OPP EXAM ONE
5.0(1)
Card Sorting
1/182
There's no tags or description
Looks like no tags are added yet.
Last updated 12:32 AM on 9/1/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
183 Terms
1
New cards
OMT
*Osteopathic Manipulative Treatment*
The therapeutic application of manually guided forces by a physician to improve physiological function and homeostasis that has been altered by somatic dysfunction.
\
The therapeutic application of manually guided forces by a physician to improve physiological function and homeostasis that has been altered by somatic dysfunction.
\
2
New cards
OPP
*Osteopathic Principles and Practice*
Historic term relating to osteopathic philosophy and application.
Course at some colleges of osteopathic medicine.
Historic term relating to osteopathic philosophy and application.
Course at some colleges of osteopathic medicine.
3
New cards
OMM
*Osteopathic Manipulative Medicine*
The application of osteopathic philosophy, structural diagnosis, and use of osteopathic manipulative treatment (OMT) in the diagnosis and management of the patient.
The application of osteopathic philosophy, structural diagnosis, and use of osteopathic manipulative treatment (OMT) in the diagnosis and management of the patient.
4
New cards
NMM
*Neuromusculoskeletal Medicine*
Specialty that emphasizes the incorporation of osteopathic manual diagnosis and osteopathic manipulative treatment into the evaluation and treatment of the nervous, muscular, and skeletal systems in their relationships to other systems of the body as well as the whole person.
5
New cards
ONMN
*Osteopathic Neuromusculoskeletal Medicine*
A primary ACGME residency program disciplined in the neuromusculoskeletal system, its comprehensive relationship to other organ systems, and its dynamic function of locomotion.
A primary ACGME residency program disciplined in the neuromusculoskeletal system, its comprehensive relationship to other organ systems, and its dynamic function of locomotion.
6
New cards
The 4 Tenets of Osteopathic Medical Philosophy
•The body is a unit; the person is a unit of body, mind, and spirit.
\
•The body is capable of self-regulation, self-healing, and health maintenance.
\
•Structure and function are reciprocally interrelated.
•Rational treatment is based upon on these principles
7
New cards
Somatic Dysfunction
Impaired or altered function of related components of the somatic (body framework) system.
This may include skeletal, arthrodial, and myofascial structures and related vascular, lymphatic, and neural elements.
8
New cards
What is the purpose of OMT?
1. Hands-on treatment aimed at:
1. Resolving primary and secondary somatic dysfunctions
1. Additional Goals:
1. Improving homeostatic mechanisms (e.g., respiratory, circulatory, immune, etc.)
2. Improving energy efficiency (e.g., reduction of the work of breathing or more efficient gait)
3. Reduction of inappropriate afferent neural stimuli
9
New cards
What are the goals of OMT?
1. Normalize structure
2. Increase functional movement
3. Remove impediments to nervous and arterial supply and venous/lymphatic return
4. Restore correct anatomical/functional relationships (correct somatic dysfunction)
5. Restore normal vascular supply (arterial)
6. Improve venous/lymphatic drainage (reduce stagnation, congestion)
7. Improve neurological function (reduce entrapments/balance ANS)
8. Remove viscerosomatic or somatovisceral reflexes and other impedances to homeostasis
9. Reduce or eliminate pain
10. Stimulate the immune system Prevent recurrences
10
New cards
The only indication for OMT is….
Somatic dysfunction
11
New cards
Who founded the osteopathic medical profession?
Andrew Taylor Still, MD, DO
12
New cards
What was the year that he said he discovered osteopathy?
1874
13
New cards
What was the name of the first osteopathic medical school? What year was it founded? Where was it founded?
American School of Osteopathy
1892
Kirksville, MO
1892
Kirksville, MO
14
New cards
If you had to express the osteopathic philosophy in about a five word sentence, what would it be?
Seek health in your patients
\
\
15
New cards
What are the two most common presenting complaints which may indicate the need for OMT?
Pain & ROM
16
New cards
Name the two values/conditions in the muscles and bones which are generally set to pathological values in somatic dysfunction, and are the first gross values reset by OMT?
Muscle length and tension
Joint surface apposition
Joint surface apposition
17
New cards
“The rule of the artery is: ______”
Supreme
18
New cards
The first state to license the practice of osteopathy was:
Vermont, 1896
19
New cards
The last state to license the practice of osteopathic medicine was:
Mississippi, 1973
20
New cards
What are the five models of somatic function and dysfunction?
Biomechanical, Respiratory-Circulatory, Neurological, Metabolic-energy
21
New cards
What is significant about 1971?
Arkansas granted Osteopathic Physicians the right to apply for unlimited licensure
22
New cards
What do we D.O.?
\
If we combine our knowledge of anatomy, physiology, and pathophysiology, we can develop safe, effective, and rational treatment methods for our patients.
If we combine our knowledge of anatomy, physiology, and pathophysiology, we can develop safe, effective, and rational treatment methods for our patients.
23
New cards
**“________ are for situations we imagine.**
**________ are for ones we don’t.”**
Techniques, Principles
24
New cards
Unconscious Incompetence
Does not necessarily recognize the deficit. May deny the usefulness of the skill. *Wrong Intuition.*
25
New cards
Conscious Incompetence
Recognizes the deficit and sees value in a new skill. Doesn’t yet know how to do the new skill. *Wrong analysis.*
26
New cards
Conscious Competence
Two Parts: Knowledge, Practice
Understands and knows how to do something. Heavy conscious involvement in executing the new skill. *Right Analysis.*
\
Understands and knows how to do something. Heavy conscious involvement in executing the new skill. *Right Analysis.*
\
27
New cards
Unconscious Competence
The skill is “second nature” and can be performed easily. Can teach others. *Right Intuition.*
28
New cards
Posture
**is the shape and position of the body when under the effects of gravity.**
29
New cards
Optimal Posture
Reduces stress on the body due to gravity during exertion.
Optimal __posture__ is a perfect distribution of the body mass around the center of gravity.
•This is achieved when postural muscles are at resting tone with no additional energy beyond basal level needed for upright posture.
Optimal __posture__ is a perfect distribution of the body mass around the center of gravity.
•This is achieved when postural muscles are at resting tone with no additional energy beyond basal level needed for upright posture.
30
New cards
Gait
Posture in Motion
31
New cards
Optimal Gait
is the maximization of energy transformation into motion.
This is achieved when the three distinct oscillatory motions of gait summate with minimal interference, maximizing energy transformation into motion.
32
New cards
Kyphosis
is the primary curve of the vertebral column at birth.
33
New cards
When do the cervical and lumbar lordosis develop?
Cervical lordosis accentuates around 4-7 months.
Lumbar lordosis develops after 12 months
34
New cards
When does a child typically take its first steps?
12mo
35
New cards
How do we analyze posture?
a.External Auditory Meatus
b.Lateral Humeral Head
c.Body of L3
d.Anterior 1/3 of sacrum
e.Greater Trochanter
f.Lateral Femoral Condyle
g.Anterior lateral Malleolus
36
New cards
Wolff’s law
bone remodels due to stress
37
New cards
What is a moment arm?
A moment arm is the length between a joint axis and the line of force acting on that joint. The longer the moment arm, the more load will be applied to the joint axis through leverage.
38
New cards
Shopping Cart Sign
Lumbar spinal stenosis can cause a person to lean forward in order to open the lumbar facets and take pressure off the nerves.
39
New cards
Scoliosis: *Definition, Screening Test, Mechanics, Obtaining Definitive Diagnosis.*
Curvature of the spine in the coronal plane.
Screen with Adams forward bending test.
Vertebrae tend to side bend in one direction and rotate in the opposite direction (this is also known as Type 1 Mechanics).
Rib problems common given the rib interface with 2 vertebral segments.
Definitive diagnosis by radiograph and measurement of Cobb angle.
40
New cards
What can we use to name and describe scoliosis?
S-curve or C-curve?
Region?
Convexity?
to the right = dextroscoliosis
to the left = levoscoliosis
Cobb angle? (from radiograph)
Apex?
Region?
Convexity?
to the right = dextroscoliosis
to the left = levoscoliosis
Cobb angle? (from radiograph)
Apex?
41
New cards
Adam’s Forward Bending Test
1\.Perform Adam’s forward bending test.
*A prominence of the rib cage (rib humping) on one side of the spine indicates a positive screen for scoliosis.*
2\.Next, have patient side-bend towards side of rib humping.
*If the rib humping reduces it is considered a* __***Functional Scoliosis***__*. Functional Scoliosis is reversible with treatment.*
*If rib humping remains fixed with positional changes the scoliosis is* __***Structural***__*. Structural Scoliosis is irreversible without surgery.*
42
New cards
Gait Cycle
One gait cycle is heel contact from one foot through heel contact of the SAME foot.
Swing Phase accounts for 40% of gait cycle
Stance Phase (single and double) accounts for 60% of gait cycle
Double Stance occurs in 20% of gait cycle
The vulnerable phases of gait are:
Heel strike to loading response
Midstance

43
New cards
Weight shifts to side of _____ leg.
planted
44
New cards
**Sacral And Innominate Motion**
•Sacrum moves in a forward torsional pattern on an oblique axis ipsilateral to the side of the planted leg.
•During leg swing the lumbar spine sidebends towards the planted leg and rotates toward the side of the swinging foot.
•The Innominate of the swinging leg rotates posteriorly and flares inward (i.e. rotates to side of planted leg on a vertical axis)
45
New cards
Pronation is a combination of
eversion, abduction, and dorsiflexion of the foot
46
New cards
Primary motion/function of pronation during gait
Eversion (subtalar joint)
Eccentric deceleration and shock absorption.
Eccentric deceleration and shock absorption.
47
New cards
Supination is commonly described as a combination of
inversion, adduction, and plantarflexion of the foot
48
New cards
Primary Motion/Function
**Inversion (subtalar joint)**
**Concentric acceleration and initiation of propulsion**
49
New cards
What are the three main events of energy conservation and gait?
1. Propulsion during push off
1. Propelling the center of mass (COM) up and forward
2. Controlling forward movement
1. COM “falls” forward
2. Deceleration at the end of the cycle
3. Shock absorption at heel strike
50
New cards
**Energy is conserved when the COM is**
**minimally displaced during gait.**
**(e.g. vertical, medio-lateral, and antero-posterior)**
51
New cards
**The most common ankle sprain is an**
**inversion ankle sprain.**
52
New cards
Midstance
one foot is bearing all the weight and in a neutral position. Knee ligaments are more vulnerable without the myofascial forces associated with pronation and supination of the foot.
\
\
53
New cards
Vulnerable phases of gait
Heel strike to loading response phase, the talus is loose from slight plantar flexion and vulnerable to inversion.
54
New cards
Antalgic Gait
(gait to avoid pain) A limp is adopted to avoid pain on weight bearing structures (hip, knee, ankle). Typically, the stance phase is shortened relative to the swing phase on the affected side (e.g. knee pain on the right decreases the stance phase of the right leg)
55
New cards
Ataxic Gait
An unsteady, uncoordinated walk, a wide base of support. Often due to cerebellar problem (e.g. intoxication, stroke). Can also be due to sensory ataxia (e.g. peripheral neuropathy)
\
\
56
New cards
Fenestrating Gait
short, accelerating steps are used to move forward, often seen in patients with Parkinson’s Disease \*\* (i.e. Shuffling Gait)
57
New cards
Hemiplegic Gait
involves unilateral flexion and circumduction of the hip due to weak extensors. Will se ipsilateral upper extremity flexion. Common post stroke.
\
\
58
New cards
Spastic Gait (Diplegic)
walk in which legs are held close together and move in a stiff manner, bilaterally. (e.g. scissor gait in patients with cerebral palsy)
\
\
59
New cards
Trendelenburg Gait
an abnormal gait caused by weakness of the abductor muscles of the lower limb (gluteus medius and gluteus minimus)
\
\
60
New cards
Steppage Gait (Foot Drop Gait)
gait in which the advancing foot is lifted higher than usual so that it can clear the ground (decreased/absent dorsiflexion). Seen in L5 and fibular neuropathies leading to weakened dorsiflexion.
61
New cards
At each visit, healthcare providers should ask at risk patients and patients >65 years of age:
\
\
Do they feel unsteady or worry about falling when standing or walking? Have they fallen in the past year ?
62
New cards
What are the **cardinal findings of somatic dysfunction?**
Tissue Texture Abnormalities
Asymmetry
Restriction of Motion
Tenderness
\
Asymmetry
Restriction of Motion
Tenderness
\
63
New cards
How many TARTs are required to diagnose somatic dysfunction?
Two
64
New cards
What are some manifestations of somatic dysfunction?
Altered muscle length and tension (imbalance/spasm). **Often chronic conditions.**
Altered connective tissue tensions (fascia/ligaments).
Joint surface malposition.
\
*Important to have a history when diagnosing*
Altered connective tissue tensions (fascia/ligaments).
Joint surface malposition.
\
*Important to have a history when diagnosing*
65
New cards
What is muscular Imbalance? How might this occur?
Occurs when the length and tensions of related muscles are unequal.
\
* Gravitational strain (posture related)
* Trauma
* Over-use (microtrauma)
* Compensation from any of the above
\
\
* Gravitational strain (posture related)
* Trauma
* Over-use (microtrauma)
* Compensation from any of the above
\
66
New cards
What are some effects of muscle imbalance on function?
* Affect dynamic function
* Alter proprioception
* Arthrodial instability due to imbalanced loads on joint surfaces
* Change joint structure
* Impede neurovascular function
* Alter proprioception
* Arthrodial instability due to imbalanced loads on joint surfaces
* Change joint structure
* Impede neurovascular function
67
New cards
Proprioception
is the subconscious mechanism involved in the self-regulation of posture and movement.
\
\
Large A-alpha fibers offer afferent input into the system from stimuli originating in receptors imbedded in every joint, tendon, and muscle and combine with information from the vestibular system to interpret the position and change in position of the soma.
\
\
Large A-alpha fibers offer afferent input into the system from stimuli originating in receptors imbedded in every joint, tendon, and muscle and combine with information from the vestibular system to interpret the position and change in position of the soma.
68
New cards
How does somatic dysfunction alter the interpretation of Stimuli?
This leads to a maladaptive, feedforward, allostatic cascade (i.e. “vicious cycle”) which can affect pain interpretation, inflammatory cascades, and protective reflexes.
\
\
69
New cards
Tensegrity
“the property of skeletal structures that employ continuous tension members and discontinuous compression members in such a way that each member operates with the maximum efficiency and economy.”
\
The way in which bony tension elements are held together by connecting elastic elements (ligaments and antigravity muscles), which helps create/maintain the balance between stability and strength
\
Fascial and musculoligamentous tensions take on primary importance as connecting elements within the system.
\
Imbalance within the system can lead to dysfunction of the system.
\
Nothing happens in isolation.
\
The predictable total structural response to tension change anywhere in the body
\
The way in which bony tension elements are held together by connecting elastic elements (ligaments and antigravity muscles), which helps create/maintain the balance between stability and strength
\
Fascial and musculoligamentous tensions take on primary importance as connecting elements within the system.
\
Imbalance within the system can lead to dysfunction of the system.
\
Nothing happens in isolation.
\
The predictable total structural response to tension change anywhere in the body
70
New cards
Regional Interdependence
Describes the clinical observations related to the relationship purported to exist between regions of the body, specifically with respect to the management of musculoskeletal disorders.
\
*“Dysfunction in any unit of the system will cause delivery of abnormal stresses to other segments of the system with the development of a subsequent dysfunction here as well.”*
\
*“Dysfunction in any unit of the system will cause delivery of abnormal stresses to other segments of the system with the development of a subsequent dysfunction here as well.”*
71
New cards
Tissue Texture Abnormalities
Temperature, Moisture (skin drag), Red reflex, Bogginess, Ropiness, stringiness
\
\
•May be present in many ways
•May not cause the dysfunction
•Can be as a result of the dysfunction
•May be remote from the dysfunction
•May be the dysfunction
•Tissue may be – edematous, tender, fibrosed, rigid, atrophied (thin), hypertonic or many other things
•Doesn’t feel normal. You have to know what normal feels like
\
\
•May be present in many ways
•May not cause the dysfunction
•Can be as a result of the dysfunction
•May be remote from the dysfunction
•May be the dysfunction
•Tissue may be – edematous, tender, fibrosed, rigid, atrophied (thin), hypertonic or many other things
•Doesn’t feel normal. You have to know what normal feels like
72
New cards
Asymmetry of Tissues
Static (no active or passive motion)
Regional Examination
Segmental Examination
\
Regional Examination
Segmental Examination
\
73
New cards
Restriction of Motion
Superficial fascia
Muscles
Deep fascia
Joints
\
Muscles
Deep fascia
Joints
\
74
New cards
Physiologic Barrier
A point at which a patient can actively move any given joint. For example, a person may actively rotate his head 80 degrees to either side
Limit of __**Active**__ Range of motion
Limit of __**Active**__ Range of motion
75
New cards
Elastic Barrier
the range between the physiologic and anatomic barrier of motion in which passive stretching (induced by the physician) occurs before tissue disruption.
Range between the physiologic and anatomic barrier of motion in which passive ligamentous stretching occurs before tissue disruption. Usually a very short distance. Ex. From physician
Range between the physiologic and anatomic barrier of motion in which passive ligamentous stretching occurs before tissue disruption. Usually a very short distance. Ex. From physician
76
New cards
Anatomic Barrier
A point at which if any movement occurs past this point it will result in disruption of tissue (muscle, ligament, tendon, bone).
\
Limit of motion imposed by an anatomic structure; the limit of __**passive**__ range of motion.
\
Limit of motion imposed by an anatomic structure; the limit of __**passive**__ range of motion.
77
New cards
Restrictive Barrier
A functional limit that abnormally diminishes the normal physiologic range. Ex. somatic dysfunction
\
Barrier lies before the physiologic barrier, and prevents full range of motion of that joint
\
A functional limit within the anatomic range of motion, which will diminish the normal physiology range
\
***For Example***, head can rotate 80 degrees left/right – restrictive barrier only lets the head rotate 60 degrees to the left and 80 degrees to the right. There may be some tenderness at the restrictive barrier.
\
\
Barrier lies before the physiologic barrier, and prevents full range of motion of that joint
\
A functional limit within the anatomic range of motion, which will diminish the normal physiology range
\
***For Example***, head can rotate 80 degrees left/right – restrictive barrier only lets the head rotate 60 degrees to the left and 80 degrees to the right. There may be some tenderness at the restrictive barrier.
\
78
New cards
79
New cards
Pathologic Barrier
Restriction of joint motion associated with pathologic change of tissues (think of arthritis or a fracture)
80
New cards
Motion loss is a result of and maintained by a __________.
restrictive barrier
81
New cards
The restrictive barrier is a result of:
\
\
somatic dysfunction
82
New cards
Tenderness
Discomfort or pain elicited by the practitioner through palpation. A state of unusual sensitivity to touch or pressure (Dorland’s).
83
New cards
Pain
an unpleasant sensation induced by noxious stimuli and generally received by specialized nerve endings
84
New cards
Hypertonic Muscle
difficulty relaxing, enlarged, tense
\
\
85
New cards
Hypotonic Muscle
weakened contraction and neurtrophism
\
\
86
New cards
Ropiness of muscle
isolated contracted fibers, cord/string like
87
New cards
Trigger Points
small discrete hypersensitive areas within myofascial structures - palpation causes referred pain away from site
88
New cards
Fibrotic Muscle
dehydrated, poss. course and contracted
\
\
89
New cards
Dense Muscle
usually tight, restrictive and thickened
\
\
90
New cards
Spastic Muscle
Severely restrictive (chronic)
\
\
91
New cards
Boggy muscle
Non-edematous but increased fluid with decreased turgor, freq. viscero-somatic
92
New cards
How much pressure should you use?
Blanching of thumbnail or fingernail occurs typically between 1 and 4 kg of pressure
\
Tenderness may be reported at levels of 8 kg of pressure with no discernable dysfunction
\
Tenderness may be reported at levels of 8 kg of pressure with no discernable dysfunction
93
New cards
Tender Point
small discrete hypersensitive areas within myofascial structures that result in localized pain
\
\
94
New cards
Chapman’s Point
small discrete nodular area located deep to the subcutaneous tissues, most often in the deep fascia or periosteum of the bone
95
New cards
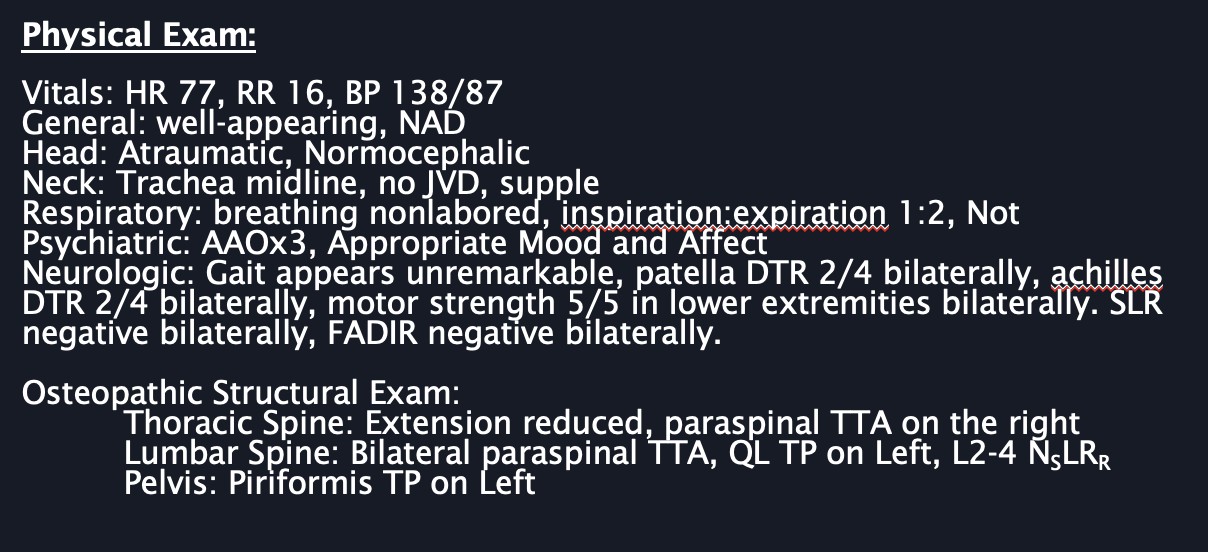
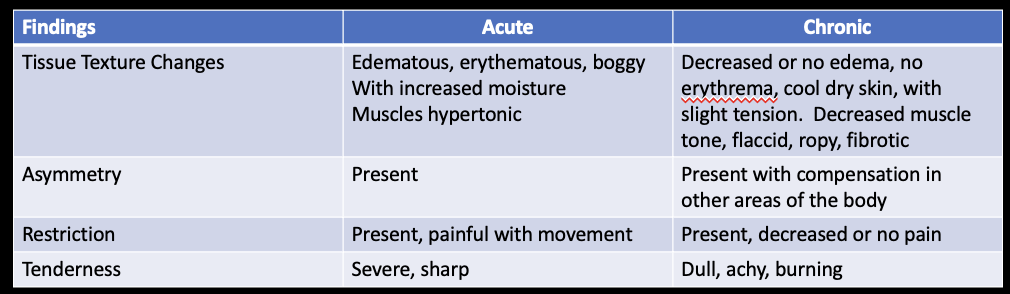
Describe an example of acute vs chronic TART findings.
\
96
New cards
Somatic Dysfunction is named
for the way they like to go
*IF* a vertebrae rotates freely to the left but is restricted to the right then the dysfunction rotates left
*IF* the elbow will flex but not extend then the dysfunction is flexed
\
*IF* a vertebrae rotates freely to the left but is restricted to the right then the dysfunction rotates left
*IF* the elbow will flex but not extend then the dysfunction is flexed
\
97
New cards
Primary vs. Secondary Somatic Dysfunction
*Primary*: the somatic dysfunction(s) that maintains a total pattern of dysfunction, including other secondary dysfunctions.
\
*Secondary*: somatic dysfunction arising either from mechanical or neurophysiologic response subsequent to or as a consequence of other etiologies.
\
\
*Secondary*: somatic dysfunction arising either from mechanical or neurophysiologic response subsequent to or as a consequence of other etiologies.
\
98
New cards
Always start your exam with
observation
99
New cards
True or False. You document that the patient is presenting to the clinic for OMT.
False
100
New cards
Exmaple of Physical Exam