Honors Biology - Immune System Test
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
microbe
any microscopic living organism (something you need a microscope to see)
indicates → size and living status
does not indicate → helpful or harmful
ex. Bacteria, viruses, fungi (like yeasts and molds).
pathogen
any biological agent that causes disease
indicates → harmful
not indicated → size or living status
Examples
bacteria
fungi (some microscopic, some not)
protists,
viruses → not living (no cells) → not microbes
prions → infectious proteins (not living → not microbes); misfolded proteins that cause brain disease
multicellular parasites (tapeworms, etc.)
allergens
substance that causes an allergic (immune) response
Specific molecules, such as food proteins and pollen grains, which noninfectious, but the immune system mistakenly recognizes them as threats and reacts like they are dangerous invaders.
innate immune response
The body’s first line of defense against an invader
non-specific → the response is independent of the type of invader (same for all)
born with innate response
adaptive (aquired) immune response
A specific immune response that develops over time after exposure to a pathogen
Occurs when the innate response is insufficient
slower, but more efficient
It involves the activation of lymphocytes (T cells and B cells) that target specific antigens. mature by developing receptors on cell surface on last page of lesson 2
Arises b/c exposure to antigen
natural exposure (active immunity) → sick, infected by pathogen
artificial exsposure (active immunity) → vaccines
can also get passive immunity from breast milk or antivenom
innate external barriers (physical, chemical, biological)
prevents pathogens from entering the body
Ex. mechanical barriers, chemical barriers, biological barriers
Mechanical barriers
external barriers like skin and hair
mucous membranes → line internal surfaces that are open to the enviroment (urinary, digestive, etc.)
mucus provides protection for cells below the mucus → prevents progress of foreign invader
in respatory system → cilia allow for mucus w/ particles/invaders to be brought to pharynx
Chemical barriers
chemicals near openings and on inner linings that protect non-specifically
mucus-producing cells also make antibacterial enzymes
in digestive system: gastic juice (low pH → acidic)
in urinary system: uring (acidic)
in reproductive system: vaginal secretion (acidic)
biological barriers
living organisms that destroy invaders non specifically
good bacteria in digestive tract + reproductive system → keep invaders from proliferating b/c have to complete with good bacteria
innate internal defense
if first part of the innate defense (external) is breached and foreign invader enters the body, the internal defenses are used to prevent further infection
Ex. innate immune cells, defensive proteins, inflammatory response, and fever response
innate immune cells (types of white blood cells)
part of innate internal defenses and work non specifically (before the adaptive response)
Phagocytes
nuetrophils (circulate in blood)
macrophages (circulate in interstitial fluid)
target foreign invaders with phagocytosis (engulf substances from enviroment → with food vacuoles and lysosomes)
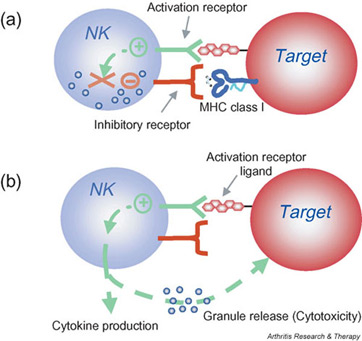
Natural Killer Cells (NKCs)
kill infected body cells (virus, cancerous) non-specifically
scan the body for cells that are missing their “ID tags”
not invaders but infected/damaged cells “self cells”
defensive proteins
function non-specifically - before the adaptive response gets activated
interferons (proteins)
infected cell detecrs infection → makes interferon (secretory protein) → go to another cell → causes production of antiviral proteins
complement system of proteins → help mark pathogens for destruction and enhance inflammatory response.

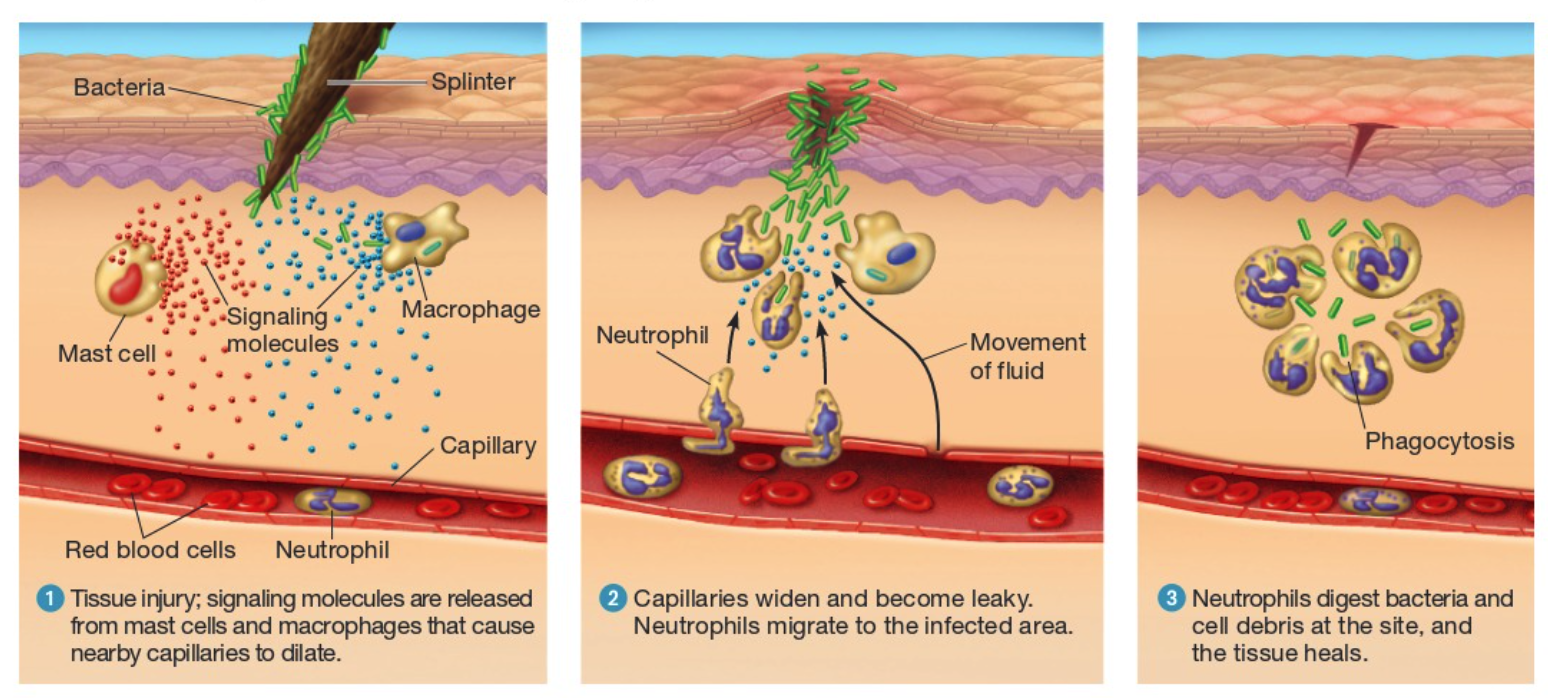
inflammatory response
Purpose: to disinfect and clean injured tissues
Step 1 → Tissue injury; signaling molecules are released from mast cells and macrophages that cause nearby capillaries to dilate (goal to get more blood)
The presence of bacteria causes the activation of two types of white blood cells
macrophages produce signaling molecules → bring fluid to the infecred area (more blood flow to the area)
mast cells → release histamines that cause blood capillary dialation (widens) → larger diameter needed for more blood + capillaries become leaky
Step 2 → Materials are released from the blood through the widened and leaky vessels
Materials (below) are released from the blood through the widenend and leaky vessels
plasma → fluid in blood
clotting proteins → aid in clotting
platelets → makes clot; cell fragments
activated complement proteins attract phagocytes from blood (nuetrophils)
Results in swelling, warmth, and redness
Step 3 → Bacteria are englufed by nuetrophils
pus → dead cell debris
Nuetrophils eventually die or are destroyed
fever
raise the set point (ideal temp)
a response to a systematic (widespread, whole body) infection
antigen
any molecule or particke that elicits an immune response
ex. proteins on the capsule of bacteria and viruses as well as venom
adaptive immunity remember the antigen
They can be bound to a pathogen or be free floating.
lymphatic system (two functions)
network of tubes, tissues, and organs that help maintain fluid balce in the body and supports immune function.
Circulatory Function → to return fluid back to the circulatory fluid
20 L (plasma) leaked into interstitial fluid → 17L reabsorbed → 3L become lymph (absorbed into lymphatic capillaries)
plasma (when in capillaries) → interstitial fluid (interstial spaces) → lymph (lymphatic vessels)
Immune Funtion → to filter interstitial fluid to remove/destroy invaders
lymphatic capillaries are intertwined with blood capillaries to collect fluid that exits the blood
eventually returned to the blodstream (lymph nodes = filtering)
Sturucture
Tubes
lymphatic system structure (tubes and tissues)
Tubes → transport of lymph/fluids through lymphatic capillaries and vessels
Tissues → concentrations/groupings of immune cells that are not organized into a defined organ but work together to protect a region of the body
ex. Peyers patches (cluster of lymphocytes found in mucous layer of small intestine)
ex. tonsils = clusters of lymphocytes found in the oral cavity
lymphatic system structure (organs)
primary lymphoid organs → where lympocytes develop and mature
red bone marrow → where blood cells are produced, lymphocytes (including NKCs) are made, and where B-cells (B for bone marrow) mature
thymus → location where T cells (T for thymus) mature
secondary lymphoid organs → where lymphocytes mount their immune response; contain B and T cells and macrophages to detect and attack invaders
lymph nodes → lymph nodes filter the lymph that flow through it. Contain masses of lymphocytes and macrophages
spleen → filters the blood that flows through it
mucosa-associated lymphoid tissue (MALT) → collection of lymphatic system tissues located in the mucous membranes that line body passages open to the outside enviro.
Ex. tonsils, appendix, and Peyer’s Patches
B-cells (humoral immune response) overview
antibody proteins used to attack foreign invaders in body fluid, removing them from it
located in secondary lymphatic tissues
millions of different B-cell b/c of different antigen receptors (born with)
T-cells (cell-mediated immune response) overview
cells (cytotoxic T-cells) used to attack foreign invaders located in body cells; kill body cells infected with pathogens
located in secondary lymphatic tissues
2 types cytotoxic T-cell and helper T-cells
antigen receptor vs. antibody
An antigen receptor is the same as an antibody except that the antigen receptor is bound in the membrane of a B or T cell while an antibody is free floating.
Antibodies and Antigen receptors have Antigen-binding sites that match specific epitopes.
Epitope
Regions of an antigen with a specific shape.
Associated with antibodies’ antigen receptor
B cell clonal selection (diagram)
Many B-cells with different antigen receptors are waiting in a secondary lymphoid organ/tissue. | ||||
⬇ | ||||
Antigen binds to a B-cell that has corresponding antigen receptors. | ||||
⬇ | ||||
Once the B-cell receives signaling molecules for a helper T-cell the B-cell becomes activated (it makes identical cells specialized against the antigen that triggered the response) | ||||
↙ ↘ | ||||
Some B-Cells differentiate into memory cells, which remain in the lymph nodes. | Some B-Cells differentiate into effector cells/plasma cells that secrete antibodies into the blood and lymph. | |||
⬇ | ⬇ | |||
Wait to help activate the immune system upon subsequent infection. | Effector cells have extra RER so they can make more antibodies (secretory proteins) which bind with the antigen. | |||
⬇ | ||||
Antigens bound by antibodies are marked for destruction (Phagocytosis) by macrophages. | ||||
Cell Differentiation
Memory Cells vs. Effector Cells
Memory Cells:
Help activate the immune system upon subsequent infections
Last for decades
Effector Cells:
Are highly effective at combating an existing infection.
Last for only 4 or 5 days before dying off
Antibodies
Structure:
Y-shaped proteins made of multiple polypeptides
protein is stablized by disulfide bridges (covalent bonds)
Heavy chain → Interior polypeptide chains
Light chain → Exterior polypeptide chains
Disulfide Bridges
Stabilized by disulfide bridges
Covalent bonds -> Stronger than IMF’s
Cannot be denatured -> can go to many parts of the body with different environments
Variable Region → Is specific for antigen binding (bind to epitopes)
Constant Region → Shared by all antibodies
Function:
Antibody binds to an antigen and inactivates the antigen by:
Neutralization (blocks viral binding sites; coats bacteria)
Agglutination (clumps viruses and cells together)
Precipitation (clumps of soluble antigens come out of solution)
Activation of complement proteins (free floating complement proteins are activated and form membrane complexes)
Neutralization, Agglutination, and Precipitation enhance…
Phagocytosis (foreign particles and cells are engulfed and digested)
Activation of complement proteins → Cell lysis (rupture of invading cell) aka. cell dies
T cells (types)
Helper T-cells
Activate the humoral response by activating B-cells.
Activate cytotoxic T-cells
Cytotoxic T-cells
Kill infected body cells
Anitgen Presenting Cells (APCs)
can be macrophages or b-cells
located in Interstitial Space and secondary lymphoid organs/tissues.
Where are the Helper T-cells located in secondary lymphoid organs/tissues when contacted by apc
What happens that causes cells to present antigens to the helper T-cell?
An APC ingests a microbe through a vacuole.
The storage vacuole combines with a lysosome.
The microbe is broken down into its antigens (nonself molecule)
The nonself molecule is combined with a self protein (which the APC makes) to form a Self-nonself complex.
The Helper T-cell with that specific antigen receptor identifies the antigen and binds to it.
The APC finally sends signaling molecules to activate the Helper T-cell.
so helper T needs signaling proteins and antigen thru self non self complex
Activated Helper T-cell
The activated Helper T-cell releases signaling molecules that do three things:
Stimulate helper T-cell division (memory helper T-cells and effector helper T-cells)
Activate B-cells (begins Humoral immune response)
Activates cell-mediated immune response (clonal selection: memory cytotoxic T-cells and effector cytotoxic T-cells)
Cytotoxic T-cells
Kill infected cells
Bind to an infected cell
Perforin molecules make holes in membrane
Enzymes that promote apoptosis (programmed cell death) enter
Infected cell is lysed (destroyed)