NUR 425 Exam 2
0.0(0)
Card Sorting
1/120
Earn XP
Description and Tags
Last updated 12:39 AM on 10/28/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
121 Terms
1
New cards
What does absolute neutrophil count measure?
The total number of neutrophils in the blood
2
New cards
Which lab test is used to monitor the intrinsic pathway?
PTT (partial prothrombin time)
3
New cards
Which lab test is used to monitor the extrinsic pathway?
PT (prothrombin time)
4
New cards
aPTT (activated partial thromboplastin time)
30-40 seconds
5
New cards
INR
1 or less
6
New cards
PTT (partial prothrombin time)
60-70 seconds
7
New cards
PT (prothrombin time)
10-13 seconds
8
New cards
What drug does PT (prothrombin time) monitor?
Warfarin (Coumadin)
9
New cards
What drug does PTT and aPTT monitor?
Heparin
10
New cards
Red Blood Cell (RBC) Count
Females: 3.61 - 5.11 million/mm3 (4)
Males: 4.21 - 5.81 million/mm3 (5)
Males: 4.21 - 5.81 million/mm3 (5)
11
New cards
Hematocrit
Females: 36% - 48% (39)
Males: 42% - 52% (45)
Males: 42% - 52% (45)
12
New cards
Hemoglobin
Females: 11.7 - 15.5 g/dL (13)
Males: 14 - 17.3 g/dL (15)
Males: 14 - 17.3 g/dL (15)
13
New cards
White Blood Cell (WBC) Count
4.50 - 11.1 103/mm3
14
New cards
Absolute Neutrophil Count (ANC)
1.5 to 8.0 (1,500 to 8,000/mm3)
15
New cards
Platelets
150,000 - 450,000/µL
16
New cards
What does a WBC shift to the left mean?
-Indicates that more immature cells are present in the blood than normal
-Occurs with acute infection, inflammation, or some other significant physical stress
-Occurs with acute infection, inflammation, or some other significant physical stress
17
New cards
What is anemia?
Occurs when there is a reduction in the oxygen-carrying capacity through either fewer RBCs or a reduction in hemoglobin
18
New cards
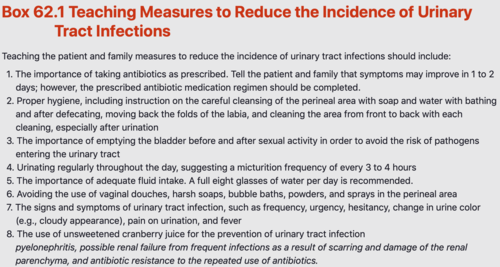
What are symptoms of decreased hematocrit?
-Shortness of breath
-Tachypnea
-Tachycardia
-Pallor
-Fatigue
-Dizziness
-Tachypnea
-Tachycardia
-Pallor
-Fatigue
-Dizziness
19
New cards
What are dietary sources of iron?
-Meat (especially red meat)
-Dark green leafy vegetables (spinach, broccoli, peas)
-Beets
-Dried beans
-Iron-fortified breakfast cereals and breads
-Cream of Wheat
-Ingesting citrus fruits such as oranges or grapefruits increases the vitamin C intake and may improve iron absorption
-Dark green leafy vegetables (spinach, broccoli, peas)
-Beets
-Dried beans
-Iron-fortified breakfast cereals and breads
-Cream of Wheat
-Ingesting citrus fruits such as oranges or grapefruits increases the vitamin C intake and may improve iron absorption
20
New cards
What are clinical manifestations of iron-deficiency anemia?
-Fatigue
-Pallor
-Tachycardia
-Tachypnea
-Glossitis (smooth, shiny tongue)
-Koilonychia (spoon-shaped nails)
-Pallor
-Tachycardia
-Tachypnea
-Glossitis (smooth, shiny tongue)
-Koilonychia (spoon-shaped nails)
21
New cards
How is iron-deficiency anemia diagnosed?
-A complete blood count (CBC) demonstrates decreased hemoglobin and hematocrit levels
-Serum ferritin levels less than or equal to 100 ug/L indicate IDA 100% of the time
-Additional diagnostic studies to confirm IDA include serum iron, total iron-binding capacity (TIBC), serum transferrin receptors, and mean corpuscular volume (MCV)
-Serum ferritin levels less than or equal to 100 ug/L indicate IDA 100% of the time
-Additional diagnostic studies to confirm IDA include serum iron, total iron-binding capacity (TIBC), serum transferrin receptors, and mean corpuscular volume (MCV)
22
New cards
What teaching do you need to provide to a client with iron-deficiency anemia?
-Dietary sources of iron
-Immediately report any signs of bleeding, increasing fatigue, or shortness of breath.
-Daily iron supplements must be taken as prescribed.
-Dangers of lead exposure
-Prenatal teaching about iron intake
-Immediately report any signs of bleeding, increasing fatigue, or shortness of breath.
-Daily iron supplements must be taken as prescribed.
-Dangers of lead exposure
-Prenatal teaching about iron intake
23
New cards
What are dietary sources of vitamin B12?
-Meat
-Seafood
-Eggs
-Dairy products
-Seafood
-Eggs
-Dairy products
24
New cards
What are clinical manifestations of vitamin B12 anemia?
-Fatigue
-Pallor
-Tachycardia
-Tachypnea
-Shortness of breath
-Dizziness
-Glossitis
-Neurological deficits:
•Symmetric paresthesia of feet and fingers
•Lhermitte's sign
•Confusion
•Depression
•Impaired taste
•Impaired balance
•Visual disturbances
•Tinnitus
-Pallor
-Tachycardia
-Tachypnea
-Shortness of breath
-Dizziness
-Glossitis
-Neurological deficits:
•Symmetric paresthesia of feet and fingers
•Lhermitte's sign
•Confusion
•Depression
•Impaired taste
•Impaired balance
•Visual disturbances
•Tinnitus
25
New cards
How is vitamin B12 anemia diagnosed?
-History and physical examination
-Vitamin B12 serum assay blood test
-Vitamin B12 serum assay blood test
26
New cards
What population is at increased risk of deficiency and may need to take a daily supplement of vitamin B12?
-Long-term vegans/vegetarians
-Those of low socioeconomic status
-Those of low socioeconomic status
27
New cards
What are clinical manifestations of folic acid deficiency?
-Fatigue
-Gray hair
-Mouth sores
-Swollen tongue
-Forgetfulness
-Depression
-Appetite loss
-Difficulty concentrating
-Birth defect
-Poor growth
-Gray hair
-Mouth sores
-Swollen tongue
-Forgetfulness
-Depression
-Appetite loss
-Difficulty concentrating
-Birth defect
-Poor growth
28
New cards
What are dietary sources of folic acid?
-Dark green vegetables
-Dried beans, legumes
-Fortified grains (breads, cereal)
-Nuts
-Bran
-Yeast
-Dried beans, legumes
-Fortified grains (breads, cereal)
-Nuts
-Bran
-Yeast
29
New cards
What teaching do you need to provide to a client with folic acid deficiency?
-Dietary sources of folate/folic acid
-Immediately report any clinical manifestations of fatigue, shortness of breath, dizziness, and confusion.
-Prenatal teaching
-Need for supplementation
-Immediately report any clinical manifestations of fatigue, shortness of breath, dizziness, and confusion.
-Prenatal teaching
-Need for supplementation
30
New cards
What teaching do you need to provide to a client with sickle cell anemia?
-Pathophysiology of disease
-Infection prevention measures
-Avoid cold temperatures and wearing tight, restrictive clothing.
-Avoid high altitudes and depressurized airplanes.
-Avoid dehydration.
-Avoid overexertion.
-Maintain activities of daily life within prescribed limitations.
-Risk of more frequent sickle cell crises during pregnancy.
-Fetal complications
-Genetic counseling
-Infection prevention measures
-Avoid cold temperatures and wearing tight, restrictive clothing.
-Avoid high altitudes and depressurized airplanes.
-Avoid dehydration.
-Avoid overexertion.
-Maintain activities of daily life within prescribed limitations.
-Risk of more frequent sickle cell crises during pregnancy.
-Fetal complications
-Genetic counseling
31
New cards
What are risk factors for sickle cell anemia?
-The sickle cell trait (SCT) is a genetic mutation that must be present in both parents in order for this form of the disease to manifest in offspring
-Parents who carry this gene have a one in four chance of producing a child with sickle cell anemia
-Precipitating factors include dehydration, cold temperatures, infection, and environments with low oxygen tension, such as depressurized airplane cabins and high mountains
-Parents who carry this gene have a one in four chance of producing a child with sickle cell anemia
-Precipitating factors include dehydration, cold temperatures, infection, and environments with low oxygen tension, such as depressurized airplane cabins and high mountains
32
New cards
What are clinical manifestations of sickle cell anemia?
-Fatigue
-Pallor
-Shortness of breath
-Vasoocclusion of blood vessels resulting in pain and swelling
-Pain usually occurs in the joints, bones, chest, and abdomen
-Growth and developmental delays
-Hand-food syndrome
-Pallor
-Shortness of breath
-Vasoocclusion of blood vessels resulting in pain and swelling
-Pain usually occurs in the joints, bones, chest, and abdomen
-Growth and developmental delays
-Hand-food syndrome

33
New cards
What are priority nursing actions for sickle cell anemia?
-Administer oxygen.
-Provide aggressive hydration.
-Administer pain medication.
-Administer blood transfusions.
-Administer antipyretics.
-Provide supportive measures.
-Provide aggressive hydration.
-Administer pain medication.
-Administer blood transfusions.
-Administer antipyretics.
-Provide supportive measures.
34
New cards
What is the treatment for sickle cell anemia crisis?
Hydration
Oxygenation (comes first)
Pain relief
Oxygenation (comes first)
Pain relief
35
New cards
What are clinical manifestations of aplastic anemia?
-Decreased RBCs: Fatigue, shortness of breath, tachycardia, pallor, dizziness, and headache
-Decreased WBCs: Increased susceptibility to infections, as well as frequent and prolonged infections
-Thrombocytopenia: Unexplained and increased incidence of bruising, nosebleeds, gum bleeding, and prolonged bleeding from cuts and other injuries
-Decreased WBCs: Increased susceptibility to infections, as well as frequent and prolonged infections
-Thrombocytopenia: Unexplained and increased incidence of bruising, nosebleeds, gum bleeding, and prolonged bleeding from cuts and other injuries
36
New cards
What teaching do you need to provide to a client with aplastic anemia?
-Avoid exposure to potential infection (individuals with acute infection, crowded places).
-Report all temperature elevations.
-Avoid activities with the potential for trauma or injury.
-Clinical manifestations of anemia
-Nutritional intake
-Report all temperature elevations.
-Avoid activities with the potential for trauma or injury.
-Clinical manifestations of anemia
-Nutritional intake
37
New cards
What are clinical manifestations of thrombocytopenia?
-Easy bruising and petechiae
-Bleeding may occur from the nose, around the gums, or from the gastrointestinal tract
-Bleeding may occur from the nose, around the gums, or from the gastrointestinal tract
38
New cards
What are priority nursing actions for thrombocytopenia?
-Implement bleeding precautions (RANDI)
-Minimize blood loss from lacerations or venipuncture.
-Avoid intramuscular injections.
-Avoid rectal temperatures, enemas, suppositories, and douches.
-Provide a safe environment.
-Use minimal inflation when assessing blood pressure.
-Minimize blood draws.
-Minimize blood loss from lacerations or venipuncture.
-Avoid intramuscular injections.
-Avoid rectal temperatures, enemas, suppositories, and douches.
-Provide a safe environment.
-Use minimal inflation when assessing blood pressure.
-Minimize blood draws.

39
New cards
What are safety interventions for thrombocytopenia?
Bleeding precautions

40
New cards
What are risk factors for leukemia?
-Genetic anomalies
-Down's syndrome
-Exposure to radiation or benzene
-Chemotherapeutic agents and/or radiation therapy
-Smoking
-White males over the age of 60
-Down's syndrome
-Exposure to radiation or benzene
-Chemotherapeutic agents and/or radiation therapy
-Smoking
-White males over the age of 60
41
New cards
What are clinical manifestations of leukemia?
Anemia: Decreased hemoglobin, fatigue, pallor, weakness, and shortness of breath, as well as bruising, petechiae nosebleeds, and bleeding gums from the decreased number of platelets
Neutropenia: Risk for infection, low-grade fevers
Thrombocytopenia: Risk for bleeding
Neutropenia: Risk for infection, low-grade fevers
Thrombocytopenia: Risk for bleeding

42
New cards
What are diagnostic tests for leukemia?
-CBC
-History and physical examination
-Bone marrow biopsy
-Genetic testing
-History and physical examination
-Bone marrow biopsy
-Genetic testing
43
New cards
What are priority nursing actions for leukemia?
-Administer chemotherapy as prescribed.
-Institute neutropenic precautions.
-Prophylactic use of antibiotics, antivirals, and antifungals as ordered
-Administer IV antibiotics.
-Symptom management (nausea/vomiting/diarrhea, ulcerations of the mouth)
-Administer ordered blood products.
-Institute neutropenic precautions.
-Prophylactic use of antibiotics, antivirals, and antifungals as ordered
-Administer IV antibiotics.
-Symptom management (nausea/vomiting/diarrhea, ulcerations of the mouth)
-Administer ordered blood products.
44
New cards
What teaching do you need to provide to a client with leukemia?
-Neutropenic precautions
-Clinical manifestations of anemia
-Manifestations of thrombocytopenia
-Bleeding precautions
-Diagnosis of leukemia
-Adverse reactions of chemotherapy or radiation
-Possibility of sterility
-Clinical manifestations of anemia
-Manifestations of thrombocytopenia
-Bleeding precautions
-Diagnosis of leukemia
-Adverse reactions of chemotherapy or radiation
-Possibility of sterility

45
New cards
What are clinical manifestations for malignant lymphoma?
-Painless swelling of the lymph nodes in the neck, underarm, and groin
-Low-grade fevers for no apparent reason
-Drenching night sweats
-Unexplained weight loss of more than 10% in less than 6 months
-Fatigue
(known as the "B symptoms")
-Generalized pruritus, or itching, with pronounced excoriation from scratching is present in a large percentage of patients presenting with Hodgkin's disease (HD)
-Low-grade fevers for no apparent reason
-Drenching night sweats
-Unexplained weight loss of more than 10% in less than 6 months
-Fatigue
(known as the "B symptoms")
-Generalized pruritus, or itching, with pronounced excoriation from scratching is present in a large percentage of patients presenting with Hodgkin's disease (HD)
46
New cards
What teaching do you need to provide to a client with malignant lymphoma?
-Disease process
-Risk of infection
-Maintaining treatment schedules
-Encourage frequent rest periods.
-Dietary intake
-Clinical manifestations of potential complications
-Possibility of sterility
-Risk of infection
-Maintaining treatment schedules
-Encourage frequent rest periods.
-Dietary intake
-Clinical manifestations of potential complications
-Possibility of sterility
47
New cards
What are clinical manifestations of multiple myeloma?
-Fatigue
-Weakness
-Bone pain
-Recurrent infections
-Weight loss
-Paresthesia
-Weakness
-Bone pain
-Recurrent infections
-Weight loss
-Paresthesia

48
New cards
What does the nursing assessment include for multiple myeloma?
-Vital signs
-Fatigue, pallor, and shortness of breath
-Pain
-Paresthesias
-Intake and output
-Serum and urine calcium
-Serum blood urea nitrogen (BUN) and creatinine
-Fatigue, pallor, and shortness of breath
-Pain
-Paresthesias
-Intake and output
-Serum and urine calcium
-Serum blood urea nitrogen (BUN) and creatinine
49
New cards
What teaching do you need to provide to a client with multiple myeloma?
-Immediately report any clinical manifestations of fatigue, shortness of breath, dizziness, or confusion.
-Report any sudden onset of severe pain or new location, especially of back pain, which could indicate a pathological fracture.
-Report changes in sensation, increased numbness and tingling, or changes in motor function.
-Instruct in the use of nonpharmacological pain management methods, such as music, relaxation, deep breathing, imagery, distraction, and progressive muscle relaxation.
-Report any sudden onset of severe pain or new location, especially of back pain, which could indicate a pathological fracture.
-Report changes in sensation, increased numbness and tingling, or changes in motor function.
-Instruct in the use of nonpharmacological pain management methods, such as music, relaxation, deep breathing, imagery, distraction, and progressive muscle relaxation.
50
New cards
What effect does renal insufficiency have on RBC count?
Decreases RBC count
51
New cards
What are examples of potential nephrotoxic substances?
-Antibiotics
-Analgesics: NSAIDS
-Other medications: ACE inhibitors, benzodiazepines, contrast media, diuretics
-Substances: Cocaine, gold, heroin, lead, mercury
-Analgesics: NSAIDS
-Other medications: ACE inhibitors, benzodiazepines, contrast media, diuretics
-Substances: Cocaine, gold, heroin, lead, mercury
52
New cards
What is anuria?
-Less than 100-mL urine output/24 hr
-Clinical significance of abnormal finding: End-stage renal disease, acute renal failure, urinary tract obstruction
-Clinical significance of abnormal finding: End-stage renal disease, acute renal failure, urinary tract obstruction
53
New cards
What is dysuria?
-Difficulty or pain with urination
-Clinical significance of abnormal finding: Urinary tract infection, cystitis (bladder infection)
-Clinical significance of abnormal finding: Urinary tract infection, cystitis (bladder infection)
54
New cards
What is enuresis?
-Involuntary urination at night
-Clinical significance of abnormal finding: Lower urinary tract disorder
-Clinical significance of abnormal finding: Lower urinary tract disorder
55
New cards
What is frequency?
-Increase in incidence of voiding, usually urinating only small amounts with each void
-Clinical significance of abnormal finding: Bladder inflammation, excessive fluid intake, urinary retention
-Clinical significance of abnormal finding: Bladder inflammation, excessive fluid intake, urinary retention
56
New cards
What is hematuria?
-Presence of blood in the urine
-Clinical significance of abnormal finding: Cystitis or other inflammation in the urinary tract, calculi, cancers of the urinary tract, renal disease, bleeding disorders, medications such as anticoagulants
-Clinical significance of abnormal finding: Cystitis or other inflammation in the urinary tract, calculi, cancers of the urinary tract, renal disease, bleeding disorders, medications such as anticoagulants
57
New cards
What is hesitancy?
-Difficulty starting the flow of urine
-Clinical significance of abnormal finding: Urethral obstruction, enlargement of the prostate gland (benign or malignant)
-Clinical significance of abnormal finding: Urethral obstruction, enlargement of the prostate gland (benign or malignant)
58
New cards
What is incontinence?
-Inability to voluntarily control micturition
-Clinical significance of abnormal finding: Bladder infections, trauma to the external sphincter, neurogenic bladder, trauma to the nerve innervating the urinary tract structures
-Clinical significance of abnormal finding: Bladder infections, trauma to the external sphincter, neurogenic bladder, trauma to the nerve innervating the urinary tract structures
59
New cards
What is nocturia?
-Frequent urination at night
-Clinical significance of abnormal finding: Heart failure, renal disease, bladder obstruction, consumption of excessive fluids late at night
-Clinical significance of abnormal finding: Heart failure, renal disease, bladder obstruction, consumption of excessive fluids late at night
60
New cards
What is oliguria?
-Decreased urine output; less than 400-mL urine output/24 hr
-Clinical significance of abnormal finding: Shock, end-stage renal disease, acute kidney injury, severe dehydration, blood transfusion reaction
-Clinical significance of abnormal finding: Shock, end-stage renal disease, acute kidney injury, severe dehydration, blood transfusion reaction
61
New cards
What is polyuria?
-Increased urine output; greater than 2,000-mL urine output/24 hr
-Clinical significance of abnormal finding: Excessive fluid intake, diabetes insipidus, diabetes mellitus, diuretic medications, diuresis phase of chronic renal failure
-Clinical significance of abnormal finding: Excessive fluid intake, diabetes insipidus, diabetes mellitus, diuretic medications, diuresis phase of chronic renal failure
62
New cards
What is renal colic?
-Pain radiating to the perineal or groin area
-Clinical significance of abnormal finding: Ureter spasm during passage of calculi, ureter obstruction
-Clinical significance of abnormal finding: Ureter spasm during passage of calculi, ureter obstruction
63
New cards
What is retention?
-Inability to completely empty the bladder of urine
-Clinical significance of abnormal finding: Normal finding briefly after childbirth, pelvic surgery, and removal of indwelling catheter
Prolonged/abnormal related to neurogenic bladder, obstruction or stricture of the urethra
-Clinical significance of abnormal finding: Normal finding briefly after childbirth, pelvic surgery, and removal of indwelling catheter
Prolonged/abnormal related to neurogenic bladder, obstruction or stricture of the urethra
64
New cards
What is urgency?
-Sudden onset of the urge to void immediately
-Clinical significance of abnormal finding: Medications, pelvic organ prolapse, cystitis, UTI
-Clinical significance of abnormal finding: Medications, pelvic organ prolapse, cystitis, UTI
65
New cards
Serum Creatinine
0.5 - 1.2 mg/dL
66
New cards
Blood Urea Nitrogen (BUN)
8 - 21 mg/dL
67
New cards
BUN/Creatinine Ratio
10:1 to 20:1
68
New cards
Uric Acid
3.5 - 8 mg/dL
69
New cards
Bicarbonate
22 - 26 mEq/L
70
New cards
Sodium
135 - 145 mEq/L
71
New cards
Potassium
3.5 - 5.0 mEq/L
72
New cards
Phosphorus
2.5 - 4.5 mEq/L
73
New cards
Calcium
8.2 - 10.2 mEq/dL
74
New cards
Urine Specific Gravity
1.005 - 1.030
75
New cards
Glomerular Filtration Rate (eGFR)
85 - 110 is ideal
> 60 normal
< 15 can indicate possible kidney failure
> 60 normal
< 15 can indicate possible kidney failure
76
New cards
What are clinical manifestations of hyperkalemia?
Cardiac abnormalities
-Life-threatening dysrhythmias such as ventricular fibrillation, ventricular tachycardia, or asystole
-The initial indication on an ECG is peaked T waves
-Life-threatening dysrhythmias such as ventricular fibrillation, ventricular tachycardia, or asystole
-The initial indication on an ECG is peaked T waves
77
New cards
What does an increased urine specific gravity indicate?
Dehydration
78
New cards
What is a nursing intervention for increased urine specific gravity?
Increase fluids for hydration
79
New cards
What are clinical manifestations of PKD?
-Hypertension
-Hematuria
-Flank pain
-Headaches
-Pain in the abdominal area
-Manifestations of UTI
-Bilaterally enlarged kidneys
-Increased abdominal girth
-Costovertebral angle tenderness
-Hematuria
-Flank pain
-Headaches
-Pain in the abdominal area
-Manifestations of UTI
-Bilaterally enlarged kidneys
-Increased abdominal girth
-Costovertebral angle tenderness
80
New cards
What are priority nursing interventions for PKD?
-Diet modification consistent with impaired renal function, specifically low potassium, phosphorus, protein, and sodium
-Fluid restriction
-Administer antihypertensive agents as ordered.
-Administer antibiotics as ordered.
-Administer pain medication as ordered.
-Fluid restriction
-Administer antihypertensive agents as ordered.
-Administer antibiotics as ordered.
-Administer pain medication as ordered.
81
New cards
How do you use therapeutic communication with a client who has PKD?
-Provide psychosocial support to client and family -Teach the client and family about prescribed treatments
82
New cards
What are the plan of care goals for a client with PKD?
-Prevent complications
-Medication compliance (antihypertensives, antibiotics, etc)
-Diet modification
-Vital signs within reasonable limits
-Absence of infection
-Medication compliance (antihypertensives, antibiotics, etc)
-Diet modification
-Vital signs within reasonable limits
-Absence of infection
83
New cards
What kind of diet should a client with PKD follow?
-Diet modification consistent with impaired renal function, specifically low potassium, phosphorus, protein, and sodium
-Diet modification is essential to prevent severe complications from eating foods high in protein, potassium, and phosphorus that the kidneys cannot excrete adequately
-Excess sodium intake can cause fluid retention
-Diet modification is essential to prevent severe complications from eating foods high in protein, potassium, and phosphorus that the kidneys cannot excrete adequately
-Excess sodium intake can cause fluid retention
84
New cards
What teaching do you need to provide to a client with PKD?
-Immediately report clinical manifestations of infection.
-Follow prescribed dietary restrictions.
-Follow prescribed antihypertensive therapy.
-Follow prescribed antibiotics for diagnosed UTIs.
-Follow prescribed dietary restrictions.
-Follow prescribed antihypertensive therapy.
-Follow prescribed antibiotics for diagnosed UTIs.
85
New cards
What are risk factors for pyelonephritis?
-Multiple pre-existing UTIs, treated or untreated which may be caused by:
+Vesicoureteral reflux
+Obstructions such as benign prostatic hypertrophy (BPH), a stricture, or a urinary stone
+A long-term indwelling urinary catheter
+Pregnancy
+Sexual activity in women
+Vesicoureteral reflux
+Obstructions such as benign prostatic hypertrophy (BPH), a stricture, or a urinary stone
+A long-term indwelling urinary catheter
+Pregnancy
+Sexual activity in women
86
New cards
What are clinical manifestations of pyelonephritis?
-Signs of infection (fever, chills, nausea, and vomiting)
-Back or flank pain
-CVA tenderness and enlarged kidneys
-Frequent and painful urination, and hematuria
-Back or flank pain
-CVA tenderness and enlarged kidneys
-Frequent and painful urination, and hematuria
87
New cards
What are clinical manifestations of pyelonephritis in the elderly?
-Fever
-Acute dysuria
-New or worse urinary urgency or incontinence
-Gross hematuria
-Suprapubic or costovertebral pain
-Acute dysuria
-New or worse urinary urgency or incontinence
-Gross hematuria
-Suprapubic or costovertebral pain
88
New cards
What are the plan of care goals for a client with pyelonephritis?
-Complications such as damage to renal structures, scarring, and chronic pyelonephritis can be avoided with proper treatment, follow-up care, and prevention
-No symptoms associated with pyelonephritis, such as burning or pain on urination, urinary frequency, hesitancy, urgency, nocturia, and hematuria
-Self-care efforts and compliance with treatment are evident from improvements in symptoms and reductions in recurrent infections
-No symptoms associated with pyelonephritis, such as burning or pain on urination, urinary frequency, hesitancy, urgency, nocturia, and hematuria
-Self-care efforts and compliance with treatment are evident from improvements in symptoms and reductions in recurrent infections
89
New cards
What are nursing actions for pyelopnephritis?
-Administer prescribed antibiotics as ordered.
-Administer prescribed pain medications.
-Provide adequate hydration, PO or IV as ordered.
-Administer prescribed pain medications.
-Provide adequate hydration, PO or IV as ordered.
90
New cards
What teaching do you need to provide to a client with pyelonephritis?
-Explain the disease condition to the patient and family.
-Instruct the patient and family on how to avoid UTIs.
-Take prescribed medications as ordered.
-Instruct the patient and family on the importance of rest.
-Instruct the patient and family on how to avoid UTIs.
-Take prescribed medications as ordered.
-Instruct the patient and family on the importance of rest.
91
New cards
What are complications of pyelonephritis?
-Scarring, chronic kidney disease (CKD), or permanent damage
-Multisystem organ failure as a result of septic shock
-Changes in mental status, fever, tachycardia, tachypnea, hypotension, oliguria, and leukopenia are the early signs of urosepsis
-Multisystem organ failure as a result of septic shock
-Changes in mental status, fever, tachycardia, tachypnea, hypotension, oliguria, and leukopenia are the early signs of urosepsis
92
New cards
What are risk factors for acute glomerulonephritis?
-Infections such as recent strep
-Immune diseases such as lupus, vasculitis, hypertension, and diabetes
-Immune diseases such as lupus, vasculitis, hypertension, and diabetes
93
New cards
What are clinical manifestations of acute glomerulonephritis?
-Proteinuria
-Hematuria
-Presence of WBCs and casts in urine
-Edema
-Decreased urine output (oliguria)
-Hypertension
-Elevated BUN and creatinine
-Hematuria
-Presence of WBCs and casts in urine
-Edema
-Decreased urine output (oliguria)
-Hypertension
-Elevated BUN and creatinine
94
New cards
What teaching do you need to provide to a client with acute glomerulonephritis?
-Overview of the disease process
-Prescribed medications
-Dietary restrictions
-Avoid infections
-Prescribed medications
-Dietary restrictions
-Avoid infections
95
New cards
What is considered the typical treatment for renal cancer?
Radical nephrectomy
96
New cards
What is a radical nephrectomy?
Involves removal of the affected kidney, adrenal gland, and surrounding tissues, such as the fascia, part of the ureter, and the draining lymph nodes
97
New cards
What is the survival rate after undergoing a radical nephrectomy?
With early detection, renal cancer has shown a 60% to 70% 5-year survival
98
New cards
What teaching do you need to provide to a client who is undergoing a radical nephrectomy?
-Avoid lifting >5 lbs
-Do not engage in strenuous activity
-Understand measures to protect function of remaining kidney (control BP, drink adequate fluids, limit NSAID use, stop smoking)
-PO hydration
-Cough and deep breathe
-Keep dressing clean
-Take medications as prescribed
-Do not engage in strenuous activity
-Understand measures to protect function of remaining kidney (control BP, drink adequate fluids, limit NSAID use, stop smoking)
-PO hydration
-Cough and deep breathe
-Keep dressing clean
-Take medications as prescribed
99
New cards
What teaching do you need to provide to a client with renal cancer?
-Teach the patient and family about the condition and any procedures or diagnostic tests.
-Teach the patient and family regarding medications.
-Provide appropriate resources for counseling regarding the disease process, tests and procedures, changes in body image, and financial concerns
-Teach the patient and family regarding medications.
-Provide appropriate resources for counseling regarding the disease process, tests and procedures, changes in body image, and financial concerns
100
New cards
What are postoperative actions following a radical nephrectomy?
-Administer pain medication as ordered.
-Administer IV hydration as ordered/encourage PO hydration as ordered.
-Encourage respiratory exercises.
-Appropriate care of catheters, stents, nephrostomy tubes, or drains
-Perform wound care as ordered.
-Administer IV hydration as ordered/encourage PO hydration as ordered.
-Encourage respiratory exercises.
-Appropriate care of catheters, stents, nephrostomy tubes, or drains
-Perform wound care as ordered.