Chapter 7 Skeletal System
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
List the general functions of bones
The functions of bone include support, movement, protection, blood cell production, and storage of minerals.
Skeletal system
Organ system consisting of bones, and the ligaments and cartilages that hold them together.
Name the living tissues found in bone
The living tissues found in bone include, bone tissue, blood, nerves, and cartilage, and other connective tissue.
Long bones
have long longitudinal axes and expanded ends. Examples of these bones are the forearm and the thigh bones.
Short bones
have equal lengths and widths. The bones of the wrists and ankles are this type. A special type of these bones is a sesamoid bone, or round bone. This type of bone is usually small and nodular and embedded in a tendon adjacent to a joint, where the tendon is compressed. The kneecap (patella) is a sesamoid bone.
Flat bones
are platelike structures with broad surfaces, such as the ribs, the scapulae, and some bones of the skull.
Irregular bones
have a variety of shapes, and most are connected to several other bones. These bones include the vertebrae that compose the backbone, and many facial bones.
Long bones consists of:
An epiphysis at either end of the long bone, which forms a joint with another bone.
The outer surface of the articulating portion is coated with a layer of hyaline cartilage called articular cartilage.
The shaft of the bone is called the diaphysis
Th metaphysics is the widening part of the bone between the diaphysis and the epiphysis
What is the purpose of the periosteum?
Encloses the bone in tough, vascular dense connective tissue, except for the articular cartilage on its ends. It firmly attaches to the bone, and the fibers are continuous with connected ligaments and tendons.
Helps form and repair bone tissue.
A bone’s ___ makes possible for its ____
Shape; functions
Processes
Bony projections that provide sites for attachment of ligaments and tendons; grooves and openings are passageways for blood vessels and nerves; and a depression of one bone might articulate with a process of another.
The wall of the diaphysis is mainly compose of tightly packed tissue called ___
Compact bone, also cortical bone.
It has a continuous extra cellular matrix with no gaps.
The epiphyses are largely composed of ___
Spongy bone, also called cancellous bone.
With thin layers of compact bone on their surfaces
Spongy bone consists of many branching bony plates called trabeculae that separates irregular spaces within spongy bone.
Compact bone in the diaphysis of a long bone forms a tube with a hollow chamber called the __
Medullary cavity that is continuous with the spaces of the spongy bone.
What is the endosteum
A thin membrane containing bone-forming cells that lines the medullary cavity as well as spaces within spongy bone.
A special type of tissue called __ fills that spongy bone spaces and the medullary cavity.
Marrow, a type of soft connective tissue.
In compact bone, the osteocytes and layers of extra cellular matrix called lamellar are concentrically clustered around a central canal (Haversian canal) forming a cylinder-shaped unit called an __
Osteon (Haversian system).
The osteons run longitudinally with the axis of the bone functioning as:
Weight-bearing pillars, resisting compression
Each central canal contains:
Blood vessels and nerves surrounded by loose connective tissue.
Blood in these vessels nourishes bone cells associated with the central canal via gap junctions between osteocytes.
Central canals extend longitudinally through bone tissue, and transverse perforating canals (Volkmann’s canals) connect the central canals.
Perforating canals contain:
Larger blood vessels and nerves by which the smaller blood vessels and nerve fibers in central canals communicate with the surface of the bone an medullary cavity.
Spongy bone, like compact bone, is composed of:
Osteocytes and extracellular matrix, but the bone cells do not aggregate around central canals
Instead, the cells lie in the trabeculae and get nutrients from substances diffusing into the canaliculi that lead to the surfaces of these thin, bony plates.
Discuss the major functions of bones.
Bones shape, support, and protect body structures, as well as aid body movements. They house tissue that produces blood cells, and store various inorganic salts.
What is Hematopoiesis?
The process of blood cell formation.
Begins in the yolk sac, which lies outside the embryo. Later in development, blood cells are manufactured in the liver and spleen, and still later, form in the bone marrow.
Red marrow
Blood-cell-forming tissue in spaces within the bones.
Contains hemoglobin (red color).
In adults, primarily found in the spongy bone of the skull, ribs, breastbone (sternum), collarbones (clavicles), backbones (vertebrae), and hip bones.
Yellow marrow
As a person ages, yellow marrow replaces red marrow.
Stores fat and does not produce blood cells.
If blood supply if deficient, yellow marrow may become red marrow.
Explain how a bone marrow transplant works.
A hollow needle and syringe remove normal red marrow cells from the spongy bone of a donor, or stem cells are separate out from the donor’s bloodstream.
Inorganic mineral salts account for about 70% of the extracellular matrix by weight and are mostly small crystals of a type of ___
Calcium phosphate called hydroxyapatite.
The human body requires calcium for a number of vital metabolic processes, including:
Muscle cell contraction
Nerve cell conduction
Blood clot formation
When blood is low on calcium:
The parathyroid hormone stimulates osteoclasts to break down tissue, releasing calcium salts from the extracellular matrix into the blood
When blood has a high amount of calcium:
Very high blood calcium inhibits osteoclast activity, and calcitonin, a hormone from the thyroid gland, stimulates osteoblasts to form bone tissue.
Bones tissue usually contains:
Calcium and phosphorus.
Small amounts of magnesium, sodium, potassium, and carbonate ions
Harmful metals (if ingested): lead, radium, and strontium.
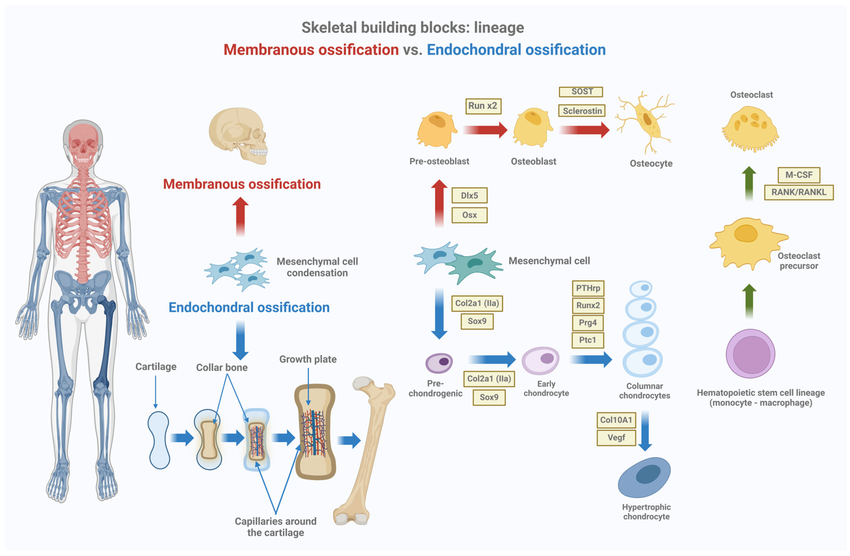
Bones that originate within sheet like layers of connective tissues are called:
Intramembranous bones
Bones that begin as masses of hyaline cartilage later replaced by bone tissue are called
Endochondral bones
Ossification
Formation of bone
Examples of intramembranous bones consists of:
Flat bones of the skull, clavicles, sternum, and some facial bones, including he mandible, maxillae, and zygomatic bones.
Osteoblast
Bone-forming cell
The process of replacing embryonic connective tissue to form an intramembranous bones is called:
Intramembranous ossification
Most of the bones of the skeleton are
Endochondral bones
The process of forming an endochondral bone by the replacement of hyaline cartilage is called:
Endochondral ossification
Primary ossification center
Bone tissue begins to replace hyaline cartilage int he center of the diaphysis.
Bone develops from it toward the ends of the cartilaginous structure.
Meanwhile, osteoblasts from the periosteum deposit compact bone around the primary ossification center.
Secondary ossification centers
Appear in the epiphyses, and spongy bone forms in all directions from them.
As the spongy bone is deposited in the diaphysis and in the epiphysis, a band of cartilage closed the epiphyseal plate remains between the two ossification centers.
Name and describe the four layers of the epiphyseal plate.
First layer: zone of resting cartilage, is closest to the end of the epiphysis. It is composed of resting cells that do not actively participate in growth
This layer anchors the epiphyseal plate to the bony tissue of the epiphysis.
Second layer: zone of proliferating cartilage, includes rows of many young cells undergoing mitosis. As new cells appear and as extracellular matrix forms around them, the cartilaginous plate thickens.
Third layer: zone of hypertrophic cartilage, rows of older cells, left behind when new cells appear form this layer, enlarging and thickening the epiphyseal plate still more.
Consequently, the entire bone lengthens
Fourth layer: zone of calcified cartilage, is thin. It is composed of dead cartilage cells and calcified extracellular matrix.
Osteaclasts
Break down the calcified matrix.
Secrete an acid that dissolves the inorganic component of the calcified matrix, and their lysosomal enzymes digest the organic components.
The bone in the central regions of the epiphyseal and the diaphysis remains __ , and hyaline cartilage on the ends of the epiphyses persists throughout life as __
Spongy; articular cartilage
Describe the development of an intramembranous bone
Intramembranous bones, such as the major skull bones, develop from thin layers of undifferentiated connective tissue in the fetus.
Partially differentiated progenitor cells develop into osteoblasts, cells which deposit bone matrix in their vicinity; the osteoblasts then produce spongy bone around themselves. Once an osteoblast is completely encased by matrix, it is called an osteocyte. The membranous tissue that remains on the outer portion of the bone develops into the periosteum. Just inside the periosteum, the osteoblasts deposit a layer pf compact bone over the spongy bone.
Explain how an endochondral bone develops.
Endochondral bones form from hyaline cartilage models in the fetus. After a period of growth in a long bone, for example, the cartilage starts to break down in the middle of the diaphysis.
Periosteum forms from tissue around the diaphysis. Blood vessels and osteoblasts of the periosteum enter the area of decomposing cartilage, and deposit spongy bone there. This is the primary ossification center. Later in development, secondary ossification centers form in the epiphyses, where spongy bone is produced. At the junctions between the diaphysis and the epiphyses, a band of active cartilage remains; this is the epiphyseal plate, which is the growth area for a growing long bone.
bone remodeling occurs throughout life as osteoclasts resorb bone tissue and osteoblasts replace the bone.
Opposing processes of resorption and deposition occur on the surfaces of the endosperm and periosteum.
Types of fractures:
Greenstick- incomplete fracture
Fissured- fracture is an incomplete longitudinal break
Comminuted- fracture is complete and fragments the bone.
Transverse- fracture is complete, and the break occurs at a right angle to the axis of the bone.
Oblique- fracture occurs at an angle other than a right angle to the axis of the bone.
Spiral- fracture caused by excessive twisting of the bone.
Factors that influence bone development, growth, and repair:
Nutrition, exposure to sunlight, hormonal secretions, and physical exercise, vitamin A (osteoblast and osteoclasts activity), C (collagen), D (dietary calcium)
Deficiency in vitamin D: rickets (children), osteomalacia (adults).
Too little growth hormone: pituitary dwarfism.
Too much growth hormone: pituitary gigantism.
Acromegaly: excess growth hormone in which hands, feet, and jaw enlarge.
About 90% of the protein that is part of the bone is collagen.
Sutúralo (wormian) bones
Extra bones that sometimes develop in sutures between the flat bones of the skull.
Axial skeleton
Consists of the bony and cartilaginous parts that support and protect the organs of the head, neck, and trunk. These parts include the following:
The skull (cranium and facial bones)
The middle ear bones (transfer sound vibrations to the hearing receptors)
The hyoid bone (located in the neck between the lower jaw and larynx).
The vertebral column (spinal column that consists of many vertebrae separated by cartilaginous intervertebral discs).
Thoracic cage (protects the organs of the thoracic cavity and the upper abdominal cavity).
Appendicular skeleton
Consists of the bones of the upper and lower limbs and the bones that anchor the limbs to the axial skeleton. It includes the following:
The pectoral girdle (formed by scapula and a clavicle).
Each upper limb consists of a: humerus, radius, and an ulna, and a hand.
Carpals, metacarpals, and phalanges
Pelvic girdle (formed by two hip bones attached to each other anteriores and to the sacrum posteriorly).
Each lower limb consists of a femur, or thigh bone; two leg bones— a large tibia, and a slender fibula, patella.
Tarsals, metatarsals, and phalanges.
Locate and name each of the bones of the cranium.
The frontal bone makes up the front part of the skull forehead), just above the eyes. The parietal bones make up the upper sides and roof of the cranium, in back of the frontal bone. The occipital bone makes up the back part of the skull and base of the cranium. The temporal bones make up the lower sides and part of the base of the cranium. The sphenoid bone extends all the way across the anterior part of the cranium; it makes up the sides and floors of the eye orbits, and a portion of the base of the cranium and sides of the skull. The ethmoid bone lies anterior to the sphenoid bone; it helps to form the nasal cavities, the eye orbits, and the nasal septum.
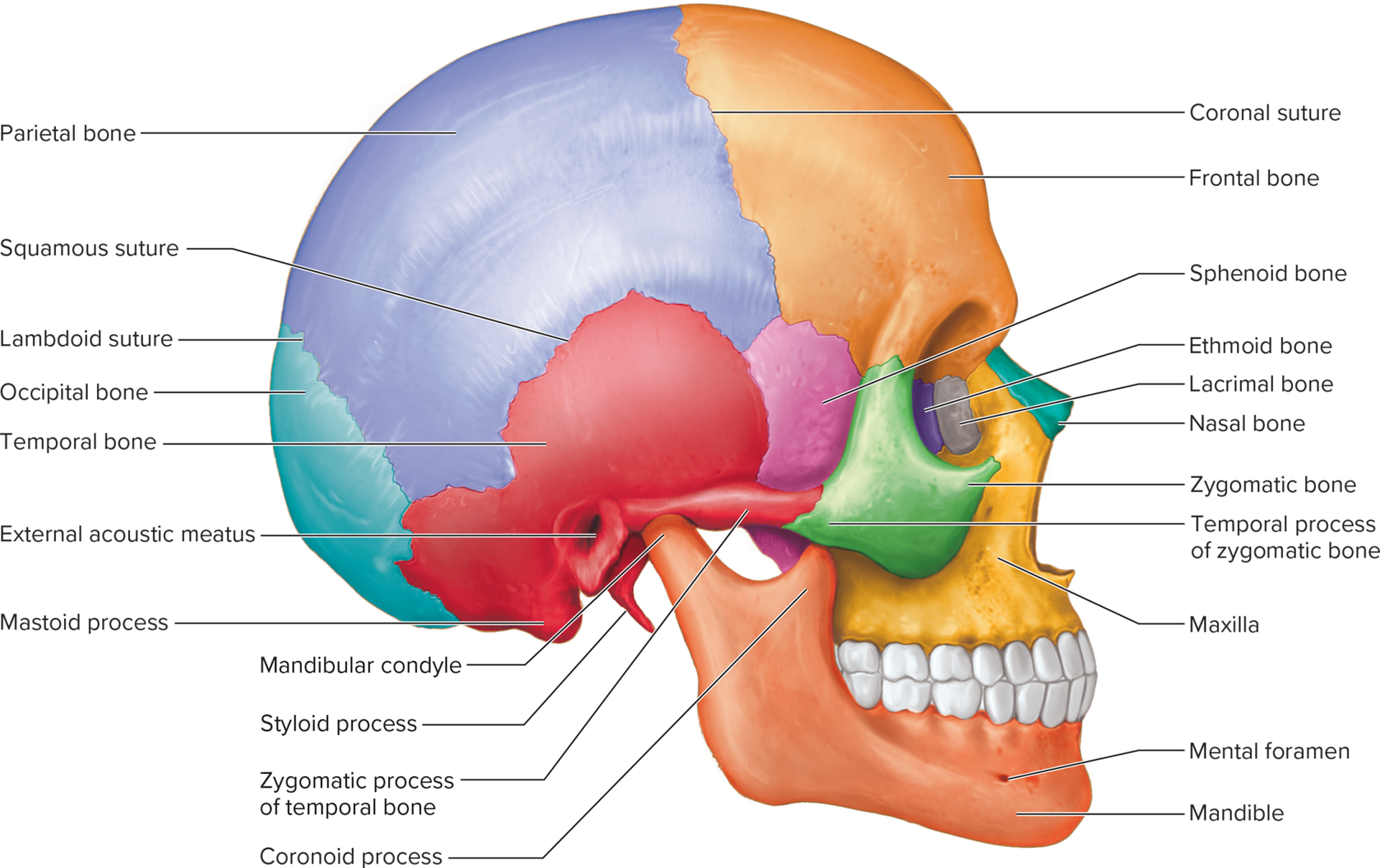
Locate and name each of the facial bones.
The maxillae are the upper jaw bones; they make up parts of the nasal cavity, hard palate, and eye orbits. The palatine bones lie behind the maxillae, and make up part of the hard palate and nasal cavity. The zygomatic bones form the cheek prominences and part of the eye orbits. The lacrimal bones form the medial corners of the eye orbits. The nasal bones form the bridge of the nose. The vomer bone forms the inferior portion of the nasal septum, along the midline of the nasal cavity. The inferior nasal conchae scroll inward from the lateral walls of the nasal cavity. The mandible is the lower jaw bone.
Explain how an adult skull differs from that of an infant.
Compared to the skull of an adult, the infantile skull has a smaller face, a more protruding forehead, larger eye orbits, a smaller jaw, a smaller nasal cavity, incompletely formed sinuses, and a frontal bone that consists of 2 portions. Also the major cranial bones have not yet completely grown together at sutures; they are joined by fibrous membranes, with soft spots between them called fontanels. The bones have not yet completed the ossification process, so they are softer than those of an adult.