UKMLA: Geriatrics
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
Alzheimer’s Disease: What is the pathophysiology?
Accumulation of tau tangles and amyloid plaques
Alzheimer’s Disease: What are the risk factors?
Over 65 y/o (most significant factor is age!!)
Apolipoprotein E (APOE) gene mutation
Down syndrome
FH
Smoking, bad diet, physical inactivity
Traumatic brain injury
Low educational attainment
Alzheimer’s Disease: What are the symptoms?
Poor memory
Language impairment
Poor ability to plan or organise tasks
Aggressive behaviour
Hallucinations
Delusions
Paranoia
Unable to recognise places or people
Loss of motor skills
Alzheimer’s Disease: What is the management?
Donepazil OR galantamine (cholinesterase inhibitor)
Memantine (NMDA receptor antagonist)
Low dose rsiperidone for behaviour and psychological symptoms of dementia
Parkinson’s Disease: What presentation is contraindicated with the use of donepazil?
Bradycardia
Constipation: What is the Rome IV criteria?
Fewer than three bowel movements per week
Hard stool in more than 25% of bowel movements
Tenesmus (sense of incomplete evacuation) in more than 25% of bowel movements
Excessive straining in more than 25% of bowel movements
A need for manual evacuation of bowel movements
Constipation: What are the risk factors?
Old age
Poor nutrition e.g. low fibre
Inactive
Medications e.g. CCB
Female
Constipation: What are the symptoms?
Less than 3 bowel movements a week
Tenesmus
Straining
Distended abdomen
Abdominal mass in left/right lower quadrants (stool)
Rectal bleeding
Haemorrhoids
Fissures
Confusion
Constipation: What are the investigations?
Faecal immunochemical test (FIT)→ detects hidden blood in stools to check for malignancy
Constipation: Under what circumstances is a constipated patient referred for cancer investigation?
Constipation with weight loss
60 y/o or older
Constipation: What is the management?
Laxatives:
Ispaghula husk → increase stool bulk
Senna → short-term relief
Lactulose→ treats constipation in patients with hepatic encephalopathy
Enema→ rapid evacuation pre-procedure or examination
Sodium docusate/macrogol→ treats constipation in patients with anal fissures (stool softener)
Constipation: What are the different MOA for laxatives?
‘BOSS’ mneumonic:
Bulk-forming→ e.g. isphagul husk
Osmotic → e.g. lactulose
Stimulating→ e.g. senna
Softening→ docusate sodium
Haemorrhagic Stroke: What is the pathophysiology?
Bleeding in the brain parenchyma, ventricles or subarachnoid space → raised ICP
Haemorrhagic Stroke: What are the risk factors?
Old age
Male
FH
Haemophilia
HTN
Cocaine use
Haemorrhagic Stroke: What are the symptoms?
Severe headache
Altered conscious (drowsy to coma)
Vomiting
Weakness
Visual loss
Seizures
HTN
Haemorrhagic Stroke: What are the investigations?
Blood glucose
Blood pressure
ECG
CT head is key investigation
Haemorrhagic Stroke:
Refer to neurosurgery
Reverse coagulation treatments
IV GTN or labetalol for HTN
Ensure patient is NBM
Ischaemic Stroke: What is the pathophysiology?
Ischaemic strokes occur due to occlusion or stenosis of the vessels supplying the central nervous system, causing infarction of tissues
Ischaemic Stroke: What is the Bamford classification criteria for a Total Anterior Circulation Stroke?
All 3 of the following:
Unilateral motor or sensory deficit (or both) affecting at least two of the face, arm and leg
Higher cerebral dysfunction (e.g. dysphagia, neglect, dyscalculia)
Homonymous hemianopia
Ischaemic Stroke: What is the Bamford classification criteria for a Partial Anterior Circulation Stroke?
2 out of the following:
Unilateral motor or sensory deficit (or both) affecting at least two of the face, arm and leg
Higher cerebral dysfunction (e.g. dysphagia, neglect, dyscalculia)
Homonymous hemianopia
Ischaemic Stroke: What is the Bamford classification criteria for a Lacunar Stroke?
Pure motor stroke
Pure sensory stroke
Sensori-motor stroke
Ataxic hemiparesis
Dysarthria-clumsy hand syndrome
Ischaemic Stroke: What is the Bamford classification criteria for a Posterior Circulation Stroke?
Cerebellar dysfunction
Conjugate eye movement disorder
Bilateral motor and/or sensory deficit
Ipsilateral cranial nerve palsy with contralateral motor and/or sensory deficit
Isolated homonymous visual field defect
Ischaemic Stroke: What are the symptoms?
Cerebellar dysfunction
Conjugate eye movement disorder
Bilateral motor and/or sensory deficit
Ipsilateral cranial nerve palsy with contralateral motor and/or sensory deficit
Isolated homonymous visual field defect
Ischaemic Stroke: What are the investigations?
Bloods
Hb1Ac and blood glucose
Lipid profile
CT to rule out haemorrhage
Carotid Doppler to identify stenosis
Echo to identify embolism
Ischaemic Stroke: What is the management?
Refer to SALT for dysphasia
NG tube and feeding within 24 hours
Physiotherapy
Thrombolysis with alteplase within 4.5 hours onset
Aspirin 300mg → for 2 weeks!!
Switch to 75mg clopidofrel
Thromboectomy
Lewy-Body Dementia: What is the pathophysiology?
Deposits of alpha-synuclein protein that form Lewy bodies
Lewy-Body Dementia: What are the clinical features?
Changes in attention
Parkinsonism→ rigidity, bradykinesia, postural instability
Visual hallucinations
If cognitive impairement and Parkinsonism develops within one year of each other, it is likely LBD.
Lewy-Body Dementia: What are the investigations?
Dopamine transporter scan (DAT)
Electroencephaalography scan (EEG)
Lewy-Body Dementia: How common is it?
Alzheimer’s
Vascular dementia
Lewy-body dementia
Parkinson’s Disease: What are the clinical features?
Bradykinesia
Asymmetric 3-5Hz "pill-rolling" resting tremor
Rigidity
Gait→ small, shuffling steps
Constipation
Olfactory issues
Depression, anxiety and hallucinations
Parkinson’s Disease: What is the pathophysiology?
It is believed to result from the accumulation of "Lewy bodies", intracellular inclusions primarily composed of misfolded alpha synuclein.
These bodies form and lead to neuronal death in the dopaminergic cells of the substantia nigra of the basal ganglia, thereby causing the characteristic symptoms.
Parkinson’s Disease: What excludes a diagnosis?
An absolute failure to respond to 1-1.5g of levodopa daily almost excludes a diagnosis of idiopathic Parkinson's disease.
Parkinson’s Disease: What is the management?
Levodopa
Can combine with carbidopa
Dopamine agonists
Selegiline (MAO-B inhibitor)
Parkinson’s Disease: Levadopa can cause nausea. Which anti-emetic can be prescribed to manage this?
Domperidone
Parkinson’s Disease: What side effect is as associated with short-term use of levodopa?
Abnormal dreams
Parkinson’s Disease: What side effect is as associated with long-term use of levodopa?
End of dose deterioration (by the end of a dose, there is not enough levodopa and symptoms return)
Vascular Dementia: What is the cause?
Ischaemic or haemorrhagic stroke
Vascular Dementia: What are the risk factors?
HTN
Diabetes
Hyperlipidaemia
Smoking
AF
Vascular Dementia: What are the symptoms?
Visual disturbance
Sensory or motor issues
Poor attention and concentration
Seizures
Memory loss
Occurs over several months to years
Patient may have PMH of stroke
Vascular Dementia: What is frontotemporal dementia?
Prominent changes in personality and behavior or language difficulties with relative sparing of memory.
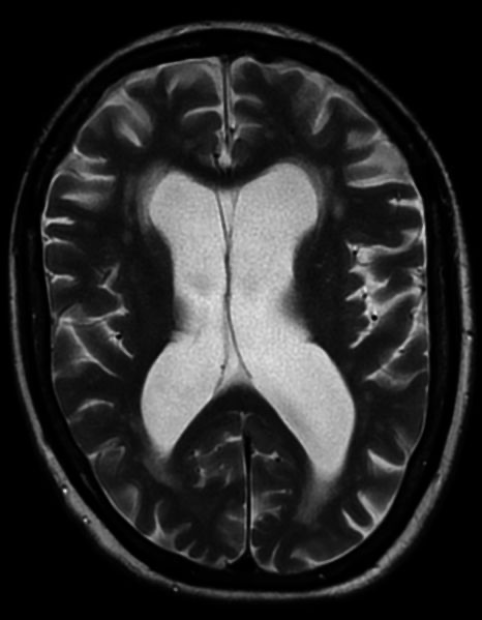
Vascular Dementia: What is the hallmark of diagnosis via MRI?
White matter and infarcts
Vascular Dementia: What is the management?
Address underlying risk factors/causes
Music/art therapy
Donepazil or memantine if they have Parkinson’s too or dementia with lewy bodies