Disease of Small Intestine
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
length of small intestine
3-9 meters
3 segments of small intestine
1. Duodenum
2. Jejunum
3. Ileum
length of duodenum
25-30 cm
________ is almost entirely retroperitoneal (located behind the peritoneum)
duodenum
Where does duodenum end?
Ligament of Treitz
dividing between upper and lower GI
Ligament of Treitz
what part of the small intestine is responsible for most of the absorption of nutrients?
Jejunum
What part of the small intestine is the distal 60%?
Ileum
What artery supplies the duodenum?
celiac artery
What artery supplies the jejunum?
superior mesenteric
What artery supplies the ileum?
superior mesenteric
What vein does the small intestine veins drain into?
portal vein
What are lacteals?
specialized lymph capillaries present in intestinal mucosa
-collect fat absorbed by the small intestine which has been packaged into chylomicrons
-intestinal lymph passes into the systemic circulation via the thoracic duct
Parasympathetic vs Sympathetic effects on digestion
parasympathetic = increase digestion
sympathetic = decrease digestion
The entire surface of the small intestine is covered by ___________________ _________
intestinal villi
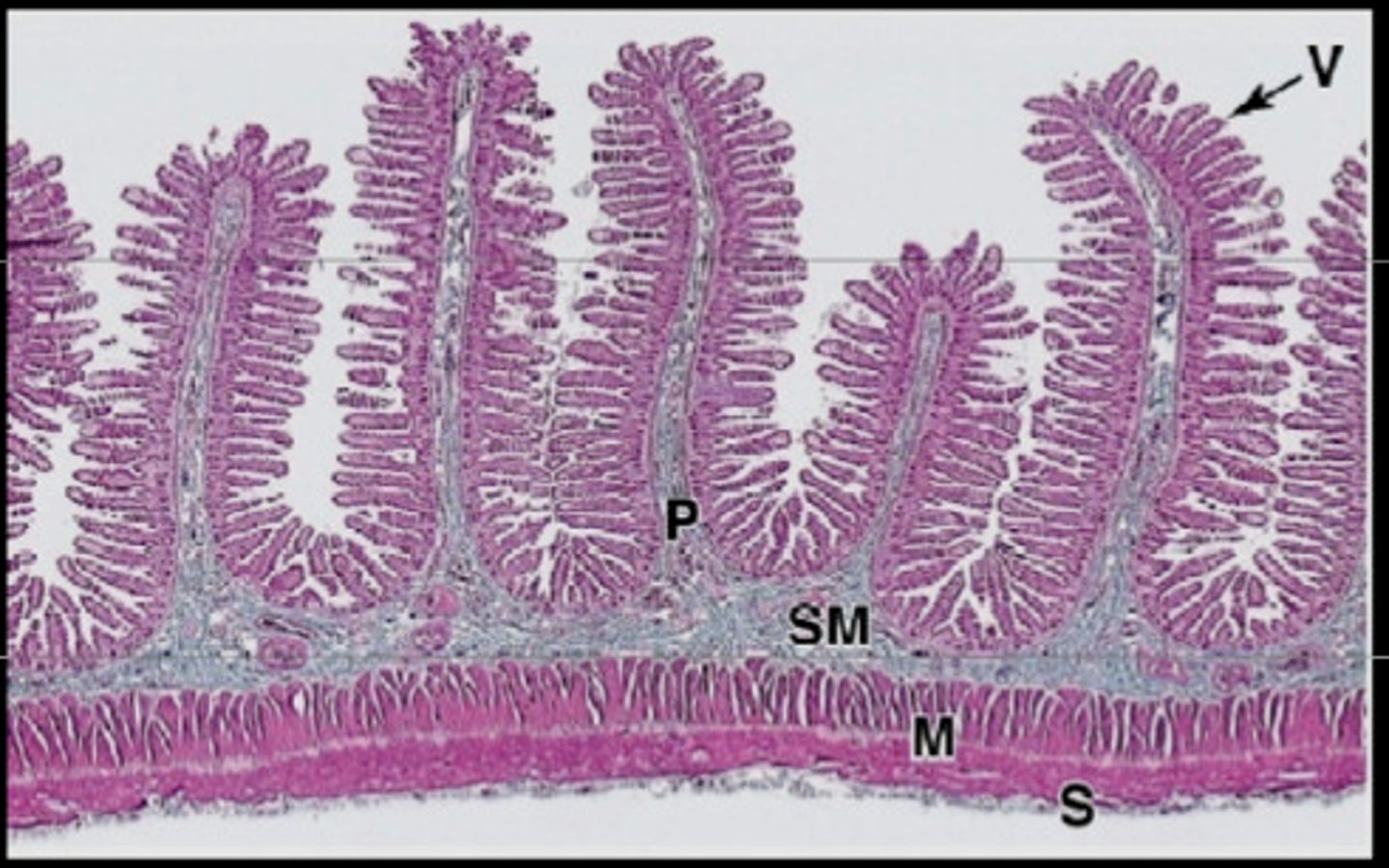
What is the function of intestinal villi?
expand the absorptive surface area of the intestinal mucosa
What are lacteal vessels?
specialized ducts of the lymphatic system to carry fats
-closely associated with the nerves and blood vessels within the intestinal lining
-carry fats to the thoracic duct
Function of intestine
secretes, digests, absorbs
Major digestion organ
small intestine
The small intestine is responsible for ______% of fluid and electrolyte absorption
90%
Where does digestion begin?
mouth (saliva)
What is poorly digested in the human small intestine?
dietary fiber and many simple carbohydrates
Where does digestion of other complex biological molecules such as fats, nucleic acids and proteins?
intestinal lumen
-initiated by salivary lipase and amylase and gastric pepsin
Describe the pathophysiology of absorption in the small intestine
-due to osmotic forces with water moving freely across membranes
-when large macromolecules are digested into monomers, osmolality INCREASES, INCREASING the influx of water
-this fluid along with bile, pancreatic juice, gastric acid, and saliva are PASSIVELY ABSORBED
Osmolality ________ as the food moves through the digestive system
decreases
Most water soluble products of absorption flow into the _______ vein
portal vein
_______ are not water soluble
lipids
What are lipids packaged into?
chylomicrons
-they are large lipoproteins that are too large to enter capillaries so they pass into the lacteal vessels and are taken to systemic circulation via the thoracic duct
What are chylomicrons?
Chylomicrons are tiny fatty droplets composed of triglycerides, small amounts of phospholipids, cholesterol, free fatty acids, and some protein.
Lipids --> ________ --> ________ --> _________duct --> _________ vein --> heart --> systemic circulation
Lipids --> chylomicrons -->lacteal --> thoracic duct --> subclavian vein --> heart --> systemic circulation
Fed vs fasting state
Fed:
-controlled by food
-move bolus downstream
Fasting:
-motility is cyclic
-periodically clears accumulated mucus, food, bacteria
Digestion and absorption are facilitated by what type of contractions?
non-propulsive segmental contractions that mix the food (creates the bolus)
After the food is made into a bolus, it is moved on by what type of contractions?
propulsive peristaltic contractions
How far does the propulsive contractions allow the food to travel?
a few centimeters at a time
The circular muscle __________ distal to the bolus and __________proximally.
The longitudinal muscle _________ distally and _______ proximally.
Circular muscle:
RELAXES distally
CONTRACTS proximally
Longitudinal muscle:
CONTRACTS distally
RELAXES proximally
What is functional dyspepsia?
recurrent upper GI discomfort of unknown etiology
-pain centered in the upper abdomen, epigastric pain or burning, early satiety, or postprandial fullness
Does functional dyspepsia have heartburn?
no
Pyrosis = ?
heartburn
What can cause functional dyspepsia?
overeating
eating too quickly
high fat foods
stress or alcohol or coffee
Is there an obvious cause for symptoms for functional dyspepsia?
no
-symptoms are non-specific
-limited in usefulness for diagnosis
-physical exam is rarely helpful
Evaluation and treatment similar to other upper GI workups
antisecretory agents
abx if H. pylori
upper endoscopy if red flag symptoms
What is lactase?
enzyme that breaks down lactose into glucose and galactose
How does lactase change as we age?
high at birth but decline as we age
Lactase deficiency can be secondary to...
Crohn's disease
celiac sprue
viral gastroenteritis
giardiasis
short bowel syndrome
malnutrition
S/S of Lactase deficiency
bloating
abdominal cramps
flatulence
osmotic diarrhea
Treatment for Lactase deficiency
-patient comfort
-lower lactose intake
-calcium supplements (risk of osteoporosis)
-lactase enzyme replacement
What is celiac disease?
an autoimmune disease in which people cant eat gluten because is damages their small intestine
S/S of celiac disease
-can take 10 years to be diagnosed correctly
infants: diarrhea/steatorrhea, weight loss, abdominal distention, weakness, muscle wasting, growth retardation
adults: diarrhea, dyspepsia, depression, iron deficiency anemia, osteoporosis, short stature, delayed puberty, amenorrhea, and reduced fertility
"dermatitis herpetiformis" = ?
celiac disease
Recommended test for celiac disease
IgA tissue transglutaminase antibody (95% sensitive/specific)
Diagnosis of celiac disease is confirmed with...
biopsy of proximal and distal duodenum
Treatment of celiac disease
-removal of all gluten from the diet (wheat, rye, barley)
-refer to dietician
-may need dietary supplement for water soluble vitamins initially
Most common abdominal surgical emergency
appendicitis
most common age for appendicitis
10-30
Cause of appendicitis
obstruction of appendix by a fecalith, inflammation, foreign body, or neoplasm
When will gangrene and perforation develop in appendicitis?
within 36 hours
S/S of appendicitis
-periumbilical or epigastric pain with anorexia then moves to RLQ within 12 hours
-steady ache worsens with walking or coughing
-N/V
-low grade fever
-RLQ TTP
-+ rebound tenderness
-Psoas, obturator, Rovsing's signs (+)
Testing for appendicitis
-Leukocytosis (high WBC)
-abdominal ultrasound or CT scan
Complications of appendicitis
perforation
peritonitis
possible sepsis
Treatment of appendicitis
surgery
What is intussusception?
The telescoping of one part of the intestinal tract into another
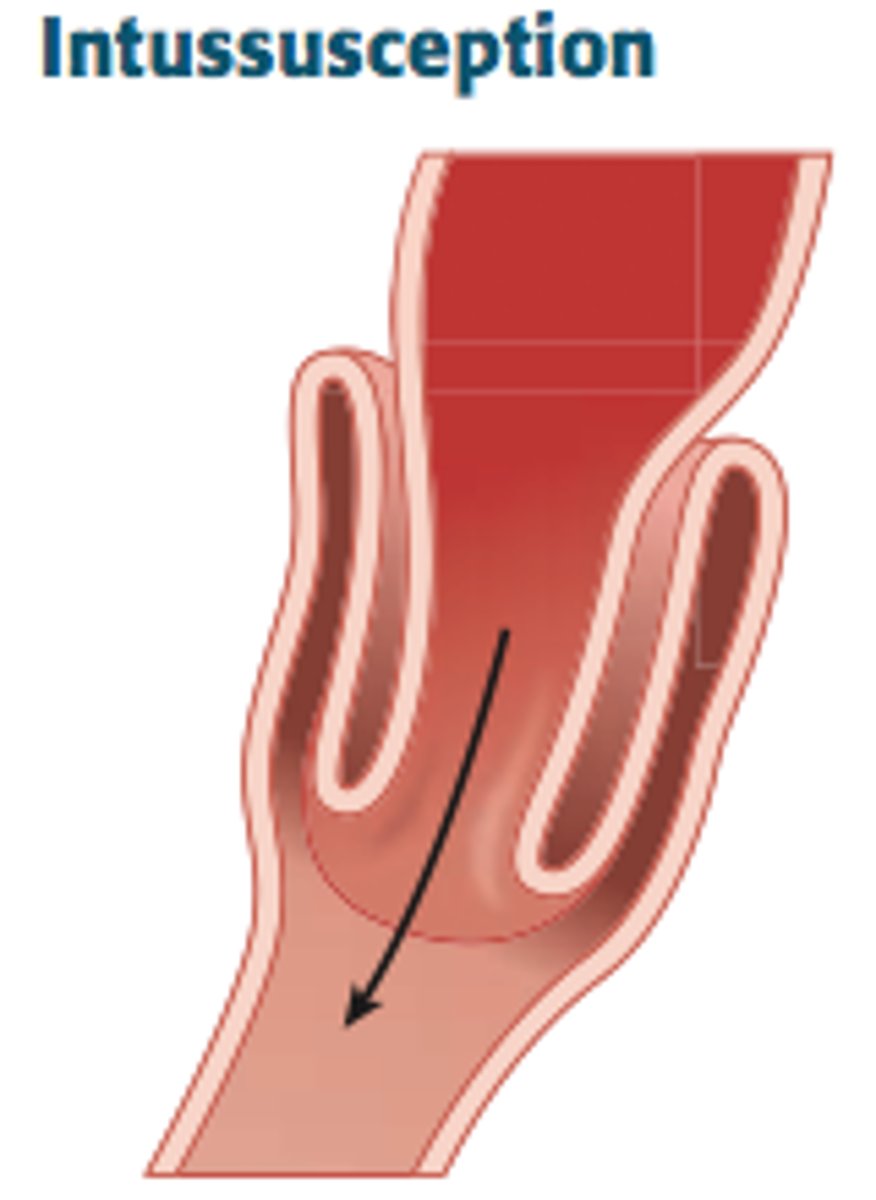
most common bowel obstruction in pts under 2 years of age
intussusception
Most common cause of intussusception in children > 6 years old
lymphoma
Most common cause of intussusception in adults
carcinoma or adenoma
S/S of intussusception
-N/V, diarrhea
-COLICKY abdominal pain
-blood tinged stool (red currant jelly stools)
Treatment of intussusception
children = air or barium enema
adults = surgery
Ischemic Bowel Disease
Inadequate blood supply resulting in vascular compromise to bowel
-true abdominal EMERGENCY
Can the intestine survive infartion?
no
even if a small segment of bowel ischemia allows intestinal pathogens into the abdominal cavity which will lead to fatal sepsis
Describe how blood loss in IBD leads to sepsis/death
loss of blood supply/blood not being able to get out -> necrosis -> after 24 hours bacterial invasion making pt sepsis -> 3-4 days after perforation -> death
The typical claim of IBD is....
pain of ischemic bowel is OUT OF PROPORTION to physical findings
Types of IBD
-chronic mesenteric arterial occlusion
-acute mesenteric arterial occlusion
-venous occlusion
-nonocclusive arterial insufficiency
What causes chronic mesenteric arterial occlusion?
atherosclerotic plaques can cause occlusions of celiac, superior mesenteric and inferior mesenteric arteries
-if 1 of the 3 arteries remains patent there is no symptoms
If 1 of the 3 arteries remains patent in chronic mesenteric arterial occlusion are there symptoms?
no
Partial occlusion of the three vessel in chronic mesenteric arterial occlusion allows enough blood flow to supply the resting intesting, but can elicit what?
"intestinal angina" after eating
-if can function at rest, but when food eaten there is angina
Complete comprised of the three vessel in chronic mesenteric arterial can be caused by hypotension, hypovolemic shock or MI, which results in what?
decreased blood flow to intestine which results in ischemic disease
What is often the cause of acute mesenteric arterial occlusion?
-emboli from the heart (A-fib) or aorta or by rupture and thrombosis of an atherosclerotic plaque
Is it more likely for a proximal or distal acute mesenteric arterial occlusion more likely to be necrotic?
proximal = bowel may survive due to collateral circulation through arcades
more distal = probability of necrosis increases
What causes venous occlusion?
liver cirrhosis
pancreatitis
Higher venous pressure combined with pt who have a hypercoagulable process are at increased risk of ___________________
acute mesenteric vein thrombosis
The intestine normally receives about ____% of total cardiac output
20%
-after meals the arterioles dilate and the blood flow can double
What happens to arterials and the bowel in the presence of shock?
arterioles constrict -> increasing central pressure (blood goes to heart and brain) -> prolonged vasoconstriction leads to ischemic bowel disease (IBD)
-form of non occlusive arterial insufficiency
Testing for Ischemic bowel disease
1. supine and upright plain films initially
2. CT with IV and oral contrast
3. MRA
Treatment of ischemic bowel disease
multisystem support if sepsis (ICU)
anticoagulation (known thrombotic event)
vasodilators (early stages)
surgery
Mechanical obstruction
occurs when intestinal contents are prevented from moving forward due to an obstacle or barrier that blocks the lumen
-lumen of gut is occluded
Is mechanical obstruction a surgical emergency?
yes
two categories of mechanical obstructions
Simple or closed loop
simple vs closed loop mechanical obstruction
single = only at one point
closed loop = two points, trapped intestine contents/secretions
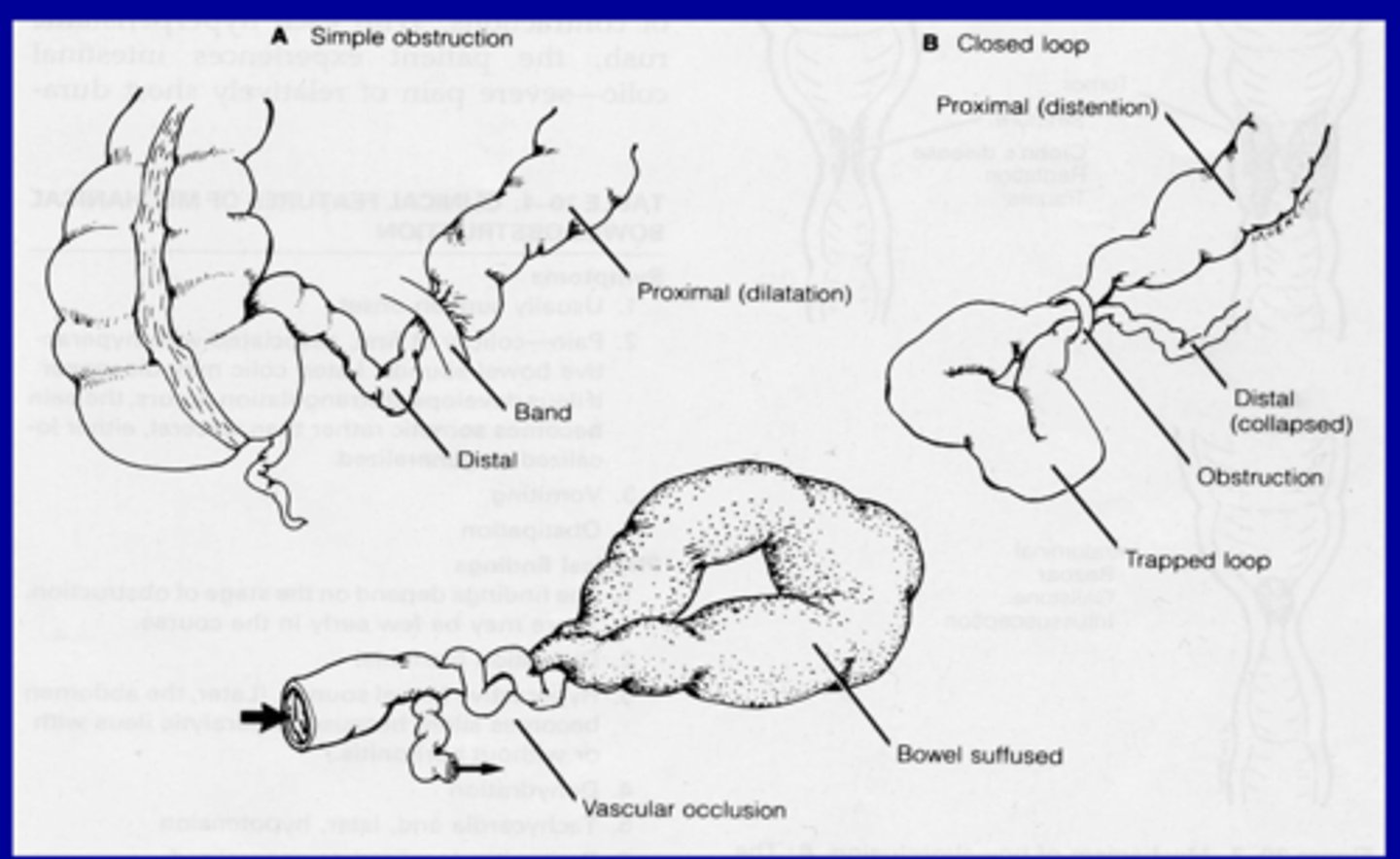
Two types of simple mechanical obstructions
1. adhesions
2. intussusception
most common cause of simple mechanical obstruction in adults
adhesions
Two types of closed loop obstruction
1. hernias
2. volvulus
most common cause of closed loop obstruction in adults
hernias
what is a volvus
intestine twisted itself into a knot
What is the cause of volvulus in children?
due to malrotation
in elderly, volvulus most typically affects what part of the colon?
cecum or sigmoid colon
Treatment of volvulus
sigmoidoscope may reduce the volvulus and allow colon to return to normal position
S/S of mechanical obstruction
-acute abdominal pain
-N/V
-pain is RHYTHMIC (associated with peristaltic waves)
-Pain is relieved by emesis
testing for obstructions (mechanical or functional)
1. plain abdominal films
upper GI with small bowel follow through
CT scan
Treatment of mechanical obstruction
surgery
-except childhood intussusception = air enema
treatment of childhood intussusception
air enema
Functional obstruction is more commonly known as ___
ileus