a type of MALT in the respiratory tract. It plays a role in immune defense against respiratory infections.
These primary and secondary organs of the immune system work together to ensure immune cell development, activation, and coordination throughout the body. The immune response is a complex interplay between these organs, allowing the body to effectively combat infections and maintain overall health.
%%__**Primary Organs:**__%%
1. Bone Marrow:
* **Function:** Bone marrow is the site of hematopoiesis, where all blood cells, including immune cells like B cells, mature. It is crucial for the production and maturation of immune cells.
2. Thymus:
* **Function:** The thymus is essential for the development and maturation of T cells. Immature T cells produced in the bone marrow migrate to the thymus to undergo selection processes that ensure they recognize antigens without attacking the body's own tissues.
%%**Secondary Organs:**%%
1. Spleen:
* **Function:** The spleen filters blood, removing damaged red blood cells and pathogens. It is also a site of immune cell interactions. B cells and T cells can encounter antigens here, leading to immune responses.
2. Lymph Nodes:
* **Function:** Lymph nodes are distributed throughout the body and serve as hubs for immune cell communication. They filter lymph (a fluid containing immune cells and antigens) and facilitate interactions between immune cells, promoting effective immune responses.
3. Tonsils and Adenoids:
* **Function:** Tonsils and adenoids are clusters of lymphoid tissue in the throat. They help trap pathogens entering the body through the mouth and nose, initiating immune responses.
4. Peyer's Patches and Appendix:
* **Function:** Peyer's patches are found in the lining of the small intestine, and the appendix is an extension of the large intestine. Both contain lymphoid tissue and contribute to the surveillance of the digestive system for pathogens.
5. Mucosa-Associated Lymphoid Tissue (MALT):
* **Function:** MALT is a collection of immune cells and tissues found in mucous membranes throughout the body, such as the respiratory and gastrointestinal tracts. MALT defends against pathogens entering through these surfaces.
6. GALT (Gut-Associated Lymphoid Tissue):
* **Function:** GALT is a type of MALT specifically located in the intestines. It monitors and responds to antigens from ingested food and pathogens.
7. Bronchus-Associated Lymphoid Tissue (BALT):
* **Function:** BALT is a type of MALT in the respiratory tract. It plays a role in immune defense against respiratory infections.
These primary and secondary organs of the immune system work together to ensure immune cell development, activation, and coordination throughout the body. The immune response is a complex interplay between these organs, allowing the body to effectively combat infections and maintain overall health.
16
New cards
Understand the differences and mechanism of primary vs secondary response
The primary immune response occurs after the first exposure to an antigen. A primary immune response results in the generation of memory immune cells. A secondary immune response occurs as a result of a second exposure to an antigen.
17
New cards
Relate how the clonal hypothesis describes how the adaptive immune system functions.
The clonal selection of lymphocytes provides a theoretical framework for understanding all the key features of adaptive immunity. Each lymphocyte carries cell-surface receptors of a single specificity, generated by the random recombination of variable receptor gene segments and the pairing of different variable chains.
18
New cards
19
New cards
Describe how the Innate immune responses can select from several effector modules to protect against different types of pathogens.
The innate immune system consists of functionally distinct 'modules' that evolved to provide different forms of protection against pathogens. It senses pathogens through pattern-recognition receptors, which trigger the activation of antimicrobial defences and stimulate the adaptive immune response.
20
New cards
How do Antibodies protect against extracellular pathogens and their toxic products.
The simplest and most direct way in which antibodies can protect from pathogens or their toxic products is by binding to them and thereby blocking their access to cells that they might infect or destroy
21
New cards
Explain how T cells orchestrate cell-mediated immunity and regulate B-cell responses to most antigens.
TH1 cells activate the microbicidal properties of macrophages, and induce B cells to make IgG antibodies that are very effective at opsonizing extracellular pathogens for uptake by phagocytic cells. TH2 cells initiate the humoral immune response by activating naive antigen-specific B cells to produce IgM antibodies.
\
In summary, T cells orchestrate cell-mediated immune responses by directly eliminating infected cells and assisting other immune cells. They also regulate B-cell responses by providing necessary signals for optimal antibody production, affinity maturation, and isotype switching. This intricate coordination ensures an effective immune response while preventing unnecessary inflammation and immune-related disorders.
\
\
In summary, T cells orchestrate cell-mediated immune responses by directly eliminating infected cells and assisting other immune cells. They also regulate B-cell responses by providing necessary signals for optimal antibody production, affinity maturation, and isotype switching. This intricate coordination ensures an effective immune response while preventing unnecessary inflammation and immune-related disorders.
\
22
New cards
Understand how Inherited and acquired defects in the immune system result in increased susceptibility to infection.
both inherited and acquired defects in the immune system can lead to increased susceptibility to infections. These defects can affect different components of the immune response, weakening the body's ability to defend against pathogens. Early detection, appropriate medical management, and preventive measures are crucial to mitigate the impact of immunodeficiencies on individuals' health.
23
New cards
Understand why adaptive immune responses is important for the control of allergies, autoimmune disease, and the rejection of transplanted organs.
The adaptive immune response plays a crucial role in controlling allergies, autoimmune diseases, and the rejection of transplanted organs. Its intricate regulatory mechanisms and ability to differentiate between self and non-self antigens are pivotal in maintaining the overall health of the body. Here's how the adaptive immune response contributes to each of these scenarios:
%%__**1. Control of Allergies:**__%% Allergies are hypersensitive immune responses to harmless substances, or allergens, such as pollen, dust mites, or certain foods. The adaptive immune response is involved in the development of allergic reactions.
* **Role of T Helper Cells:** In allergic reactions, a specific type of T helper cell (Th2) becomes overactive. Th2 cells produce cytokines that promote antibody production of the IgE class.
* **IgE Antibodies:** These IgE antibodies bind to allergens and trigger the release of histamines from mast cells and basophils, leading to allergy symptoms like itching, swelling, and difficulty breathing.
* **Regulatory T Cells (Tregs):** Tregs play a role in dampening immune responses and maintaining immune tolerance. In allergic individuals, the balance between Th2 cells and Tregs may be disrupted, leading to exaggerated responses.
%%__**2. Control of Autoimmune Diseases:**__%% Autoimmune diseases occur when the immune system mistakenly attacks the body's own tissues. The adaptive immune response plays a role in regulating self-tolerance and preventing autoimmune reactions.
* **Central Tolerance:** During T cell development in the thymus and B cell development in the bone marrow, cells with receptors that strongly recognize self-antigens are eliminated or inactivated, preventing autoimmune responses.
* **Peripheral Tolerance:** Regulatory T cells (Tregs) help suppress self-reactive immune cells in the periphery, preventing autoimmune reactions.
%%__**3. Rejection of Transplanted Organs:**__%% Transplanted organs are recognized as foreign by the recipient's immune system, leading to an immune response that can result in rejection.
* **Direct and Indirect Recognition:** T cells recognize donor antigens on transplanted organs. Direct recognition involves T cells recognizing donor MHC molecules directly. Indirect recognition occurs when recipient T cells recognize processed donor antigens presented on self-MHC molecules.
* **Cell-Mediated Immunity:** Cytotoxic T cells (CD8+ T cells) can directly attack transplanted cells, leading to cell-mediated rejection.
* **Humoral Immunity:** B cells can produce antibodies against antigens on transplanted organs, contributing to antibody-mediated rejection.
* I**mmunosuppressive Drugs:** To prevent rejection, recipients of transplants often need immunosuppressive drugs that dampen the adaptive immune response. These drugs can lower the body's ability to respond to infections, making patients more susceptible to diseases.
In summary, the adaptive immune response's ability to discriminate between self and non-self antigens is essential for maintaining immune tolerance and preventing harmful reactions such as allergies, autoimmune diseases, and the rejection of transplanted organs. Understanding and modulating the adaptive immune response are central to managing these conditions and maintaining overall immune health.
%%__**1. Control of Allergies:**__%% Allergies are hypersensitive immune responses to harmless substances, or allergens, such as pollen, dust mites, or certain foods. The adaptive immune response is involved in the development of allergic reactions.
* **Role of T Helper Cells:** In allergic reactions, a specific type of T helper cell (Th2) becomes overactive. Th2 cells produce cytokines that promote antibody production of the IgE class.
* **IgE Antibodies:** These IgE antibodies bind to allergens and trigger the release of histamines from mast cells and basophils, leading to allergy symptoms like itching, swelling, and difficulty breathing.
* **Regulatory T Cells (Tregs):** Tregs play a role in dampening immune responses and maintaining immune tolerance. In allergic individuals, the balance between Th2 cells and Tregs may be disrupted, leading to exaggerated responses.
%%__**2. Control of Autoimmune Diseases:**__%% Autoimmune diseases occur when the immune system mistakenly attacks the body's own tissues. The adaptive immune response plays a role in regulating self-tolerance and preventing autoimmune reactions.
* **Central Tolerance:** During T cell development in the thymus and B cell development in the bone marrow, cells with receptors that strongly recognize self-antigens are eliminated or inactivated, preventing autoimmune responses.
* **Peripheral Tolerance:** Regulatory T cells (Tregs) help suppress self-reactive immune cells in the periphery, preventing autoimmune reactions.
%%__**3. Rejection of Transplanted Organs:**__%% Transplanted organs are recognized as foreign by the recipient's immune system, leading to an immune response that can result in rejection.
* **Direct and Indirect Recognition:** T cells recognize donor antigens on transplanted organs. Direct recognition involves T cells recognizing donor MHC molecules directly. Indirect recognition occurs when recipient T cells recognize processed donor antigens presented on self-MHC molecules.
* **Cell-Mediated Immunity:** Cytotoxic T cells (CD8+ T cells) can directly attack transplanted cells, leading to cell-mediated rejection.
* **Humoral Immunity:** B cells can produce antibodies against antigens on transplanted organs, contributing to antibody-mediated rejection.
* I**mmunosuppressive Drugs:** To prevent rejection, recipients of transplants often need immunosuppressive drugs that dampen the adaptive immune response. These drugs can lower the body's ability to respond to infections, making patients more susceptible to diseases.
In summary, the adaptive immune response's ability to discriminate between self and non-self antigens is essential for maintaining immune tolerance and preventing harmful reactions such as allergies, autoimmune diseases, and the rejection of transplanted organs. Understanding and modulating the adaptive immune response are central to managing these conditions and maintaining overall immune health.
24
New cards
Explain how vaccination is the most effective means of controlling infectious diseases.
\
Vaccination is the most effective means of controlling infectious diseases because it harnesses the power of the immune system to prevent and manage infections. By introducing weakened or inactivated forms of pathogens or their components into the body, vaccines stimulate the immune response without causing illness. This preparation equips the immune system to recognize and defend against the actual pathogen in case of future exposure. Here's how vaccination works and why it's so effective:
****1. Priming the Immune System:**
Vaccines contain antigens from pathogens that mimic those found on the actual pathogens. When the vaccine is administered, the immune system recognizes these antigens as foreign and mounts an immune response.
****2. Activation of Immune Responses:**
The immune response triggered by vaccines involves both the innate and adaptive immune systems. Immune cells such as dendritic cells present vaccine antigens to T cells and B cells, initiating a specific immune reaction.
****3. Generation of Memory Cells:**
During the immune response, memory B cells and memory T cells are formed. These cells "remember" the specific antigens from the vaccine. This memory provides rapid and robust responses if the person is later exposed to the actual pathogen.
****4. Quick and Effective Response to Infections:**
If a vaccinated individual encounters the real pathogen, memory cells are quickly activated. Antibodies and immune cells target and neutralize the pathogen before it can cause illness. This rapid response often prevents the disease from developing or reduces its severity.
****5. Herd Immunity:**
When a significant portion of a population is vaccinated against a disease, the spread of the pathogen is limited. This protects individuals who cannot be vaccinated due to medical reasons, indirectly reducing disease transmission and outbreaks.
****6. Eradication of Diseases:**
Vaccination has led to the successful eradication of smallpox and the near-elimination of diseases like polio and measles in many parts of the world. This demonstrates the powerful impact of widespread vaccination.
****7. Safe and Cost-Effective:**
Vaccines undergo rigorous testing for safety and efficacy before approval. They are generally safer than the diseases they prevent. Moreover, the economic burden of treating diseases and their complications is far greater than the cost of vaccination programs.
****8. Preventing Outbreaks:**
Vaccination helps prevent outbreaks of contagious diseases that can spread rapidly in communities. Diseases like measles, mumps, and pertussis can be controlled through high vaccination coverage.
In summary, vaccination is a proactive and effective strategy for controlling infectious diseases. It prepares the immune system to recognize and respond to pathogens before they cause illness, ultimately reducing disease burden, preventing outbreaks, and safeguarding public health.
Vaccination is the most effective means of controlling infectious diseases because it harnesses the power of the immune system to prevent and manage infections. By introducing weakened or inactivated forms of pathogens or their components into the body, vaccines stimulate the immune response without causing illness. This preparation equips the immune system to recognize and defend against the actual pathogen in case of future exposure. Here's how vaccination works and why it's so effective:
****1. Priming the Immune System:**
Vaccines contain antigens from pathogens that mimic those found on the actual pathogens. When the vaccine is administered, the immune system recognizes these antigens as foreign and mounts an immune response.
****2. Activation of Immune Responses:**
The immune response triggered by vaccines involves both the innate and adaptive immune systems. Immune cells such as dendritic cells present vaccine antigens to T cells and B cells, initiating a specific immune reaction.
****3. Generation of Memory Cells:**
During the immune response, memory B cells and memory T cells are formed. These cells "remember" the specific antigens from the vaccine. This memory provides rapid and robust responses if the person is later exposed to the actual pathogen.
****4. Quick and Effective Response to Infections:**
If a vaccinated individual encounters the real pathogen, memory cells are quickly activated. Antibodies and immune cells target and neutralize the pathogen before it can cause illness. This rapid response often prevents the disease from developing or reduces its severity.
****5. Herd Immunity:**
When a significant portion of a population is vaccinated against a disease, the spread of the pathogen is limited. This protects individuals who cannot be vaccinated due to medical reasons, indirectly reducing disease transmission and outbreaks.
****6. Eradication of Diseases:**
Vaccination has led to the successful eradication of smallpox and the near-elimination of diseases like polio and measles in many parts of the world. This demonstrates the powerful impact of widespread vaccination.
****7. Safe and Cost-Effective:**
Vaccines undergo rigorous testing for safety and efficacy before approval. They are generally safer than the diseases they prevent. Moreover, the economic burden of treating diseases and their complications is far greater than the cost of vaccination programs.
****8. Preventing Outbreaks:**
Vaccination helps prevent outbreaks of contagious diseases that can spread rapidly in communities. Diseases like measles, mumps, and pertussis can be controlled through high vaccination coverage.
In summary, vaccination is a proactive and effective strategy for controlling infectious diseases. It prepares the immune system to recognize and respond to pathogens before they cause illness, ultimately reducing disease burden, preventing outbreaks, and safeguarding public health.
25
New cards
Which of the following examples can be considered an illustration of vaccination?
\
A. An individual that becomes ill with chickenpox, but does not develop it again due to the development of immunological memory
B. Administering the serum of animals immune to diphtheria to protect against the effects of diphtheria toxin in and exposed individual
\
C. A bacterial infection that results in complement activation and destruction of the pathogen
\
D. Inoculating an individual with cowpox in order to protect that individual against smallpox
D. Inoculating an individual with cowpox in order to protect that individual against smallpox
26
New cards
Classify the following as lymphoid or myeloid in origin
* **Eosinophils :** Myeloid
* **B Cells:** Lymphoid
* **Neutrophils:** Myeloid
* **NK Cells:** Lymphoid
* **Mast Cells:** Myeloid
* **Macrophages:** Myeloid
* **ILC’s:** Lymphoid
* **Red Blood Cells:** Myeloid
27
New cards
Which of the following are part of the innate immune system?
A. Endothelial cells
B. Red blood cells
C. Granulocytes
D. Macrophages
E. Lymphocytes
\
A. Endothelial cells
C. Granulocytes
D. Macrophages
E. Lymphocytes
\
C. Granulocytes
D. Macrophages
E. Lymphocytes
\
28
New cards
Which of the following support a microbiome?
A. The stomach
B. The skin
C. The small intestine
D. The cornea of the eye
E. The mouth
F. The inner Ear
G. The large Intestine
B. The skin
C. The small intestine
E. The mouth
G. The large Intestine
C. The small intestine
E. The mouth
G. The large Intestine
29
New cards
Which of the following cause pores in a pathogen to kill them?
A. RegIII
B. MAC
C. Lysozyme
D. Defensin
A. RegIII
B. MAC
D. Defensin
B. MAC
D. Defensin
30
New cards
Which of the following are part of our anatomical barrier that protects us from infection?
A. Bacteria living on the surface of our skin
B. The electrical charge of our epithelial cells
C. Soap residue left over from when we wash
D. Tight junctions in our epithelium
A. Bacteria living on the surface of our skin
D. Tight junctions in our epithelium
D. Tight junctions in our epithelium
31
New cards
What are the common routes of infection and what type of pathogen exploit these routes?
1. **Respiratory Route:**
* Pathogens: Viruses (e.g., influenza, SARS-CoV-2), bacteria (e.g., Streptococcus pneumoniae).
* Entry: Inhaled airborne droplets containing pathogens.
* Target: Respiratory tract (nose, throat, lungs).
2. **Gastrointestinal (GI) Route:**
* Pathogens: Bacteria (e.g., Salmonella, Escherichia coli), viruses (e.g., norovirus, rotavirus).
* Entry: Ingestion of contaminated food, water, or surfaces.
* Target: GI tract (stomach, intestines).
3. **Fecal-Oral Route:**
* Pathogens: Bacteria (e.g., Vibrio cholerae), viruses (e.g., hepatitis A).
* Entry: Ingestion of water or food contaminated with fecal matter.
* Target: GI tract.
4. **Direct Contact:**
* Pathogens: Bacteria (e.g., Staphylococcus aureus), viruses (e.g., herpes simplex virus).
* Entry: Physical contact between infected and susceptible individuals.
* Target: Skin and mucous membranes.
5. **Bloodborne Route:**
* Pathogens: Viruses (e.g., HIV, hepatitis B), bacteria (e.g., Treponema pallidum causing syphilis).
* Entry: Contaminated blood or blood products entering the bloodstream.
* Target: Blood cells and various organs.
6. **Vector-Borne Route:**
* Pathogens: Parasites (e.g., Plasmodium causing malaria), bacteria (e.g., Borrelia burgdorferi causing Lyme disease).
* Entry: Transfer through bites of arthropod vectors like mosquitoes, ticks, or fleas.
* Target: Varies depending on the pathogen.
7. **Vertical Transmission:**
* Pathogens: Viruses (e.g., rubella), bacteria (e.g., group B Streptococcus).
* Entry: Transmission from mother to offspring during pregnancy, childbirth, or breastfeeding.
* Target: Neonates and developing fetuses.
8. **Urogenital Route:**
* Pathogens: Bacteria (e.g., Neisseria gonorrhoeae), viruses (e.g., herpes simplex virus).
* Entry: Contact with infected genital, urinary, or reproductive tissues or fluids.
* Target: Genital and urinary tracts.
9. **Zoonotic Route:**
* Pathogens: Varied (e.g., avian influenza, rabies, Ebola virus).
* Entry: Transmission from animals to humans through direct contact, consumption, or environmental exposure.
* Target: Varies depending on the pathogen.
10. **Mucosal Route:**
* Pathogens: Various pathogens exploiting different routes (respiratory, gastrointestinal, urogenital).
* Entry: Invasion through mucosal surfaces lining respiratory, digestive, or reproductive tracts.
* Target: Mucosal tissues and associated systems.
32
New cards
What is the difference between an extracellular and an intracellular pathogen?
Extracellular pathogens remain outside host cells, easier to target directly. Intracellular pathogens survive inside host cells, harder to eliminate without collateral da
33
New cards
Where does tissue damage stem from in an infection?
Tissue damage stems from pathogen toxins/replication and immune response inflammation/cytotoxicity.
\
__Tissue Damage in Infection:__
* **Pathogen Activity:** Many pathogens, such as bacteria, viruses, and parasites, can directly damage host tissues as part of their life cycle. For example, bacteria may produce toxins that harm surrounding cells, viruses can destroy host cells during replication, and parasites can cause physical damage as they feed or move within tissues.
* **Inflammatory Response:** The host's immune response triggers inflammation to combat the infection. While inflammation is essential for defense, excessive or prolonged inflammation can lead to collateral damage to healthy tissues.
* **Immune Cell Activity:** Immune cells, such as neutrophils and macrophages, are recruited to sites of infection. While they aim to eliminate pathogens, their aggressive actions can inadvertently damage nearby tissues.
* **Cytokine Storms:** In severe infections, an excessive release of cytokines (cytokine storm) by immune cells can lead to systemic inflammation and tissue damage.
* **Immune Complexes:** In some cases, immune complexes (antigen-antibody complexes) can accumulate in tissues, triggering inflammation and damage.
* **Secondary Infections:** Weakened tissues can become susceptible to secondary infections by opportunistic pathogens, exacerbating tissue damage.
\
__Tissue Damage in Infection:__
* **Pathogen Activity:** Many pathogens, such as bacteria, viruses, and parasites, can directly damage host tissues as part of their life cycle. For example, bacteria may produce toxins that harm surrounding cells, viruses can destroy host cells during replication, and parasites can cause physical damage as they feed or move within tissues.
* **Inflammatory Response:** The host's immune response triggers inflammation to combat the infection. While inflammation is essential for defense, excessive or prolonged inflammation can lead to collateral damage to healthy tissues.
* **Immune Cell Activity:** Immune cells, such as neutrophils and macrophages, are recruited to sites of infection. While they aim to eliminate pathogens, their aggressive actions can inadvertently damage nearby tissues.
* **Cytokine Storms:** In severe infections, an excessive release of cytokines (cytokine storm) by immune cells can lead to systemic inflammation and tissue damage.
* **Immune Complexes:** In some cases, immune complexes (antigen-antibody complexes) can accumulate in tissues, triggering inflammation and damage.
* **Secondary Infections:** Weakened tissues can become susceptible to secondary infections by opportunistic pathogens, exacerbating tissue damage.
34
New cards
Explain the physical and chemical barriers of the body by location.
__**Physical barriers:**__ Skin, mucus, ciliated epithelium.
__**Chemical barriers:**__ Stomach acidity, antimicrobial peptides, normal flora.
\
**Physical Barriers:**
1. **Skin:**
* Location: Outermost layer of the body.
* Explanation: The skin acts as a physical barrier, preventing the entry of pathogens. The outermost layer, the stratum corneum, consists of dead skin cells and keratin, making it difficult for microorganisms to penetrate.
2. **Mucous Membranes:**
* Location: Found in the respiratory, gastrointestinal, urogenital, and ocular tracts.
* Explanation: Mucous membranes secrete mucus, a sticky fluid that traps pathogens. For example, the respiratory tract has cilia that move mucus and trapped pathogens away from the lungs.
Chemical Barriers:
1. **Stomach Acid:**
* Location: Stomach.
* Explanation: The stomach produces hydrochloric acid that helps to destroy ingested pathogens by creating an acidic environment that is harmful to many microorganisms.
2. **Enzymes:**
* Location: Throughout the body, including the digestive system and mucous membranes.
* Explanation: Enzymes like lysozyme are present in bodily fluids like saliva, tears, and mucous secretions. Lysozyme breaks down bacterial cell walls, preventing infection.
3. **Defensins:**
* Location: Various mucous membranes and body fluids.
* Explanation: Defensins are antimicrobial peptides that attack the membranes of pathogens, disrupting their integrity and killing them.
4. **Sebum:**
* Location: Skin's sebaceous glands.
* Explanation: Sebum is an oily substance produced by sebaceous glands that helps keep the skin moisturized and forms a protective barrier against certain pathogens.
5. **Sweat:**
* Location: Sweat glands in the skin.
* Explanation: Sweat contains antimicrobial peptides that inhibit the growth of certain bacteria on the skin's surface.
__**Chemical barriers:**__ Stomach acidity, antimicrobial peptides, normal flora.
\
**Physical Barriers:**
1. **Skin:**
* Location: Outermost layer of the body.
* Explanation: The skin acts as a physical barrier, preventing the entry of pathogens. The outermost layer, the stratum corneum, consists of dead skin cells and keratin, making it difficult for microorganisms to penetrate.
2. **Mucous Membranes:**
* Location: Found in the respiratory, gastrointestinal, urogenital, and ocular tracts.
* Explanation: Mucous membranes secrete mucus, a sticky fluid that traps pathogens. For example, the respiratory tract has cilia that move mucus and trapped pathogens away from the lungs.
Chemical Barriers:
1. **Stomach Acid:**
* Location: Stomach.
* Explanation: The stomach produces hydrochloric acid that helps to destroy ingested pathogens by creating an acidic environment that is harmful to many microorganisms.
2. **Enzymes:**
* Location: Throughout the body, including the digestive system and mucous membranes.
* Explanation: Enzymes like lysozyme are present in bodily fluids like saliva, tears, and mucous secretions. Lysozyme breaks down bacterial cell walls, preventing infection.
3. **Defensins:**
* Location: Various mucous membranes and body fluids.
* Explanation: Defensins are antimicrobial peptides that attack the membranes of pathogens, disrupting their integrity and killing them.
4. **Sebum:**
* Location: Skin's sebaceous glands.
* Explanation: Sebum is an oily substance produced by sebaceous glands that helps keep the skin moisturized and forms a protective barrier against certain pathogens.
5. **Sweat:**
* Location: Sweat glands in the skin.
* Explanation: Sweat contains antimicrobial peptides that inhibit the growth of certain bacteria on the skin's surface.
35
New cards
How does the microbiome contribute to host defense?
Microbiome competes with pathogens for attachment/nutrients, stimulates innate immunity through PAMPs. Disruption increases susceptibility.
\
* **Competitive Exclusion:** The microbiome occupies various niches in and on the body, preventing the colonization of potentially harmful pathogens. This phenomenon is known as competitive exclusion, where beneficial microbes outcompete pathogens for resources.
* **Nutrient Competition:** Beneficial microbes in the microbiome consume available nutrients, limiting the resources available to pathogens and hindering their growth.
* **pH Regulation:** Microbes can produce acids that help maintain a slightly acidic environment, discouraging the growth of certain pathogens that thrive in alkaline conditions.
* **Immune System Education:** The microbiome interacts with the host's immune system, aiding in its development and education. Exposure to diverse microbes helps train the immune system to differentiate between harmless and harmful entities.
* **Barrier Reinforcement:** The microbiome contributes to the maintenance of skin and mucosal barrier integrity, preventing pathogens from entering the body.
* **Production of Antimicrobial Compounds:** Some microbes in the microbiome produce antimicrobial compounds that help inhibit the growth of pathogenic microorganisms.
* **Metabolite Production:** Microbes in the gut microbiome can metabolize dietary compounds into bioactive molecules that influence the immune system and contribute to host defense.
* **Pathogen Suppression:** Some microbes produce substances that directly inhibit the growth of pathogens, providing protection against infections.
* **Modulation of Inflammation:** The microbiome can influence the immune system's response, helping to maintain an appropriate balance between inflammation and immune regulation.
\
* **Competitive Exclusion:** The microbiome occupies various niches in and on the body, preventing the colonization of potentially harmful pathogens. This phenomenon is known as competitive exclusion, where beneficial microbes outcompete pathogens for resources.
* **Nutrient Competition:** Beneficial microbes in the microbiome consume available nutrients, limiting the resources available to pathogens and hindering their growth.
* **pH Regulation:** Microbes can produce acids that help maintain a slightly acidic environment, discouraging the growth of certain pathogens that thrive in alkaline conditions.
* **Immune System Education:** The microbiome interacts with the host's immune system, aiding in its development and education. Exposure to diverse microbes helps train the immune system to differentiate between harmless and harmful entities.
* **Barrier Reinforcement:** The microbiome contributes to the maintenance of skin and mucosal barrier integrity, preventing pathogens from entering the body.
* **Production of Antimicrobial Compounds:** Some microbes in the microbiome produce antimicrobial compounds that help inhibit the growth of pathogenic microorganisms.
* **Metabolite Production:** Microbes in the gut microbiome can metabolize dietary compounds into bioactive molecules that influence the immune system and contribute to host defense.
* **Pathogen Suppression:** Some microbes produce substances that directly inhibit the growth of pathogens, providing protection against infections.
* **Modulation of Inflammation:** The microbiome can influence the immune system's response, helping to maintain an appropriate balance between inflammation and immune regulation.
36
New cards
Define the epithelium of the body and locations where it is considered a primary barrier to infection.
Epithelium is continuous cell sheet covering exterior/interior surfaces. Physical/chemical barrier at skin, respiratory tract, GI tract, etc.
\
Epithelium Definition: Epithelium refers to a type of tissue that covers the external surfaces of the body and lines the internal cavities and organs. It acts as a protective barrier, regulating the exchange of substances between the body and its environment. Epithelial cells are closely packed and often form layers, providing a barrier against pathogens, physical damage, and dehydration.
__**Locations where Epithelium is a Primary Barrier to Infection:**__
1. __**Skin (Integumentary System):**__
* **Role**: The skin's outermost layer is composed of stratified squamous epithelium, which provides a physical barrier against pathogens, preventing their entry.
* **Barrier Function:** Skin prevents microbes from entering the body, along with its sebaceous (oil) and sweat glands that produce antimicrobial substances.
2. __**Respiratory Tract:**__
* **Role:** Epithelium lines the respiratory passages, including the nose, throat, and lungs.
* **Barrier Function:** The respiratory epithelium, along with mucus and cilia, traps and removes inhaled pathogens, preventing their entry into the lungs.
3. __**Gastrointestinal Tract:**__
* **Role**: The GI tract is lined with various types of epithelium along its length, including the stomach, intestines, and colon.
* **Barrier Function:** The epithelial lining prevents pathogens from entering the bloodstream and interacts with the gut microbiome to regulate immune responses.
4. __**Genitourinary Tract:**__
* **Role**: The genitourinary system includes the urinary and reproductive tracts, which are lined with specialized epithelium.
* **Barrier Function:** The epithelium of the urinary tract and genitalia prevents pathogens from ascending into the urinary bladder and reproductive organs.
5. __**Mucous Membranes:**__
* **Role:** Mucous membranes, found in various locations like the oral cavity, nasal passages, and digestive tract, consist of epithelial cells covered by a layer of mucus.
* **Barrier Function:** The mucous layer traps pathogens, preventing their entry into underlying tissues.
6. __**Eye (Conjunctiva):**__
* **Role:** The conjunctiva, a thin mucous membrane, covers the front surface of the eye.
* **Barrier Function**: It acts as a barrier against pathogens and foreign particles, contributing to eye health.
In these locations, epithelium serves as a primary barrier to infection by physically preventing the entry of pathogens and contributing to the overall defense of the body against external threats.
\
Epithelium Definition: Epithelium refers to a type of tissue that covers the external surfaces of the body and lines the internal cavities and organs. It acts as a protective barrier, regulating the exchange of substances between the body and its environment. Epithelial cells are closely packed and often form layers, providing a barrier against pathogens, physical damage, and dehydration.
__**Locations where Epithelium is a Primary Barrier to Infection:**__
1. __**Skin (Integumentary System):**__
* **Role**: The skin's outermost layer is composed of stratified squamous epithelium, which provides a physical barrier against pathogens, preventing their entry.
* **Barrier Function:** Skin prevents microbes from entering the body, along with its sebaceous (oil) and sweat glands that produce antimicrobial substances.
2. __**Respiratory Tract:**__
* **Role:** Epithelium lines the respiratory passages, including the nose, throat, and lungs.
* **Barrier Function:** The respiratory epithelium, along with mucus and cilia, traps and removes inhaled pathogens, preventing their entry into the lungs.
3. __**Gastrointestinal Tract:**__
* **Role**: The GI tract is lined with various types of epithelium along its length, including the stomach, intestines, and colon.
* **Barrier Function:** The epithelial lining prevents pathogens from entering the bloodstream and interacts with the gut microbiome to regulate immune responses.
4. __**Genitourinary Tract:**__
* **Role**: The genitourinary system includes the urinary and reproductive tracts, which are lined with specialized epithelium.
* **Barrier Function:** The epithelium of the urinary tract and genitalia prevents pathogens from ascending into the urinary bladder and reproductive organs.
5. __**Mucous Membranes:**__
* **Role:** Mucous membranes, found in various locations like the oral cavity, nasal passages, and digestive tract, consist of epithelial cells covered by a layer of mucus.
* **Barrier Function:** The mucous layer traps pathogens, preventing their entry into underlying tissues.
6. __**Eye (Conjunctiva):**__
* **Role:** The conjunctiva, a thin mucous membrane, covers the front surface of the eye.
* **Barrier Function**: It acts as a barrier against pathogens and foreign particles, contributing to eye health.
In these locations, epithelium serves as a primary barrier to infection by physically preventing the entry of pathogens and contributing to the overall defense of the body against external threats.
37
New cards
What chemical defenses does the epithelium and phagocytic cells produce that have antimicrobial properties
Epithelial cells and phagocytes produce antimicrobial peptides like defensins, cathelicidins, lysozyme, and complement proteins.
\
__**Epithelium and Phagocytic Cell Chemical Defenses:**__
1. **Defensins**:
* **Produced by:** Epithelial cells, neutrophils, and other immune cells.
* **Antimicrobial Action:** Defensins are small cationic peptides that disrupt bacterial and fungal cell membranes, leading to cell lysis and death.
2. **Cathelicidins:**
* **Produced by:** Epithelial cells and phagocytes.
* **Antimicrobial Action:** Cathelicidins are antimicrobial peptides that exhibit broad-spectrum activity against bacteria, fungi, and some viruses.
3. **Lysozyme:**
* **Produced by:** Epithelial cells, tears, saliva, and other secretions.
* **Antimicrobial Action:** Lysozyme breaks down bacterial cell walls by cleaving the bonds between sugar molecules in the peptidoglycan layer, leading to bacterial lysis.
4. **Reactive Oxygen Species (ROS):**
* **Produced by:** Phagocytes during the respiratory burst.
* **Antimicrobial Action:** ROS, including superoxide anions and hydrogen peroxide, have potent antimicrobial effects by damaging pathogen components.
5. **Reactive Nitrogen Species (RNS):**
* **Produced by:** Phagocytes.
* **Antimicrobial Action:** RNS, such as nitric oxide (NO), can modify proteins and nucleic acids in pathogens, inhibiting their growth and function.
6. **Hydrolytic Enzymes:**
* **Produced by:** Phagocytes, including macrophages and neutrophils.
* **Antimicrobial Action:** Hydrolytic enzymes released into phagosomes break down engulfed pathogens.
\
__**Epithelium and Phagocytic Cell Chemical Defenses:**__
1. **Defensins**:
* **Produced by:** Epithelial cells, neutrophils, and other immune cells.
* **Antimicrobial Action:** Defensins are small cationic peptides that disrupt bacterial and fungal cell membranes, leading to cell lysis and death.
2. **Cathelicidins:**
* **Produced by:** Epithelial cells and phagocytes.
* **Antimicrobial Action:** Cathelicidins are antimicrobial peptides that exhibit broad-spectrum activity against bacteria, fungi, and some viruses.
3. **Lysozyme:**
* **Produced by:** Epithelial cells, tears, saliva, and other secretions.
* **Antimicrobial Action:** Lysozyme breaks down bacterial cell walls by cleaving the bonds between sugar molecules in the peptidoglycan layer, leading to bacterial lysis.
4. **Reactive Oxygen Species (ROS):**
* **Produced by:** Phagocytes during the respiratory burst.
* **Antimicrobial Action:** ROS, including superoxide anions and hydrogen peroxide, have potent antimicrobial effects by damaging pathogen components.
5. **Reactive Nitrogen Species (RNS):**
* **Produced by:** Phagocytes.
* **Antimicrobial Action:** RNS, such as nitric oxide (NO), can modify proteins and nucleic acids in pathogens, inhibiting their growth and function.
6. **Hydrolytic Enzymes:**
* **Produced by:** Phagocytes, including macrophages and neutrophils.
* **Antimicrobial Action:** Hydrolytic enzymes released into phagosomes break down engulfed pathogens.
38
New cards
What is compliment? \n
The complement system is a cascade of soluble proteins that opsonize pathogens, induce inflammation, and directly kill some bacteria/viruses.
\
The complement system is a complex and vital part of the immune system that enhances the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism. It consists of a group of proteins that work together to trigger a series of chemical reactions, ultimately leading to the elimination of pathogens. The complement system plays a crucial role in both innate and adaptive immune responses.
__**The complement system can be activated through three main pathways:**__
1. %%**Classical Pathway:**%% Triggered by the binding of antibodies to pathogens. When antibodies attach to a pathogen's surface, complement proteins bind to the antibody-antigen complexes, initiating a cascade of reactions.
2. %%**Lectin Pathway:**%% Initiated by the binding of specific proteins called lectins to carbohydrates on the surface of pathogens. This pathway is a part of the innate immune response.
3. %%**Alternative Pathway:**%% This pathway is continuously active at a low level and can be spontaneously triggered by certain molecules present on the surface of microorganisms. It serves as a surveillance mechanism for detecting potential threats.
__When activated, the complement system can lead to several outcomes:__
* %%Opsonization:%% The complement proteins coat pathogens, marking them for recognition and ingestion by phagocytic cells.
* %%**Inflammation:**%% Complement proteins can stimulate the release of inflammatory molecules, attracting immune cells to the site of infection.
* %%**Membrane Attack Complex (MAC) Formation:**%% A complex of complement proteins assembles on the surface of pathogens, creating pores in their membranes, which can lead to cell lysis.
* %%**Enhancement of Adaptive Immune Responses:**%% The complement system helps bridge innate and adaptive immunity by facilitating the activation of B cells and enhancing antibody production.
In summary, the complement system is a sophisticated defense mechanism that contributes to the rapid and effective elimination of pathogens and immune response coordination. It is an integral part of both the innate and adaptive immune systems.
\
The complement system is a complex and vital part of the immune system that enhances the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism. It consists of a group of proteins that work together to trigger a series of chemical reactions, ultimately leading to the elimination of pathogens. The complement system plays a crucial role in both innate and adaptive immune responses.
__**The complement system can be activated through three main pathways:**__
1. %%**Classical Pathway:**%% Triggered by the binding of antibodies to pathogens. When antibodies attach to a pathogen's surface, complement proteins bind to the antibody-antigen complexes, initiating a cascade of reactions.
2. %%**Lectin Pathway:**%% Initiated by the binding of specific proteins called lectins to carbohydrates on the surface of pathogens. This pathway is a part of the innate immune response.
3. %%**Alternative Pathway:**%% This pathway is continuously active at a low level and can be spontaneously triggered by certain molecules present on the surface of microorganisms. It serves as a surveillance mechanism for detecting potential threats.
__When activated, the complement system can lead to several outcomes:__
* %%Opsonization:%% The complement proteins coat pathogens, marking them for recognition and ingestion by phagocytic cells.
* %%**Inflammation:**%% Complement proteins can stimulate the release of inflammatory molecules, attracting immune cells to the site of infection.
* %%**Membrane Attack Complex (MAC) Formation:**%% A complex of complement proteins assembles on the surface of pathogens, creating pores in their membranes, which can lead to cell lysis.
* %%**Enhancement of Adaptive Immune Responses:**%% The complement system helps bridge innate and adaptive immunity by facilitating the activation of B cells and enhancing antibody production.
In summary, the complement system is a sophisticated defense mechanism that contributes to the rapid and effective elimination of pathogens and immune response coordination. It is an integral part of both the innate and adaptive immune systems.
39
New cards
What are the stages of compliment action?
Stages: Recognition, activation, opsonization, inflammation, formation of membrane attack complex.
\
\
__**Stages of Complement Action:**__
1. %%**Initiation:**%%
* **Recognition:** Antibodies (classical), lectins (lectin), or spontaneous hydrolysis (alternative) trigger pathways.
* **Formation:** Enzyme complexes activate.
2. %%**Amplification and Cascade:**%%
* **C3 Activation:** C3 is split into C3a (inflammatory) and C3b (opsonin).
* **Convertase Formation:** C3b forms convertases, amplifying reaction.
3. %%**MAC Formation:**%%
* **C5 Cleavage:** C5 splits into C5a (inflammatory) and C5b (MAC starter).
* **MAC Assembly:** C5b associates with C6-9 to create pores.
4. %%**Inflammation and Opsonization:**%%
* **Inflammation:** C3a and C5a attract immune cells.
* **Opsonization**: C3b enhances pathogen engulfment.
5. %%**Regulation and Termination:**%%
* **Regulatory Proteins:** Factor H controls host cell activation.
* **Control:** DAF disassembles convertases, moderating inflammation.
The complement system's stages collaborate for effective pathogen recognition, elimination, and regulation.
\
\
__**Stages of Complement Action:**__
1. %%**Initiation:**%%
* **Recognition:** Antibodies (classical), lectins (lectin), or spontaneous hydrolysis (alternative) trigger pathways.
* **Formation:** Enzyme complexes activate.
2. %%**Amplification and Cascade:**%%
* **C3 Activation:** C3 is split into C3a (inflammatory) and C3b (opsonin).
* **Convertase Formation:** C3b forms convertases, amplifying reaction.
3. %%**MAC Formation:**%%
* **C5 Cleavage:** C5 splits into C5a (inflammatory) and C5b (MAC starter).
* **MAC Assembly:** C5b associates with C6-9 to create pores.
4. %%**Inflammation and Opsonization:**%%
* **Inflammation:** C3a and C5a attract immune cells.
* **Opsonization**: C3b enhances pathogen engulfment.
5. %%**Regulation and Termination:**%%
* **Regulatory Proteins:** Factor H controls host cell activation.
* **Control:** DAF disassembles convertases, moderating inflammation.
The complement system's stages collaborate for effective pathogen recognition, elimination, and regulation.
40
New cards
Describe the three pathways of compliment action.
Three pathways: Classical (antibody-triggered), lectin (microbial carbohydrate-triggered), alternative (spontaneous C3 hydrolysis).
\
__**Classical Pathway:**__
* Initiated by antibody binding.
* C1 enzyme complex activates C4 and C2.
* Forms C4b2a (C3 convertase).
* Leads to opsonization, inflammation, and MAC.
__**Lectin Pathway:**__
* Triggered by lectin binding to pathogen carbs.
* MASP enzymes activate C4 and C2.
* Generates C4b2a (C3 convertase).
* Aids opsonization, inflammation, pathogen clearance.
__**Alternative Pathway:**__
* Begins with C3 hydrolysis or binding to pathogens.
* Forms C3bBb (C3 convertase).
* Rapid innate defense, inflammation, opsonization.
\
__**Classical Pathway:**__
* Initiated by antibody binding.
* C1 enzyme complex activates C4 and C2.
* Forms C4b2a (C3 convertase).
* Leads to opsonization, inflammation, and MAC.
__**Lectin Pathway:**__
* Triggered by lectin binding to pathogen carbs.
* MASP enzymes activate C4 and C2.
* Generates C4b2a (C3 convertase).
* Aids opsonization, inflammation, pathogen clearance.
__**Alternative Pathway:**__
* Begins with C3 hydrolysis or binding to pathogens.
* Forms C3bBb (C3 convertase).
* Rapid innate defense, inflammation, opsonization.
41
New cards
What triggers their response? \n
Triggered by:
* Antibodies,
* carbohydrates,
* spontaneous C3 tickover.
* Antibodies,
* carbohydrates,
* spontaneous C3 tickover.
42
New cards
What are the mediators of their activation. \n
All pathways activate C3/C5 for opsonization but recognize different triggers.
\
\n __Complement Pathways Activation:__
* Classical: Antibodies
* Lectin: Carbohydrates, lectins
* Alternative: Spontaneous C3 hydrolysis
\
\n __Complement Pathways Activation:__
* Classical: Antibodies
* Lectin: Carbohydrates, lectins
* Alternative: Spontaneous C3 hydrolysis
43
New cards
How do these pathways differ and how are they similar?
***Complement Pathways: Differences and Similarities:***
==__Differences:__==
* Trigger:
* Classical: Activated by antibody-antigen complexes.
* Lectin: Triggered by lectins binding to carbohydrates on pathogens.
* Alternative: Spontaneously activated by hydrolysis of C3 or pathogen surfaces.
* Initiating Complex:
* Classical: C1 complex (C1q, C1r, C1s) binds to antibodies.
* Lectin: Lectins bind to carbohydrates, initiating MASP enzymes.
* Alternative: Spontaneous C3 hydrolysis or properdin binding.
* C3 Convertase Formation:
* Classical: C4b2a complex.
* Lectin: C4b2a complex.
* Alternative: C3bBb complex.
* Dependency on Antibodies:
* Classical: Requires antibody involvement.
* Lectin: Independent of antibodies.
* Alternative: Partially independent of antibodies.
==__Similarities:__==
* Amplification: All pathways amplify C3 cleavage.
* C3 Convertase: All generate C3 convertases for further activation.
* Opsonization: Result in opsonization of pathogens.
* Inflammation: Induce inflammation via anaphylatoxins.
* Membrane Attack Complex (MAC): Can lead to MAC formation for pathogen lysis.
Overall, all pathways lead to the activation of complement proteins, resulting in opsonization, inflammation, and pathogen elimination. They differ in initiation triggers and mechanisms but share core components and outcomes.
==__Differences:__==
* Trigger:
* Classical: Activated by antibody-antigen complexes.
* Lectin: Triggered by lectins binding to carbohydrates on pathogens.
* Alternative: Spontaneously activated by hydrolysis of C3 or pathogen surfaces.
* Initiating Complex:
* Classical: C1 complex (C1q, C1r, C1s) binds to antibodies.
* Lectin: Lectins bind to carbohydrates, initiating MASP enzymes.
* Alternative: Spontaneous C3 hydrolysis or properdin binding.
* C3 Convertase Formation:
* Classical: C4b2a complex.
* Lectin: C4b2a complex.
* Alternative: C3bBb complex.
* Dependency on Antibodies:
* Classical: Requires antibody involvement.
* Lectin: Independent of antibodies.
* Alternative: Partially independent of antibodies.
==__Similarities:__==
* Amplification: All pathways amplify C3 cleavage.
* C3 Convertase: All generate C3 convertases for further activation.
* Opsonization: Result in opsonization of pathogens.
* Inflammation: Induce inflammation via anaphylatoxins.
* Membrane Attack Complex (MAC): Can lead to MAC formation for pathogen lysis.
Overall, all pathways lead to the activation of complement proteins, resulting in opsonization, inflammation, and pathogen elimination. They differ in initiation triggers and mechanisms but share core components and outcomes.
44
New cards
What regulates the formation and stability of C3 convertases determine the extent of complement activation?
1. **Regulation of C3 Convertases and Complement Activation:** The formation and stability of C3 convertases, which are key enzymes in the complement system, are regulated by several factors that determine the extent of complement activation. These regulatory mechanisms help prevent excessive complement activation and potential damage to host cells.
1. **Decay-Accelerating Factor (DAF):**
* **Function:** DAF is a cell surface protein that accelerates the decay of C3 and C5 convertases.
* **Result:** By disassembling convertases, DAF limits their activity and reduces complement amplification.
2. **Factor H:**
* **Function:** Factor H is a plasma protein that competes with Factor B for binding to C3b, preventing the formation of the alternative pathway C3 convertase (C3bBb).
* R**esult:** Factor H helps regulate and control the alternative pathway's amplification loop.
3. **Membrane Cofactor Protein (MCP):**
* **Function:** MCP promotes the degradation of C3b, limiting its deposition on host cells and preventing further complement activation.
* **Result:** MCP helps protect host cells from complement-mediated damage.
4. **Properdin:**
* **Function:** Properdin stabilizes the alternative pathway C3 convertase (C3bBb), leading to increased amplification.
* **Result:** Properdin can enhance complement activation, contributing to defense against pathogens.
5. **Factor I and Factor H Cooperation:**
* **Function:** Factor I, in the presence of Factor H, cleaves C3b into inactive fragments.
* **Result:** This cleavage prevents the formation of C3 convertases and reduces complement activation.
6. **Controlled Cleavage:**
* **Function:** Regulatory proteases (e.g., Factor I) cleave complement components to control their activity.
* **Result:** Controlled cleavage prevents excessive activation and maintains complement homeostasis.
45
New cards
What are the final outcomes of Compliment activation?
* **Opsonization:** Coating pathogens for phagocytosis.
* **Inflammation:** Attracting immune cells to infection site.
* **MAC Formation:** Creating pores in pathogen membranes.
* **Pathogen Elimination:** Destroying and clearing pathogens.
* **Adaptive Immunity:** Bridging innate and adaptive responses.
* **Immune Complex Clearance:** Removing antigen-antibody complexes.
* **Immune Homeostasis:** Controlled activation prevents harm.
* **Inflammation:** Attracting immune cells to infection site.
* **MAC Formation:** Creating pores in pathogen membranes.
* **Pathogen Elimination:** Destroying and clearing pathogens.
* **Adaptive Immunity:** Bridging innate and adaptive responses.
* **Immune Complex Clearance:** Removing antigen-antibody complexes.
* **Immune Homeostasis:** Controlled activation prevents harm.
46
New cards
Explain the other effects that compliment fragments have on the body.
* **Chemotaxis:** Guiding immune cells to infection.
* **Phagocytosis:** Easier recognition for engulfment.
* **Mast Cell Activation:** Release of inflammatory mediators.
* **Immune Cell Activation:** Enhanced immune response.
* **Antigen Presentation:** Efficient presentation to T cells.
* **Immune Complex Clearance:** Breakdown and removal.
* **Vascular Permeability:** Immune cell transport to sites.
* **Phagocytosis:** Easier recognition for engulfment.
* **Mast Cell Activation:** Release of inflammatory mediators.
* **Immune Cell Activation:** Enhanced immune response.
* **Antigen Presentation:** Efficient presentation to T cells.
* **Immune Complex Clearance:** Breakdown and removal.
* **Vascular Permeability:** Immune cell transport to sites.
47
New cards
Name the compliment control proteins which prevent host damage.
__Complement Control Proteins:__
1. **Decay-Accelerating Factor (DAF):** Accelerates decay of C3 and C5 convertases, reducing their activity.
2. **Factor H:** Competes with Factor B to regulate the alternative pathway, preventing excessive amplification.
3. **Membrane Cofactor Protein (MCP):** Promotes degradation of C3b, protecting host cells.
4. **C1 Inhibitor:** Inhibits C1 complex, preventing excessive classical pathway activation.
5. **C4b-binding Protein (C4BP):** Binds to C4b, limiting its interaction with other complement components.
These control proteins ensure that complement activation is balanced and controlled, preventing damage to host cells and tissues while effectively targeting pathogens.
1. **Decay-Accelerating Factor (DAF):** Accelerates decay of C3 and C5 convertases, reducing their activity.
2. **Factor H:** Competes with Factor B to regulate the alternative pathway, preventing excessive amplification.
3. **Membrane Cofactor Protein (MCP):** Promotes degradation of C3b, protecting host cells.
4. **C1 Inhibitor:** Inhibits C1 complex, preventing excessive classical pathway activation.
5. **C4b-binding Protein (C4BP):** Binds to C4b, limiting its interaction with other complement components.
These control proteins ensure that complement activation is balanced and controlled, preventing damage to host cells and tissues while effectively targeting pathogens.
48
New cards
Name some strategies of pathogens to avoid compliment activation.
**Pathogen Strategies to Evade Complement Activation:**
1. **Capsule Formation:** Pathogens develop thick capsules that hinder complement protein binding and opsonization.
2. **Decoy Molecules:** Pathogens produce molecules that mimic host regulators, preventing complement activation.
3. **Enzymatic Degradation:** Some pathogens secrete proteases that break down complement proteins.
4. **Surface Mimicry:** Pathogens display host-like molecules on their surface, tricking the immune system.
5. **Binding to Host Regulators:** Pathogens bind host regulatory proteins, shielding themselves from complement attack.
6. **Inhibition of C3 Convertase:** Some bacteria secrete proteins that inhibit C3 convertase formation.
7. **Formation of Complement Resistant Membrane: P**athogens modify their surface to prevent MAC formation.
8. **Antigenic Variation:** Rapidly changing surface antigens evade immune recognition and complement action.
These strategies allow pathogens to subvert the host's complement system, enabling their survival and establishment of infection.
1. **Capsule Formation:** Pathogens develop thick capsules that hinder complement protein binding and opsonization.
2. **Decoy Molecules:** Pathogens produce molecules that mimic host regulators, preventing complement activation.
3. **Enzymatic Degradation:** Some pathogens secrete proteases that break down complement proteins.
4. **Surface Mimicry:** Pathogens display host-like molecules on their surface, tricking the immune system.
5. **Binding to Host Regulators:** Pathogens bind host regulatory proteins, shielding themselves from complement attack.
6. **Inhibition of C3 Convertase:** Some bacteria secrete proteins that inhibit C3 convertase formation.
7. **Formation of Complement Resistant Membrane: P**athogens modify their surface to prevent MAC formation.
8. **Antigenic Variation:** Rapidly changing surface antigens evade immune recognition and complement action.
These strategies allow pathogens to subvert the host's complement system, enabling their survival and establishment of infection.
49
New cards
Considering that bacteria & other pathogens have preferred routes of entry. Which of the following defenses would be an obstacle for influenza to circumvent before causing an infection
\
Select:
\
Lysozyme
Mucus
Cilia
Fatty Acids
Compliment
\
Select:
\
Lysozyme
Mucus
Cilia
Fatty Acids
Compliment
Lysozyme
Mucus
Compliment
Mucus
Compliment
50
New cards
Which of the following are not a type of vaccine?
\
a) live unaltered virus. Injected straight into the arm.
b) None of the above
c) Cow or other animal pathogens
d) Messenger RNA vaccines
e) Toxic Secretion
\
a) live unaltered virus. Injected straight into the arm.
b) None of the above
c) Cow or other animal pathogens
d) Messenger RNA vaccines
e) Toxic Secretion
b) None of the above
51
New cards
Compliment is a soluble factor which helps the innate immune system recognize a pathogen and is the only innate immune factor which isn't modulated by the adaptive immune system.
\
a) True
b) False
\
a) True
b) False
b) False
\
The Classical pathway (although not the major actor of the compliment system) activates with the binding of an antibody to the pathogen's surface which sets off a compliment cascade.
\
\
In addition to the classical cascade cytokines released by both innate and adaptive immune systems help support the circulation and activation of compliment by promoting inflammation.
\
The Classical pathway (although not the major actor of the compliment system) activates with the binding of an antibody to the pathogen's surface which sets off a compliment cascade.
\
\
In addition to the classical cascade cytokines released by both innate and adaptive immune systems help support the circulation and activation of compliment by promoting inflammation.
52
New cards
In a process called 'Tick over' compliment C3 is activated by ____________.
\
Fill in the blank
\
Fill in the blank
Hydrolysis
\
This process also inactivates C3 functionally turning it on and then off again over and over (Ticking over) until either it finds something or it is no longer needed and is recycled.
\
C3 'Tick over' is the process where C3 can be spontaneously activated and inactivated by water through a process called hydrolysis. This process can happen repeatedly turning on this hydrolyzed C3 on and off like an engine ticking over and over again starting and stopping. This process is important because it allows C3 to be activated spontaneously in case there is an undetected pathogen nearby but also turns back off in case there isn't and an activated C3(H2O) could be dangerous to the local cells.
\
This process also inactivates C3 functionally turning it on and then off again over and over (Ticking over) until either it finds something or it is no longer needed and is recycled.
\
C3 'Tick over' is the process where C3 can be spontaneously activated and inactivated by water through a process called hydrolysis. This process can happen repeatedly turning on this hydrolyzed C3 on and off like an engine ticking over and over again starting and stopping. This process is important because it allows C3 to be activated spontaneously in case there is an undetected pathogen nearby but also turns back off in case there isn't and an activated C3(H2O) could be dangerous to the local cells.
53
New cards
What are the key differences between innate and adaptive receptors?
Innate receptors are encoded in the germline and are fixed in their specificity, recognizing broad patterns called PAMPs (Pathogen-Associated Molecular Patterns) and DAMPs (Danger-Associated Molecular Patterns). In contrast, adaptive receptors, like antibodies and T-cell receptors, are generated somatically and have highly specific antigen recognition.
54
New cards
Describe the different types of PRR’s that the innate immune system uses on their cell surface to detect PAMPs and DAMPs
The innate immune system uses various Pattern Recognition Receptors (PRRs) on their cell surfaces to detect PAMPs and DAMPs. These include Toll-like receptors (TLRs), NOD-like receptors (NLRs), and RIG-I-like receptors (RLRs), among others. Each type of receptor has distinct specificities and functions in recognizing different microbial or danger signals.
55
New cards
\
Explain how G-coupled protein receptors send signals in pathogen recognition.
Explain how G-coupled protein receptors send signals in pathogen recognition.
G-coupled protein receptors play a role in pathogen recognition by linking the recognition of microbe-associated patterns (e.g., PAMPs) to intracellular signaling pathways. When these receptors bind to specific patterns, they activate G-proteins, initiating a cascade of intracellular events that ultimately lead to an immune response, including the production of inflammatory cytokines and the activation of immune cells. This signaling pathway enhances the efficiency of intracellular pathogen killing.
56
New cards
List several phagocytic mechanisms for killing pathogens. Which are used by Macrophages and which neutrophils?
\
* %%__Macrophages use various mechanisms, including:__%%
* **Phagosome-lysosome fusion:** Pathogens are engulfed and delivered to lysosomes for degradation.
* **Reactive oxygen species (ROS) production:** Macrophages generate ROS to kill ingested microbes.
* **Nitric oxide (NO) production:** Macrophages release NO, which has antimicrobial properties.
* %%__Neutrophils employ similar mechanisms, such as:__%%
* Phagosome-lysosome fusion.
* **Respiratory burst:** Neutrophils produce ROS during the respiratory burst to kill pathogens.
* %%__Macrophages use various mechanisms, including:__%%
* **Phagosome-lysosome fusion:** Pathogens are engulfed and delivered to lysosomes for degradation.
* **Reactive oxygen species (ROS) production:** Macrophages generate ROS to kill ingested microbes.
* **Nitric oxide (NO) production:** Macrophages release NO, which has antimicrobial properties.
* %%__Neutrophils employ similar mechanisms, such as:__%%
* Phagosome-lysosome fusion.
* **Respiratory burst:** Neutrophils produce ROS during the respiratory burst to kill pathogens.
57
New cards
What are the 3 essential roles inflammation have in combating infections?
* **Recruitment of Immune Cells:** Inflammation attracts immune cells (like neutrophils and macrophages) to the site of infection.
* **Enhancement of Microbial Killing:** It increases the efficiency of phagocytosis and intracellular pathogen killing.
* **Tissue Repair:** Inflammation stimulates tissue repair and regeneration after infection.
* **Enhancement of Microbial Killing:** It increases the efficiency of phagocytosis and intracellular pathogen killing.
* **Tissue Repair:** Inflammation stimulates tissue repair and regeneration after infection.
58
New cards
List the types of molecules that Toll- like Receptors can recognize
* **Bacterial components:** Such as lipopolysaccharides (LPS), lipoproteins, and peptidoglycans.
* **Viral nucleic acids:** Such as double-stranded RNA (dsRNA), single-stranded RNA (ssRNA), and unmethylated CpG DNA motifs.
* **Fungal components:** Including β-glucans and mannan.
* **Endogenous danger signals:** Such as heat shock proteins and high mobility group box 1 (HMGB1).
* **Viral nucleic acids:** Such as double-stranded RNA (dsRNA), single-stranded RNA (ssRNA), and unmethylated CpG DNA motifs.
* **Fungal components:** Including β-glucans and mannan.
* **Endogenous danger signals:** Such as heat shock proteins and high mobility group box 1 (HMGB1).
59
New cards
Understand why the location of different TLR’s relate to where they are located.
* **Cell Surface TLRs (TLR1, TLR2, TLR4, TLR5, TLR6, and TLR11):** These are situated on the cell membrane and recognize extracellular pathogens like bacteria.
* **Intracellular TLRs (TLR3, TLR7, TLR8, TLR9):** These are found within endosomes and detect nucleic acids from viruses and intracellular pathogens.
* **Location matches function:** Cell surface TLRs detect pathogens before they enter cells, while intracellular TLRs survey the interior for infected cells.
* **Intracellular TLRs (TLR3, TLR7, TLR8, TLR9):** These are found within endosomes and detect nucleic acids from viruses and intracellular pathogens.
* **Location matches function:** Cell surface TLRs detect pathogens before they enter cells, while intracellular TLRs survey the interior for infected cells.
60
New cards
Know which TLR’s are classically found in which innate immune cell.
* **Macrophages and Dendritic Cells:** They typically express a wide range of TLRs, including TLR2, TLR4, TLR7, TLR8, and TLR9.
* **Neutrophils:** They primarily express TLR2 and TLR4.
* **B Cells:** B cells mainly express TLR1, TLR6, TLR7, and TLR9.
* **Natural Killer (NK) Cells:** NK cells may express TLR3, TLR7, and TLR9.
* **Location of TLRs on these cells:** The expression of these TLRs matches the specific pathogens these cells encounter and respond to.
* **Neutrophils:** They primarily express TLR2 and TLR4.
* **B Cells:** B cells mainly express TLR1, TLR6, TLR7, and TLR9.
* **Natural Killer (NK) Cells:** NK cells may express TLR3, TLR7, and TLR9.
* **Location of TLRs on these cells:** The expression of these TLRs matches the specific pathogens these cells encounter and respond to.
61
New cards
\
What other proteins are associated with TLR’s to assist their function and why are they needed?
What other proteins are associated with TLR’s to assist their function and why are they needed?
* **CD14:** Enhances TLR2 and TLR4 responses to bacterial components like LPS.
* **MD-2:** Required for TLR4 recognition of LPS.
* **MyD88:** An adaptor protein used by most TLRs to activate downstream signaling.
* **TRIF:** An adaptor protein used by TLR3 and TLR4 to activate different signaling pathways.
* **TRAM:** An adaptor protein involved in TLR4 signaling.
* **Importance:** These proteins assist TLRs by facilitating the recognition of specific ligands and activating the appropriate signaling cascades.
* **MD-2:** Required for TLR4 recognition of LPS.
* **MyD88:** An adaptor protein used by most TLRs to activate downstream signaling.
* **TRIF:** An adaptor protein used by TLR3 and TLR4 to activate different signaling pathways.
* **TRAM:** An adaptor protein involved in TLR4 signaling.
* **Importance:** These proteins assist TLRs by facilitating the recognition of specific ligands and activating the appropriate signaling cascades.
62
New cards
Describe the intracellular signaling used in TLR signaling
* **TLR Activation:** When TLRs recognize PAMPs, they initiate a signaling cascade.
* **MyD88-Dependent Pathway:** Most TLRs signal through the adaptor protein MyD88, which leads to the activation of NF-κB and pro-inflammatory cytokine production.
* **TRIF-Dependent Pathway:** TLR3 and TLR4 use the adaptor protein TRIF, leading to the production of type I interferons (IFNs) and pro-inflammatory cytokines.
* **Results:** These pathways coordinate immune responses to different pathogens.
* **MyD88-Dependent Pathway:** Most TLRs signal through the adaptor protein MyD88, which leads to the activation of NF-κB and pro-inflammatory cytokine production.
* **TRIF-Dependent Pathway:** TLR3 and TLR4 use the adaptor protein TRIF, leading to the production of type I interferons (IFNs) and pro-inflammatory cytokines.
* **Results:** These pathways coordinate immune responses to different pathogens.
63
New cards
Describe NOD-like receptors and what they detect.
\
\
* **NLRs are Intracellular Sensors:** NLRs are a family of intracellular receptors that detect various PAMPs and DAMPs.
* **Recognition:** They recognize bacterial components (like peptidoglycans) and signs of cellular damage.
* **Function:** Upon activation, NLRs can form complexes called inflammasomes, leading to the activation of inflammatory responses, including the production of IL-1β and IL-18.
* **Recognition:** They recognize bacterial components (like peptidoglycans) and signs of cellular damage.
* **Function:** Upon activation, NLRs can form complexes called inflammasomes, leading to the activation of inflammatory responses, including the production of IL-1β and IL-18.
64
New cards
Explain what is an inflammasome and what it’s function is in infection response
* **Inflammasome Formation:** An inflammasome is a multiprotein complex formed by NLRs when they sense danger signals.
* **Function:** The inflammasome's primary function is to activate caspase-1, which cleaves pro-inflammatory cytokines (e.g., pro-IL-1β) into their active forms (e.g., IL-1β). This process initiates an intense inflammatory response.
* **Role in Infection Response: I**nflammasomes play a crucial role in host defense by initiating inflammation and recruiting immune cells to the infection site.
* **Function:** The inflammasome's primary function is to activate caspase-1, which cleaves pro-inflammatory cytokines (e.g., pro-IL-1β) into their active forms (e.g., IL-1β). This process initiates an intense inflammatory response.
* **Role in Infection Response: I**nflammasomes play a crucial role in host defense by initiating inflammation and recruiting immune cells to the infection site.
65
New cards
Know what RIG-I is and what type of pathogen detection does it accomplish.
* **Pathogen Detection:** RIG-I is a cytoplasmic receptor that detects viral RNA, specifically double-stranded RNA with 5'-triphosphate ends.
* **Function:** Upon activation, RIG-I triggers signaling pathways that lead to the production of type I interferons (IFNs) and pro-inflammatory cytokines.
* **Role:** RIG-I plays a significant role in antiviral immune responses by detecting RNA viruses and initiating the host defense against them.
* **Function:** Upon activation, RIG-I triggers signaling pathways that lead to the production of type I interferons (IFNs) and pro-inflammatory cytokines.
* **Role:** RIG-I plays a significant role in antiviral immune responses by detecting RNA viruses and initiating the host defense against them.
66
New cards
Relate how do Dendritic cells and Macrophages differ in their response to innate receptor signaling
* **Macrophages:** Typically, macrophages are potent producers of pro-inflammatory cytokines like IL-1β and TNF-α in response to TLR activation. They play a crucial role in phagocytosis and inflammation at the site of infection.
* **Dendritic Cells (DCs):** DCs excel at antigen presentation, linking innate and adaptive immunity. They produce fewer pro-inflammatory cytokines but are essential for initiating adaptive immune responses by activating T cells.
* **Functional Differences:** Macrophages are primarily involved in rapid pathogen clearance and immediate inflammation, while DCs focus on initiating adaptive immune responses through antigen presentation
* **Dendritic Cells (DCs):** DCs excel at antigen presentation, linking innate and adaptive immunity. They produce fewer pro-inflammatory cytokines but are essential for initiating adaptive immune responses by activating T cells.
* **Functional Differences:** Macrophages are primarily involved in rapid pathogen clearance and immediate inflammation, while DCs focus on initiating adaptive immune responses through antigen presentation
67
New cards
Describe the different families of receptor proteins.
* **Pattern Recognition Receptors (PRRs):** PRRs are a family of receptor proteins that include Toll-like receptors (TLRs), NOD-like receptors (NLRs), and RIG-I-like receptors (RLRs). They recognize pathogen-associated molecular patterns (PAMPs) and danger-associated molecular patterns (DAMPs).
* **Cytokine Receptors:** These receptors are activated by cytokines, which are signaling molecules secreted by immune cells. Examples include interferon receptors and interleukin receptors.
* **Complement Receptors:** Complement receptors, like CR1 and CR2, recognize complement fragments and play roles in opsonization and immune cell activation.
* **Cell Adhesion Molecules:** These molecules facilitate cell-cell interactions and include selectins, integrins, and members of the immunoglobulin superfamily.
* **Cytokine Receptors:** These receptors are activated by cytokines, which are signaling molecules secreted by immune cells. Examples include interferon receptors and interleukin receptors.
* **Complement Receptors:** Complement receptors, like CR1 and CR2, recognize complement fragments and play roles in opsonization and immune cell activation.
* **Cell Adhesion Molecules:** These molecules facilitate cell-cell interactions and include selectins, integrins, and members of the immunoglobulin superfamily.
68
New cards
Differentiate between local and systemic effects of cytokines released by macrophages.
* **Local Effects:** Macrophages release cytokines, such as IL-1β and TNF-α, locally at the site of infection or inflammation. These cytokines induce local responses, such as vasodilation, increased vascular permeability, and recruitment of immune cells to the infected tissue.
* **Systemic Effects:** Some cytokines, like IL-6 and IL-12, can also enter the bloodstream, leading to systemic effects. For example, IL-6 is involved in the acute-phase response, which affects the entire body.
* **Systemic Effects:** Some cytokines, like IL-6 and IL-12, can also enter the bloodstream, leading to systemic effects. For example, IL-6 is involved in the acute-phase response, which affects the entire body.
69
New cards
Describe the three classes of chemokine molecules released by macrophages and how they effect immune cell recruitment.
* **CXC Chemokines:** These chemokines are characterized by a pair of cysteine amino acids separated by a non-cysteine amino acid (C-X-C motif). They primarily attract neutrophils and are important for early inflammatory responses.
* **CC Chemokines:** CC chemokines have adjacent cysteine amino acids (C-C motif). They are involved in the recruitment of monocytes, eosinophils, and lymphocytes.
* **CX3C Chemokines:** These chemokines have three amino acids between the cysteine residues (C-X3-C motif). CX3CL1 (fractalkine) is a prominent example that attracts T cells and monocytes.
* **CC Chemokines:** CC chemokines have adjacent cysteine amino acids (C-C motif). They are involved in the recruitment of monocytes, eosinophils, and lymphocytes.
* **CX3C Chemokines:** These chemokines have three amino acids between the cysteine residues (C-X3-C motif). CX3CL1 (fractalkine) is a prominent example that attracts T cells and monocytes.
70
New cards
Explain what Selectins, Integrins and members of the Immunoglobulin Superfamily cause leukocyte rolling and cellular adhesion in an immune response.
* **Selectins:** Selectins are adhesion molecules expressed on endothelial cells and leukocytes. They mediate leukocyte rolling by weak, transient interactions with carbohydrate ligands on endothelial cells.
* **Integrins**: Integrins are cell surface receptors that undergo conformational changes upon activation. They play a crucial role in the firm adhesion of leukocytes to endothelial cells by binding to immunoglobulin superfamily members like ICAM-1.
* **Immunoglobulin Superfamily:** Members of the immunoglobulin superfamily, such as ICAM-1 and VCAM-1, are expressed on endothelial cells. They interact with integrins on leukocytes, promoting strong adhesion and transmigration into tissues.
* **Integrins**: Integrins are cell surface receptors that undergo conformational changes upon activation. They play a crucial role in the firm adhesion of leukocytes to endothelial cells by binding to immunoglobulin superfamily members like ICAM-1.
* **Immunoglobulin Superfamily:** Members of the immunoglobulin superfamily, such as ICAM-1 and VCAM-1, are expressed on endothelial cells. They interact with integrins on leukocytes, promoting strong adhesion and transmigration into tissues.
71
New cards
Describe the phases of neutrophil rolling and recruitment to the site of an infection.
* **Tethering and Rolling: I**nitially, neutrophils tether to the endothelial cells lining blood vessels via selectin molecules. They roll along the endothelium due to weak interactions between selectins and their ligands.
* **Activation:** Chemokines released at the infection site activate neutrophils. This causes conformational changes in integrins on neutrophils, preparing them for firm adhesion.
* **Firm Adhesion:** Neutrophils firmly adhere to endothelial cells through interactions between integrins (on neutrophils) and immunoglobulin superfamily members like ICAM-1 (on endothelial cells).
* **Diapedesis:** Neutrophils squeeze between endothelial cells and migrate towards the site of infection.
* **Chemotaxis:** Neutrophils follow chemical gradients of chemokines towards the source of infection.
* **Phagocytosis:** Upon reaching the infection site, neutrophils engulf and destroy pathogens through phagocytosis and the release of antimicrobial molecules.
* **Activation:** Chemokines released at the infection site activate neutrophils. This causes conformational changes in integrins on neutrophils, preparing them for firm adhesion.
* **Firm Adhesion:** Neutrophils firmly adhere to endothelial cells through interactions between integrins (on neutrophils) and immunoglobulin superfamily members like ICAM-1 (on endothelial cells).
* **Diapedesis:** Neutrophils squeeze between endothelial cells and migrate towards the site of infection.
* **Chemotaxis:** Neutrophils follow chemical gradients of chemokines towards the source of infection.
* **Phagocytosis:** Upon reaching the infection site, neutrophils engulf and destroy pathogens through phagocytosis and the release of antimicrobial molecules.
72
New cards
Explain what is the acute-phase response induced by macrophages and dendritic cells
* The acute-phase response is a systemic reaction triggered by inflammatory signals, including cytokines released by activated macrophages and dendritic cells.
* It involves the liver, which produces acute-phase proteins, such as C-reactive protein (CRP) and serum amyloid A (SAA), in response to pro-inflammatory cytokines.
* These proteins help neutralize pathogens and enhance the immune response. CRP, for example, can bind to microbial surfaces and promote their clearance.
* The acute-phase response also includes increased production of cytokines, such as IL-6, which can have systemic effects, such as fever.
* It involves the liver, which produces acute-phase proteins, such as C-reactive protein (CRP) and serum amyloid A (SAA), in response to pro-inflammatory cytokines.
* These proteins help neutralize pathogens and enhance the immune response. CRP, for example, can bind to microbial surfaces and promote their clearance.
* The acute-phase response also includes increased production of cytokines, such as IL-6, which can have systemic effects, such as fever.
73
New cards
Describe the response to virus infected host cells and what Interferons induce these defenses.
* When a cell becomes infected by a virus, it can produce type I interferons (IFN-α and IFN-β).
* Type I interferons have several antiviral effects:
* They induce neighboring cells to enter an antiviral state, making them more resistant to viral infection.
* They activate natural killer (NK) cells, enhancing their ability to kill virus-infected cells.
* They increase the expression of major histocompatibility complex (MHC) molecules on infected cells, facilitating their recognition and elimination by cytotoxic T cells.
* They inhibit viral replication within infected cells.
* Type I interferons have several antiviral effects:
* They induce neighboring cells to enter an antiviral state, making them more resistant to viral infection.
* They activate natural killer (NK) cells, enhancing their ability to kill virus-infected cells.
* They increase the expression of major histocompatibility complex (MHC) molecules on infected cells, facilitating their recognition and elimination by cytotoxic T cells.
* They inhibit viral replication within infected cells.
74
New cards
\
Describe the different Lymphoid cells of the innate immune system which provide early protection during an infection.
Describe the different Lymphoid cells of the innate immune system which provide early protection during an infection.
* **Natural Killer (NK) Cells:** NK cells are cytotoxic lymphocytes that can directly kill virus-infected and tumor cells. They play a crucial role in early defense against infected host cells.
* **Innate Lymphoid Cells (ILCs):** ILCs are a group of lymphocytes that do not express antigen-specific receptors. They contribute to early immune responses by producing cytokines that help regulate inflammation and immune cell recruitment.
* **Gamma Delta (γδ) T Cells: T**hese T cells express a unique T cell receptor (TCR) and are involved in the early immune response, particularly in mucosal tissues. They can recognize specific antigens and contribute to host defense.
* **Innate Lymphoid Cells (ILCs):** ILCs are a group of lymphocytes that do not express antigen-specific receptors. They contribute to early immune responses by producing cytokines that help regulate inflammation and immune cell recruitment.
* **Gamma Delta (γδ) T Cells: T**hese T cells express a unique T cell receptor (TCR) and are involved in the early immune response, particularly in mucosal tissues. They can recognize specific antigens and contribute to host defense.
75
New cards
Describe how the recruitment of immune cells changes over the time course of an infection. How does this relate to their jobs?
* **Early Response (Immediate):** During the early stages of infection, innate immune cells like neutrophils and macrophages are quickly recruited to the site of infection. Neutrophils are among the first responders and play a critical role in phagocytosing pathogens.
* **Inflammatory Response (Hours to Days):** As the infection progresses, local tissue damage and pathogen presence lead to the release of inflammatory cytokines. These cytokines stimulate the recruitment of additional immune cells, including monocytes, dendritic cells, and more neutrophils. The goal is to enhance the immune response and clear the infection.
* **Adaptive Immune Response (Days to Weeks):** Over time, adaptive immune cells like B cells and T cells are activated and recruited. B cells produce antibodies, while cytotoxic T cells target infected cells. This adaptive response is highly specific and provides long-term immunity.
* **Resolution and Memory (Weeks to Months)**: **S**uccessful clearance of the infection leads to the resolution phase, during which immune cells are gradually reduced in number. However, some immune memory cells remain, providing rapid and specific responses upon re-exposure to the same pathogen.
The timing of immune cell recruitment corresponds to their roles. Innate immune cells act quickly to limit pathogen spread, while adaptive immune cells provide a more specific and durable defense.
* **Inflammatory Response (Hours to Days):** As the infection progresses, local tissue damage and pathogen presence lead to the release of inflammatory cytokines. These cytokines stimulate the recruitment of additional immune cells, including monocytes, dendritic cells, and more neutrophils. The goal is to enhance the immune response and clear the infection.
* **Adaptive Immune Response (Days to Weeks):** Over time, adaptive immune cells like B cells and T cells are activated and recruited. B cells produce antibodies, while cytotoxic T cells target infected cells. This adaptive response is highly specific and provides long-term immunity.
* **Resolution and Memory (Weeks to Months)**: **S**uccessful clearance of the infection leads to the resolution phase, during which immune cells are gradually reduced in number. However, some immune memory cells remain, providing rapid and specific responses upon re-exposure to the same pathogen.
The timing of immune cell recruitment corresponds to their roles. Innate immune cells act quickly to limit pathogen spread, while adaptive immune cells provide a more specific and durable defense.
76
New cards
\
Explain how NK cells identify the difference between healthy and infected cells
Explain how NK cells identify the difference between healthy and infected cells
* NK (Natural Killer) cells have a critical role in immune surveillance to detect and eliminate abnormal or infected cells.
* They use a balance of activating and inhibitory receptors to distinguish between healthy and infected cells.
* Healthy cells express MHC class I molecules on their surface. These molecules are recognized by inhibitory receptors on NK cells, sending a signal that prevents NK cell activation.
* Infected or stressed cells may down-regulate MHC class I expression as part of their defense mechanism or due to viral interference. This loss of MHC class I makes the cell less likely to inhibit NK cell activation.
* In addition to inhibitory receptors, NK cells also have activating receptors that can recognize stress-induced molecules on infected cells, such as NKG2D.
* When the balance tips towards activating signals outweighing inhibitory signals, NK cells become activated, leading to target cell lysis or apoptosis.
This balance of signals allows NK cells to identify and eliminate cells that have lost their normal MHC class I expression, a common feature of infected or cancerous cells, while sparing healthy cells with intact MHC class I expression
* They use a balance of activating and inhibitory receptors to distinguish between healthy and infected cells.
* Healthy cells express MHC class I molecules on their surface. These molecules are recognized by inhibitory receptors on NK cells, sending a signal that prevents NK cell activation.
* Infected or stressed cells may down-regulate MHC class I expression as part of their defense mechanism or due to viral interference. This loss of MHC class I makes the cell less likely to inhibit NK cell activation.
* In addition to inhibitory receptors, NK cells also have activating receptors that can recognize stress-induced molecules on infected cells, such as NKG2D.
* When the balance tips towards activating signals outweighing inhibitory signals, NK cells become activated, leading to target cell lysis or apoptosis.
This balance of signals allows NK cells to identify and eliminate cells that have lost their normal MHC class I expression, a common feature of infected or cancerous cells, while sparing healthy cells with intact MHC class I expression
77
New cards
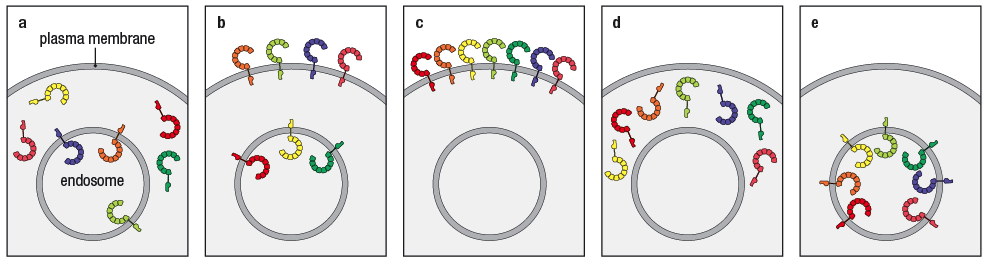
As a family, TLRs can recognize PAMPs associated with a broad array of different pathogens, including bacteria, viruses, and fungi. Patients with a specific susceptibility to herpesvirus infections have a defect in their ability to respond to viral nucleic acids using TLR-3, TLR-7, or TLR-9, even though these proteins are expressed in the patients’ cells.
Analysis of the TLRs in macrophages and dendritic cells from these patients showed a defect in membrane localization of these three TLRs.
Which of the following below show arrangements that would prevent these TLR's from doing their job properly?
\
Choose all that apply:
C
D
A
B
E
Analysis of the TLRs in macrophages and dendritic cells from these patients showed a defect in membrane localization of these three TLRs.
Which of the following below show arrangements that would prevent these TLR's from doing their job properly?
\
Choose all that apply:
C
D
A
B
E
Answer:
**C**
\
TLR-3,7&9 are endosomal TLRs and in this picture all TLRs are on the surface. This would produce TLRs but they would be in the wrong place to encounter the viral nucleic acids
**C**
\
TLR-3,7&9 are endosomal TLRs and in this picture all TLRs are on the surface. This would produce TLRs but they would be in the wrong place to encounter the viral nucleic acids
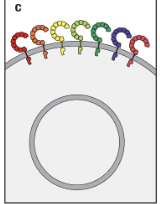
78
New cards
Macrophages express multiple types of receptors on their surface that stimulate phagocytosis of microbes, leading to pathogen internalization and destruction. Many of these receptors, such as Dectin-1, rely on direct recognition of a PAMP on the pathogen surface. However, some receptors that stimulate phagocytosis rely on soluble factors (not associated with the phagocyte membrane) to identify and mark the pathogen for uptake by the phagocyte. That would include which of the following?
\
Select all that Apply:
\
a. The class A scavenger receptor
b. The complement receptor
c. The Fc Receptor
d. The Macrophage C-type lectin receptor
e. The mannose receptor
\
\
Select all that Apply:
\
a. The class A scavenger receptor
b. The complement receptor
c. The Fc Receptor
d. The Macrophage C-type lectin receptor
e. The mannose receptor
\
b. The complement receptor
c. The Fc Receptor
\
c. The Fc Receptor
\
79
New cards
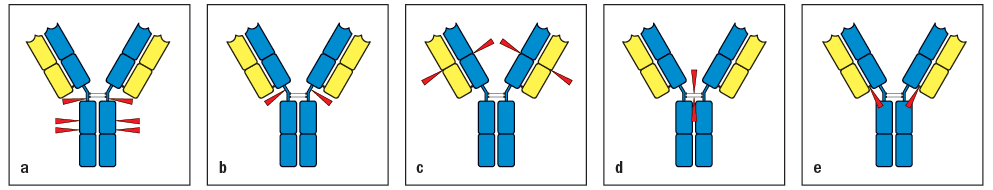
Early studies analyzing the antibody protein fragments generated after proteolytic cleavage revealed important information about the overall structure of the antibody molecule. Which cleavage pattern (indicated by the red triangles in Figure Below) yields a fragment that has lower antigen-binding avidity than the intact antibody?
\
Select all that apply:
A
D
C
E
B
\
Select all that apply:
A
D
C
E
B
Answers:
\
**D.**
**C.**
**B.**
\
**D.**
**C.**
**B.**
80
New cards
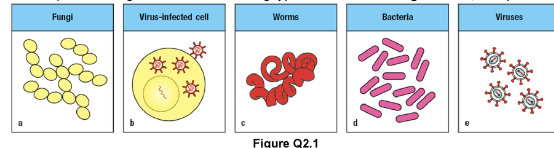
Antibodies, complement proteins, and phagocytic cells provide effective protection against all of the following types of infections in the pictures below except:
1. Fungi
2. Virus-infected cell
3. Worms
4. Bacteria
5. Viruses
Options:
a. Antibodies, compliment, and Phagocytes
b. Antibodies and phagocytes
c. Antibodies and compliment
d. Antibodies, compliment, and Phagocytes
E. Antibodies
1. Fungi
2. Virus-infected cell
3. Worms
4. Bacteria
5. Viruses
Options:
a. Antibodies, compliment, and Phagocytes
b. Antibodies and phagocytes
c. Antibodies and compliment
d. Antibodies, compliment, and Phagocytes
E. Antibodies
1. **Fungi**: Antibodies, compliment, and Phagocytes
2. **Virus-**infected cell: Antibodies and phagocytes
3. **Worms**: Antibodies and compliment
4. **Bacteria:** Antibodies, compliment, and Phagocytes
5. **Viruses:** Antibodies
\
81
New cards
Which of the following __does__ occur during an inflammatory response?
\
Choose all that Apply:
a. Tissue injury repair
b. Decreased vascular permeability
c. Local blood clotting
d. Increased heart rate
e. Trafficking of __lymphocytes__ to the site of injure
\
Choose all that Apply:
a. Tissue injury repair
b. Decreased vascular permeability
c. Local blood clotting
d. Increased heart rate
e. Trafficking of __lymphocytes__ to the site of injure
a. Tissue injury repair
c. Local blood clotting
e. Trafficking of __lymphocytes__ to the site of injure
\
Blood clotting stops the injury and blood loss but also attempts to localize the infective agents to the tissue with the injury.
Tissue repair is an important part of the inflammatory process because not only is infection often associated with tissue damage but also because the inflammatory process does damage to the surrounding tissue.
ILC's as well as NK cells are innate immune cells which are lymphocytes and trafficked to the site of inflammation to fight off a pathogen.
c. Local blood clotting
e. Trafficking of __lymphocytes__ to the site of injure
\
Blood clotting stops the injury and blood loss but also attempts to localize the infective agents to the tissue with the injury.
Tissue repair is an important part of the inflammatory process because not only is infection often associated with tissue damage but also because the inflammatory process does damage to the surrounding tissue.
ILC's as well as NK cells are innate immune cells which are lymphocytes and trafficked to the site of inflammation to fight off a pathogen.
82
New cards
Describe the structure of an antibody. Be able to \n identify the heavy and light chain as well as variable \n and constant regions
* __**Antibody Structure:**__
* Antibodies are Y-shaped proteins, also known as immunoglobulins.
* Each antibody consists of four polypeptide chains - two identical heavy chains and two identical light chains.
* The heavy chains are larger and have more complex structures compared to the light chains.
* __**Heavy and Light Chains Identification:**__
* **Heavy Chains:**
* Provide structural support and stability.
* Determine the antibody's class (IgG, IgM, IgA, etc.).
* Recognizable by their larger size.
* **Light Chains:**
* Lighter in weight and size.
* Exist in two types: kappa (κ) and lambda (λ).
* __**Variable and Constant Regions:**__
* **Variable Regions:**
* Found at the ends of both heavy and light chains.
* Highly diverse in amino acid sequence, allowing recognition of different antigens.
* Form antigen-binding sites.
* **Constant Regions:**
* Found in the stem of the Y-shaped antibody.
* More uniform in amino acid sequence within a particular class of antibodies.
* Determine the antibody's effector functions.
* Antibodies are Y-shaped proteins, also known as immunoglobulins.
* Each antibody consists of four polypeptide chains - two identical heavy chains and two identical light chains.
* The heavy chains are larger and have more complex structures compared to the light chains.
* __**Heavy and Light Chains Identification:**__
* **Heavy Chains:**
* Provide structural support and stability.
* Determine the antibody's class (IgG, IgM, IgA, etc.).
* Recognizable by their larger size.
* **Light Chains:**
* Lighter in weight and size.
* Exist in two types: kappa (κ) and lambda (λ).
* __**Variable and Constant Regions:**__
* **Variable Regions:**
* Found at the ends of both heavy and light chains.
* Highly diverse in amino acid sequence, allowing recognition of different antigens.
* Form antigen-binding sites.
* **Constant Regions:**
* Found in the stem of the Y-shaped antibody.
* More uniform in amino acid sequence within a particular class of antibodies.
* Determine the antibody's effector functions.
83
New cards
Understand the different fragments of an immunoglobulin.
__**Immunoglobulin Fragments:**__
* **Fc (Crystallizable Fragment):**
* Stem of the Y-shaped antibody.
* Determines the antibody's class and effector functions (e.g., activation of complement, binding to Fc receptors on immune cells).
* **Fab (Antigen-Binding Fragment):**
* The "arms" of the Y-shaped antibody.
* Contains the variable regions responsible for binding to antigens.
* **F(ab’)2:**
* A fragment that results from the cleavage of an antibody at the hinge region.
* Contains two Fab regions.
* **pFc’:**
* Fragment resulting from cleavage at the hinge region.
* Contains the Fc region and part of the Fab region.
* **Fc (Crystallizable Fragment):**
* Stem of the Y-shaped antibody.
* Determines the antibody's class and effector functions (e.g., activation of complement, binding to Fc receptors on immune cells).
* **Fab (Antigen-Binding Fragment):**
* The "arms" of the Y-shaped antibody.
* Contains the variable regions responsible for binding to antigens.
* **F(ab’)2:**
* A fragment that results from the cleavage of an antibody at the hinge region.
* Contains two Fab regions.
* **pFc’:**
* Fragment resulting from cleavage at the hinge region.
* Contains the Fc region and part of the Fab region.
84
New cards
Identify the hypervariable regions and their effect on binding.
* Also known as Complementarity Determining Regions (CDRs).
* Found in the variable regions of both heavy and light chains.
* Form the antigen-binding site.
* Have high diversity in amino acid sequences.
* Contribute significantly to antigen specificity and binding affinity.
* Found in the variable regions of both heavy and light chains.
* Form the antigen-binding site.
* Have high diversity in amino acid sequences.
* Contribute significantly to antigen specificity and binding affinity.
85
New cards
Explain how the shape of the CDR relates to the size and shape of the antigen
* The CDRs are flexible loops at the tips of the variable regions.
* The shape and size of the CDRs must complement the shape and size of the antigen for effective binding.
* This "lock-and-key" fit ensures specific and tight binding between the antibody and antigen.
* The shape and size of the CDRs must complement the shape and size of the antigen for effective binding.
* This "lock-and-key" fit ensures specific and tight binding between the antibody and antigen.
86
New cards
Know the different forces which shape antigen – antibody binding.
__**Forces in Antigen-Antibody Binding:**__
* **Van der Waals Forces:**
* Weak electrostatic forces between atoms in close proximity.
* **Hydrogen Bonds:**
* Attraction between a hydrogen atom covalently bonded to an electronegative atom and another electronegative atom.
* **Ionic Bonds:**
* Attraction between positively and negatively charged ions.
* **Hydrophobic Interactions:**
* Nonpolar molecules are driven together in an aqueous environment.
* **Covalent Bonds** (less common in antigen-antibody binding).
* **Van der Waals Forces:**
* Weak electrostatic forces between atoms in close proximity.
* **Hydrogen Bonds:**
* Attraction between a hydrogen atom covalently bonded to an electronegative atom and another electronegative atom.
* **Ionic Bonds:**
* Attraction between positively and negatively charged ions.
* **Hydrophobic Interactions:**
* Nonpolar molecules are driven together in an aqueous environment.
* **Covalent Bonds** (less common in antigen-antibody binding).
87
New cards
Understand the steric restrictions to antibody binding.
* Refers to the spatial arrangement and shape of molecules.
* Antibodies have a specific three-dimensional structure.
* Binding is highly dependent on the complementary shapes of the antibody and antigen.
* Large or bulky antigens may not fit into the antigen-binding site of the antibody
* Antibodies have a specific three-dimensional structure.
* Binding is highly dependent on the complementary shapes of the antibody and antigen.
* Large or bulky antigens may not fit into the antigen-binding site of the antibody
88
New cards
Explain the difference between polyclonal and monoclonal antibodies and their importance in immunity and medicine.
* **Polyclonal Antibodies:**
* Produced by multiple B cell clones in response to a complex antigen.
* Contain a mixture of different antibodies, each recognizing a different epitope on the antigen.
* More diverse in their antigen-binding specificity.
* Used in various laboratory applications.
* **Monoclonal Antibodies:**
* Produced by a single B cell clone.
* Highly specific, as they recognize a single epitope on an antigen.
* Often created using hybridoma technology.
* Widely used in diagnostic tests, therapeutic treatments, and research.
* **Importance:**
* Polyclonal antibodies are useful for detecting a broad range of epitopes on complex antigens.
* Monoclonal antibodies provide high specificity and are crucial in precision medicine, such as targeted cancer therapies.
* Produced by multiple B cell clones in response to a complex antigen.
* Contain a mixture of different antibodies, each recognizing a different epitope on the antigen.
* More diverse in their antigen-binding specificity.
* Used in various laboratory applications.
* **Monoclonal Antibodies:**
* Produced by a single B cell clone.
* Highly specific, as they recognize a single epitope on an antigen.
* Often created using hybridoma technology.
* Widely used in diagnostic tests, therapeutic treatments, and research.
* **Importance:**
* Polyclonal antibodies are useful for detecting a broad range of epitopes on complex antigens.
* Monoclonal antibodies provide high specificity and are crucial in precision medicine, such as targeted cancer therapies.
89
New cards
Describe the five different subclasses of antibodies and how their differences relate to their functional differences.
1. **IgM:**
* Pentameric structure, first antibody produced during an immune response.
* Efficient at agglutinating pathogens and activating complement.
2. **IgG:**
* Most abundant antibody in the bloodstream.
* Provides long-lasting immunity and crosses the placenta to protect developing fetuses.
3. **IgA:**
* Found in bodily secretions (saliva, tears, mucus).
* Provides localized immunity on mucosal surfaces.
4. **IgE:**
* Involved in allergic reactions and defense against parasitic infections.
* Binds to mast cells and basophils, triggering release of inflammatory mediators.
5. **IgD:**
* Found on the surface of B cells.
* Exact function is less clear but may play a role in B cell activation.
90
New cards
Know the TCRα:β heterodimer and its similarity to the Fab fragment of immunoglobulin.
* T Cell Receptor composed of two chains, α and β.
* Similar to Fab fragment of immunoglobulin in that it recognizes antigenic peptides.
* Similar to Fab fragment of immunoglobulin in that it recognizes antigenic peptides.
91
New cards
\
Understand the limitations in how the TCR interacts with its antigen.
Understand the limitations in how the TCR interacts with its antigen.
* TCRs can only recognize peptides presented by MHC molecules.
* The interaction is highly specific and requires a precise fit between the TCR, peptide, and MHC molecule.
* TCRs have limited diversity compared to antibodies due to a more restricted genetic recombination process.
* The interaction is highly specific and requires a precise fit between the TCR, peptide, and MHC molecule.
* TCRs have limited diversity compared to antibodies due to a more restricted genetic recombination process.
92
New cards
Describe the different classes of MHC molecules.
* **MHC Class I:**
* Found on the surface of all nucleated cells.
* Presents peptides derived from intracellular proteins (e.g., viral proteins).
* Composed of one alpha chain (encoded by HLA-A, -B, or -C gene) and one beta-2 microglobulin chain.
* **MHC Class II:**
* Found primarily on antigen-presenting cells (e.g., dendritic cells, macrophages, B cells).
* Presents peptides derived from extracellular proteins (e.g., bacterial proteins).
* Composed of an alpha chain (encoded by HLA-DP, -DQ, or -DR gene) and a beta chain.
\
* Found on the surface of all nucleated cells.
* Presents peptides derived from intracellular proteins (e.g., viral proteins).
* Composed of one alpha chain (encoded by HLA-A, -B, or -C gene) and one beta-2 microglobulin chain.
* **MHC Class II:**
* Found primarily on antigen-presenting cells (e.g., dendritic cells, macrophages, B cells).
* Presents peptides derived from extracellular proteins (e.g., bacterial proteins).
* Composed of an alpha chain (encoded by HLA-DP, -DQ, or -DR gene) and a beta chain.
\
93
New cards
Explain the difference between peptides which bind to MHC I and MHC II.
* **MHC I:**
* Binds peptides derived from endogenous proteins, typically those within the cell.
* Presents peptides to CD8+ cytotoxic T cells.
* Peptides are usually 8-10 amino acids long.
* **MHC II:**
* Binds peptides derived from exogenous proteins, typically from outside the cell.
* Presents peptides to CD4+ helper T cells.
* Peptides can be longer, often 13-25 amino acids.
\
* Binds peptides derived from endogenous proteins, typically those within the cell.
* Presents peptides to CD8+ cytotoxic T cells.
* Peptides are usually 8-10 amino acids long.
* **MHC II:**
* Binds peptides derived from exogenous proteins, typically from outside the cell.
* Presents peptides to CD4+ helper T cells.
* Peptides can be longer, often 13-25 amino acids.
\
94
New cards
Understand how MHC heredity is generated from parents to their children and how this impacts their immune systems.
**MHC Alleles:**
* Inherited from both parents.
* Individuals can have multiple different alleles for each MHC gene (one from each parent).
* This diversity in MHC alleles contributes to an individual's ability to present a wide range of peptides.
* Inherited from both parents.
* Individuals can have multiple different alleles for each MHC gene (one from each parent).
* This diversity in MHC alleles contributes to an individual's ability to present a wide range of peptides.
95
New cards
\
Know how the CD4 and CD8 cell-surface proteins of T cells directly contact MHC molecules and are required to make an effective response to antigen.
Know how the CD4 and CD8 cell-surface proteins of T cells directly contact MHC molecules and are required to make an effective response to antigen.
* **CD4:**
* Binds to MHC class II molecules.
* Found on helper T cells.
* Enhances the interaction between T cells and antigen-presenting cells.
* **CD8:**
* Binds to MHC class I molecules.
* Found on cytotoxic T cells.
* Enhances the interaction between T cells and infected cells.
* Binds to MHC class II molecules.
* Found on helper T cells.
* Enhances the interaction between T cells and antigen-presenting cells.
* **CD8:**
* Binds to MHC class I molecules.
* Found on cytotoxic T cells.
* Enhances the interaction between T cells and infected cells.
96
New cards
Understand the difference in expression of MHC I and MHC II on various cells of the body.
* **MHC I:**
* Expressed on almost all nucleated cells.
* Presents peptides from proteins produced within the cell.
* **MHC II:**
* Mainly expressed on antigen-presenting cells (dendritic cells, macrophages, B cells).
* Presents peptides from proteins acquired from the extracellular environment.
* \
* Expressed on almost all nucleated cells.
* Presents peptides from proteins produced within the cell.
* **MHC II:**
* Mainly expressed on antigen-presenting cells (dendritic cells, macrophages, B cells).
* Presents peptides from proteins acquired from the extracellular environment.
* \
97
New cards
\
Know about the distinct subset of T cells bears an alternative receptor made up of γ and δ chains and how they differ in form and function than their counterparts.
Know about the distinct subset of T cells bears an alternative receptor made up of γ and δ chains and how they differ in form and function than their counterparts.
γδ T Cells:
* Possess TCRs composed of gamma (γ) and delta (δ) chains.
* Less common than αβ T cells (the typical T cell subtype).
* Often found in mucosal tissues and have diverse functions, including rapid response to stress-induced antigens.
* Possess TCRs composed of gamma (γ) and delta (δ) chains.
* Less common than αβ T cells (the typical T cell subtype).
* Often found in mucosal tissues and have diverse functions, including rapid response to stress-induced antigens.
98
New cards
Describe how genes are used to encode antibody variability.
Antibody variability is achieved through a process called somatic recombination. This process involves the rearrangement of gene segments within the immunoglobulin genes in the progenitors of antibody-producing cells. Multiple V (Variable), D (Diversity), and J (Joining) gene segments are present at each immunoglobulin locus. During somatic recombination, these segments are rearranged to form a unique combination, leading to the generation of diverse antibodies.
99
New cards
Explain how the V(D)J and C segments of the immunoglobulin gene relate to the structure of an antibody.
The V(D)J segments code for the variable region of the antibody, which is responsible for binding to specific antigens. These segments determine the antigen-binding specificity of the antibody. The C (Constant) segments, on the other hand, code for the constant region of the antibody, which is involved in various effector functions such as complement activation and binding to immune cells. The combination of the V(D)J region and the C region determines the overall structure and function of the antibody.
100
New cards
Understand the difference between heavy and light chain gene segments.
Immunoglobulin molecules are composed of two types of chains: heavy chains and light chains. Heavy chain genes encode the larger, structurally more complex portion of the antibody. They consist of V, D, and J segments. Light chain genes encode the smaller portion of the antibody and consist only of V and J segments, lacking a D segment. The combination of heavy and light chains contributes to the diversity and specificity of the antibody repertoire.