16 - Endocrine
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
Endocrine System
Transfer of information through chemical signals
Acts with nervous system to coordinate and integrate activity of body cells
Influences metabolic activities via hormones transported in blood
Response slower but longer lasting than nervous system
Chemical classes of hormones
Amino acid-based hormones
Amino acid derivatives, peptides, and proteins
Steroids
Synthesized from cholesterol
Gonadal and adrenocortical hormones
Mechanism of Hormone Action depends on
chemical nature and receptor location
water-soluble hormones
Lipid-soluble hormones
Water-soluble hormone mechanism
(all amino acid–based hormones except thyroid hormone)
Act on plasma membrane receptors
Act via G protein second messengers
Cannot enter cell
Lipid-soluble hormone mechanism
(steroid and thyroid hormones)
Act on intracellular receptors that directly activate genes
Can enter cell
Target cell activation depends on what factors
concertation
receptor availability
binding ability
Hormones influence number of their _
receptors
Upregulation—target cells form more receptors in response to low hormone levels
Downregulation—target cells lose receptors in response to high hormone levels
Control of Hormone Release
Blood levels of hormones
Controlled by negative feedback systems
Vary only within narrow, desirable range
Endocrine gland stimulated to synthesize and release hormones in response to
Humoral stimuli
Neural stimuli
Hormonal stimuli
Hormones circulate in blood either
free or bound
Steroids and thyroid hormone are attached to plasma proteins
All others circulate without carriers
Concentration of circulating hormone reflects
Rate of release
Speed of inactivation and removal from body
Hormones removed from blood by
Degrading enzymes
Kidneys
Liver
Half-life (in hormones)
time required for hormone's blood level to decrease by half
Varies from fraction of minute to a week
Interaction of Hormones at Target Cells
Multiple hormones may act on same target at same time
Permissiveness
Synergism
Antagonism
Permissiveness
one hormone cannot exert its effects without another hormone being present
Synergism
more than one hormone produces same effects on target cell → amplification
Antagonism
one or more hormones oppose(s) action of another hormone
Plots used in Endocrinology
Scatchard plot
Titration curve
Dose Response Curve
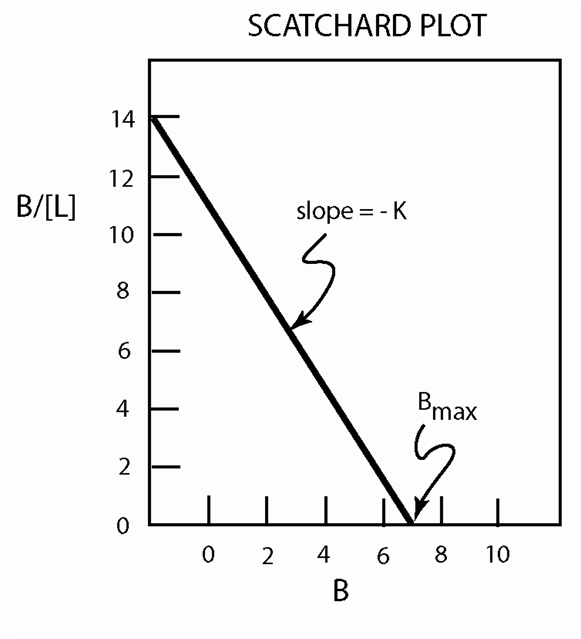
Scatchard plot
plots bound/free….showing affinity
Plots total amount of bound ligand/free concentration against total bound ligand.
-K = Association constant for ligand receptor binding
Bmax = Number of binding sites for ligand
Affinity of receptor for ligand and # of binding sites
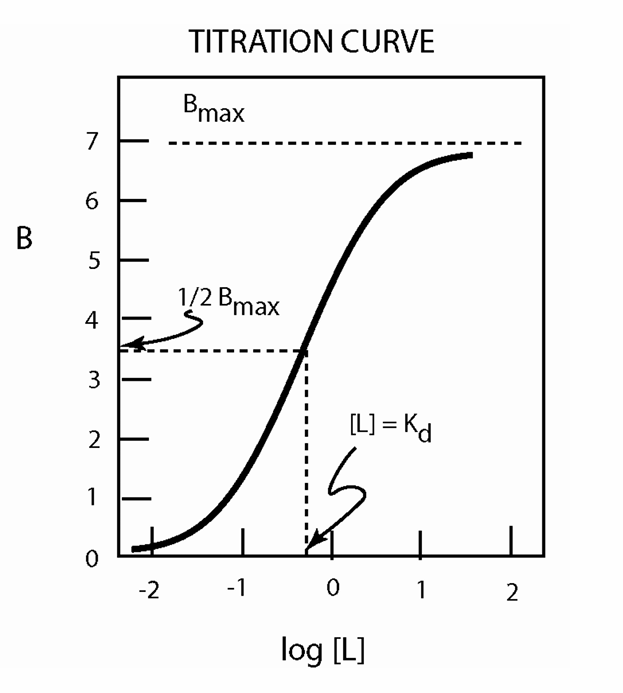
Titration Curve
Plots amount of bound ligand against the logarithm of the free ligand concentration.
Used to identify the concentration of ligand at which ½ of receptors are occupied, shows how affinity is determined above and below Kd
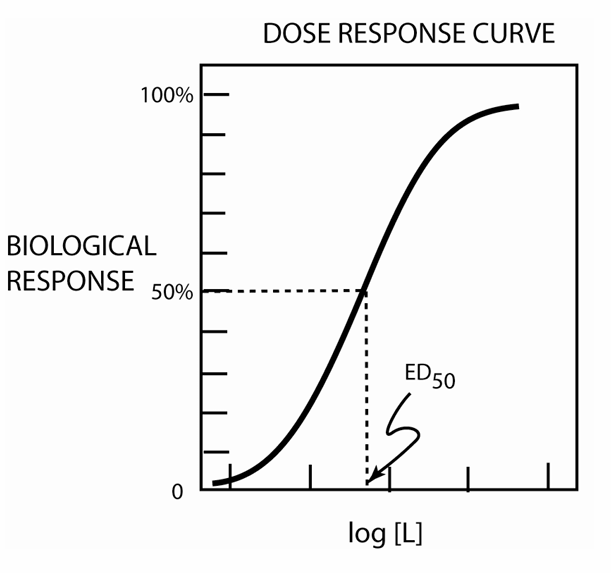
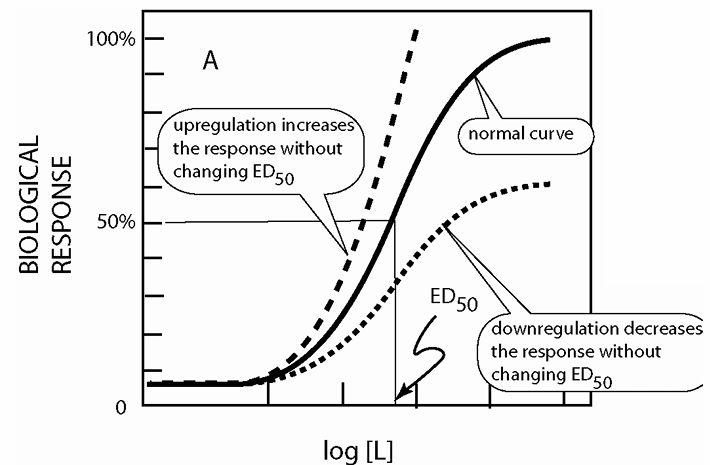
Dose-response Curve
Uses a biological response (instead of receptor occupancy) to show hormone effects.
ED50 = concentration of hormone at 50% max target cell activity
Dose-response curves can be
upregulated or downregulated
Sensitivity of target tissues to hormones can change with conditions
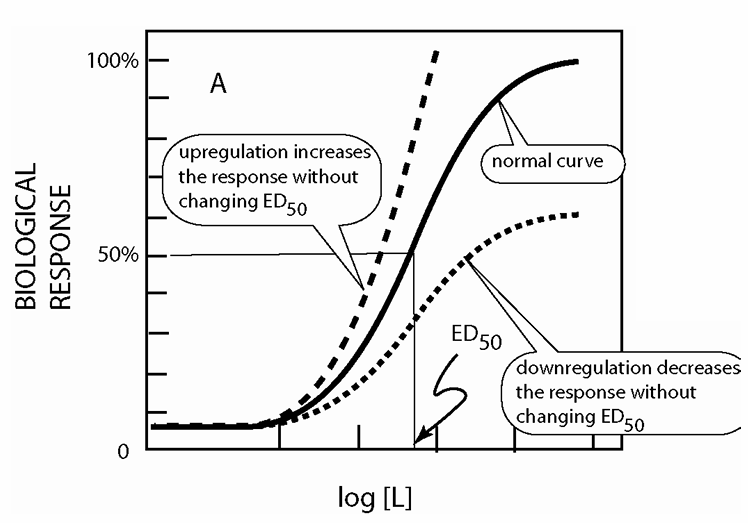
Maximal response of a target tissue can be altered by changing:
Number of active cells in the tissue
Number of receptor molecules in the tissue
Effectiveness of each receptor molecule
Dose response curves show mechanisms by
which target tissue responsiveness to a hormone can change
Upregulation/downregulation: Alteration in the number of active receptors
Exposure to a ligand almost always results in downregulation of (fewer) receptors
Some hormones amplify their action with upregulation FSH, estradiol
positive feedback loops, amplifying action
Desensitization changes the concentration dependence of the target tissue
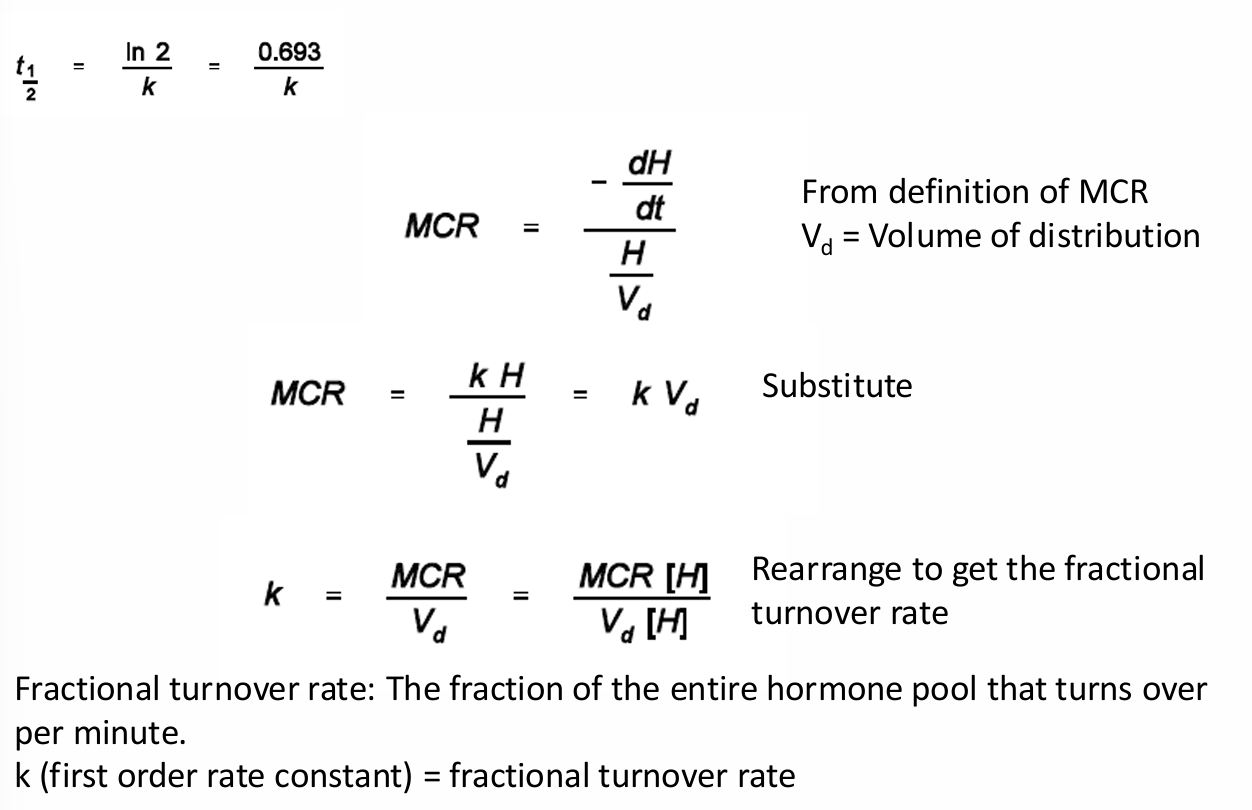
Half-Life and metabolic clearance rate (MCR) describe
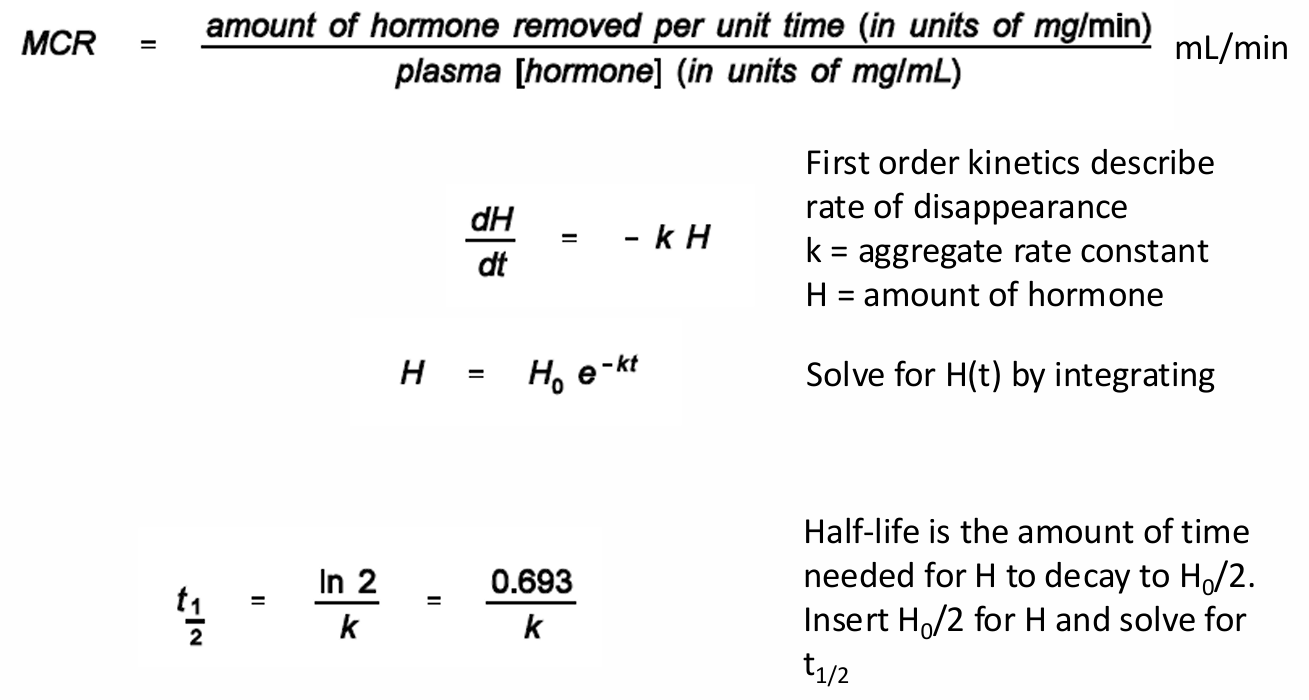
MCR is inversely related to _
the half life
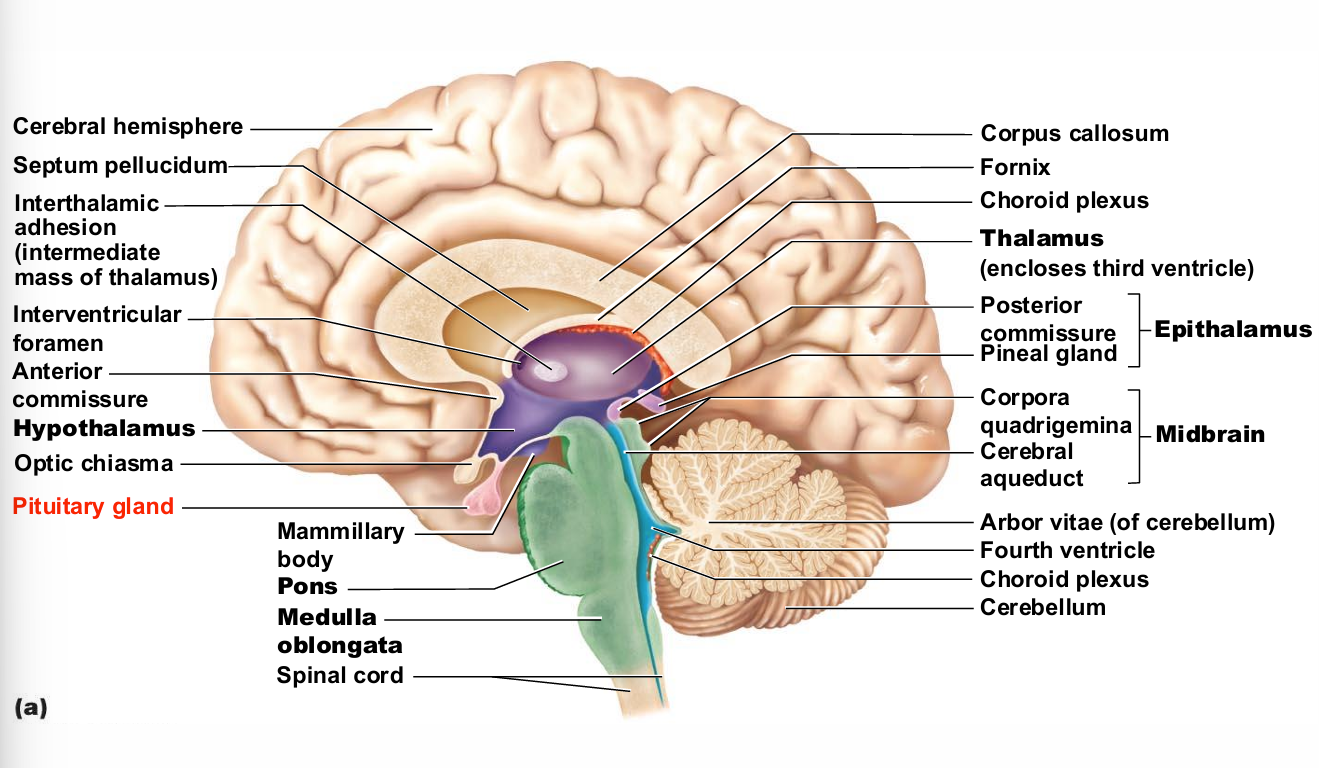
Hypothalamus
The portion of the brain that maintains the body’s homeostasis
Link between the endocrine and nervous systems (through the pituitary gland)
Produces releasing and inhibiting hormones, which stop and start the production of other hormones throughout the body
Pituitary gland lodes
posterior pituitary (lobe)
anterior lobe
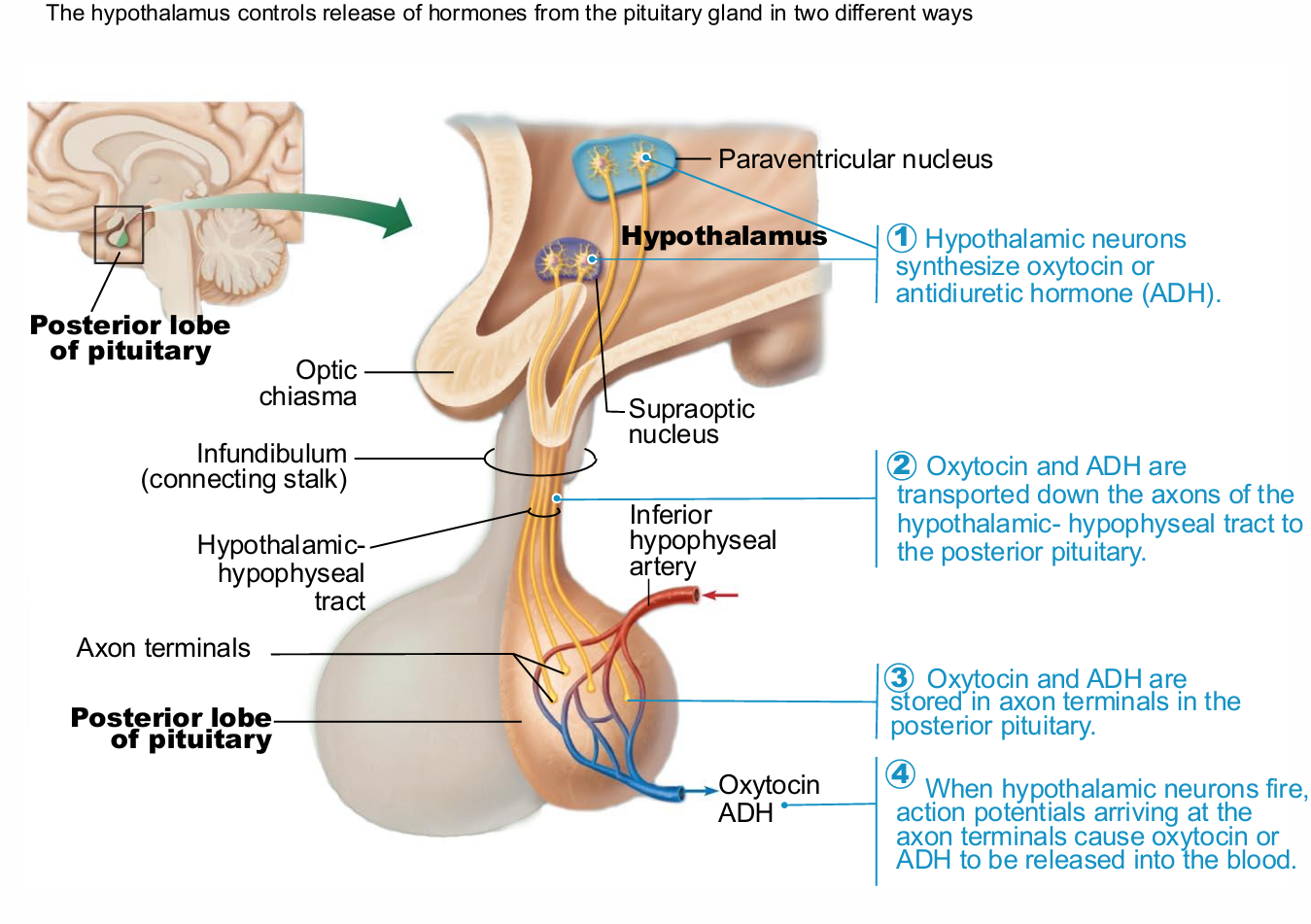
posterior pituitary (lobe)
Downgrowth of hypothalamic neural tissue
Neural connection to hypothalamus (hypothalamic hypophyseal tract)
Nuclei of hypothalamus synthesize neurohormones oxytocin (produced in similar quantities in male and female) and antidiuretic hormone (ADH)
Neurohormones are transported to and stored in posterior pituitary
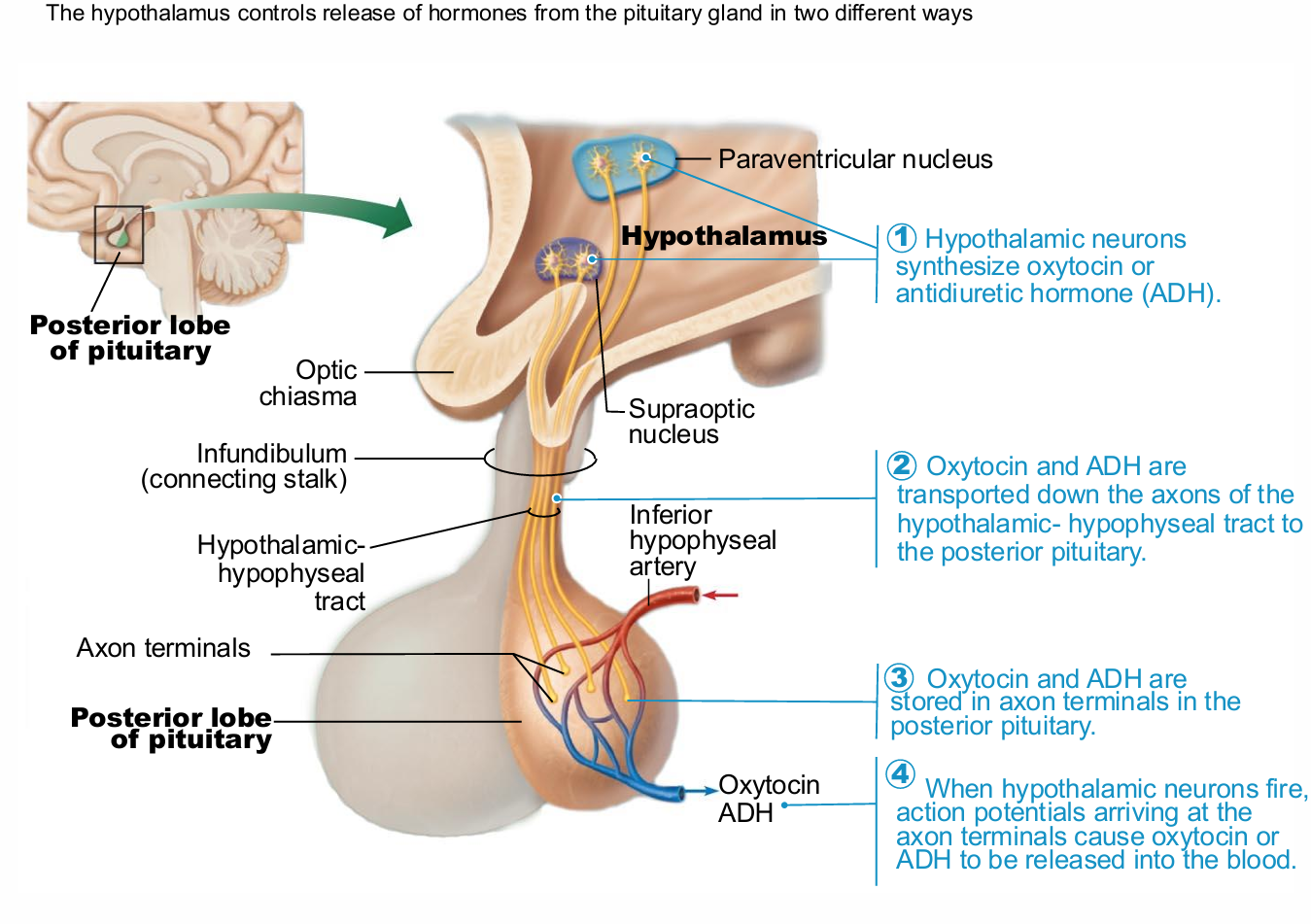
Steps of oxytocin and ADH release from pituitary galnd
Hypothalamic neurons synthesize oxytocin or antidiuretic hormone (ADH)
Oxytocin and ADH are transported down the axons of the hypothalamic- hypophyseal tract to the posterior pituitary.
Oxytocin and ADH are stored in axon terminals in the posterior pituitary.
When hypothalamic neurons fire, action potentials arriving at the axon terminals cause oxytocin or ADH to be released into the blood
Oxytocin vs ADH
Each composed of nine amino acids
Almost identical – differ in two amino acids
very different physiological effects
Oxytocin
Strong stimulant of uterine contraction
Released during childbirth
Hormonal trigger for milk ejection
suckling increases production
Acts as neurotransmitter in brain
is in males, but greater in females
play role in affectionate actions
ADH
aka Vasopressin
Inhibits or prevents urine formation
Regulates water balance
Targets kidney tubules → reabsorb more water
Release also triggered by pain, low blood pressure, and drugs
Inhibited by alcohol, diuretics
High concentrations → vasoconstriction
ADH pathologies
Diabetes insipidus
Syndrome of inappropriate ADH secretion (SIADH)
Diabetes insipidus
cause by things like head trauma
common in comatose patients
ADH deficiency due to hypothalamus or posterior pituitary damage
Must keep well-hydrated
Syndrome of inappropriate ADH secretion (SIADH)
Retention of fluid, headache, disorientation
Fluid restriction; blood sodium level monitoring
caused by things like meningitis and cancers
Anterior Lobe
Originates as outpocketing of oral mucosa
master endocrine gland in body
Vascular connection to hypothalamus
Hypophyseal portal system
Primary capillary plexus
Hypophyseal portal veins
Secondary capillary plexus
Carries releasing and inhibiting hormones to anterior pituitary to regulate hormone secretion
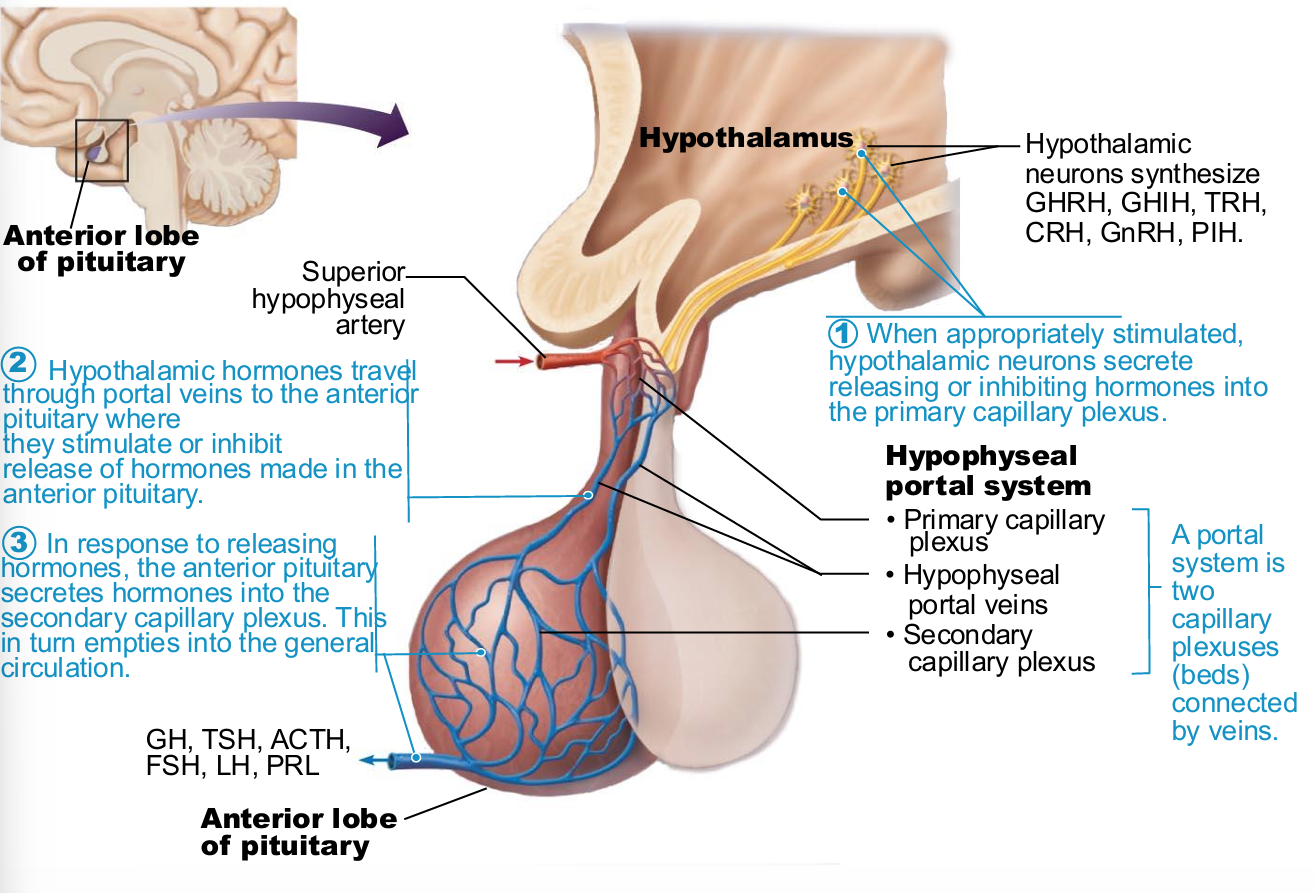
Release of hormones from Anterior Lobe
When appropriately stimulated, hypothalamic neurons secrete releasing or inhibiting hormones into the primary capillary plexus
Hypothalamic hormones travel through portal veins to the anterior pituitary where they stimulate or inhibit release of hormones made in the anterior pituitary.
In response to releasing hormones, the anterior pituitary secretes hormones into the secondary capillary plexus. This in turn empties into the general circulation.
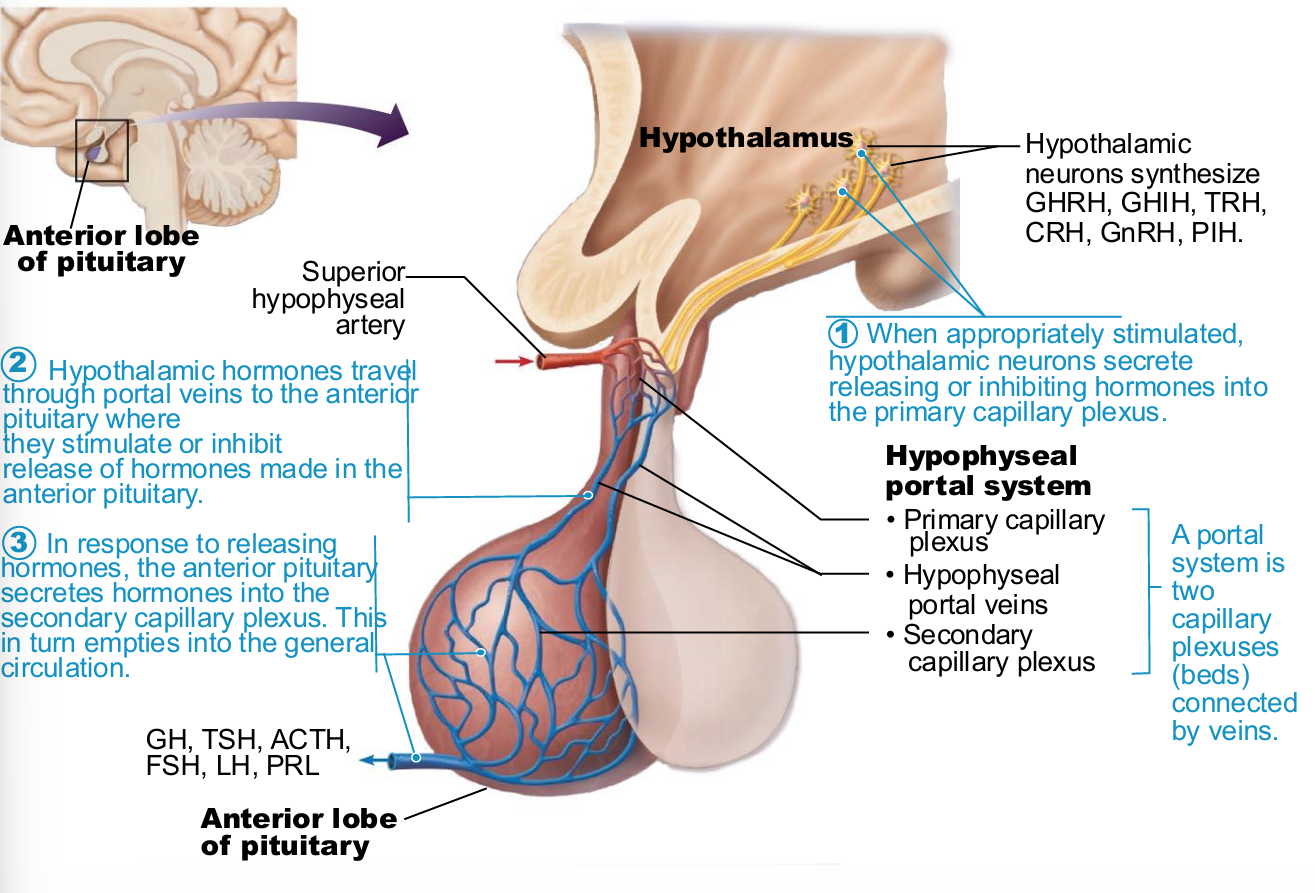
Anterior Pituitary Hormones
Growth hormone (GH)
Thyroid-stimulating hormone (TSH) or thyrotropin
Adrenocorticotropic hormone (ACTH)
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH)
Prolactin (PRL)
All are proteins
All except GH activate cyclic AMP second messenger systems at their targets
TSH, ACTH, FSH, and LH are all tropic hormones (regulate secretory action of other endocrine glands
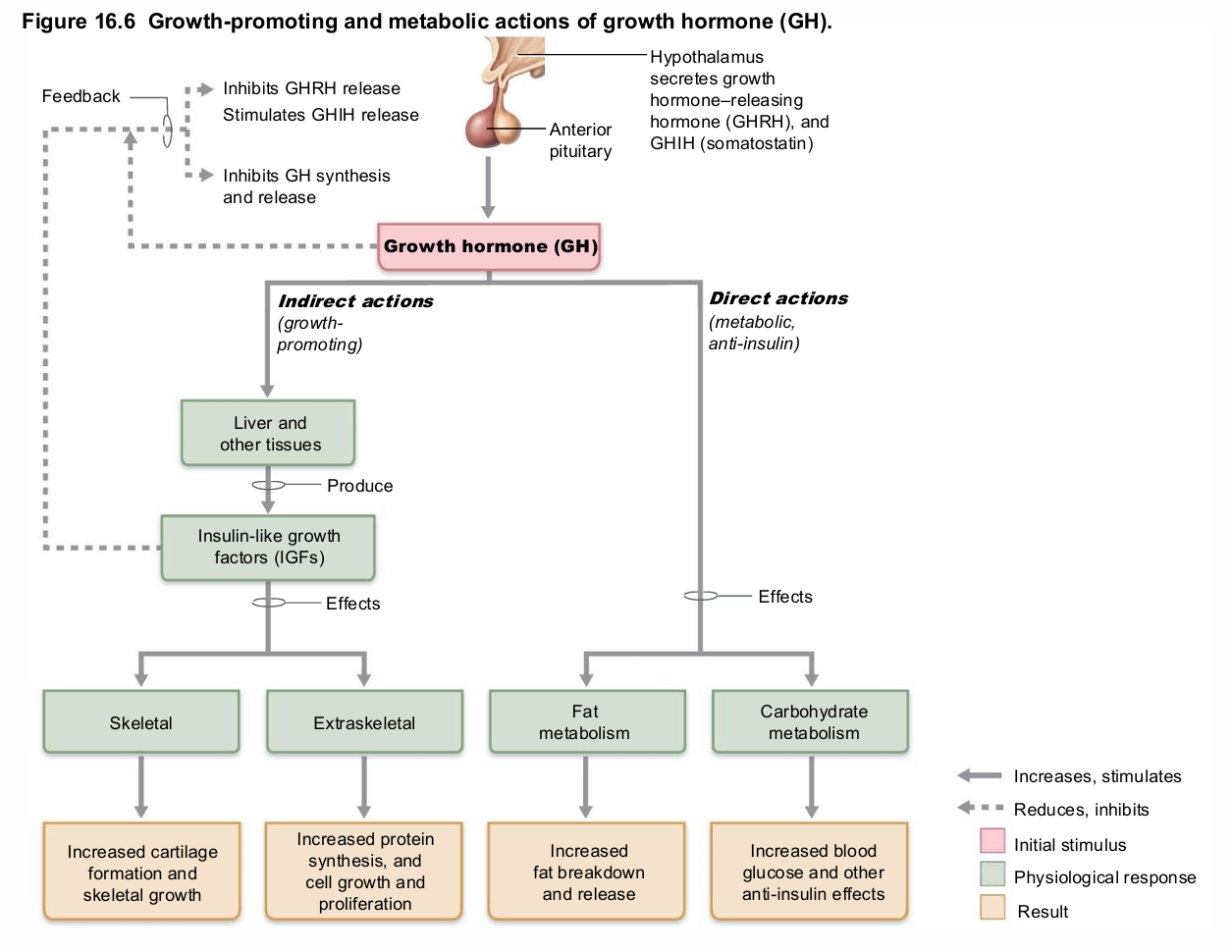
Growth Hormone
aka: GN or Somatotropin
Produced by somatotropic cells
Direct actions on metabolism
Indirect actions on growth
Mediates growth via growth-promoting proteins – insulin-like growth factors (IGFs)
IGFs stimulate
Uptake of nutrients → DNA and proteins
Formation of collagen and deposition of bone matrix
Major targets—bone and skeletal muscle
but do exist in all tissues
GH actions on metabolism
Increases blood levels of fatty acids; encourages use of fatty acids for fuel; protein synthesis
Decreases rate of glucose uptake and metabolism – conserving glucose
→ Glycogen breakdown and glucose release to blood (anti-insulin effect)
GH release chiefly regulated by _
hypothalamic hormones
Growth hormone–releasing hormone (GHRH)
Stimulates release
Growth hormone–inhibiting hormone (GHIH) (somatostatin)
Inhibits release
Ghrelin (hunger hormone) also stimulates release but plays less of a role
Homeostatic Imbalances of Growth Hormone
Hypersecretion
In children results in gigantism
In adults results in acromegaly
Hyposecretion
In children results in pituitary dwarfism
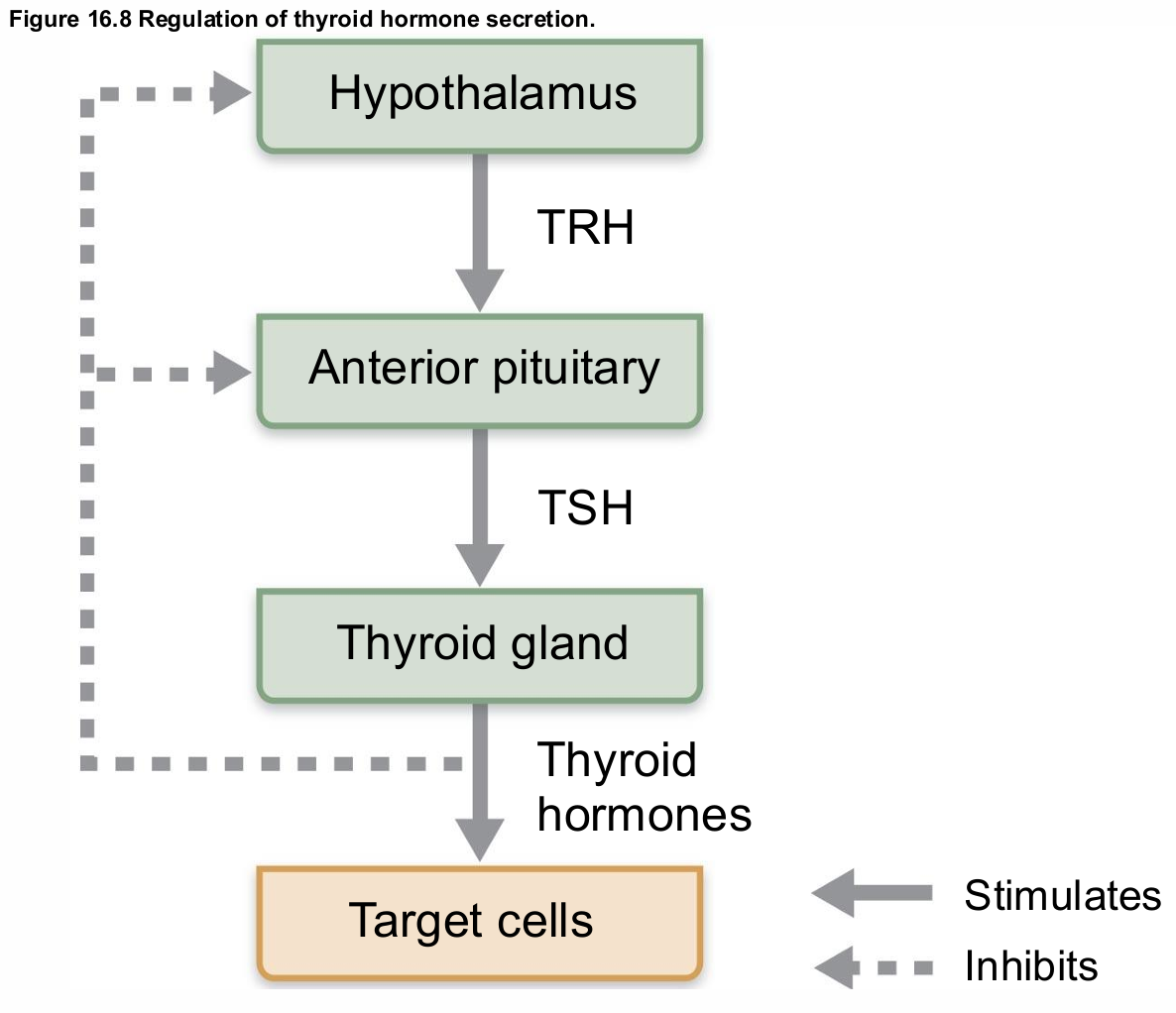
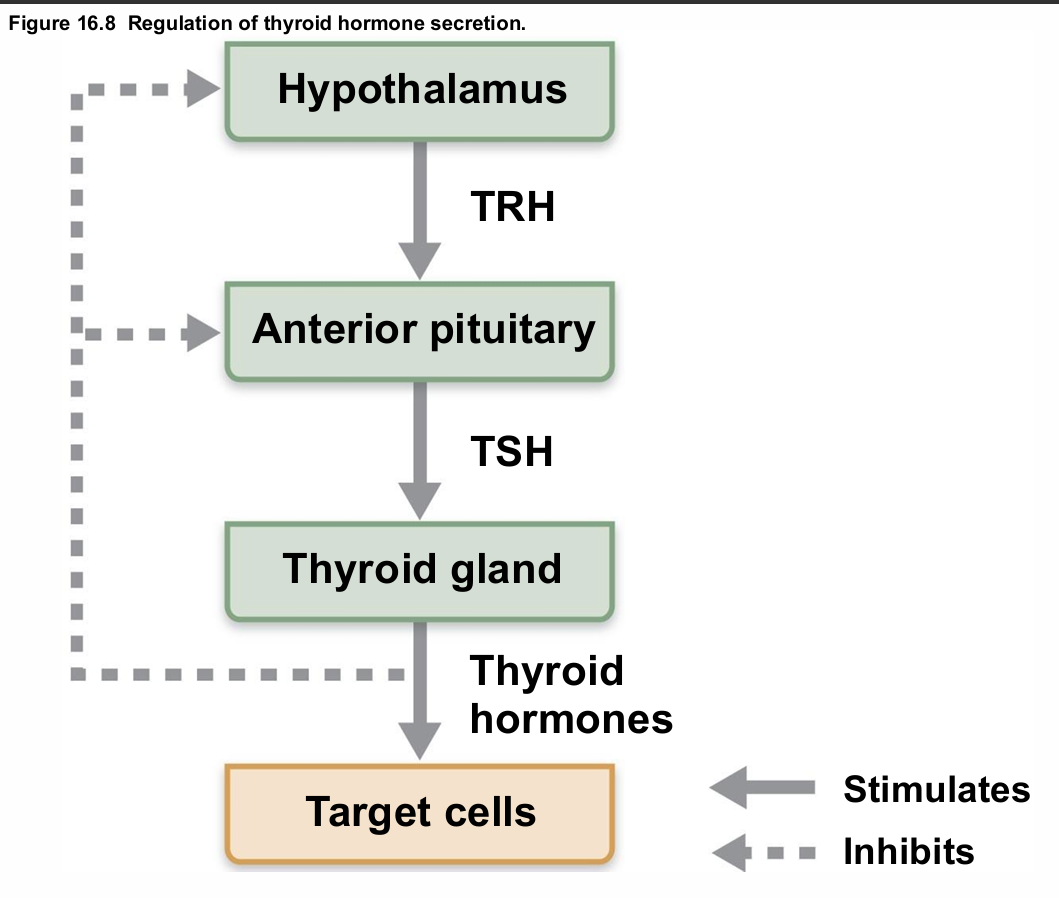
Thyroid Stimulating Hormone
aka Thyrotropin
Produced by thyrotropic cells of anterior pituitary
Stimulates normal development and secretory activity of thyroid
Release triggered by thyrotropin-releasing hormone from hypothalamus
Inhibited by rising blood levels of thyroid hormones that act on pituitary and hypothalamus
Adrenocorticotropic Hormone
aka Corticotropin
Secreted by corticotropic cells of anterior pituitary
Stimulates adrenal cortex to release corticosteroids
Regulation of ACTH release
Triggered by hypothalamic corticotropin-releasing hormone (CRH) in daily rhythm
Internal and external factors such as fever, hypoglycemia, and stressors can alter release of CRH
Gonadotropins
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
Secreted by gonadotropic cells of anterior pituitary
FSH stimulates gamete (egg or sperm) production
LH promotes production of gonadal hormones
Absent from the blood in prepubertal individuals
Regulation of gonadotropin release
Triggered by gonadotropin-releasing hormone (GnRH) during and after puberty
Suppressed by gonadal hormones (feedback)
Prolactin
aka PRL
Secreted by prolactin cells of anterior pituitary
Stimulates milk production
Role in males not well understood
Regulation of PRL release
Primarily controlled by prolactin-inhibiting hormone (PIH) (dopamine)
Blood levels rise toward end of pregnancy
Suckling stimulates PRL release and promotes continued milk production
similar to oxytocin
Hypersecretion causes inappropriate lactation, lack of menses, infertility in females, and impotence in males
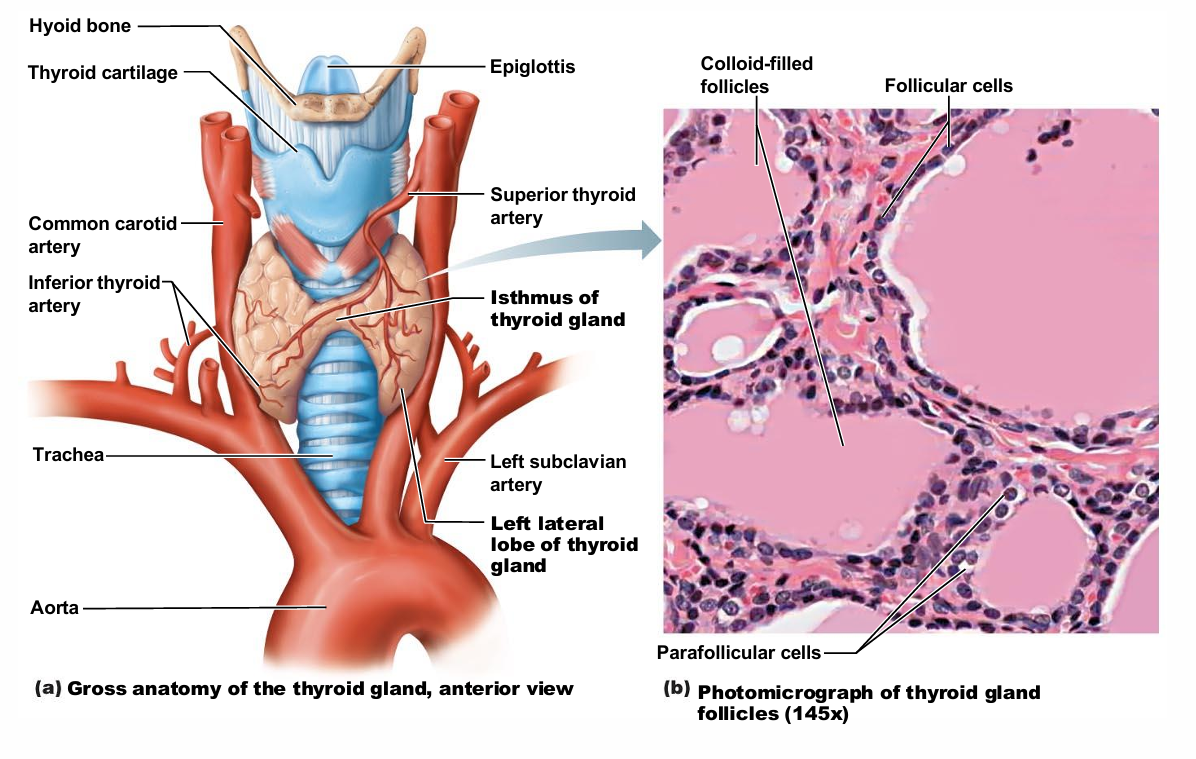
Thyroid Gland
Two lateral lobes connected by median mass called isthmus
Composed of follicles (follicular cells) that produce glycoprotein thyroglobulin
Colloid (fluid with thyroglobulin + iodine) fills lumen of follicles and is precursor of thyroid hormone
Parafollicular cells produce the hormone calcitonin
Thyroid Hormone Structure
Actually two related compounds
T4 (thyroxine); has 2 tyrosine molecules + 4 bound iodine atoms
T3 (triiodothyronine); has 2 tyrosines + 3 bound iodine atoms
Thyroid Hormone
Affects virtually every cell in body
Major metabolic hormone
Increases metabolic rate and heat production (calorigenic effect)
Regulation of tissue growth and development
Development of skeletal and nervous systems
Reproductive capabilities
Maintenance of blood pressure
Synthesis of Thyroid Hormone
Thyroid gland stores hormone extracellularly
Thyroglobulin synthesized and discharged into follicle lumen
Iodides (I–) actively taken into cell and released into lumen
Iodide oxidized to iodine (I2),
Iodine attaches to tyrosine, mediated by peroxidase enzymes
Iodinated tyrosines link together to form T3 and T4
Colloid is endocytosed and vesicle is combined with a lysosome
T3 and T4 are cleaved and diffuse into bloodstream
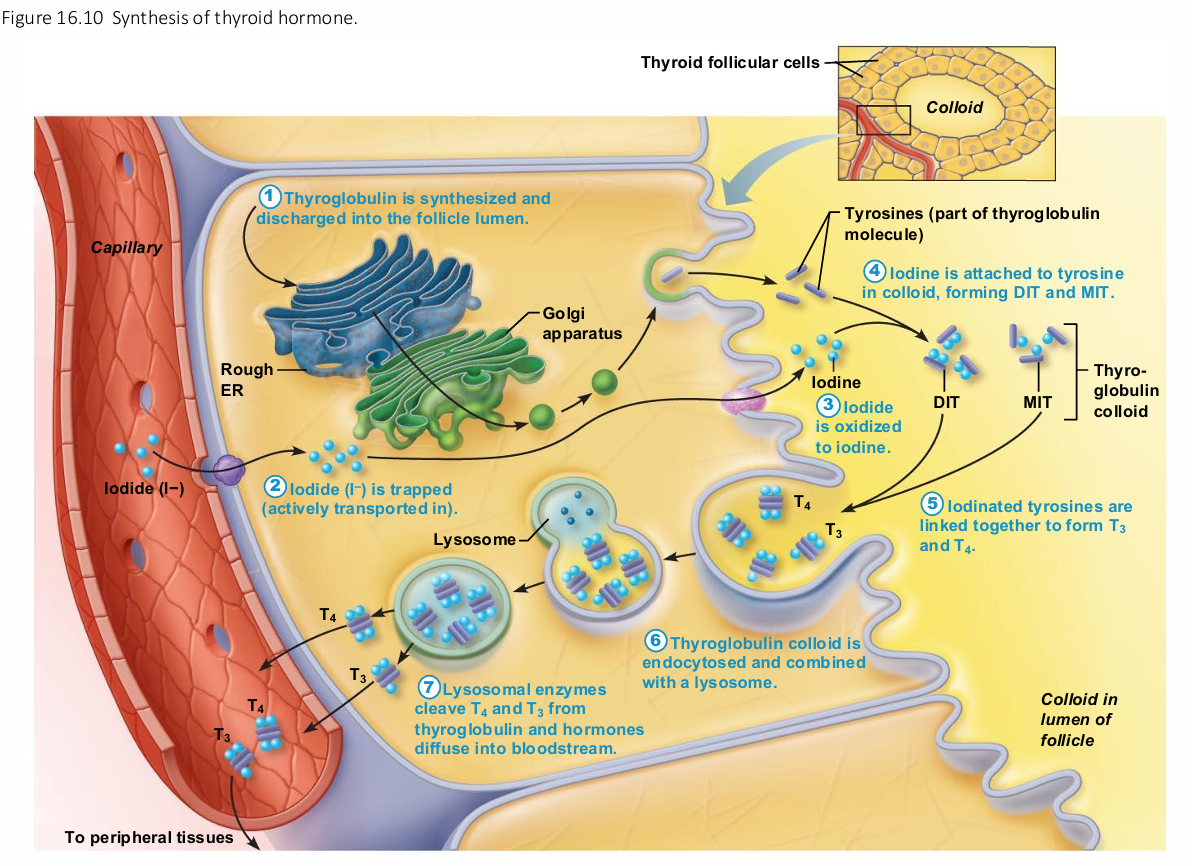
Transport and Regulation of TH
T4 and T3 transported by thyroxine-binding globulins (TBGs)
Both bind to target receptors, but T3 is ten times more active than T4
Peripheral tissues convert T4 to T3
Negative feedback regulation
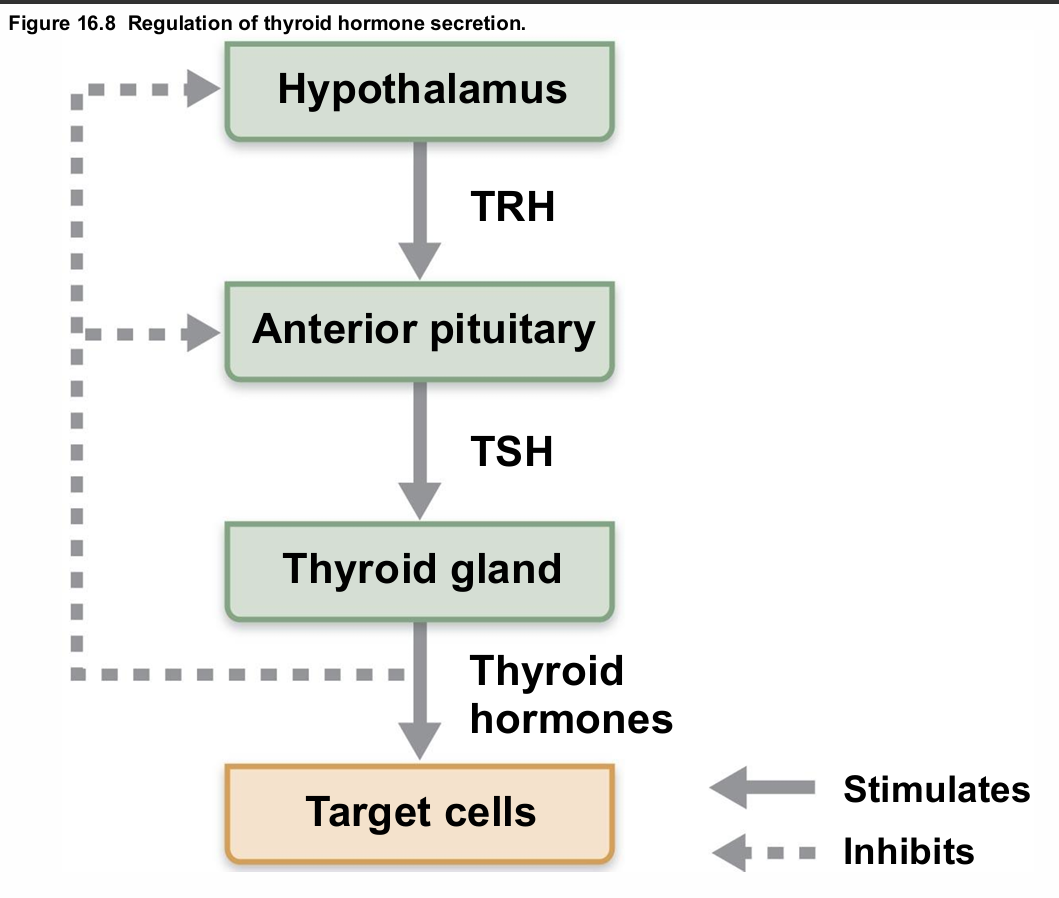
Negative feedback regulation of TH release
Rising TH levels provide negative feedback inhibition on release of TSH
Hypothalamic thyrotropin-releasing hormone (TRH) can overcome negative feedback during pregnancy or exposure to cold
Homeostatic Imbalances of TH
Hyposecretion in adults—myxedema; goiter if due to lack of iodine
Hyposecretion in infants—cretinism
leads to neurological defects if not treated
Hypersecretion—most common type is Graves' disease
obvious sign, eyeball protursion
Calcitonin
Produced by parafollicular (C) cells
No known physiological role in humans
Antagonist to parathyroid hormone (PTH)
At higher than normal doses
Inhibits osteoclast activity and release of Ca2+ from bone matrix
Stimulates Ca2+ uptake and incorporation into bone matrix
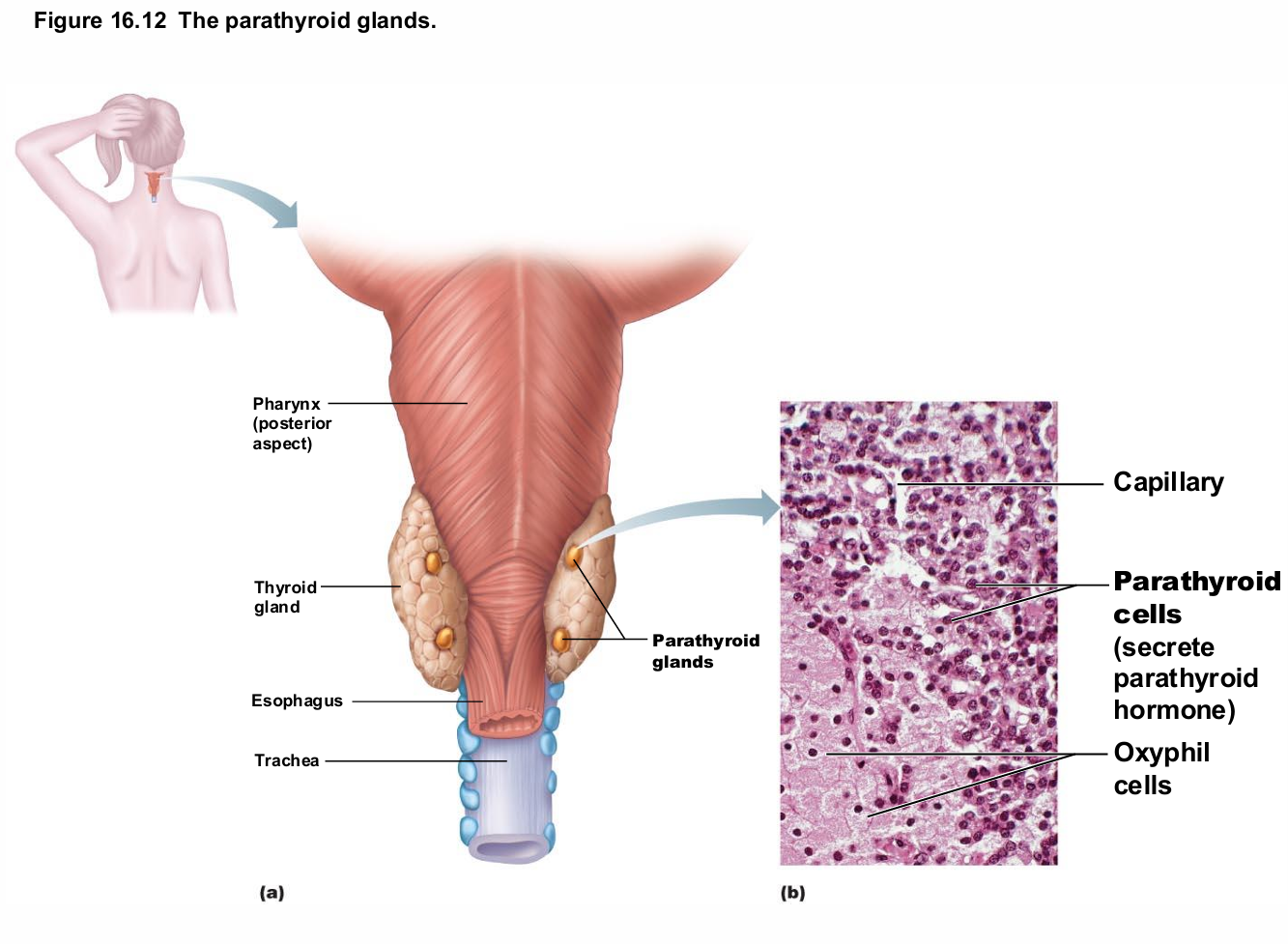
Parathyroid Glands
Four to eight tiny glands embedded in posterior aspect of thyroid
Contain oxyphil cells (function unknown) and parathyroid cells that secrete parathyroid hormone (PTH) or parathormone
PTH—most important hormone in Ca2+ homeostasis
causes degradation of bone to increase Ca2+ in blood
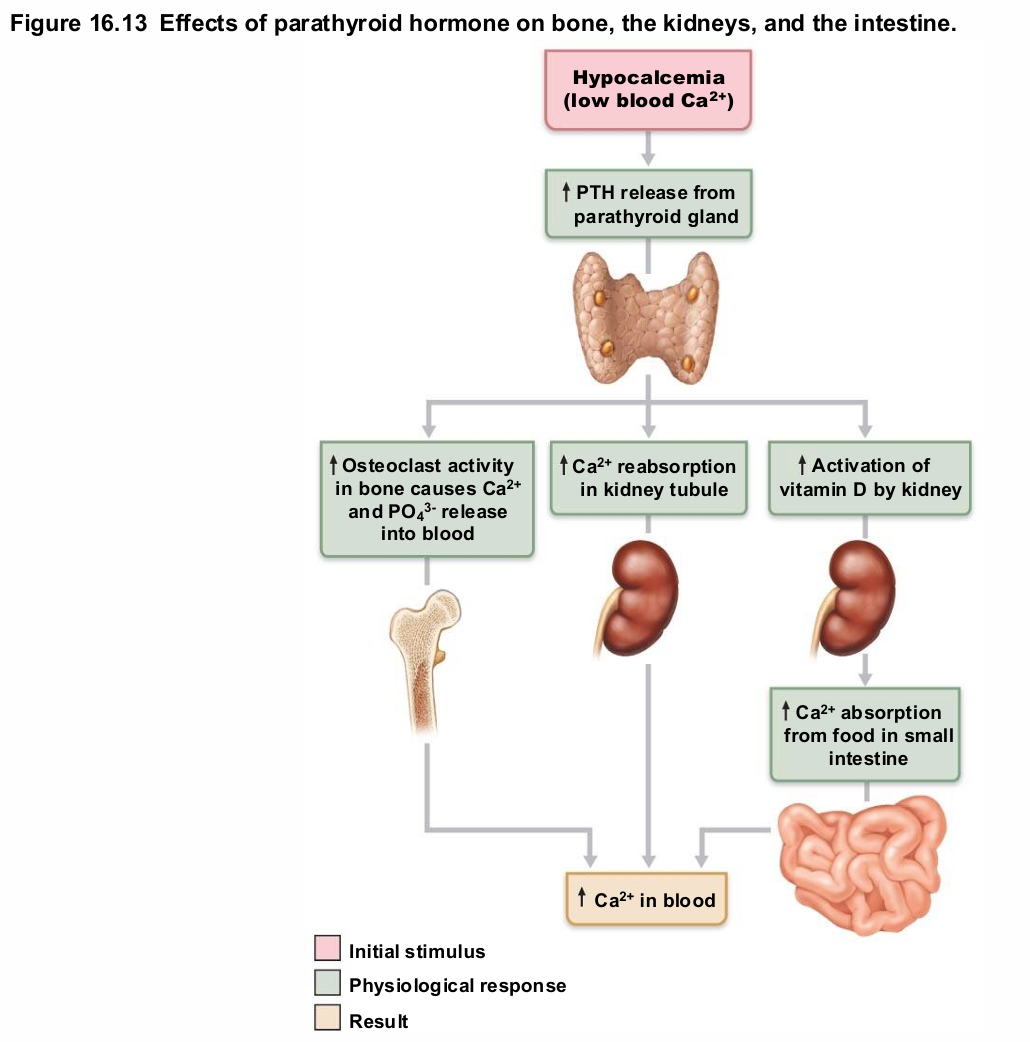
Parathyroid Hormone
Functions
Stimulates osteoclasts to digest bone matrix and release Ca2+ to blood
Enhances reabsorption of Ca2+ and secretion of phosphate by kidneys
Promotes activation of vitamin D (by kidneys); increases absorption of Ca2+ by intestinal mucosa
Negative feedback control: rising Ca2+ in blood inhibits PTH release
Homeostatic Imbalances of PTH
Hyperparathyroidism due to tumor
Bones soften and deform
Elevated Ca2+ depresses nervous system and contributes to formation of kidney stones
Hypoparathyroidism following gland trauma or removal or dietary magnesium deficiency
Results in tetany, respiratory paralysis, and death
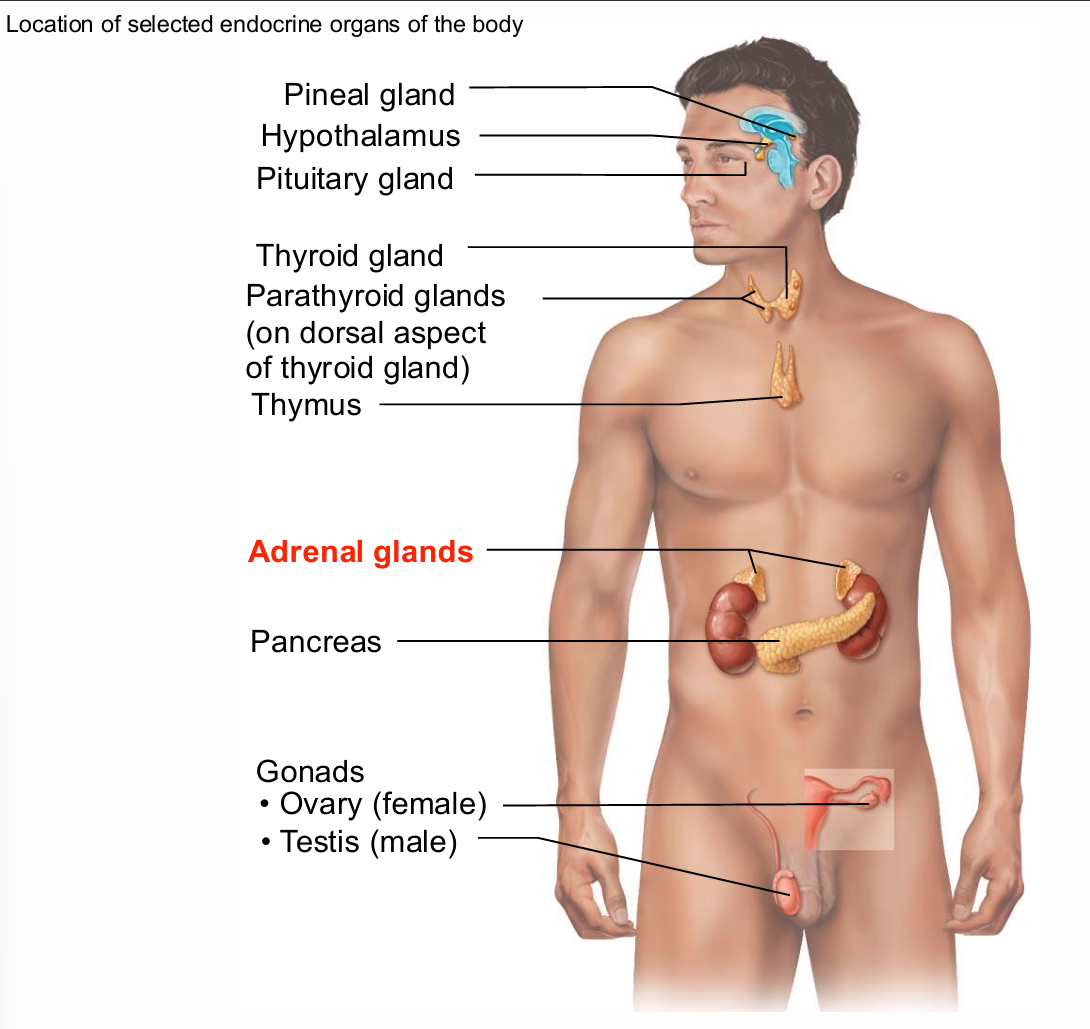
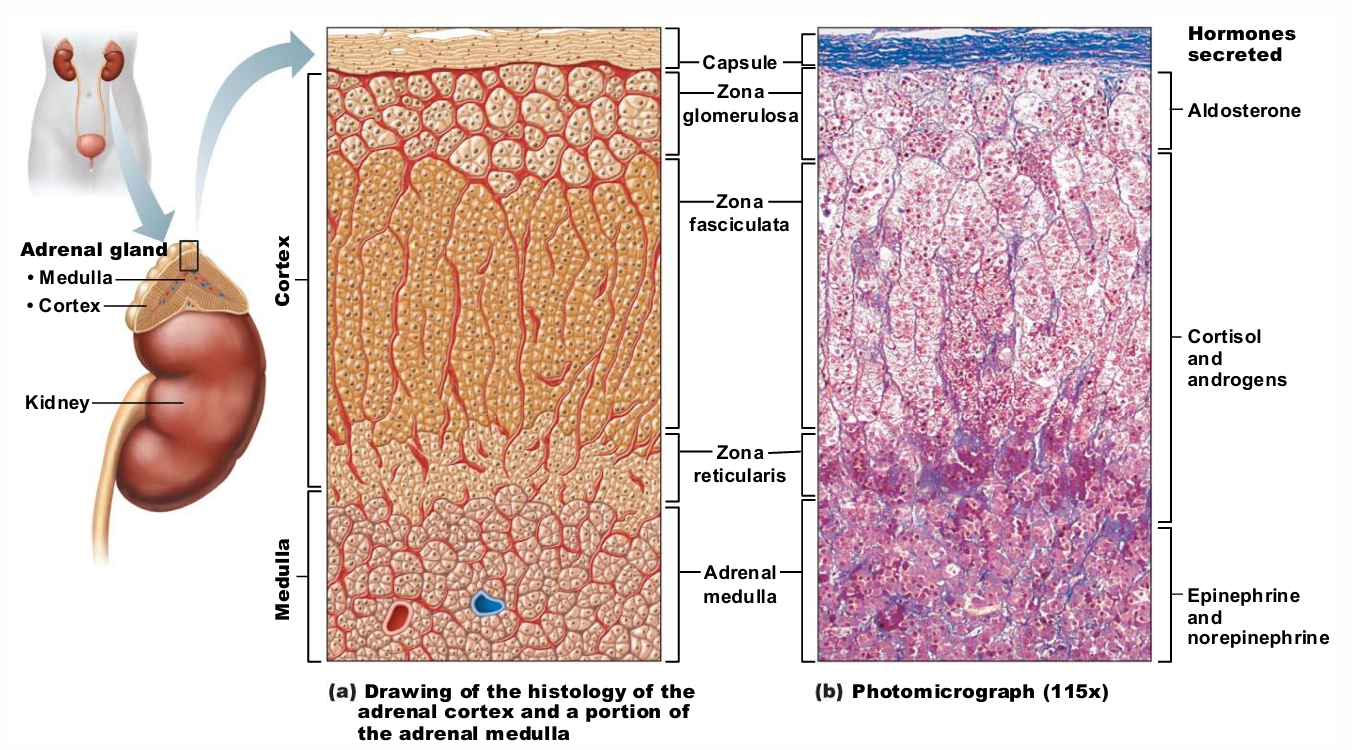
Adrenal Glands
aka suprarenal
Paired, pyramid-shaped organs atop kidneys
Structurally and functionally are two glands in one
Adrenal medulla—nervous tissue; part of sympathetic nervous system
Adrenal cortex—three layers of glandular tissue that synthesize and secrete corticosteroids
Adrenal Cortex
Three layers of cortex produce the different corticosteroids
Zona glomerulosa—mineralocorticoids
Zona fasciculata—glucocorticoids
Zona reticularis—gonadocorticoids
Mineralocorticoids
Regulate electrolytes (primarily Na+ and K+) in ECF
Importance of Na+: affects ECF volume, blood volume, blood pressure, levels of other ions
Importance of K+: sets RMP of cells
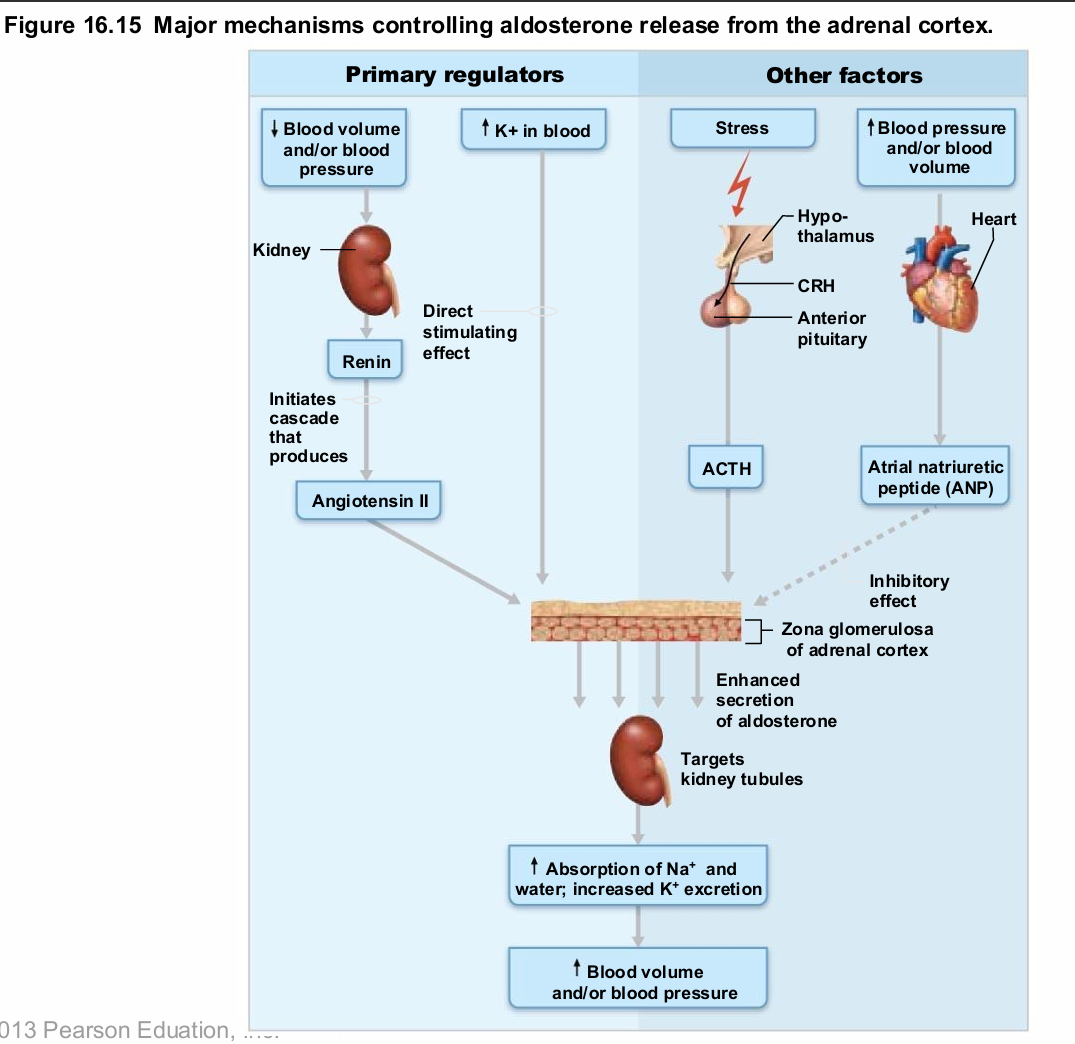
Aldosterone most potent mineralocorticoid
Stimulates Na+ reabsorption and water retention by kidneys; elimination of K+
Aldosterone
Most potent mineralocorticoid
Stimulates Na+ reabsorption and water retention by kidneys; elimination of K+
Release triggered by
Decreasing blood volume and blood pressure
Rising blood levels of K+
Mechanisms of Aldosterone Secretion
Renin-angiotensin-aldosterone mechanism: decreased blood pressure stimulates kidneys to release renin → triggers formation of angiotensin II, a potent stimulator of aldosterone release
Plasma concentration of K+: increased K+ directly influences zona glomerulosa cells to release aldosterone
ACTH: causes small increases of aldosterone during stress
Atrial natriuretic peptide (ANP): blocks renin and aldosterone secretion to decrease blood pressure
Homeostatic Imbalances of Aldosterone
Aldosteronism—hypersecretion due to adrenal tumors
Hypertension and edema due to excessive Na+
Excretion of K+ leading to abnormal function of neurons and muscle