homeostasis and the kidney
1/9
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
10 Terms
homeostasis and the kidney
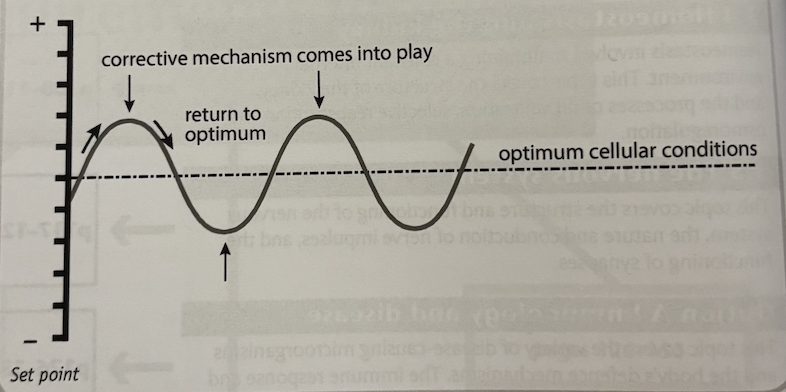
homeostasis is the maintenance of the internal environment within tolerable limits. to accomplish this, the body uses negative feedback, whereby the body responds in such a way as to reverse the direction of change. this tends to keep physical parameters constant e.g. temperature at 37 degrees, and glucose at 90mg per 100cm³ blood. this involves:
INPUT - a change away from the set point or norm e.g. rise in core body temp
RECEPTOR - a sensory that detects the change from the set point, e.g. temperature receptors
CONTROL CENTRE - or coordinator detects signals from receptors and coordinates a response via effectors e.g. hypothalamus in the brain
EFFECTOR - bring about changes which returns the body to set point e.g. glands in skin release sweat
OUTPUT - corrective procedure, e.g. evaporation of sweat cools skin
excretion
excretion is the removal of wastes made by the body e.g. carbon dioxide and water from respiration and urea from deamination of excess amino acids. surplus amino acids are deaminated in the liver: the amine group (-NH2) is removed, converted to ammonia and then into urea. urea is removed from the body by the kidney. the organic acid that remains can be used in respiration, or converted to lipids or glucose
the kidney
the kidney has two main functions:
excretion - excretion of nitrogenous waste i.e. urea from the body
osmoregulation - control of the water potential body fluids including blood
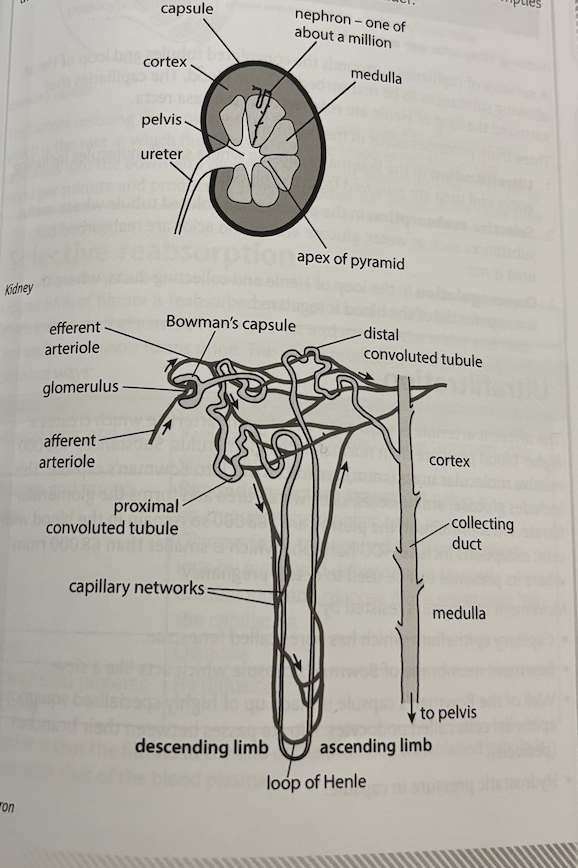
the body has two kidneys, each containing around a million nephrons, each nephron is 30mm long. they are supplied with blood containing oxygen and waste (including urea) from the renal artery, and filtered blood returns to the general circulation by the renal vein. excess water and solutes including urea is called urine, and it drains into the collecting ducts and pelvis which empties urine into the ureter. each ureter connects to the bladder
a network of capillaries surrounds the convoluted tubules and loop of Henle, allowing substances to be reabsorbed into the blood. the capillaries that surrounded the loop of Henle are referred to as the vasa recta. three main processes occur in the nephron:
ultrafiltration in the bowman’s capsule where small molecules including water and urea are removed from the blood
selective reabsorption in the proximal convoluted tubule where useful substances such as water, glucose and amino acids are reabsorbed but urea is not
osmoregulation in the loop of Henle and collecting ducts, where the water potential of the blood is regulated
ultrafiltration
the different arteriole is wider than the efferent arteriole which creates a higher blood pressure than normal in the glomerulus. substances <68000 relative molecular mass (rmm) are forced out into Bowmans capsule. this includes glucose, amino acids, salts, water, urea and forms the glomerular filtrate. most proteins in the plasma are >68000 so remain in the blood with cells: exceptions include HCG hormone which is smaller than 68000 rmm where its presence can be used to detect pregnancy
movement of filtrate is resisted by:
capillary epithelium which has pores called fenestrae
basement membrane of Bowmans capsule which acts like a sieve
wall of the Bowmans capsule is made up of highly specialised squamous epithelial cells called podocytes. filtrate passes between their branches (pedicels)
hydrostatic pressure in capsule
Low water potential of the blood in glomerulus (lowered by loss of water into capsule)
the factors resisting the movement of filtrate determine the filtration rate, which is the rate at which fluid passes from the blood in the glomerular capillaries into the Bowmans capsule. the kidneys receive around 1100cm³ of blood per minute and produce 125cm³ of glomerular filtrate in the same time.
selective reabsorption
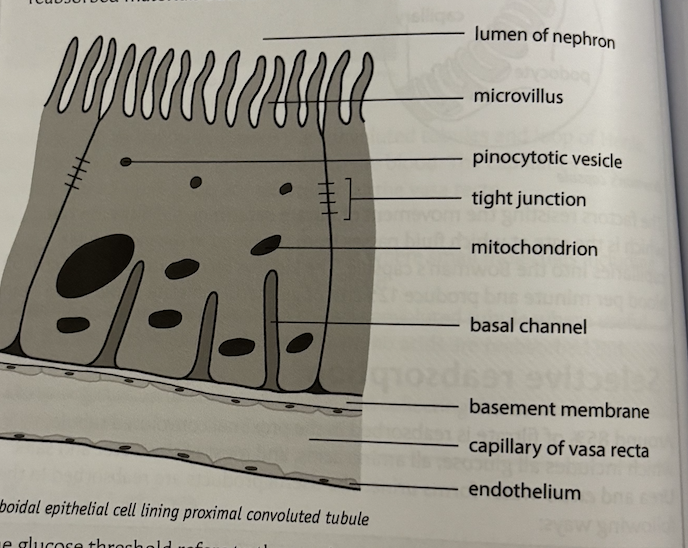
around 85% of filtrate is reabsorbed in the proximal convoluted tubule, which includes all glucose, all amino acids, and most of the water and salts. urea and excess water forms urine. the useful products are reabsorbed in the following ways:
mineral ions, and salts - facilitated diffusion and active transport into epithelial cells
glucose and amino acids - secondary active transport using a co-transport with two sodium ions by facilitated diffusion into the cell. sodium ions and glucose move separately into the capillaries
water - osmosis
some filtered proteins and urea - by diffusion
the proximal convoluted tubule is adapted for reabsorption in the following ways:
cells lining the tubule have a large surface area due to the presence of microvilli and basal channels (infolding of the membrane in contact with the capillary). there are also large numbers of nephrons
cells contain many mitochondria which provide ATP for active transport of solutes
close association with capillaries which creates a short diffusion pathway between cells and the peritubular capillaries
tight junctions are found between adjacent cells which prevent seepage of reabsorbed materials back into the filtrate
the glucose threshold refers to the maximum mass of glucose that can be reabsorbed in the proximal convoluted tubule. where blood glucose concentrations are very high e.g. in type 1 and 2 diabetes, not all of it can be reabsorbed in the tubule, so some remains in the filtrate and therefore in the urine. the majority of water (90%) is reabsorbed in the loop of Henle and distal convoluted tubule and collecting duct. the volume of water reabsorbed in the convoluted tubule and collecting duct varies according to the body’s needs.
osmoregulation
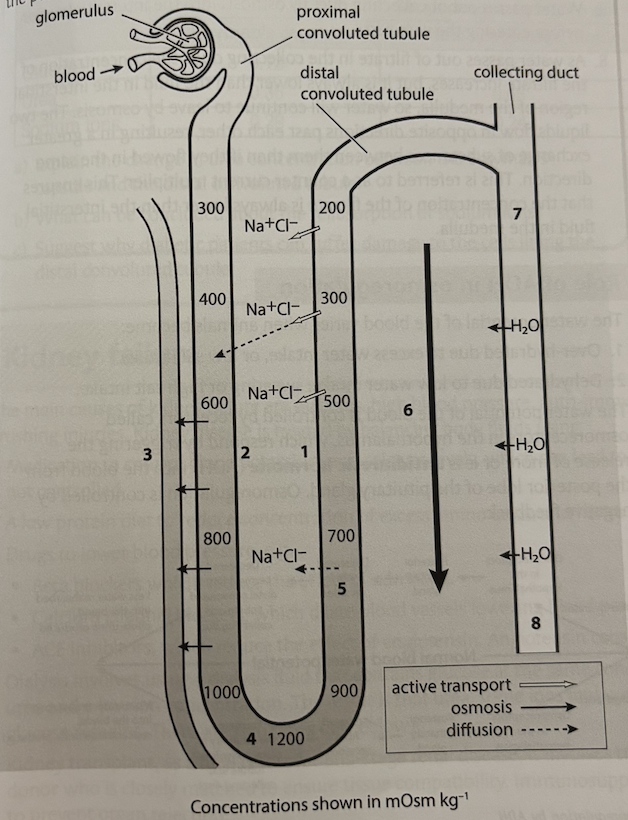
controlling the water potential of the body is important in animals as it maintains the concentration of enzymes and metabolites, and prevents cells from bursting or creating. the loop of Henle is responsible for reabsorption of some water from the descending limb, but its main function is to create an increasing ion concentration within the interstitial region of the medulla, which allows water to be reabsorbed by the collecting duct. the volume of water reabsorbed from the DCT and collecting duct, and hence the resulting water potential of the blood, is influenced by antidiuretic hormone, which increases the permeability of the tubule and duct walls to water
Na+ and Cl- ions are actively pumped out of the ascending limb
this creates an increasing ion concentration in the interstitial region
walls of the descending limb are permeable to water so water leaves by osmosis into the interstitial region before entering the capillaries (vasa recta)
water is progressively lost down the descending limb reaching typically a concentration of 1200 most kg^-1 of water at the base. (longer loops can reach much higher concentrations because more Na+ and Cl- ions can be actively transported out of the ascending limb
the concentration of the filtrate decreases in the lumen of the nephron in the ascending limb, as Na+ and Cl- ions are actively pumped out
this creates an increasing ion concentration gradient in the interstitial region towards the base of the loop
water passes out of the collecting duct by osmosis into the interstitial region before entering the vasa recta
as water passes out of filtrate in the collecting duct, the concentration of the filtrate increases, but is is always lower than the fluid in the interstitial region of the medulla, so water will continue to leave by osmosis. the two liquids flow in opposite directions past each other, resulting in a greater exchange of substances between them than if they flowed in the same direction. this is referred to as a counter current multiplier. this ensures that the concentration of the filtrate is always lower than the interstitial fluid in the medulla
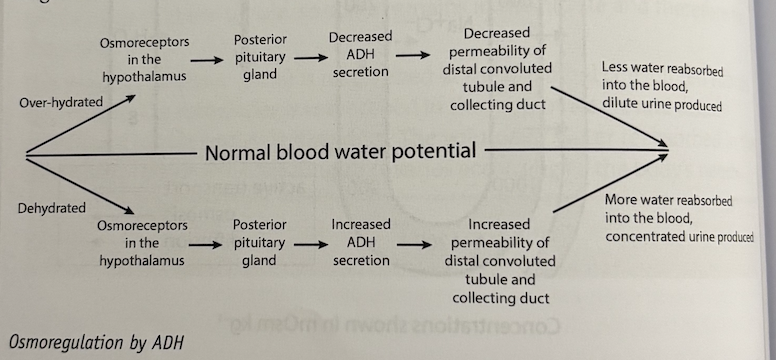
role of ADH in osmoregulation
the water potential of the blood varies when animals become:
over hydrated due to excess water intake, or low salt intake
dehydrated due to low water intake, sweating or high salt intake
the water potential of the blood is controlled by receptors called osmoreceptors in the hypothalamus, which respond by triggering the release of more or less antidiuretic hormone (ADH) into the blood from the posterior lobe of the pituitary gland. osmoregulation is controlled by negative feedback.
ADH binds to membrane receptor proteins found on the surface of cells lining the distal convoluting tubule and collecting duct walls. the binding of ADH triggers vesicles containing intrinsic membrane proteins called aquaporins containing pores that allow water to pass through the walls down the water potential gradient. when ADH concentration falls, aquaporins are removed from the cell membrane
kidney failure
the main causes of kidney failure are diabetes, high blood pressure, auto-immune disease, infection and crushing injuries. kidney disease is treated by balancing body fluids using:
medication to control blood potassium and calcium levels, which can lead to heart disease and kidney stones if not controlled
a low protein diet to reduce concentration of excess amino acids and hence concentration of urea
drugs to lower blood pressure e.g.
- beta blockers, which reduce the effects of adrenaline
- calcium channel blockers, which dilate blood vessels, lowering blood pressure
- ACE inhibitors, which reduce the effect of angiotensin. angiotensin causes blood vessels to constrictdialysis involves using a dialysis fluid that contains glucose at the same concentration as the blood, but has no urea and low ion concentration. the result is that urea, some ions and water diffuse out of the blood, but glucose remains
kidney transplant, as a final resort for end-stage renal disease. it involves transplanting one kidney from a donor who is closely matched to ensure tissue compatibility. immunosuppressants have to be used afterwards to prevent organ rejection
dialysis
there are two types:
haemodialysis which takes blood (usually from an artery in the arm), and passes it through a dialyser containing thousands of fibres each consisting of selectively permeable dialysis tubing and dialysis fluid. to ensure maximum transfer, a counter current is used where blood and dialysis fluid move in opposite directions. heparin is used to prevent the blood from clotting. dialysis takes several; hours and is repeated several times a week
peritoneal dialysis involves passing dialysis fluid into the peritoneum through a catheter. the peritoneum contains numerous capillaries which exchange materials with the dialysis fluid, which is changed after about 40 minutes, and the process repeated several times a day. this type has the advantage that the patient is able to move around, but is less effective than haemodialysis so fluid retention is likely
excretion in other animals
freshwater fish excrete ammonia:
ammonia is highly soluble but is very toxic so it cannot be stored. it must be excreted immediately using large volumes of water to dilute it (which is freely available to freshwater fish)
mammals excrete urea:
urea is much less toxic than ammonia and so requires less water to dilute it, and can be stored for short periods of time
it requires energy to convert ammonia to urea but is an adaptation to life on land, as it helps prevent dehydration because less water is needed to excrete it
birds, reptiles and insects excrete uric acid:
uric acid is virtually non-toxic and therefore requires very little water to dilute it
the conversion of ammonia to uric acid requires much energy but allows these animals to survive in very arid environments
a major advantage for birds is that very small volumes of water are needed reducing weight in flight
the length of the loop of henle is an adaptation to where the animal has evolved. beavers, which live in fresh water where water is plentiful, have very short loops of henle and produce large volumes of dilute urine. animals that live in arid environments e.g. the kangaroo rat, have much longer loops of henle and produce small volumes of highly concentrated urine. they have a higher proportion of these nephrons which are referred to as juxtamedullary nephrons, with the Bowmans capsule being located closer to the medulla and loops of henle which penetrate deep into the medulla. the longer the loop of henle, the more concentrated the urine that can be produced (which saves water), because a higher ion concentration int he medulla can be created by the counter current multiplier.
animals in arid environments also rly more on metabolic water e.g. the camel which largely respires fat stored in its hump. other mammals show behavioural adaptations such as being nocturnal, coming out at night to forage when its cooler.