Ch. 27: Glomerular Filtration, Renal blood flow, and their control
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
What is the hallmark value (volume) of
Renal Plasma Flow (RPF)
Glomerular Filtration Rate (GFR)
Reabsorption (REAB)
Urinary excretion
625 ml/min
125 ml/min (125 mL/min = 180 L/day)
124 ml/min
1 ml/min
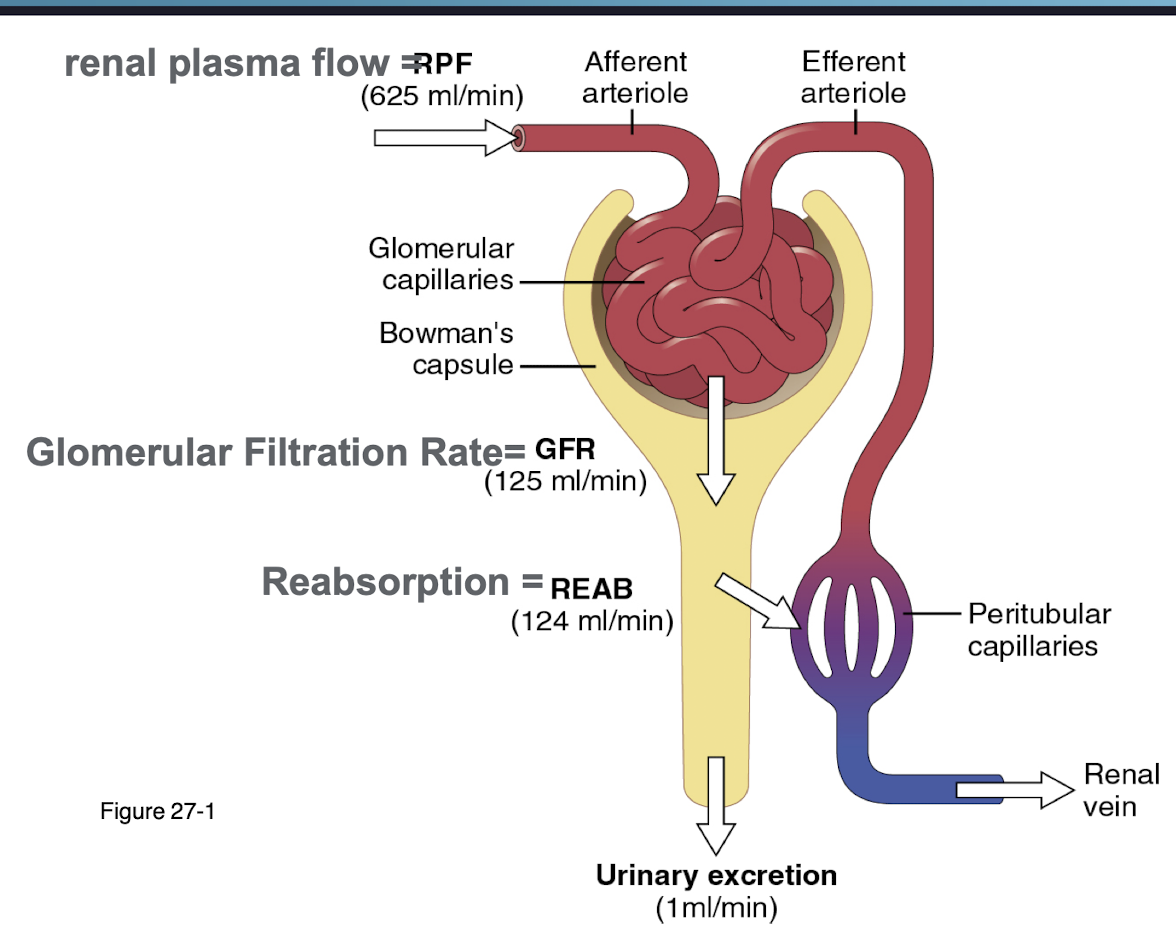
What is filtration fraction defined as?
What is the value?
the proportion of renal plasma flow (RPF) that is filtered into the Bowman's capsule by the glomerulus
20% of plasma is filtered
The endothelial layer of the glomerulus is made up of ______ and ______.
Define each as well.
a. lamina densa and glycocalyx
b. glycocalyx and fenstrated endothelial cells
c. podocytes and glycocalyx
d. endothelial cells and podocytes
b. glycocalyx and fenstrated endothelial cells
glycocalyx is a negatively charged gel that coats the endothelium cells
repels negative charged ions/things in teh blood to avoid them getting stuck (ex: albumin)
fenstarted endothelial cells make up the blood vessels in the glomerulus
the _____ provides a scaffold that supports the physiological function of the glomerular endothelium and podocytes.
glomerular basement membrane
under normal conditions does not constitute a major charge barrier but is still generally negatively charged
Which part of the glomerulus decides how much fluid can enter the glomerular barrier?
a. glomerular basement membrane
b. podocytes
c. glycocalyx
a. glomerular basement membrane
Podocytes regulate glomerular endothelial cell growth, survivial, differentiation and permeability by releasing the essential paracrine cytokine known as ______.
They line the nephron acting as a net to catch _______.
vascular endothelial growth factor A (VEGFA) - responsible for new blood vessel formation
smaller misses such as proteins
Which of the following will be repelled versus filtered through the glyococalyx?
a. Magnesium
b. Calcium
c. Potassium
d. hydrogen ions
e. plasma proteins
e. plasma proteins
the glycocalyx is negatively charged and the proteins are too - they will repel each other
most minerals are positively charged and will get filtered
T/F: Size matters in filtration of the glycocalyx
true
negative charge + small molecule = filtered through
negative charge + large molecule = not filtered through
Clinial: Renal disease can be silent, what are some early detection signs in at-risk patients?
hypertension - sheer stress will increase pressure of filtration breaking the filter or damaging the barrier
diabetes: diabetic neuropathy - sheer stress and oxidative pressure
pregnancy: gestational proteinuric hypertension (preclampsia)
in preclampsia, the blood vessels are not growing properly/damaged, increasing BP
if a signal is sent to the placenta, it inactivates VEGFA, stopping endothelial production and leading to inadequate blood flow and nutrient delivery to the fetus.
What is microalbuminuria?
What are the causes?
How are diabetic patient’s related?
urine excretion of 30 to 150 mg of albumin a day
early diabetes, hypertension, glomerular hyperfiltration
diabetic patients with microalbuminuria are 10-20 fold more likely to develop persistent proteinuria
what is Rhabdomyolysis?
Breakdown of muscle tissue (myoglobin) that is released into the blood, reaching the kidneys and filtered by the glomerulus, causing kidney disease
myoglobin should remain in the muscles but excessive myoglobin can lead to acute kidney injury. It can result from intense exercise, trauma, or certain medications.
Fe(2+) from myoglobin will produce overwhelming superoxide dismutase activity (antioxidate) damaging reaction oxygen species (ROS)
free radicals will damage the cells in the proximal tubules responsible for reabsorption = kills cells by damaging the DNA and mitochondria
How will rhabdomyolysis effect the…
proximal convoluted tubule
distal convoluted tubule
urine output
free radicals will damage the cells in the proximal tubules responsible for reabsorption = kills cells by damaging the DNA and mitochondria
forms obstructive casts
decreases output causing decrease in K+ excretion effecting water, pH and sodium balances = pressure on vascular system)
Which direction will pressure increase due to obstruction from Rhabdomyolysis?
Toward the glomerulus
What is the formula for glomerular filtration rate?
GFR = NFP x Kf
normal values of GFR are 125 ml/min
N = glomerular hydrostatic pressure (GHP)
F = bowman capsule pressure (BCP)
P = glomerular colloid pressure (GCP)
Kf = filtration coefficient
If we have an increase in glomerular hydrostatic pressure (GHP) what can we expect about the rate of GFR?
What if GHP decreases?
increase in GHP will occur at the efferent arteriole and increase GFR because the increase in pressure increases the rate of plasma flow
decrease in GHP will occur at the afferent arteriole and decrease GFR
Define
glomerular hydrostatic pressure (GHP)
glomerular colloid osmotic pressure (GOP)
Bowman’s capsule pressure (BCP)
GHP - pressure by the blood pushing on the walls (pushes towards the bowman’s capsule)
GOP - draw in of liquid due to the blood being full of proteins (pushes towards the bowman’s capsule)
BCP - pressure caused by fluid entering the capsule and backed up due to bottlenecking of volume size (pushes towards the arterioles)
Which aspect of the GFR equation (GFR = NFR x Kf) is constant?
Kf
What are some diseases that reduce Kf and GFR?
chronic hyptertension
obesity/diabetes mellitus
glomerulonephritis
Describe how hypertension is related to GFR
thickening and narrowing of the renal artery will reduce blood flow
improper perfusion of kidneys occurs
kidney ischemia
inflammation of renal tissue
glomerulosclerosis
reduced glomerular filtration rate
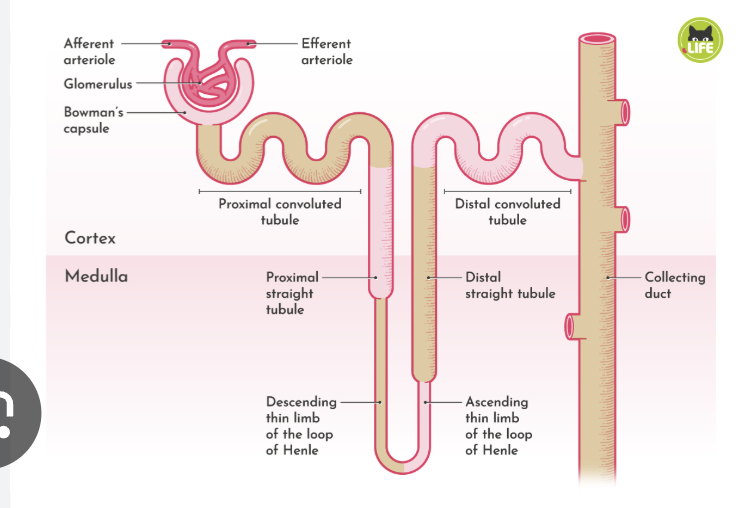
The Bowman’s Capsule Hydrostatic pressure normally changes based on ______.
What are some clinical diagnoses that can affect BCP?
Changes based on function of GFR
Tubular obstruction, kidney stones, and tubular necrosis will cause a block in the collecting duct and decrease net filtration and increase BCP. This will effect how much we absorb and filtration rate
Define oncotic pressure
amount of protein relative to plasma - opposes filtration in the kidneys
osmotic force from plasma proteins that pulls water back into the glomerular capillaries, opposing filtration.
What are the factors influencing glomerular capillary oncotic pressure (pi G)? (2)
Increase in arterial plasma oncotic pressure (pi A) and filtration fraction (FF) both INCREASE the glomerular capillary oncotic pressure (pi G), promoting fluid reabsorption back into the capillaries.
_______ is the determinant of GFR most subject to physiological control
a. glomerular hydrostatic pressure (PG or GHP)
b. arterial plasma oncotic pressure (pi A)
c. filtration fraction (FF)
d. coefficient of filtration (Kf)
a. glomerular hydrostatic pressure (PG or GHP)
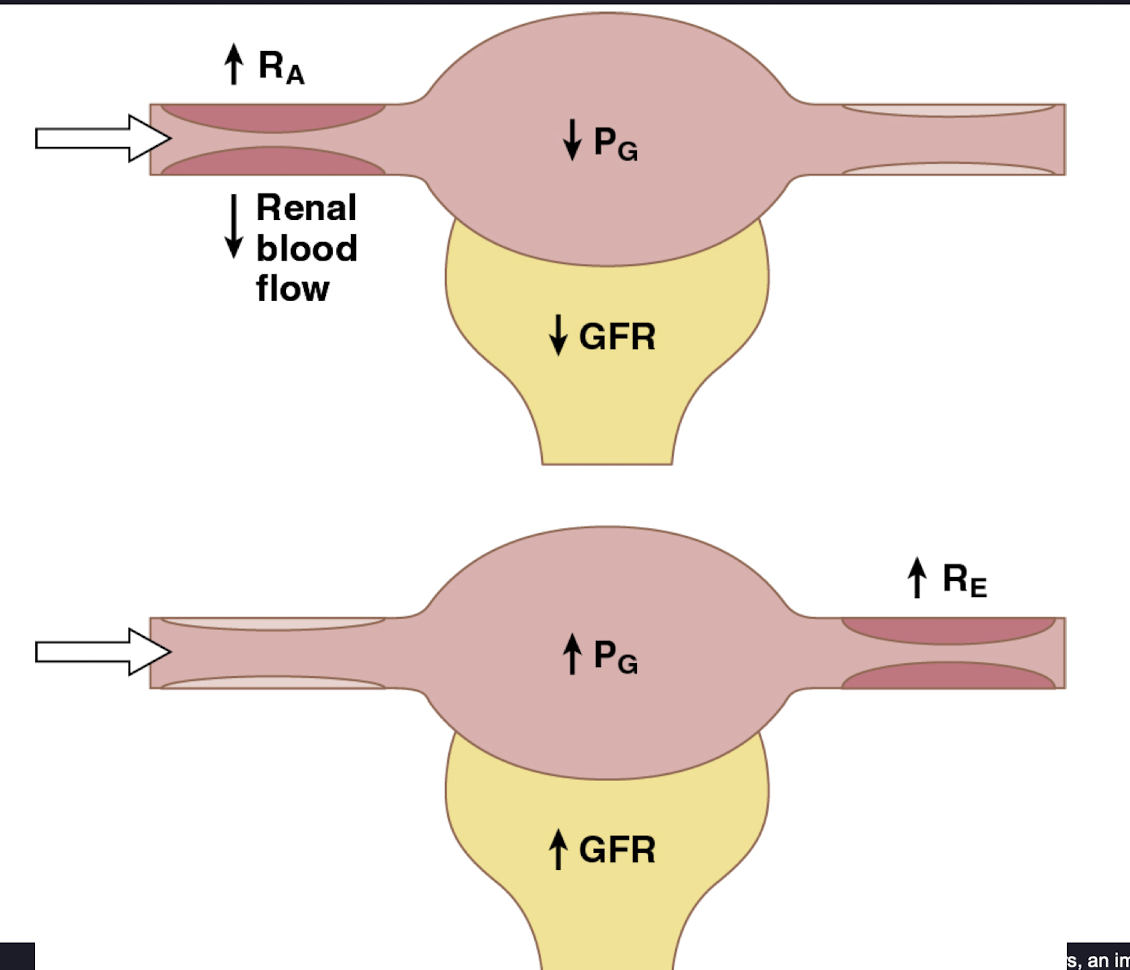
What are 3 factors that influence PG/GHP?
arterial pressure
afferent arteriolar resistence
efferent arteriolar resistence
what can we expect to see of the rate of renal blood flow if the afferent arteriole is constricted versus efferent arteriole? How do they effect GFR?
constricted afferent arteriole will decrease renal blood flow because it increases resistance to blood entering the glomerulus and therefore decreasing GFR
constricted efferent arteriole will decrease renal blood flow because it increases resistance to blood exiting the glomerulus, which can initially increase GFR (and GHP).
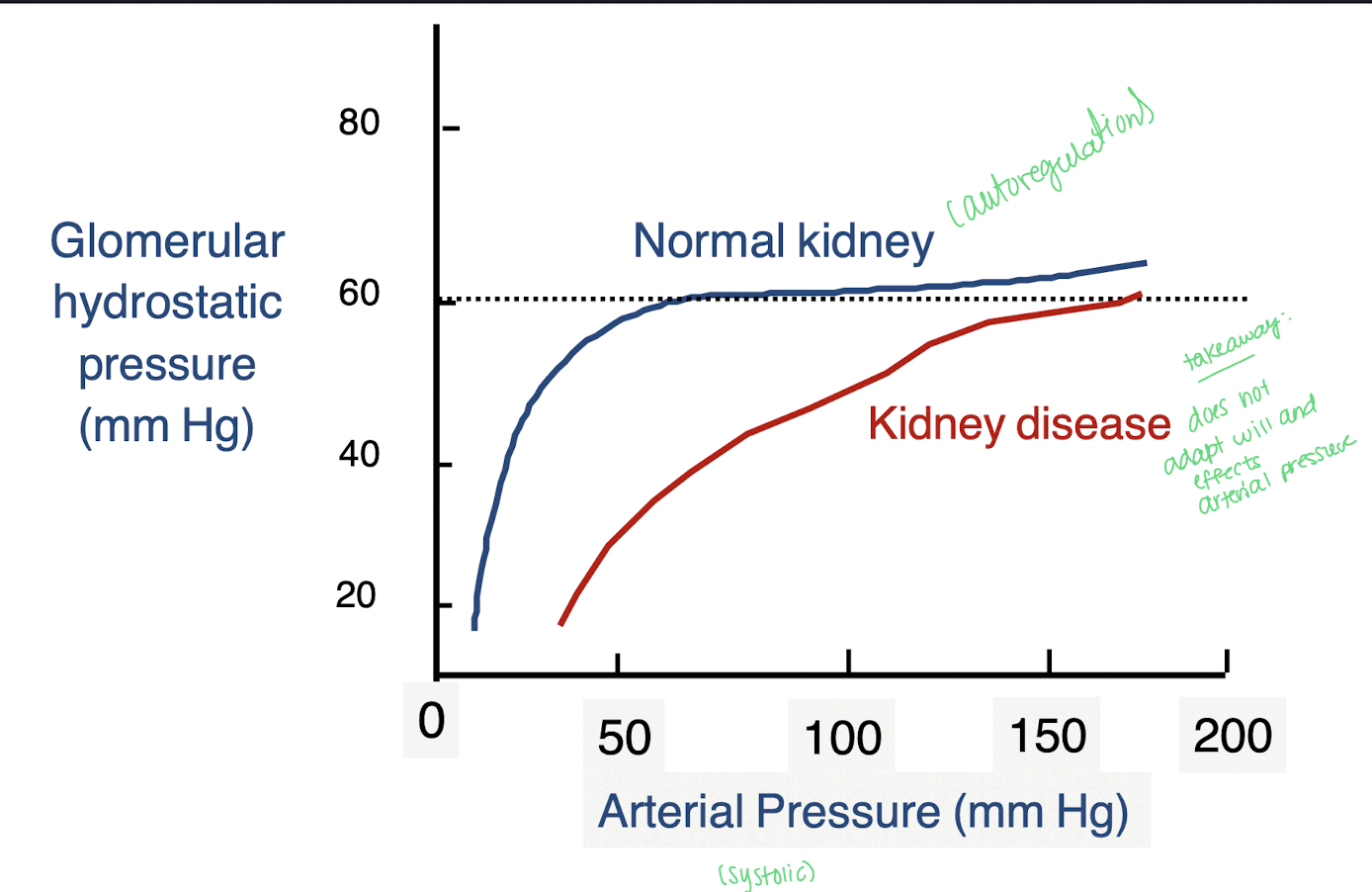
Explain autoregulation of GHP with a normal kidney versus kidney disease
In a normal kidney, as arterial pressure (systolic) rises, GHP will rise due to increased glomerular perfusion; however, in kidney disease, this autoregulatory mechanism may be impaired, leading to a reduced ability to maintain stable GHP despite fluctuations in arterial pressure.
autoregulation protects nephrons and ensures steady urine output
Why do we see that when renal blood flow increases, GFR will remain the same?
GFR is tightly regulated due to mechanisms like autoregulation, which allows the kidney to maintain constant filtration rates despite changes in blood flow.
GHP - [BCP - GOP]
What happens to GFR with an increase in Kf?
What happens to GFR with an increase in PB (pressure in Bowman’s capsule)?
GFR increases
GFR decreases
PB is when pressure caused by fluid entering the capsule will bottleneck; opposes the filtration pressure driving fluid out of the glomerular caps
GHP - [BCP - GOP]
What happens to GFR with an increase in Pi G (GOP)?
What happens to GFR when both Pi A (arterial pressure) and Pi G increase?
What happens to GFR when filtration fraction increases?
GFR decreases
GFR decreases
GFR increases when the filtration fraction increases, as more fluid is filtered from the blood into the nephron, enhancing overall filtration.
GHP - [BCP - GOP]
What happens to GFR when PG (GHP) increases?
What happens to GFR when RA increases and PG decreases?
What happens to GFR when RE increases and PG decreases?
increases
GFR decreases
GFR decreases
Why is high renal blood flow needed for high GFR?
High renal blood flow is essential for maintaining a high glomerular filtration rate (GFR) because it ensures adequate pressure in the glomeruli to facilitate the filtration of blood.
A large fraction of renal oxygen consumption is related to renal _______
tubular sodium reabsorption
Water follows Na+ as it enters with the Na+/K+ pump
What are two ways we can control GFR and Renal blood flow?
neurohumoral
local (intrinsic)
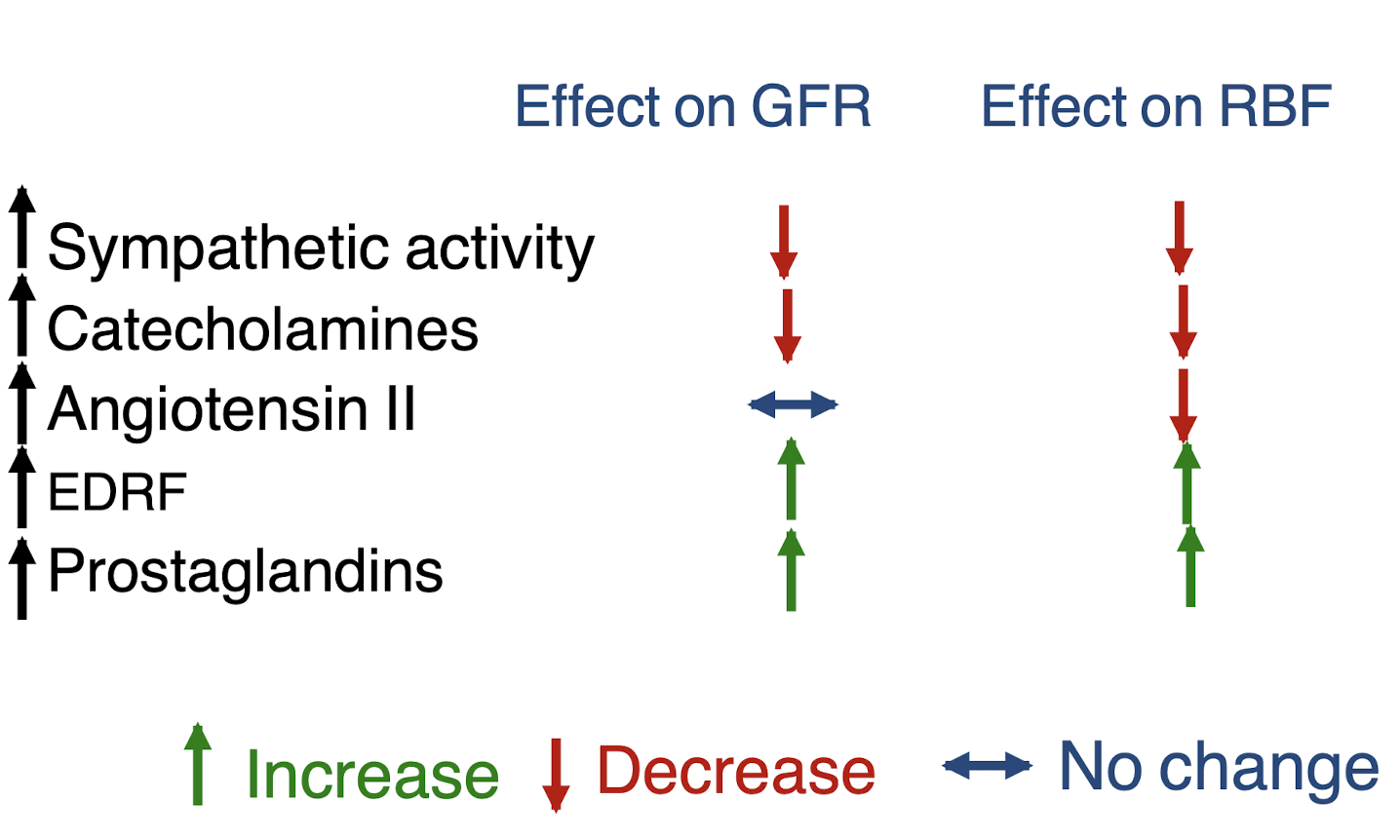
Control of GFR and renal blood flow:
explain how sympathetics/catecholamines have an effect - use the example of severe hemorraging
We will see an increase in RA (afferent arteriole) and an increase in RE (constriction on both sides). This is decrease GFR and renal blood flow
RBF will decrease because blood will be shunted to the brain and heart for survival
GFR decreases because of loss of blood
Control of GFR and renal blood flow:
What can we see when Angiotensin II acts on the glomerulus arteriole such as in a low sodium diet or volume depletion ?
Angiotensin II only acts on efferent arteriole, closing it off. This will prevent a decrease in GFR because of an autoregulation raising GHP and offsets by decreasing renal blood flow
think of an equation: Decrease in RBF + increase in RE = neutral GFR
Control of GFR and renal blood flow:
What effects do Prostoglandins have on GFR and RBF. Such will occur with use of NSAIDS in a volume depleted pt or patient with heart failure, or cirrhosis
Prostaglandins (which are paracrines) will vasodilate the afferent arteriole. Therefore a decrease in the pressure in the afferent arteriole and stable pressure in the efferent arteriole will cause in increase in GFR and RBF.
NSAIDS inhibit prostaglandins not allowing for vasodilation
Control of GFR and renal blood flow:
What effect do Endothelial derived nitric oxide (EDRF) have on GFR and RBF such as in the occurrence of inhibiting extreme vasoconstriction?
Pressure in the afferent and efferent arteriole will decrease causing an increase in both GFR and RBF because EDRF or NO is a vasodilator.
Summary slide for neurohormonal control of GFR and RBF
What are the 3 methods of LOCAL control of GFR and RBF?
Occurs through autoregulation with:
Myogenic mechanism - muscle origin
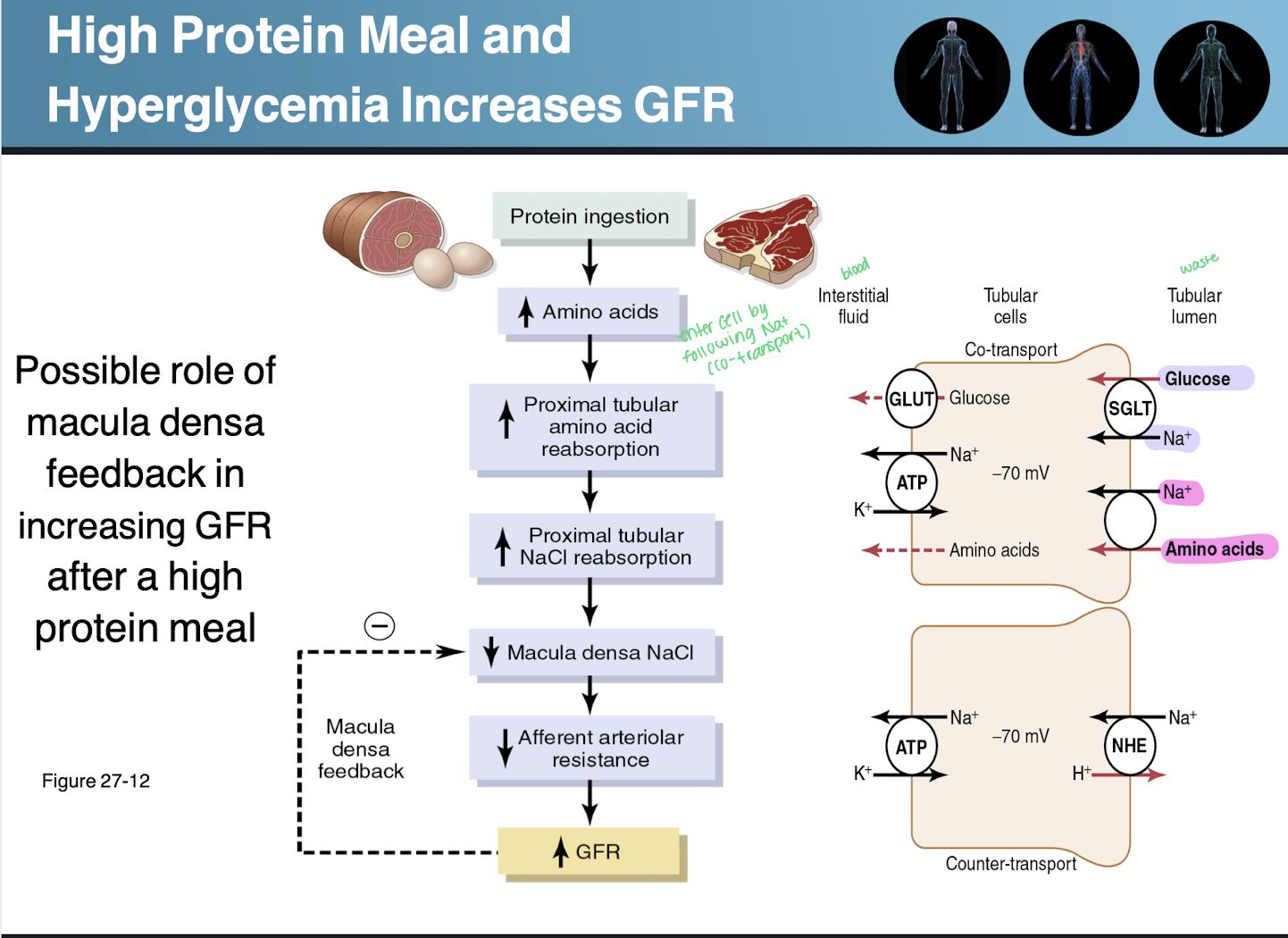
macula densa feedback - tubuloglomerular feedback occuring at the distal convoluted tubule
Angiotensin II - contributes to GFR but not RBF regulation
Angiotensin effects _______ but not _______
effects GFR
but not RBF regulation
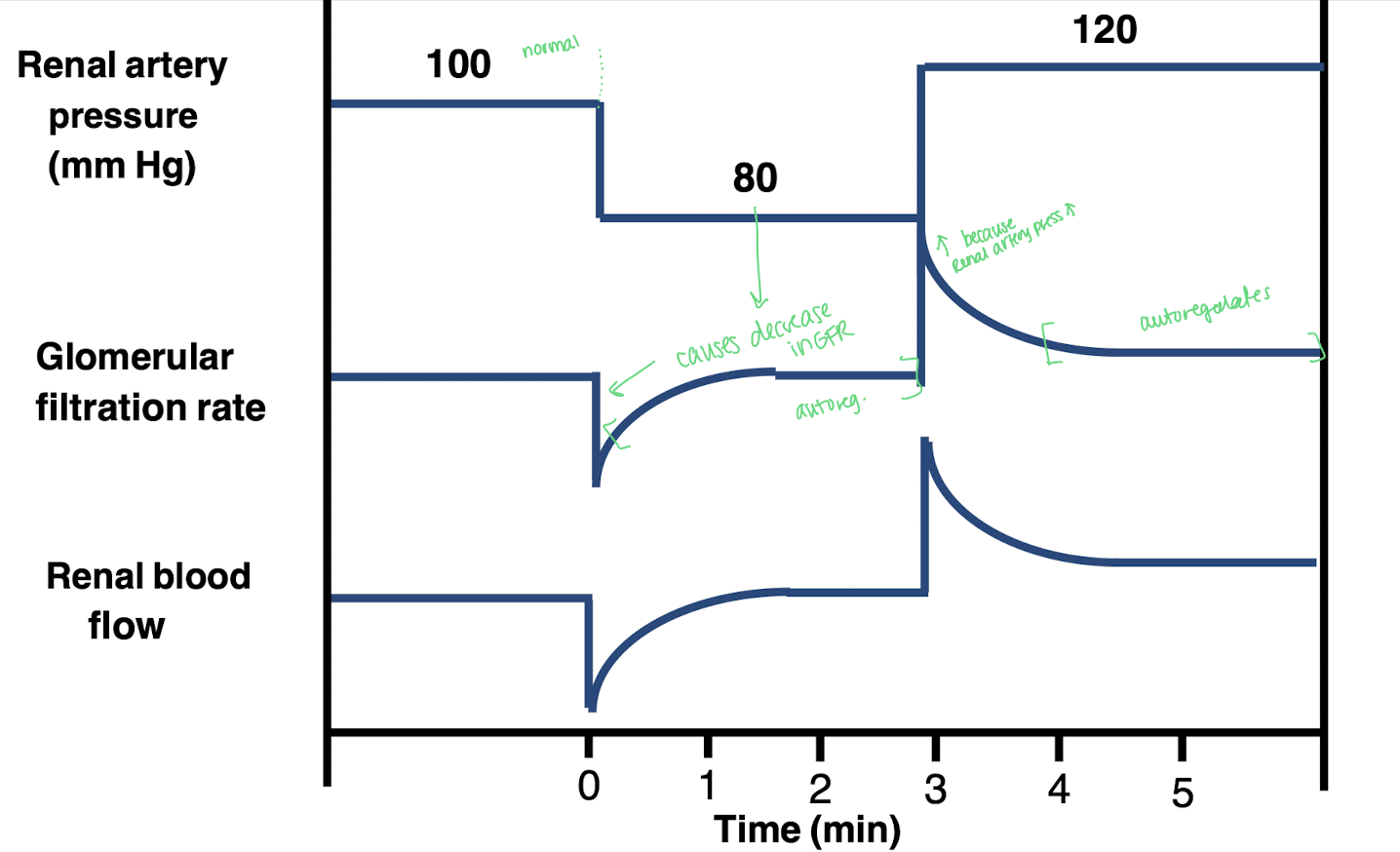
Explain the mechanism of renal regulation with renal artery pressure, GFR, and RBF
All pressure values will begin at normal. As renal artery pressure decreases from 100 mmHg to <80 mmHg, it will cause a decrease in GFR because the renal artery pressure is the driving force for blood to enter the glomerulus and without it = less filtration and less GFR. This will decrease RBF too.
Autoregulation will kick in and GFR will move to 80 mmHg and RBF will stabilize. This mechanism involves the myogenic response and feedback from the macula densa.
GFR will then increase because the renal artery pressure will increase but once it becomes too high autoregulation will occur again bringing the level back to ideal range.
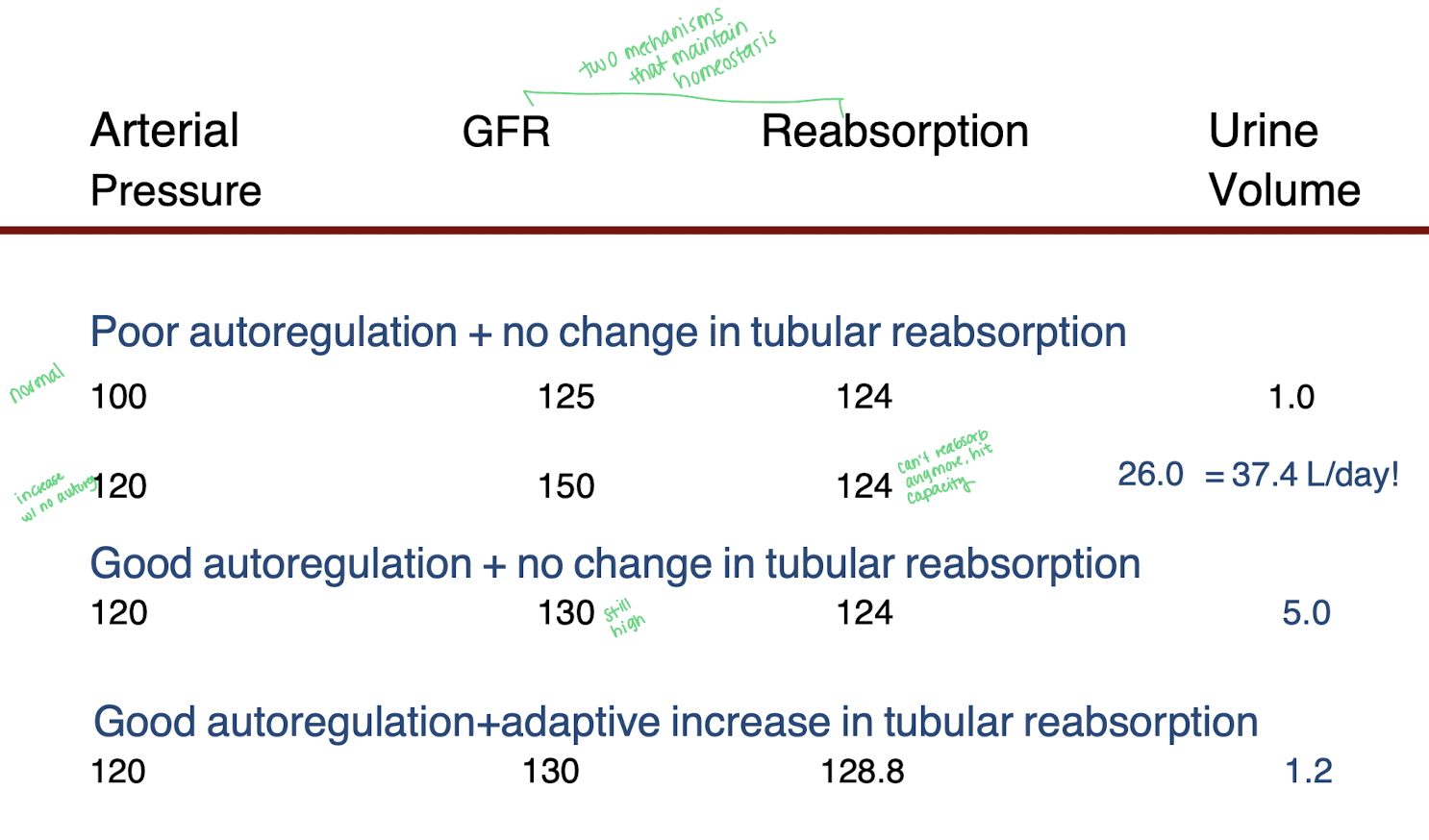
What are two mechanisms in autoregulation that maintain homeostasis?
GFR and reabsorption
Explain why in the chart provided why when GFR increases from 125 to 150, the reabsorption rate remains the same at 124. How does that effect urine volume?
Arterial pressure increased from 100 to 120 so the GFR will increase from 125 to 150. The reabsorption rate remains the same because the nephron's ability to reabsorb substances is maximal, leading to a constant reabsorption rate of 124.
This results in an increase in urine volume as the excess filtrate that is not reabsorbed is excreted.
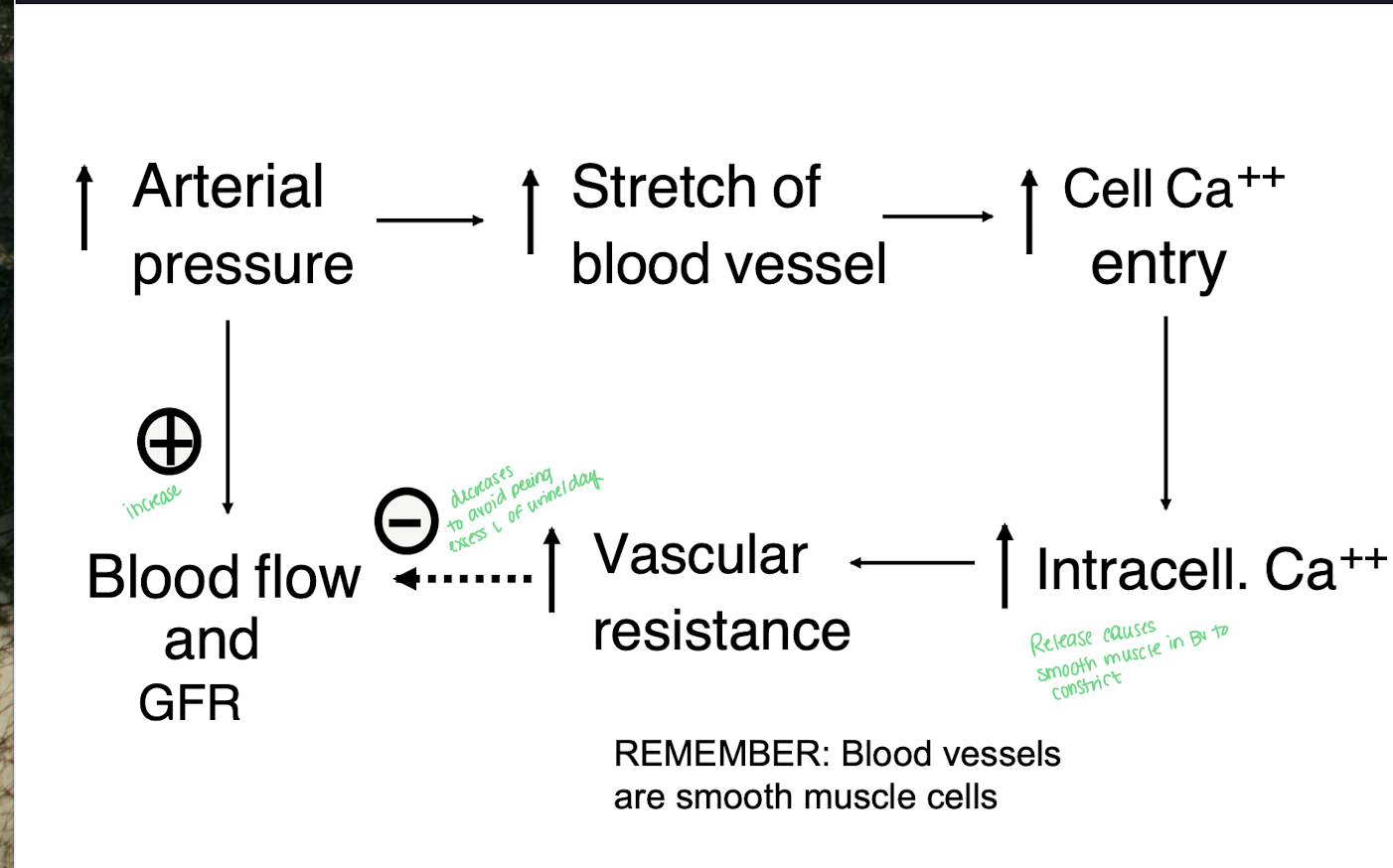
Explain the myogenic mechanism for local control of GFR and RBF
increase in arterial pressure will increase stretch of blood vessels (smooth muscle)
Ca+ cells will enter and the intracellular Ca+ level will increase leading to constriction of blood vessels
This will increase vascular resistence
decreases renal blood flow and GFR
Increase in the arterial pressure will directly cause an increase in renal blood flow and GFR (going back to #1)
Describe macula densa cells
located in the distal nephron within the juxtaglomerular complex
sense salt and flow through the distal convoluted tubule that come in contact with the afferent and efferent arterioles
They regulate glomerular filtration rate by signaling changes in sodium concentration and flow, influencing renal blood flow.
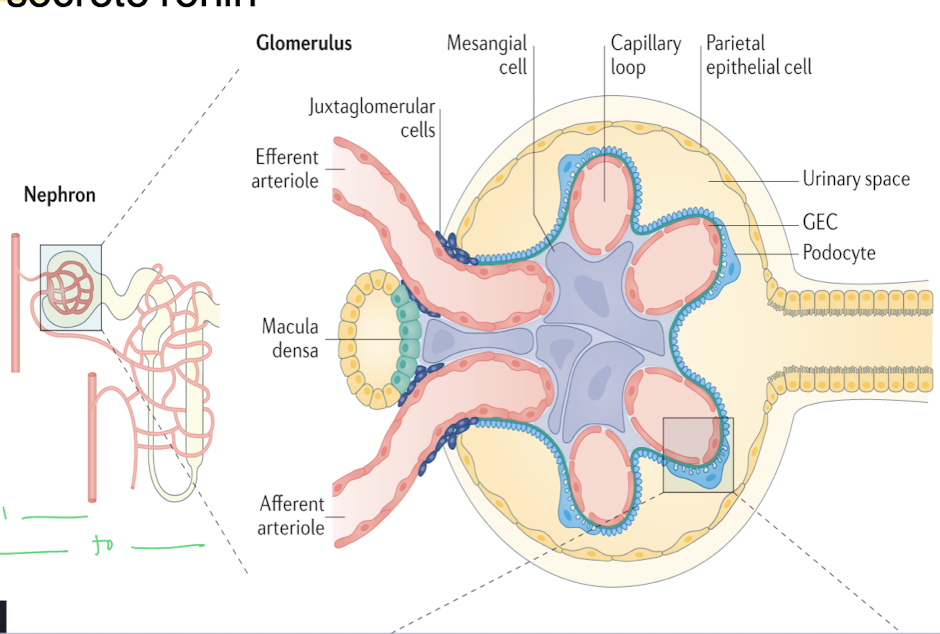
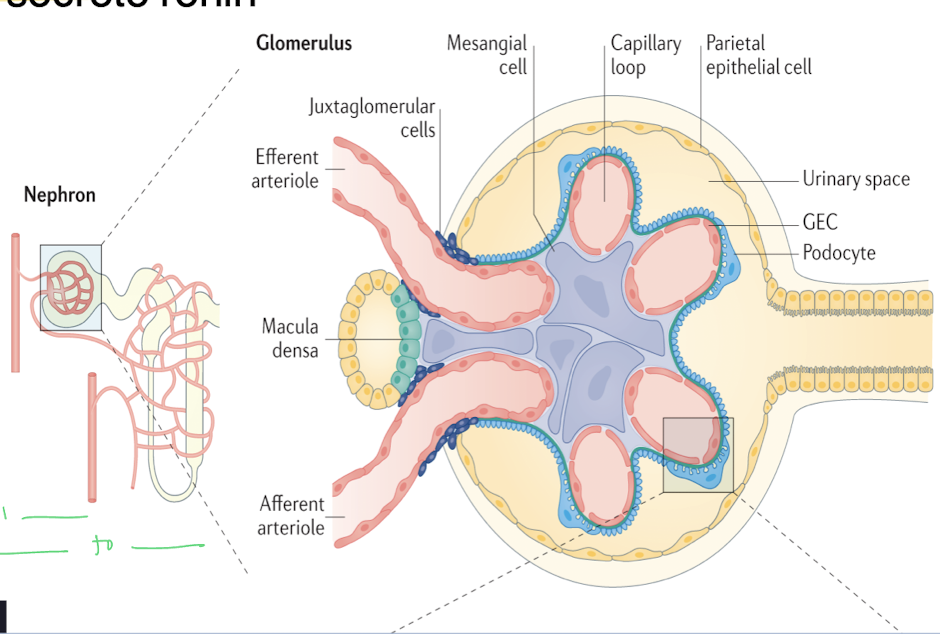
Juxtaglomerular cells secrete ______
a. podocytes
b. renin
c. albumin proteins
d. NaCl
b. renin - activates RAAS pathway to regulate blood pressure and fluid balance.
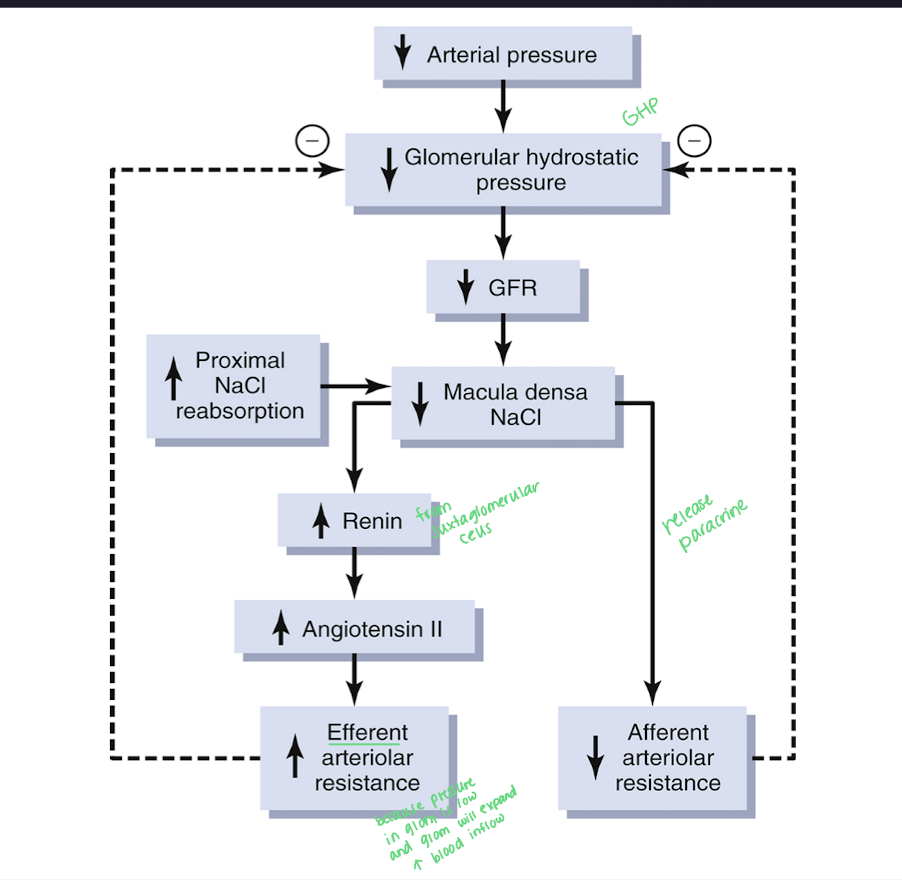
Explain the macula densa feedback with helps with local control of GFR and RBF
Begins with a decrease in GFR
Decrease in distal NaCl delivery
Decrease in macula densa NaCl reabsorption causing the feedback to occur
the decrease in afferent arteriolar resistance and activation of the macula densa will have the afferent arterioles dilate
causing an increase in GFR
Explain how GFR can be regulated by Angiotensin II
stimulus is the decrease in GFR
sensed by the macula densa cells with a decrease in NaCl
causes the increase release of renin and Angio II
Angio II can directly increase blood pressure
Angio II will constrict the efferent arteriolar arteries, increasing resistence
both will then increase GFR
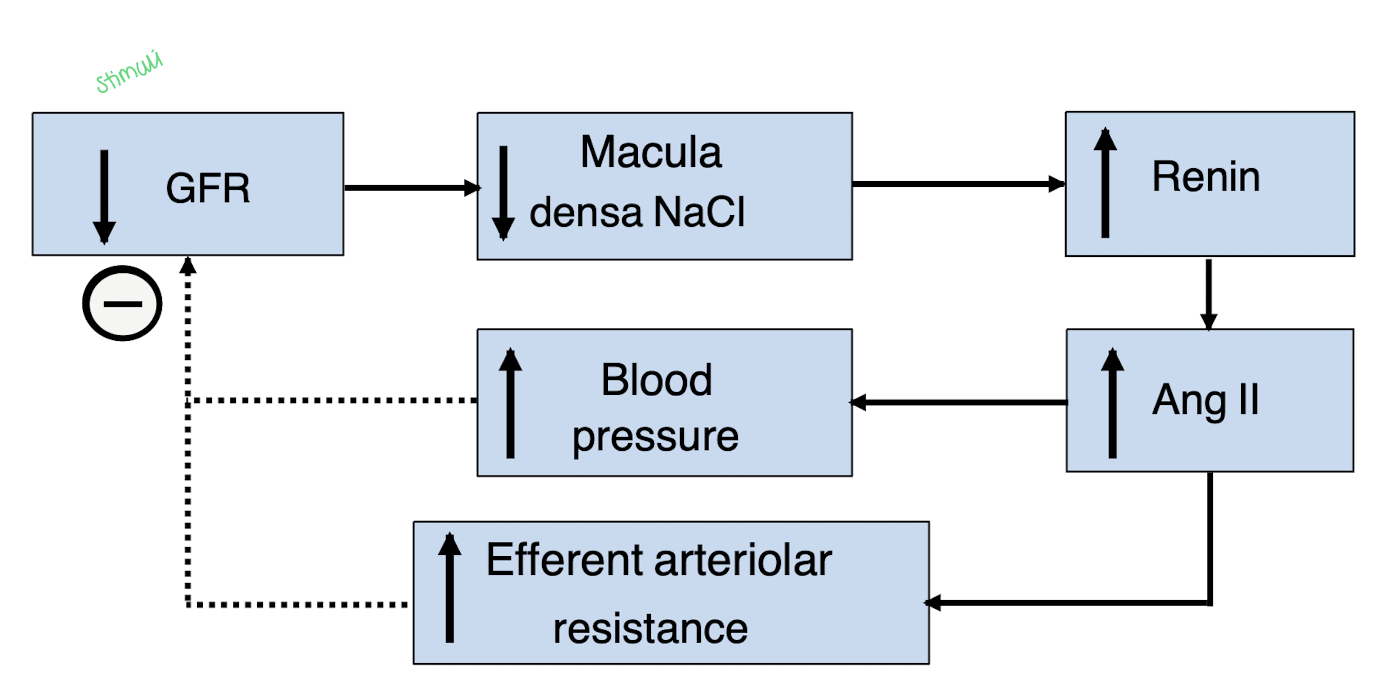
Give an overview of the Macula densa feedback mechanism for GFR regulation (include renin and angiogensin II)
What other factors can influence GFR?
aging - decrease GFR 10% a decade after 40 y/o
hyperglycemia - increases GFR (DM) due to increase in the Kf because of damage to the glycocalyx
dietary protein - high protein increases GFR and low protein decreases GFR