GI Malignancies
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
92 Terms
In TNM staging, what does T, N, and M stand for?
T = Tumor size
N = Lymph node involvement
M = Metastasis
What is the most common type of esophageal cancer in the US?
Adenocarcinoma
What is the most common type of esophageal cancer worldwide?
Squamous cell carcinoma
Is esophageal cancer more common in males or females?
Males
What is associated with SCC?
Chronic alcohol use and smoking
More common in African Americans
Most people with esophageal cancer present with ---------------- disease.
advanced
In esophageal cancer, what causes hoarseness?
Recurrent laryngeal N.
Which type of esophageal carcinoma is associated with Barrett's esophagus?
Adenocarcinoma
What does it mean when someone with esophageal cancer has supraclavicular or cervical LAD and hepatomegaly?
The patient has metastatic disease
What labs do you order in someone with esophageal cancer?
Anemia
Nonspecific labs
- Increased LFTs, ALP = hepatic or boney metastasis
- Hypoalbuminemia = Malnutrition
What imaging do you order in someone with esophageal cancer?
- Barium esophagram
- CXR
- Upper endoscopy --> Biopsy
What scan would you order to determine the staging for esophageal cancer?
CT with contrast
Endoscopic ultrasound with guided fine needle aspiration biopsy
How do you treat curable esophageal cancer?
This depends on the staging.
If its curable then surgery and chemo and radiation can be used
How do you treat incurable esophageal cancer?
Chemotherapy
Chemoradiation
What is the 3rd most common cancer death worldwide?
Gastric Adenocarcinoma
What are the two types of gastric adenocarcinoma?
Intestinal
Diffuse
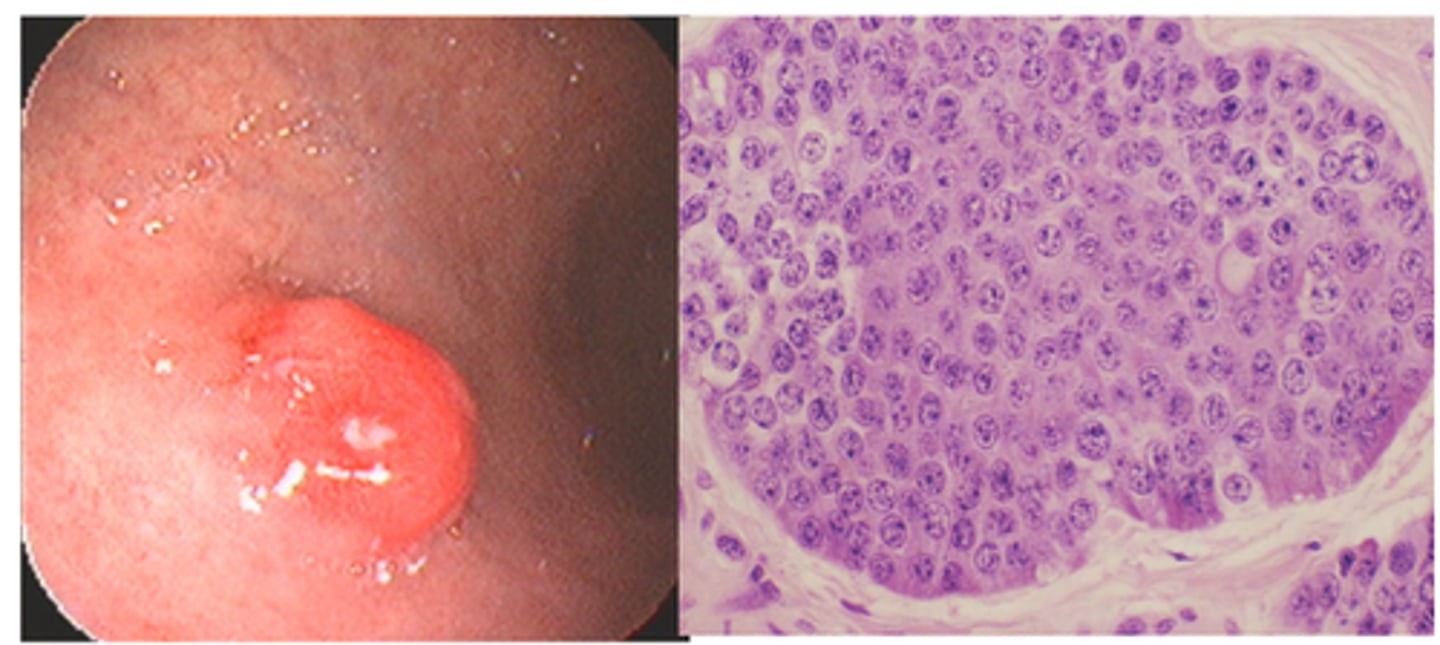
Which type of gastric adenocarcinoma forms grandular structures?
Intestinal adenocarcinoma
Which type of gastric adenocarcinoma lacks glandular formation?
Diffuse
Its poorly differentiated, signet-ring cells, and lacks glandular formation
What is the most common type of gastric adenocarcinoma?
Intestinal
What is the strongest risk factor for gastric adenocarcinoma?
Chronic H. Pylori = Strongest risk factor
Who is diffuse type gastric adenocarcinoma most common in?
M = F
Its more common in younger patients
Which type of gastric adenocarcinoma is NOT associated with H. Pylori?
Diffuse type
Which part of the stomach do gastric cancers arise from?
Body and antrum
What is the most favorable prognosis gastric adenocarcinoma morphology?
Superficial spreading
Where is virchow node?
gastric adenocarcinoma
L supraventricular LAD
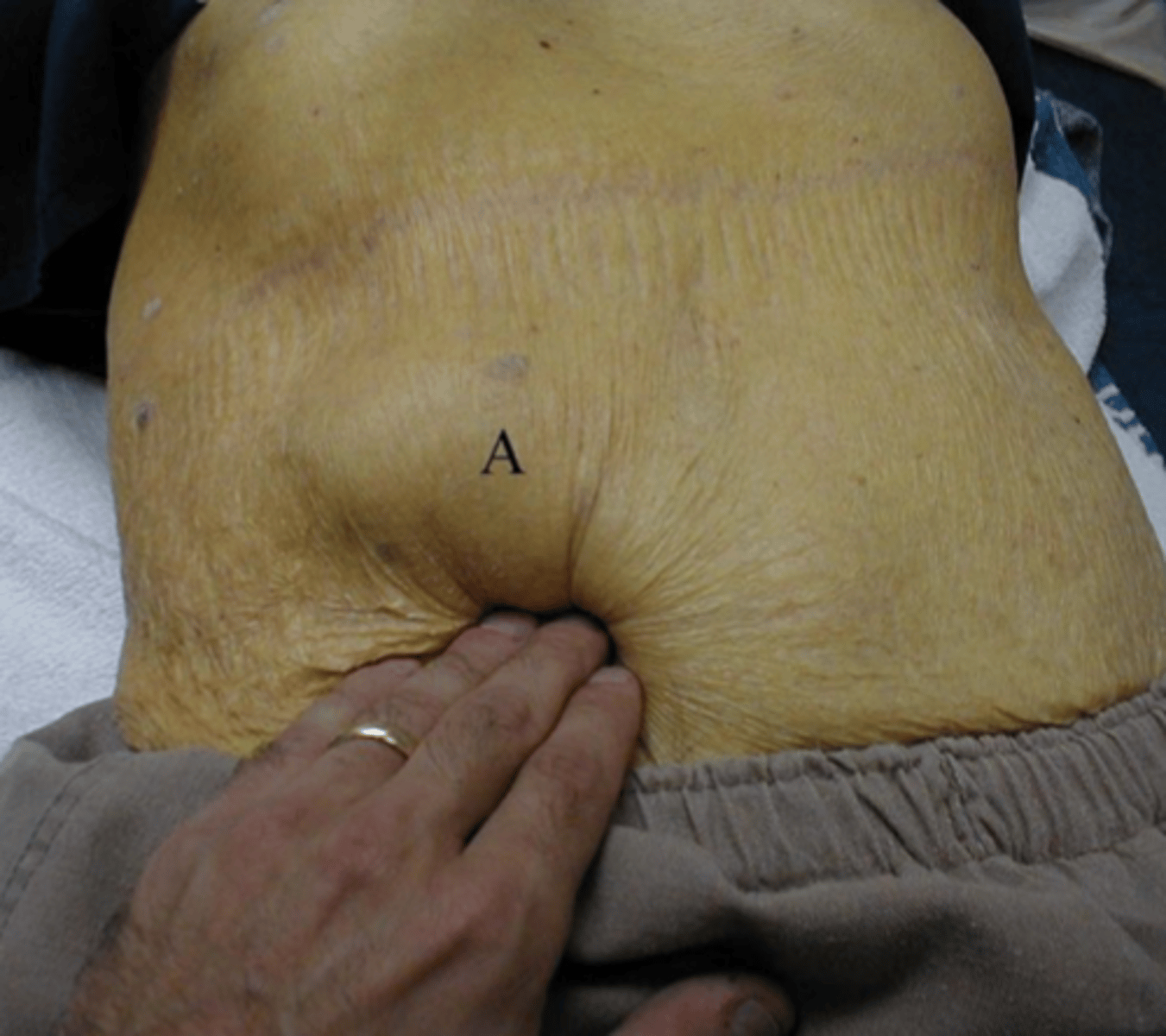
Where is sister mary joseph node?
umbilical nodule
Where is Blumer's shelf?
right rectal shelf
Where is krukenburg tumor?
ovarian mets
Found in gastric adenocarcinoma
What labs can you order to assess for adenocarcinoma?
CBC: Anemia or blood loss
Elevated LFTs, ALP = hepatic or bony mets
HER2 amplication and overexpression
What imaging could you order if you suspect gastric adenocarcinoma?
Upper endoscopy
CT with contrast
Gastric adenocarcinoma will have which tumor markers?
MSI
dMMR
PD-L1 - determines if tumor will respond to immunotherapy
HER2
How do you treat gastric adenocarcinoma?
Surgical resection
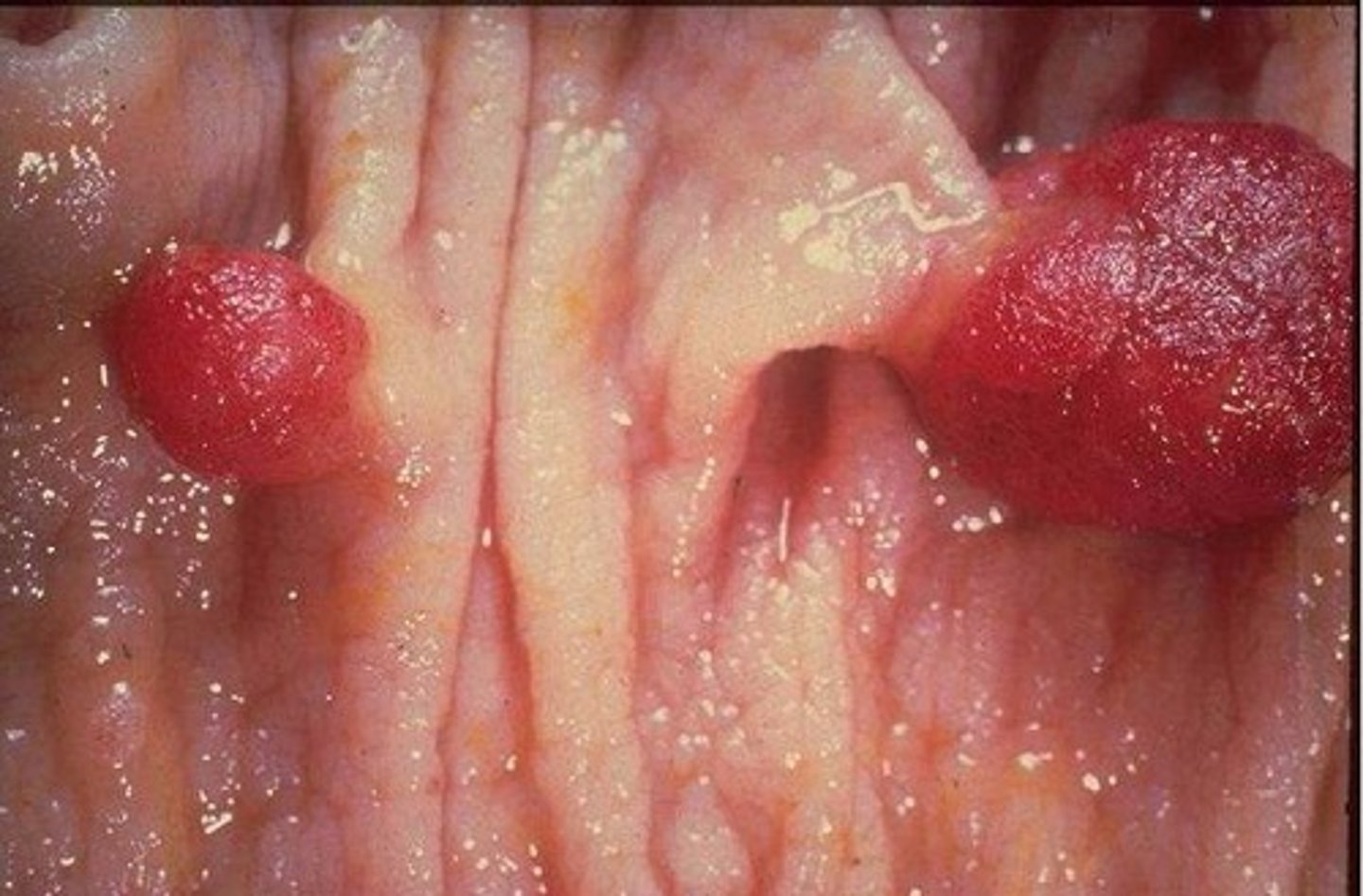
What are the majority of gastric neuroendocrine tumors caused by?
hypergastrinemia
and are associated with pernicious anemia or zollinger-ellison syndrome
Differentiate the three different types of gastric neuroendocrine tumors.
Type 1 - Chronic atrophic gastritis
Type 2 - Zollinger-Ellison Syndrome
Type 3 - Not related to gastrin secretion
What lab work do you order for someone with gastric neuroendocrine tumor?
serum gastrin level
Upper endoscopy
A 68-year-old man presents with progressive solid food dysphagia, 20-pound weight loss, and hoarseness. He also reports a chronic cough. Exam reveals supraclavicular lymphadenopathy.
What is the most likely diagnosis?
A) Achalasia
B) GERD
C) Esophageal cancer
D) Zenker's diverticulum
What is causing the hoarseness in his voice?
What are some labs you can order to confirm your suspected diagnosis?
What imagining do you order?
How do you treat this patient?
1.C) Esophageal cancer
2.) His recurrent laryngeal nerve is involved. This is causing the hoarseness in his voice.
3.) Hypoalbuminemia would likely be present due to malnutrition.
He might have anemia and elevated LFTs if it has metastasize to the liver.
4.) We can order a barium esophagram, CXR, or upper endoscopy biopsy.
To determine stating you should order a CT with contrast. If you suspect metastasis then get a biopsy. Endoscopic ultrasound with guided fine needle aspiration biopsy would also be useful to obtain.
5.) If its curable you can do chemo +/- radiation.
What 3rd most common cancer death worldwide?
Gastric adenocarcinoma
A 34-year-old woman presents with early satiety, unintentional weight loss, and persistent epigastric discomfort. She has no history of smoking, alcohol use, or chronic H. pylori infection. Physical exam reveals mild abdominal distention but no palpable mass. An upper endoscopy reveals diffuse thickening of the stomach wall without a discrete mass. Biopsy shows poorly differentiated signet ring cells.
Which of the following is most likely true about this patient's condition?
A) It is strongly associated with environmental exposures
B) It occurs equally in men and women
C) It is almost always linked to chronic H. pylori infection
D) It primarily affects elderly patients
B) It occurs equally in men and women
The patient has diffuse type gastric adenocarcinoma
A 69-year-old man presents with progressive epigastric pain, unintentional weight loss, and new onset iron-deficiency anemia. He has a long-standing history of smoking and frequent consumption of smoked and pickled foods. Upper endoscopy reveals an ulcerated mass in the antrum of the stomach. Biopsy confirms the diagnosis of moderately differentiated adenocarcinoma.
Which of the following is most strongly associated with this patient's condition?
A) Chronic Helicobacter pylori infection
B) Germline CDH1 mutation
C) Prior gastric bypass surgery
D) Alcoholic liver disease
A) Chronic Helicobacter pylori infection
The patient has intestinal type gastric adenocarcinoma. Note that this type of carcinoma is the most common type.
A 63-year-old man presents with complaints of early satiety, progressive weight loss, and vague epigastric discomfort over the past three months. He also reports intermittent episodes of dark, tarry stools. Physical examination reveals a firm, palpable left supraclavicular lymph node. Laboratory studies show iron-deficiency anemia. An upper endoscopy reveals an ulcerated mass in the stomach.
Which of the following findings would most likely be seen if the disease has metastasized to the ovaries?
A) Sister Mary Joseph nodule
B) Blumer's shelf
C) Krukenberg tumor
D) Virchow node
What does this patient have?
What tumor markers would this person have?
How do you treat this condition?
C) Krukenberg tumor
1.) This patient has gastric adenocarcinoma
2.) HER2
- You would also evaluate for dMMR, PD-L1
3.) Surgical resection is the only therapy with curative potential
A 58-year-old woman presents with a 6-month history of vague upper abdominal discomfort and early satiety. She also reports occasional flushing and chronic diarrhea. Past medical history is significant for pernicious anemia requiring B12 injections. Upper endoscopy reveals a small, firm, submucosal nodule in the gastric body. Biopsy confirms a well-differentiated neuroendocrine tumor.
Which of the following is most likely elevated in this patient?
A) Carcinoembryonic antigen (CEA)
B) Gastrin
C) Alpha-fetoprotein (AFP)
D) CA-19-9
What is the diagnosis?
B) Gastrin
Gastric neuroendocrine tumor
Non-hodgkin's b cell and diffuse B cell are which type of gastric lymphomas?
Primary gastric lymphomas
A 59-year-old man presents with abdominal discomfort, early satiety, and a 15-pound unintentional weight loss over the past two months. He also reports intermittent melena. Upper endoscopy reveals a large ulcerated lesion in the stomach. Biopsies demonstrate dense lymphocytic infiltration consistent with gastric lymphoma. Testing for H. pylori is positive.
What is the first-line management for this patient?
A) Immediate surgical resection
B) H. pylori eradication therapy
C) Chemotherapy with R-CHOP
D) Radiation therapy
B) H. pylori eradication therapy
Note that occasional use of radiation therapy and surgical resection is NOT recommended for patients with gastric lymphoma.
A 61-year-old woman presents with vague upper abdominal pain, early satiety, and a 10-pound weight loss over 3 months. She reports intermittent episodes of melena but denies hematemesis. Physical exam is unremarkable. Upper endoscopy reveals an ulcerated mass lesion in the body of the stomach. Biopsies show lymphoid infiltration suspicious for gastric lymphoma.
Which laboratory test would be most appropriate to order next?
Which imaging study should be performed for staging?
What is the preferred diagnostic method to confirm gastric lymphoma?
What is the initial management if H. pylori infection is confirmed?
1.) H. pylori testing
2.) CT of the chest, abdomen, and pelvis
3.) B) EUS with biopsy
4.) C) H. pylori eradication therapy
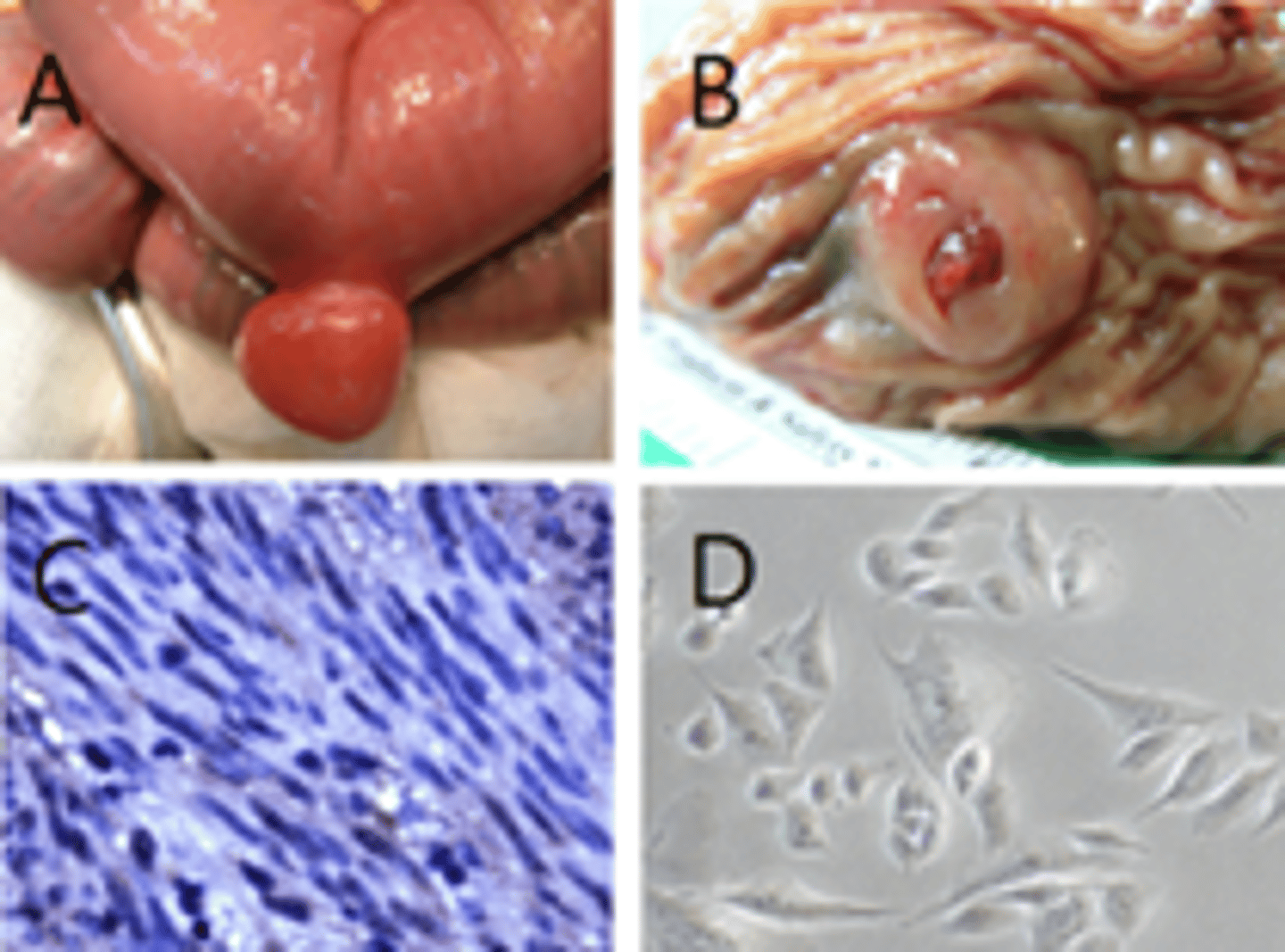
How would you manage a mesenchymal tumor that is less then 2cm?
EUS surveillance
How would you manage a mesenchymal tumor that is greater then 2 cm?
Surgery
A 60-year-old man undergoes an upper endoscopy for evaluation of vague upper abdominal pain. During the procedure, a 2.5 cm submucosal mass is incidentally discovered in the gastric fundus. He denies weight loss, bleeding, or obstructive symptoms. Biopsies are taken. Histology shows spindle-shaped cells consistent with a gastrointestinal stromal tumor (GIST).
Which diagnostic method is most appropriate to confirm the diagnosis?
Which imaging modality is recommended to assess for extent of disease?
How should this tumor be managed based on its size?
1. EUS with fine-needle aspiration (FNA) biopsy
2.) CT Abdomen/Pelvis with contrast
3.) Since the tumor is greater then 2cm it should be surgically removed
Where are small intestinal adenocarcinomas most commonly found?
Duodenum or proximal jejunum
What is the most common site of small bowel carcinoma?
Ampulla of Vater
A 64-year-old man presents with progressive jaundice, dark urine, and pale stools over several weeks. He also reports mild right upper quadrant discomfort and an unintended 10-pound weight loss. Physical exam reveals scleral icterus. Laboratory studies show elevated total and direct bilirubin levels. Imaging reveals a mass at the ampulla of Vater causing bile duct obstruction.
What does this patient have?
What is causing the jaundice?
How do you manage this patient?
1.) Small intestinal adenocarcinoma
2.) Jaundice due to bile duct obstruction or bleeding.
3.) Early lesions are eligible for surgical resection. Chemo +/- radiation may be necessary
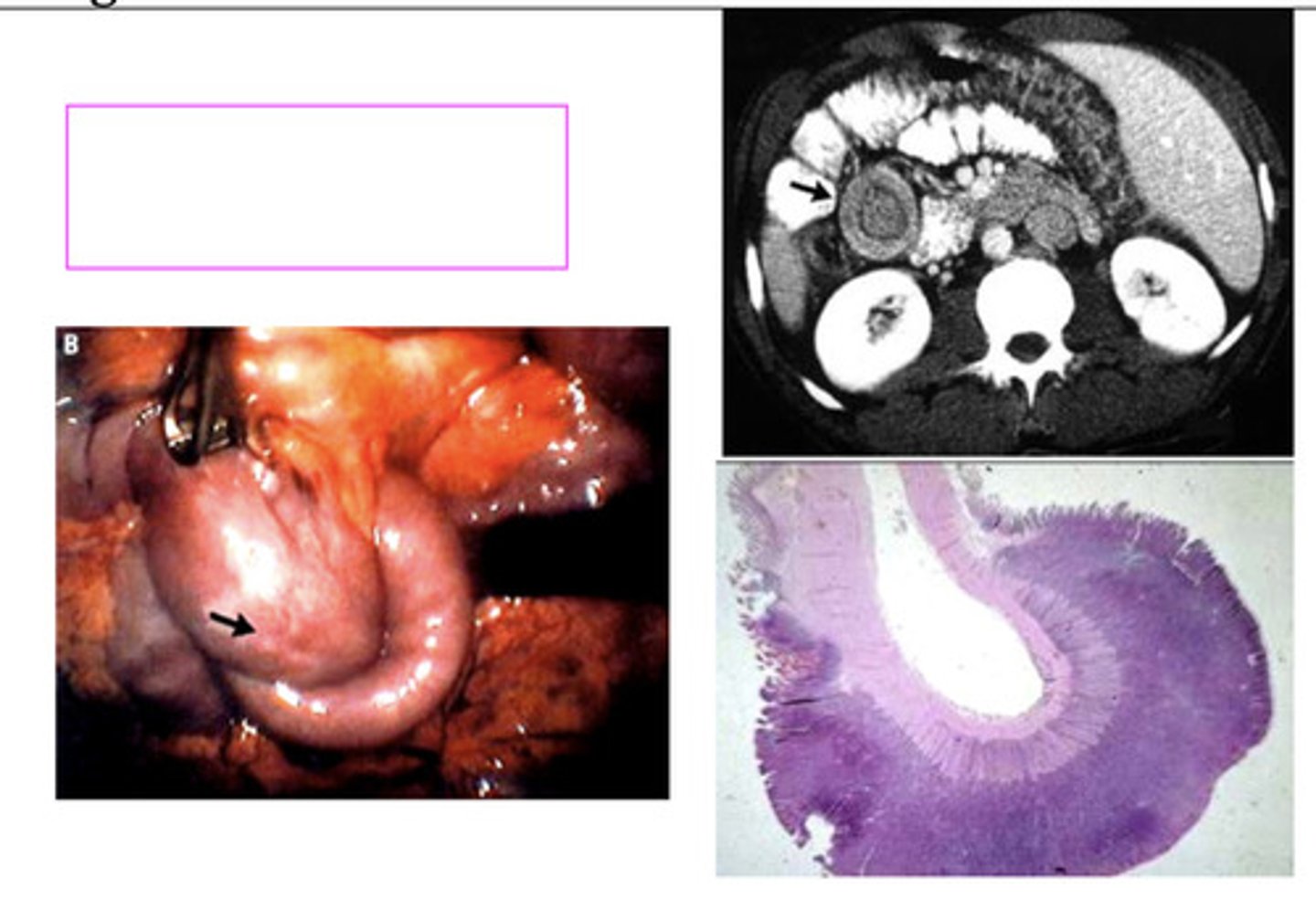
What is the most common location for GI intestinal neuroendocrine tumors?
Small intestine
- Most common in the distal ileum
A 55-year-old woman presents with episodic facial flushing, wheezing, diarrhea, and abdominal cramping over the past few months. She denies any recent travel or dietary changes. On physical exam, she has telangiectasias on her face and mild lower extremity edema. CT imaging shows multiple liver lesions and a small mass in the distal ileum.
Which serum marker would be most useful to support the diagnosis?
A) Carcinoembryonic antigen (CEA)
B) 5-HIAA (5hydroxyindoleacetic acid) in a 24-hour urine collection
C) Alpha-fetoprotein (AFP)
D) CA 19-9
What other serum marker not listed would also be useful to support this diagnosis?
What is likely the diagnosis?
What imaging should you order for diagnosis?
What imaging should you order for staging and determine if tumors will respond to somatostatin therapy?
What is the treatment?
B) 5-HIAA (5hydroxyindoleacetic acid) and platelet serotonin. This is elevated in patients with metastatic disease.
1.) Chromogranin A (CgA) is elevated in most NETs
2.) Intestinal Neuroendocrine Tumor
3.) CT abdomen with contrast
4.) You can do a somatostatin receptor scintigraphy and DOTATATE PET scan
5.) If this patient just had tumors confined to the small intestine you could do surgical resection. Unfortunately this patient has a more advanced disease. Since this patient is symptomatic you should use a long acting somatostatin analog. If the patient were asymptomatic you would want to wait until they are symptomatic before starting therapy.
A 65-year-old man presents with a 3-month history of abdominal pain, diarrhea, unintentional weight loss, and intermittent nausea. He also notes blood-tinged stools. Physical exam reveals mild abdominal distention and pallor. Laboratory studies reveal microcytic anemia and hypoalbuminemia. A barium small bowel study shows an irregular, partially obstructing mass in the ileum.
Which laboratory findings are most commonly associated with this disease?
A) Elevated alkaline phosphatase and hypercalcemia
B) Anemia and hypoalbuminemia
C) Elevated lipase and amylase
D) Leukocytosis and thrombocytosis
What imaging modality is most appropriate to assess the extent of disease?
A) CT enterography or barium radiography
B) Non-contrast abdominal X-ray
C) MRI brain
How is the diagnosis of small intestine lymphoma confirmed?
1.) B) Anemia and hypoalbuminemia
2.) B) CT enterography
3.) B) Endoscopic biopsy of the mass
What is the most common location of small intestine sarcoma?
Jejunum and Ileum
What causes small intestine sarcoma?
Human Herpes Virus 8
A 49-year-old man presents with unintentional weight loss and intermittent episodes of melena over the past few months. He denies changes in bowel habits or significant abdominal pain. Past medical history is significant for HIV infection. Physical examination is unremarkable. Imaging reveals a large mass in the ileum arising within a Meckel's diverticulum. Biopsy of the lesion reveals spindle cells consistent with sarcoma, and PCR testing detects Human Herpesvirus 8 (HHV-8).
What is the most likely diagnosis?
How do you treat it?
1.) Small intestine sarcoma
2.) Treatment ranges from chemo to surgery or radiation
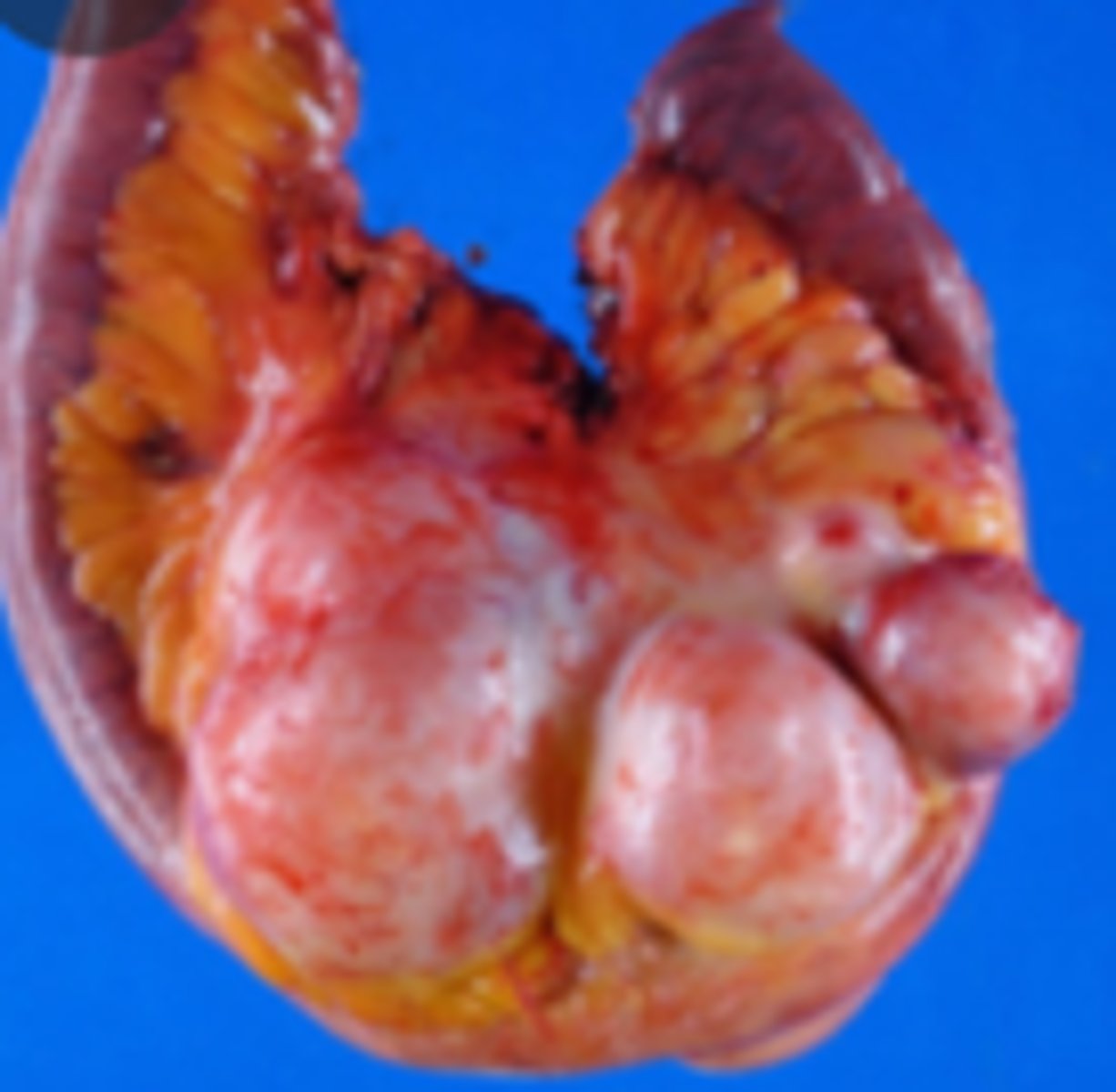
Which type of adenomatous polyps has the highest risk of becoming colorectal cancer?
Villous adenoma
What is the most common type of adenomatous polyps?
Tubulous adenoma - nonpedunculated
What causes pseudopolyps in colon?
IBD, non-cancerous
Which type makes up 90% of colon polyps and has a low risk for malignancy?
Hyperplastic
True/False: Patients with colon polyps will need a colonoscopy more frequently then the guidelines recommend.
True!
What type of cancer are most colorectal cancers?
Almost all are adenocarcinoma
______________ are associated with the greatest risk for colorectal cancer.
Villous adenomas
85% of sporadic colorectal cancer arise from _____________ and have loss of function of 1 or more tumor suppressor genes.
adenomatous polyp
What are the tumor suppressor genes found in colorectal cancer?
APC, p53, DCC
How is colorectal cancer activated?
Through oncogenes such as BRAF and KRAS
5% of colorectal cancer are caused by inherited germline mutations known as ______________.
polyposis syndromes
What are two major inherited polyposis syndromes that increase the risk of colorectal cancer?
Familial Adenomatous Polyposis (FAP)
Hereditary Nonpolyposis Colorectal Cancer (HNPCC), also known as Lynch syndrome
A 67-year-old woman presents with increasing fatigue and weakness over the past few months. She denies abdominal pain, changes in bowel habits, or weight loss. Physical examination is unremarkable. Laboratory evaluation reveals a microcytic anemia. Fecal occult blood test (FOBT) is positive. A colonoscopy reveals a mass in the ascending colon.
Which of the following best explains this patient's presentation?
A) Obstructive colicky abdominal pain due to a left-sided lesion
B) Chronic blood loss from a right-sided colon cancer
C) Tenesmus and hematochezia from a rectal mass
D) Rapidly growing tumor causing acute bowel obstruction
B) Chronic blood loss from a right-sided colon cancer
A 62-year-old man presents with a 4-month history of intermittent cramping lower abdominal pain, constipation alternating with diarrhea, and a noticeable decrease in stool caliber. He has also unintentionally lost 8 pounds. He has hematochezia. Physical exam reveals mild tenderness in the left lower quadrant. A colonoscopy identifies an obstructing mass in the sigmoid colon.
Which of the following is the most likely underlying cause of this patient's symptoms?
A) Chronic blood loss from a right-sided colon cancer
B) Obstructive mass from a left-sided colon cancer
C) Carcinoid tumor causing serotonin secretion
D) Inflammatory bowel disease flare
What tumor marker could you find in this patient?
What labs could you order?
What diagnostic test do you order to confirm your suspected diagnosis?
What imaging should you order?
How do you treat it?
1.) B) Obstructive mass from a left-sided colon cancer
2.) CEA antigen
3.) CBC, CMP, ALP
4.) Colonoscopy is diagnostic test for colorectal cancer. Should receive colonoscopy at age 45 if no risk factors then repeat every 10 years. If you have a family history start 10 years prior to the age at which the family member was diagnosed and repeat every 5 years.
5.) 4.) CT with contrast of the chest, abdomen, pelvis - preop staging
PET CT
6.) Management depends on stage.
- Surgery
- Chemotherapy
Which oncogenes may be activated with colorectal cancer?
BRAF and KRAS
Which tumor suppressor genes might be activated with colorectal cancer?
APC, p53, DCC
What is the most common type of anal carcinoma?
Squamous cell
What percent of anal carcinomas are associated with HPV?
80%
A 56-year-old woman presents with a 3-month history of rectal bleeding, pain during defecation, and a sensation of a mass near her anus. She initially thought it was hemorrhoids, but symptoms have progressively worsened. On physical examination, there is a firm, ulcerated lesion at the anal verge.
Which of the following imaging studies would be most appropriate to evaluate for local invasion and distant metastasis?
A) Abdominal ultrasound
B) CT scan and MRI of the pelvis
C) Barium enema
D) Colonoscopy
What is the diagnosis?
What is the treatment?
1.) B) CT scan and MRI of the pelvis
2.)Anal carcinoma
3.) Surgery +/- chemo +/- radiation
--> Management depends on tumor location and stage
Which cells does hepatocellular carcinoma arise from?
parenchymal cells
Which cells does cholangiocarcinoma arise from?
ductal cells
Hepatocellular carcinoma is most commonly associated with ______________.
cirrhosis
A 58-year-old man with a history of chronic hepatitis C presents with increasing fatigue, unintentional weight loss, and new onset abdominal ascites. On physical exam, he appears cachectic with a distended abdomen and shifting dullness. Hepatomegaly with tenderness is noted, and a bruit is heard over the right upper quadrant.
What labs should you order?
What imaging should you order to confirm the diagnosis?
What is the diagnosis?
What is the treatment?
1.) CBC, CMP, hepatitis panel
AFP, Vitamin K, PT/INR, PTT
2.) MRI
3.) Hepatocellular carcinoma
4.) Surgery - resection vs. transplant
How do you screen for hepatocellular carcinoma?
Surveillance those with chronic HBV or those with cirrhosis caused by HCV, HBV, or alcohol
Hepatic ultrasound and AFP levels every 6 months
What is Courvoisier's sign and when would you find it?
Palpable, enlarged, and painless gall bladder in a patient with jaundice.
Found in those with pancreatic cancer.
What is the most common symptom of biliary tract cancer?
progressive jaundice
A 72-year-old man presents with progressive yellowing of his skin and eyes over the past two months. He reports pruritus, dark urine, pale stools, and a 15-pound unintentional weight loss. He also notes right upper quadrant discomfort but no fever or chills. On physical exam, he has profound jaundice, scratch marks on his skin, a palpable, nontender gallbladder, and hepatomegaly.
What best explains the palpable gallbladder in this patient?
What tumor marker would you likely find as its found in more then 85% of people with this condition?
What other labs could you order?
What imaging would you order?
1.) Obstructing malignancy of the biliary tract (Courvoisier's sign)
2.) CA-199
3.) Since this patient has jaundice you would find direct hyperbilirubinemia, increased ALP and GGT.
4.) Order CT with Contrast of abdomen
Is pancreatic carcinoma more common in males or females?
Males
What is the most common type of pancreatic cancer?
adenocarcinoma
What is the most common location for pancreatic carcinoma?
Pancreatic head
______________ (palpable gallbladder) may be found with pancreatic carcinoma.
Courvoisier sign
What tumor marker would you find with pancreatic carcinoma?
CA-199
What imaging would you order for someone with pancreatic carcinoma?
CT Chest/abdomen/Pelvis
EUS with FNA biopsy
PET
A 68-year-old man presents to the clinic with complaints of mid-back pain, early satiety, and an unintentional 20-pound weight loss over the past three months. He also reports new-onset jaundice and dark urine. His past medical history includes a 30-pack-year smoking history and type 2 diabetes mellitus diagnosed one year ago. On physical examination, scleral icterus and a palpable, non-tender gallbladder are noted.
Which of the following is the most likely diagnosis?
A) Acute pancreatitis
B) Pancreatic carcinoma
C) Cholangiocarcinoma
D) Gallstone disease
B) Pancreatic carcinoma
How do you treat pancreatic carcinoma when the cancer is at the head of the pancreas?
Whipple
How do you treat pancreatic carcinoma when the cancer is at the body and tail of the pancreas?
Distal pancreatectomy