3. General Therapeutic Principles for GI Disorders
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
130 Terms
What percent of total body water is composed of intracellular fluid?
66%
What percent of total body water is composed of extracellular fluid?
33%
Of the extracellular fluid, what percent is composed of interstitial fluid?
75% or 3/4
Of the extracellular fluid, what percent is composed of intravascular fluid?
25%
Fluid deficit of the interstitial fluid is ________.
dehydration
Fluid deficit of what is dehydration?
interstitial fluid
What causes signs of dehydration with deficit?
interstitial fluid deficit
Fluid deficit of of the intravascular fluid is ________.
hypovolemia
Fluid deficit of what is hypovolemia?
intravascular fluid
What causes signs of hypovolemia with deficit?
intravascular fluid deficit
What component is what is changed with IV fluids?
intravascular fluid
What are fluids used in GIT disease to address?
D
S
E
dehydration
shock
electrolyte imbalances
When using fluids, what must be determined?
electrolyte abnormalities and acid-base status
________ ________ fluids correct acid-base deficits faster than ________ fluids.
balanced isotonic; acidifying
What are examples of balanced isotonic fluids?
L
N
P
LRS
normosol-R
plasmalyte-A
What are examples of acidifying fluids?
0.9% NaCl
What is a common pathology in chronic GIT disease?
hypoalbuminemia
When it comes to hypoalbuminemia, how is it most critical to be addressed?
treatment of underlying disease and nutritional support
What are sources of oncotic support for hypoalbuminemia?
B
C
H
S
blood products (fresh frozen plasma, whole blood)
canine-specific albumin
human specific albumin (not recommended)
synthetic colloids (hetastarch)
What are the different routes for fluid therapy?
E
P
S
enteral (PO)
parenteral (IV, IO)
subcutaneous (SC)
What is the best route for the GIT of fluid therapy? What is something that could affect this?
enteral (PO); patient needs to be able to tolerate oral fluids
When are parenteral fluids (IV, IO) indicated?
hypovolemic/dehydrated patient or in one that cannot tolerate enteral fluids
When are subcutaneous fluids indicated?
only for cases of mild dehydration or administration of maintenance fluids
What is the concentration of maintenance fluids?
20-30 mL/kg
What is the rate of fluid therapy dictated by?
the rate and severity of fluid loss
What is the general rule when it comes to the rate of fluid therapy?
replace like with like (replace acute severe losses rapidly and chronic losses more slowly)
Ideally, fluid deficits and electrolyte imbalances are corrected within how long?
24 hours
What are daily crystalloid fluids based on calculating?
D
M
O
dehydration
maintenance
ongoing losses
What is the dehydration assessment of a euhydrated (normal) animal?
< 5% dehydrated
Describe a dehydration assessment of 5-6%.
mild dehydration, with minimal loss of skin turgor and semi-dry MM
Describe a dehydration assessment of 7-8%.
moderate dehydration, with moderate loss of skin turgor, dry MM, weak rapid pulses, and sunken eyes
Describe a dehydration assessment of 9-10%.
severe dehydration, with marked loss of skin turgor, sunken eyes, tachycardia, dry MM, weak pulses, and hypotension
How do you calculate dehydration deficit?
body weight (kg) X % dehydration = fluid deficit (L)
Sally is a 35 kg, 5 year old female spayed lab who present for vomiting, diarrhea, and anorexia of 24 hours duration. She is approximately 7% dehydrated after having gotten into the garbage. What is her dehydration deficit?
35 kg X 0.07 = 2.45 L or 2,450 mL
What are the maintenance needs for a dog?
60 mLs/kg/day
What are the maintenance needs for a cat?
40 mLs/kg/day
How do you calculate maintenance needs?
body weight (kg) X maintenance concentration = maintenance needs (mLs/day)
What are Sally’s (35 kg) maintenance needs for fluids?
35 kg X 60 mLs/kg = 2,100 mLs/day
1 cup of vomit/diarrhea is about how many mLs?
240 mLs
What are Sally’s (35 kg) ongoing losses if she’s lost about 2 cups of V/D in the last hour?
240 mL + 240 mL = 480 mLs of fluid that need to be added back
What is the initial resuscitation fluid bolus for a dog?
15-20 mLs/kg
What is the initial resuscitation fluid bolus for a cat?
5-10 mLs/kg
How do you calculate the fluid rate?
dehydration deficit + maintenance + ongoing losses
How do you calculate the initial resuscitation bolus for a dog?
body weight (kg) X 15-20mLs/kg
Determine Sally’s fluid rate and initial resuscitation bolus. Her body weight is 35 kg, her dehydration deficit is 2,450 mLs, her maintenance is 2,100 mLs, and her ongoing losses are 480 mLs.
2,450 mLs + 2,100 mLs + 480 mLs = 5,030 mLs/day or 210 mLs/hour
35 kg X 15 mLs/kg = 525 mLs IV isotonic crystalloid over 15-20 mins
5,030 mLs/day - 525 mLs = 4,505 mLs/day or 188 mLs/hour
What should adjustments be made based on?
R
W
V
response to fluid
weight
vitals
When giving fluids, you do not want more than what percent weight gain?
> 10% weight gain
It is important to add ________ to the fluids at some point, but not more than ____ ________.
KCl; 0.5 mmol/kg/hr
What are some signs of overloading of fluids/overhydration?
P
P
P
R
pulmonary edema
pulmonary effusion
pitting edema
respiratory distress
In patients with normal vascular permeability, only ________ of the IV isotonic crystalloids administered remain in the intravascular space after 30 minutes. ________ has moved into the interstitial space. This is why you may need to add colloids like hetastarch or hypertonic saline.
25%; 75%
What species overhydrate easily?
cats
What is the classic triad that hypovolemic cats present with? How is this different from dogs?
hypotension, hypothermia, and bradycardia; dogs get tachycardia
What is very frequently used to address non-specific GIT disease, particularly acute?
symptomatic therapy
What is a good way to dietarily management acute GIT disease?
bland, easily digestible diets
What should homemade versions of a bland, easily digestible diet include?
B
L
L
B
B
boiled chicken
lean hamburger
low fat cottage cheese
boiled rice
boiled potatoes
What is selected if dietary allergy or intolerance is suspected?
elimination (hypoallergenic) diets
What are examples of diets used in dietary allergy or intolerance?
S
H
H
sole source protein/antigen diets
hydrolyzed diets
homemade hypoallergenic diets
When is an ultra low fat diet indicated?
dogs with protein losing enteropathy due to intestinal lymphangiectasia
When might low fat diets be indicated?
for weight loss and chronic pancreatitis
What is often useful in the management of large intestinal diarrhea?
fiber
type of fiber that is metabolized by bacteria to form VFAs that are trophic to enterocytes
soluble fiber
type of fiber that increases fecal bulk, which stimulates motility and decreases spasms
insoluble fiber
When should you not use a high fiber diet?
for the management of obstipation or strictures
How do you calculate the basal energy requirement for cats and dogs?
30 X body weight in kg + 70 = kcal/day
How do you calculate the maintenance energy requirement?
BER X adjustment factor = kcal/day
What does the maintenance energy requirement account for?
increases in metabolism
Jack is a 1 year old intact MinPin (10 kg) who is recovering from his injuries after being HBC. How many kcals/day?
30 X 10 kg + 70 = 370 kcals/day (BER)
370 X 1.5 (adjustment factor for trauma) = 555 kcals/day (MER)
What may improve the appetite in patients with low vitamin B12 levels?
cobalamin supplementation
What are special nutritional management practices?
W
C
warm, aromatic food
control nausea
What appetite stimulant can be used in both dogs and cats?
mirtazapine
What appetite stimulant is used in cats?
cyproheptadine
FDA approved appetite stimulant for dogs
capromorelin (entyce)
FDA approved appetite stimulant for cats with CKD and weight loss
capromorelin (elura)
What type of feeding should be used whenever possible? Why?
enteral nutrition; gut mucosa is dependent on local nutrition for healthy structure and function
What is another type of feeding possibility? What are different types?
O
N
P
E
G
E
tube feeding
orogastric
nasogastric/esophageal
pharyngostomy
esophagostomy
gastrostomy
enterostomy
How should you confirm NG tube placement?
with radiographs
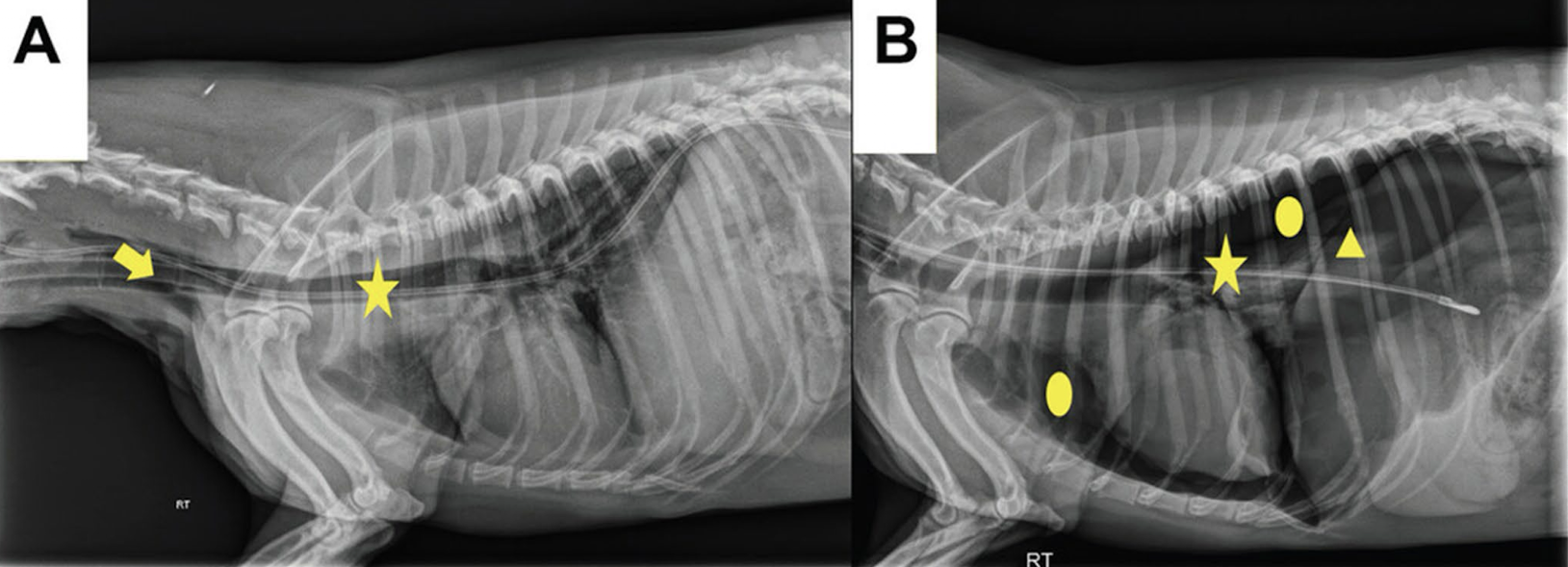
What is wrong with the placement of this NG tube in image A? What is going on in image B?
the tube is in the trachea; tube is in the correct location but it caused a pneumothorax

What is the wrong with the NG tube in this radiograph?
it is coiled
type of feeding that passes the GIT
parenteral nutrition
IV solution that is customized and administered through a dedicated jugular IV catheter
total parenteral nutrition (TPN)
provides only about 50% of the caloric requirement and can be given through a peripheral catheter
partial parenteral nutrition (PPN)
What are the major disadvantages of parenteral nutrition?
R
C
A
risk of infection
cost
availability
What are the peripherally acting antiemetics?
K
A
kaopectate/bismuth subsalicylate (pepto bismol)
aminopentamide (centrine)
What are the centrally acting antiemetics?
M
O
M
C
P
maropitant (cerenia, NK 1 antagonist)
ondansetron (zofran, 5 HT antagonist)
metoclopramide (reglan, inhibits CRTZ, prokinetic)
chlorpromazine
prochlorperazine (compazine)
What are the effects of antacids?
L
A
lower gastric acid levels
anti-dyspeptic effect (although not true antiemetics)
What are the major categories of antacids?
A
G
P
acid titrating drugs
gastric acid secretion inhibitors (H2 blockers)
proton pump inhibitors (PPIs)
What are examples of acid titrating drugs?
aluminum/magnesium hydroxide
What are examples of H2 blockers?
C
F
R
N
cimetidine (tagamet)
famotidine (pepcid)
ranitidine (zantac)
nizatidine (axid)
Which H2 blockers do not have prokinetic properties?
cimetidine and famotidine
Which H2 blockers have gastric prokinetic properties?
ranitidine and nizatidine
With H2 blockers, there is ________ of receptors so that acid ________ occurs with ________-________ use.
upregulation; escape; long-term
What are the most effective drugs used to decrease gastric acid secretion in dogs and cats?
proton pump inhibitors
What are examples of proton pump inhibitors?
O
l
E
omeprazole (prilosec)
lansoprazole (prevacid)
esomeprazole (nexium)
What is the purpose of intestinal protectants?
form a local coating or barrier
What are examples of intestinal protectants?
K
P
B
S
M
kaolin
pectin
barium sulfate
sucralfate (carafate)
misoprostol (cytotec)
intestinal protectant that forms an internal “bandage” on ulcerated mucosa
sucralfate (carafate)
intestinal protectant that is a prostaglandin E1 analog
misoprostol (cytotec)
What is used to treat exocrine pancreatic insufficiency (EPI)?
pancreatic enzyme supplement (viokase-V)
True or false: The powdered form of the pancreatic enzyme supplement works best. It should be mixed with food but it is not necessary to “incubate.”
true
What is the purpose of motility modifiers?
drugs that delay or shorten transit time in the GIT