Local Anesthesia: Lecture 10 Readings - Mand Nerve Injuries Implants & Paresthesia
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
What has become the standard of care for simple and complex edentulous areas of the maxilla and mandible?
dental implant surgery
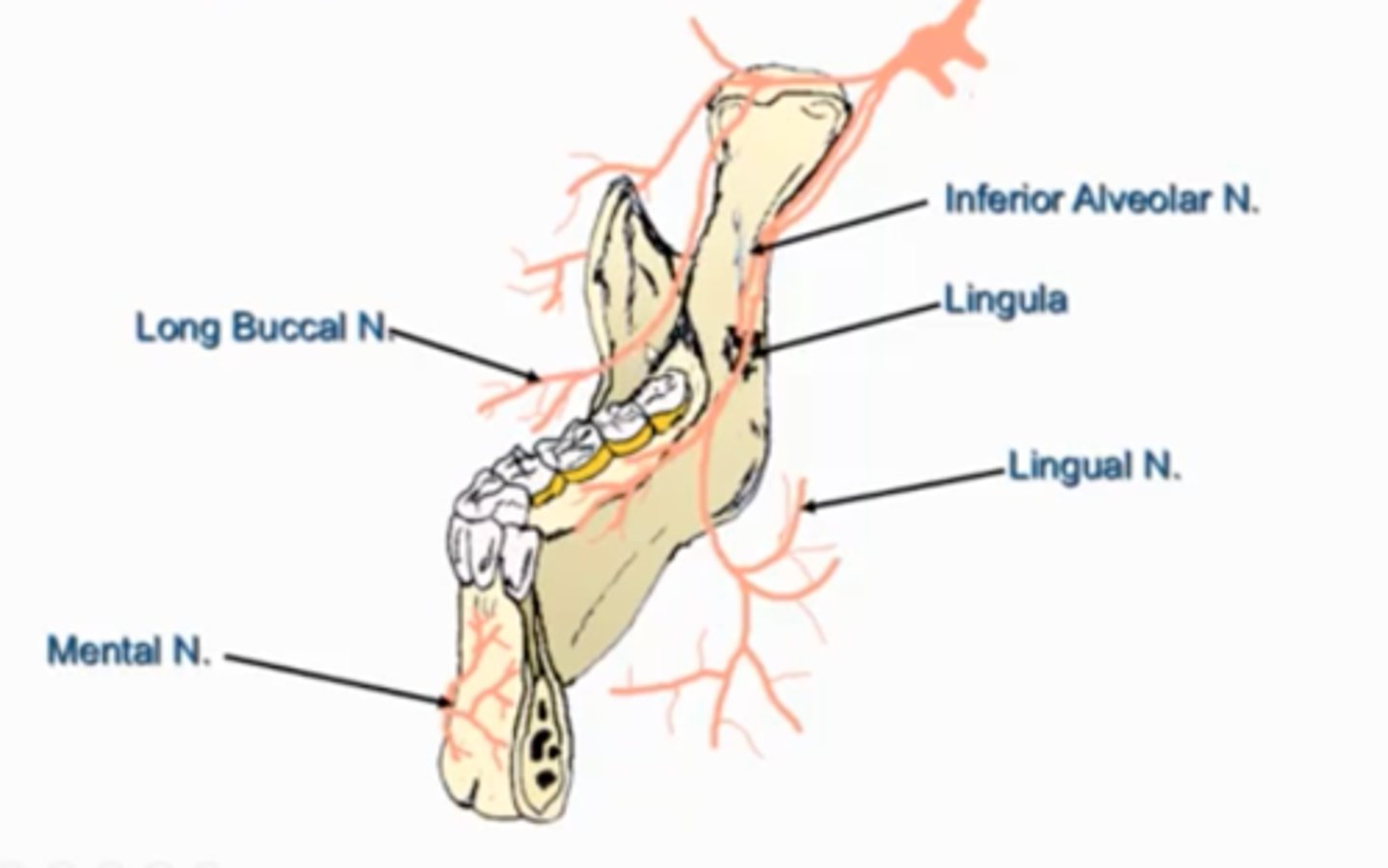
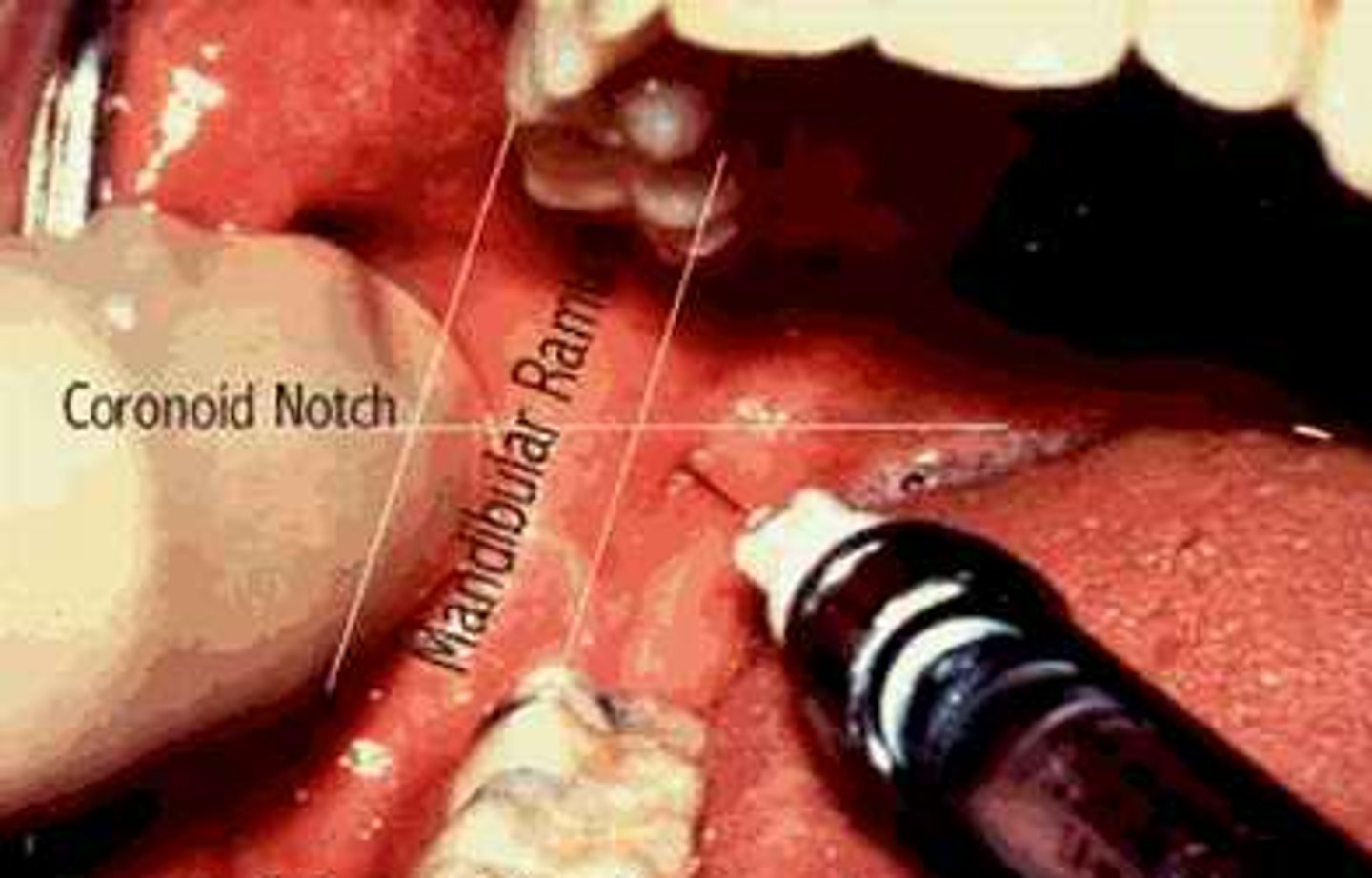
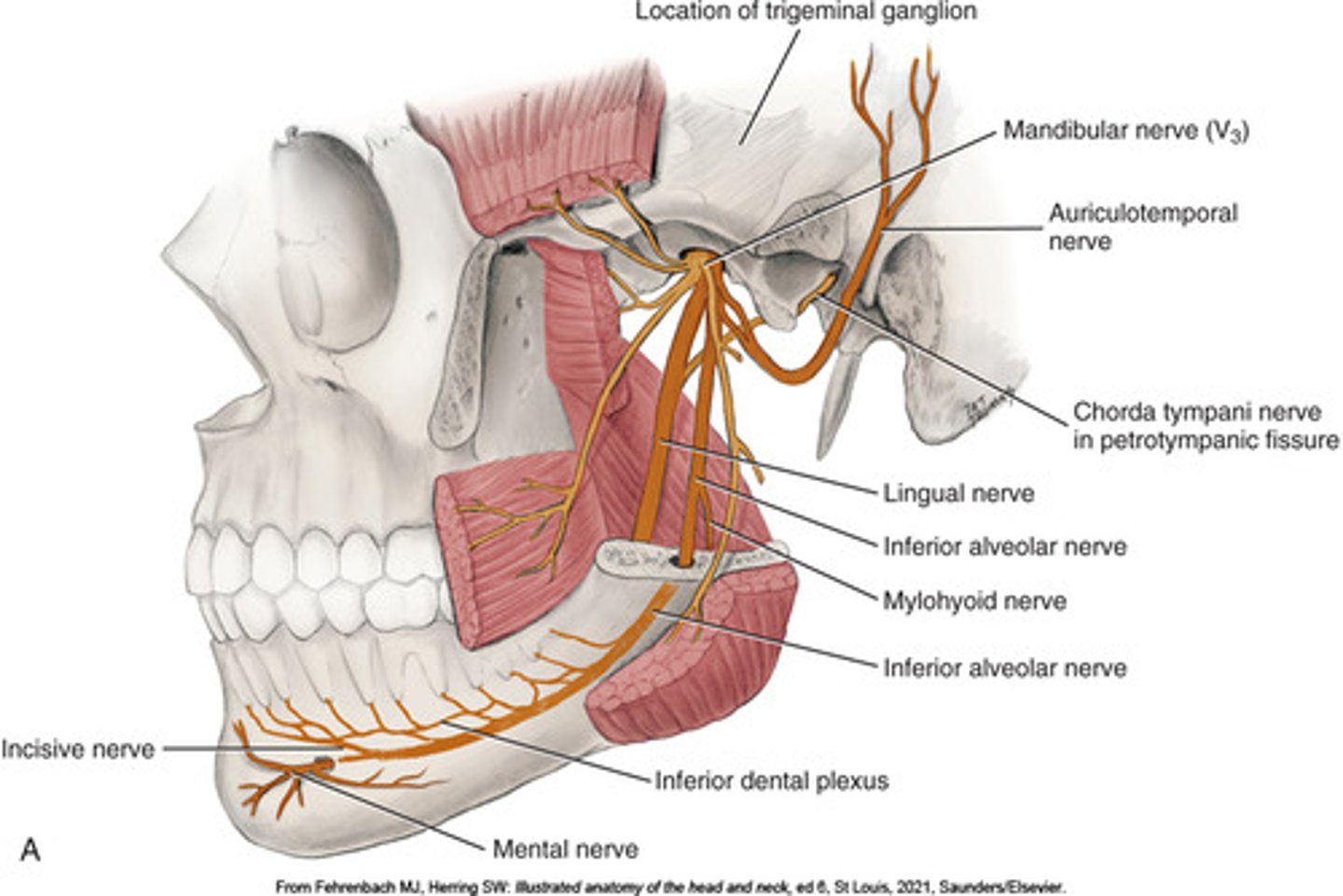
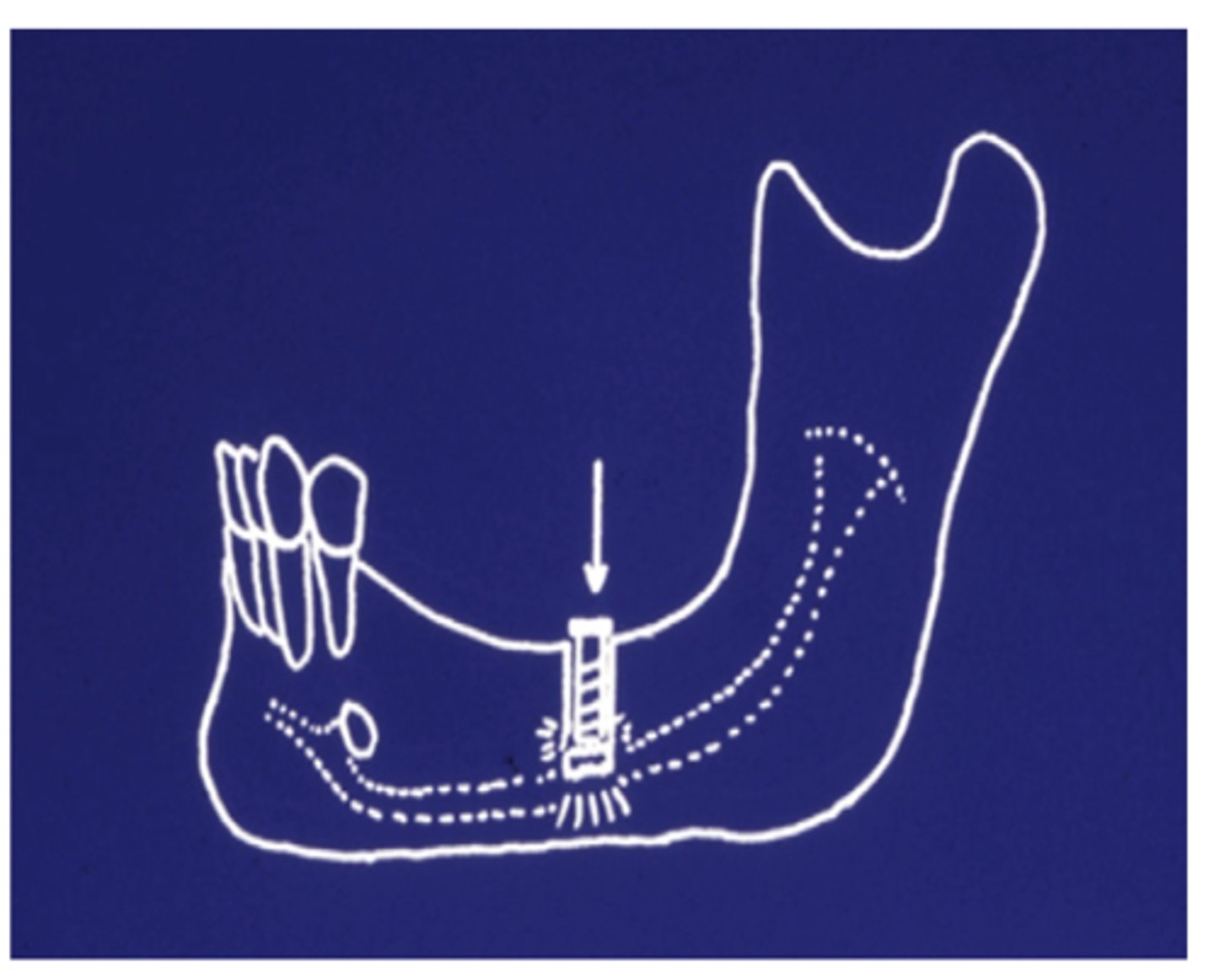
What is at risk of injury - a known complication of implant restorations of the posterior mandible?
branches of the mandibular division of trigeminal nerve:
-inferior alveolar nerve (IAN)
-lingual nerve
-mental nerve
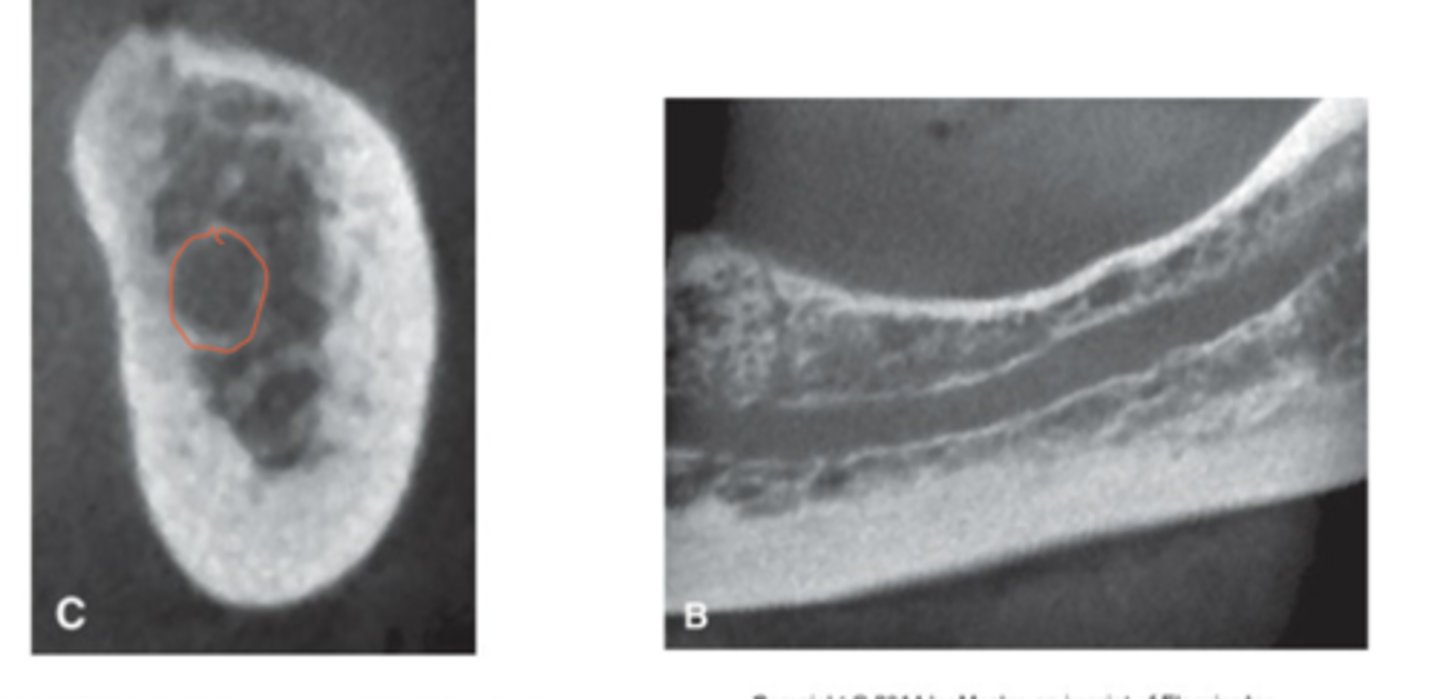
What can be used to assist in localization of the inferior alveolar canal for implant surgery?
cone beam computed tomography (CT) scans and high definition panoramic radiographs
Can mandibular nerve injury occur despite correct planning with advanced imaging?
Yes, nerve injury is still possible even with proper planning.
What type of dysfunction is a known complication of branches of the mandibular division of CN V injury during implant surgery?
Sensory dysfunction, which can be persistent or painful.
Why is altered sensation after implant surgery a significant concern for clinicians?
It can lead to medicolegal implications and patient distress.
What is key to maximizing recovery from nerve injury after implant surgery?
Prompt recognition, acknowledgment of symptoms, and timely management

What are the two main problems clinicians face after a nerve injury from dental implants?
(1) Treating the neurosensory disturbance
(2) Deciding how to restore the affected dental area

How can implantologists best support patients experiencing nerve injuries?
Maintain a supportive relationship and provide appropriate treatment recommendations.
What is the focus of the article regarding mandibular nerve (MdN) injuries?
Causes and management of MdN injuries from dental implant surgery.
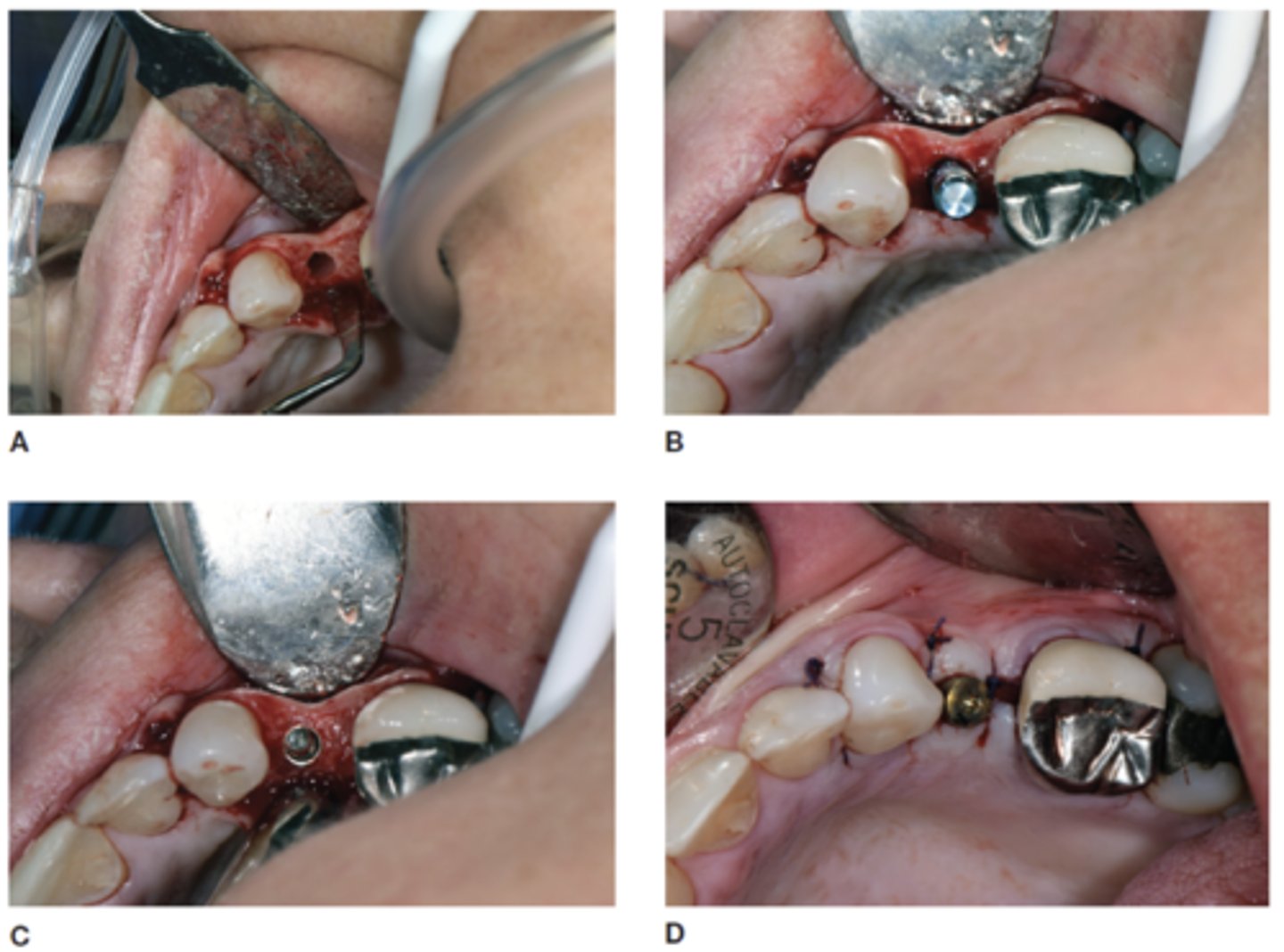
What are the four most frequent causes of MdN injury during dental implant surgery?
(1) Errors in evaluation and planning
(2) Local anesthetic injection
(3) Bone drilling
(4) Implant placement
Which nerves can be injured by local anesthetic injection during implant procedures?
IAN Inferior alveolar nerve (IAN), lingual nerve (LN), and mental nerve (MN).
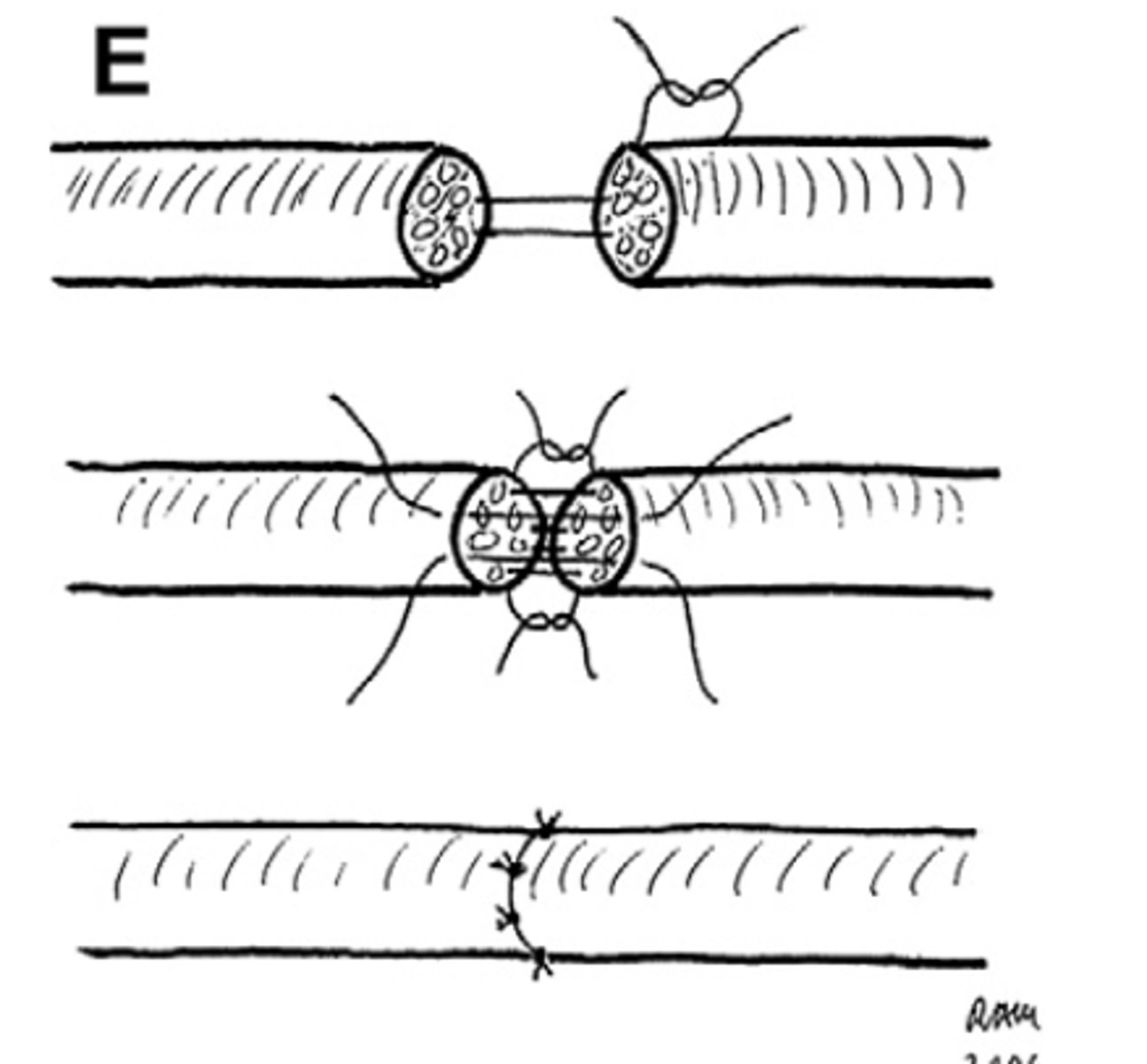
What are the three proposed mechanisms of nerve injury from anesthetic injections?
(1) Direct intraneural injection w/ mechanical injury to the nerve
(2) interruption of vessels in mesoneurium -> Hemorrhage -> scar formation
(3) Chemical toxicity from contaminated carpules

What is recommended to be done before all local anesthetic injections?
aspiration
What should a clinician do if a patient reports paresthesia during injection?
Withdraw needle a few millimeters, aspirate again, and record the event in the chart.
What patient sensation during injection may indicate nerve contact?
shock-like paresthesia

How common is nerve injury from local anesthetic injections?
Reported incidence is between 1 in 26,762 to 1 in 160,571
Why can it be hard to tell if nerve injury was from injection or implant surgery?
Sedated patients can't report paresthesia during injection, and injuries may lack clinical or radiographic signs.

What may a small percentage of patients who have suffered an injection-related injury be misdiagnosed with?
injury related to the dental implant surgery -> subsequently undergo diagnostic or exploratory surgical procedures that reveal no visible nerve injury at implant location
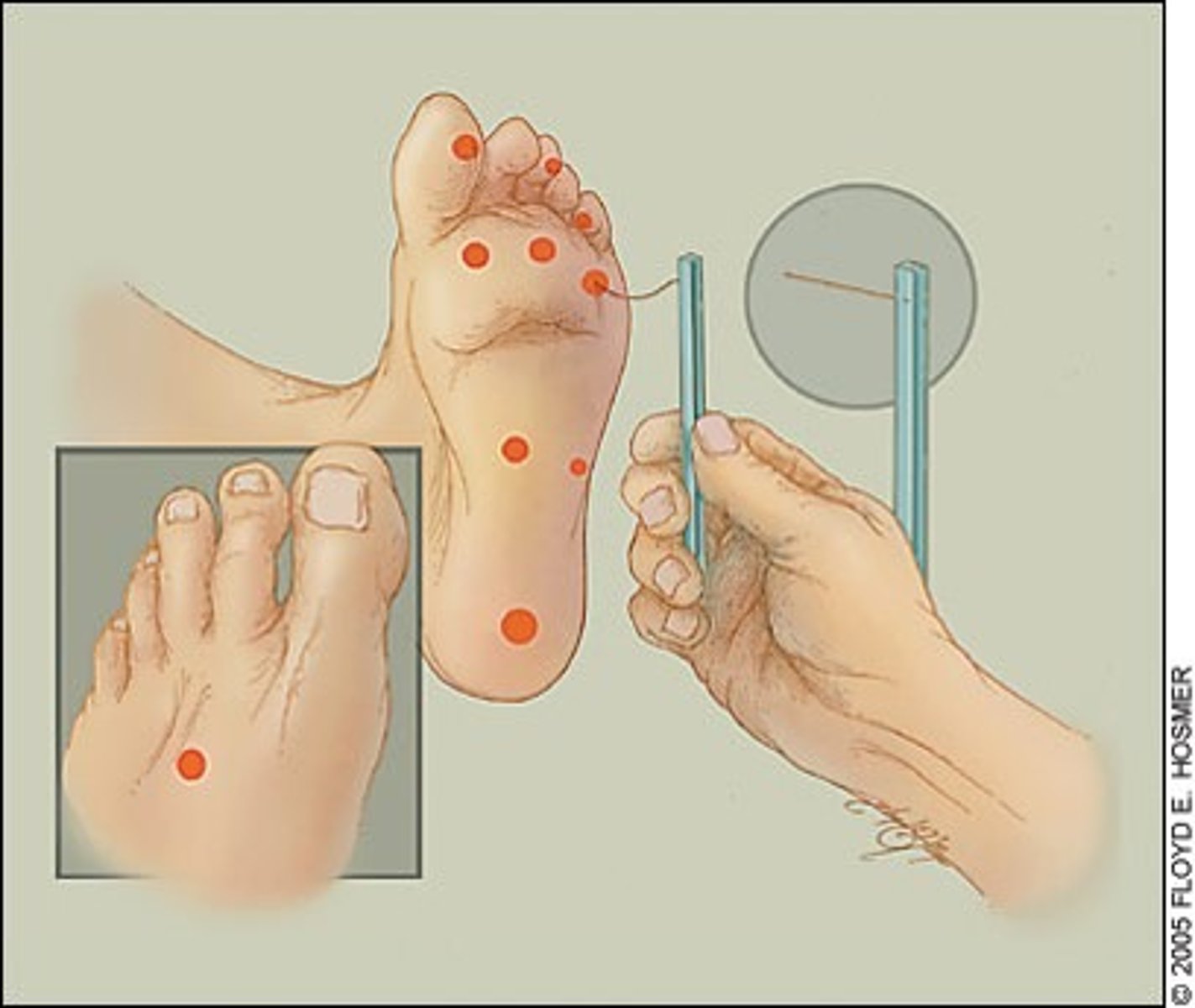
What scale is used to evaluate neurosensory disturbances in the oral and maxillofacial region?
Medical Research Council Scale (MRCS)
What is crucial for successful nerve injury recovery according to Seddon?
Timely diagnosis and treatment—delays risk missing the optimal repair window.

What is treatment of the pt with dental implant-associated nerve injury dependent on?
correct diagnosis of the injury and timely management
When can corticosteroids be given perioperatively to reduce nerve injury risk?
Some recommend preoperative administration; others wait until post-op.
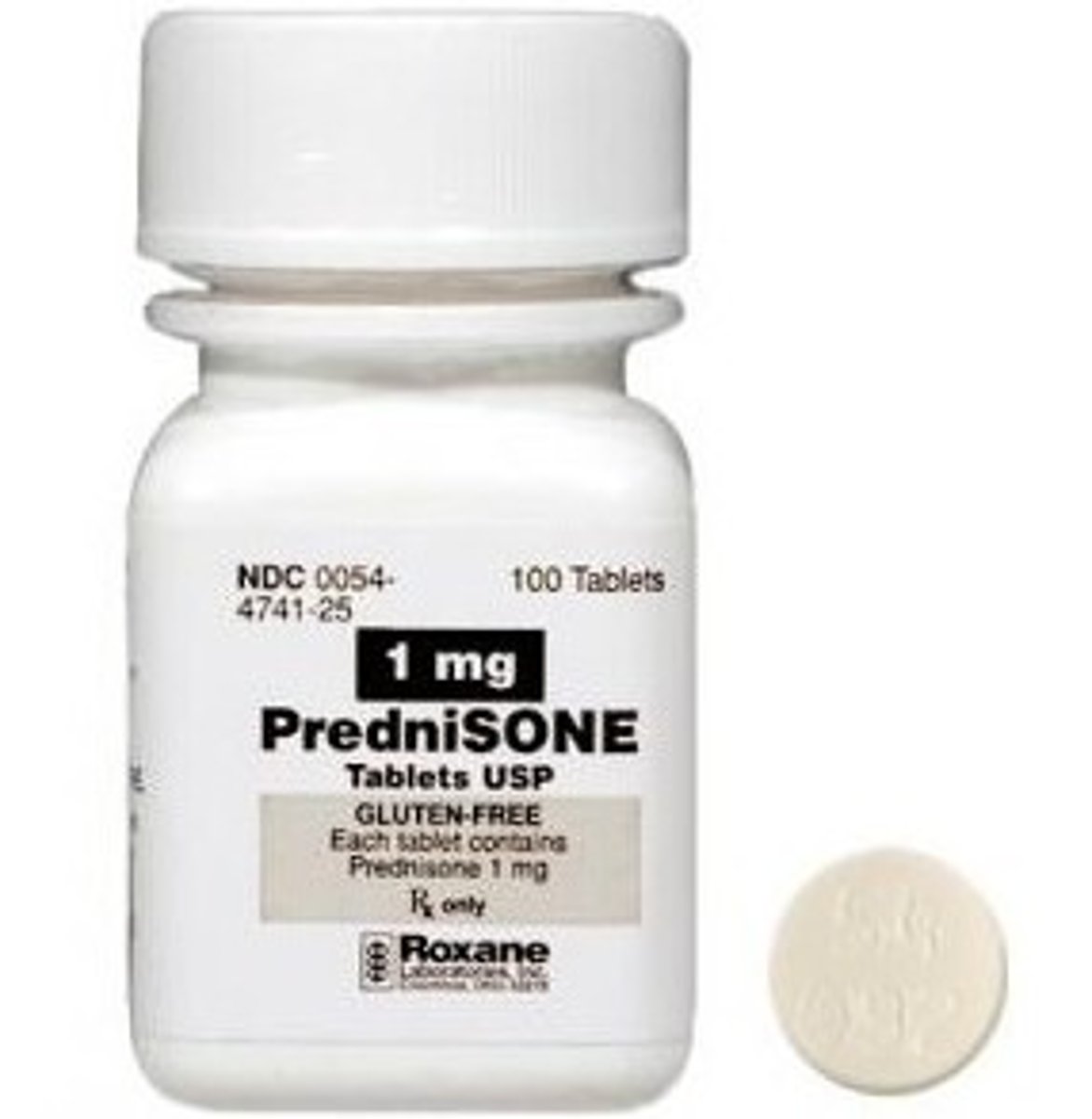
Are corticosteroids effective when given after a nerve injury has occurred?
No significant benefit shown; post-injury administration is questionable.
When is it recommended to see a patient with painful altered sensation post-implant?
As soon as possible, ideally within 24 hours.
What should be done first to assess nerve injury post-implant?
Oral exam, neurosensory testing (NST), and a panoramic radiograph
If a panoramic x-ray shows no implant-IAC contact, what is the next step?
Monitor expectantly with serial NST; no removal or repositioning needed.
What if a panoramic x-ray shows possible implant-IAC overlap?
Obtain a CT scan to determine true relationship.
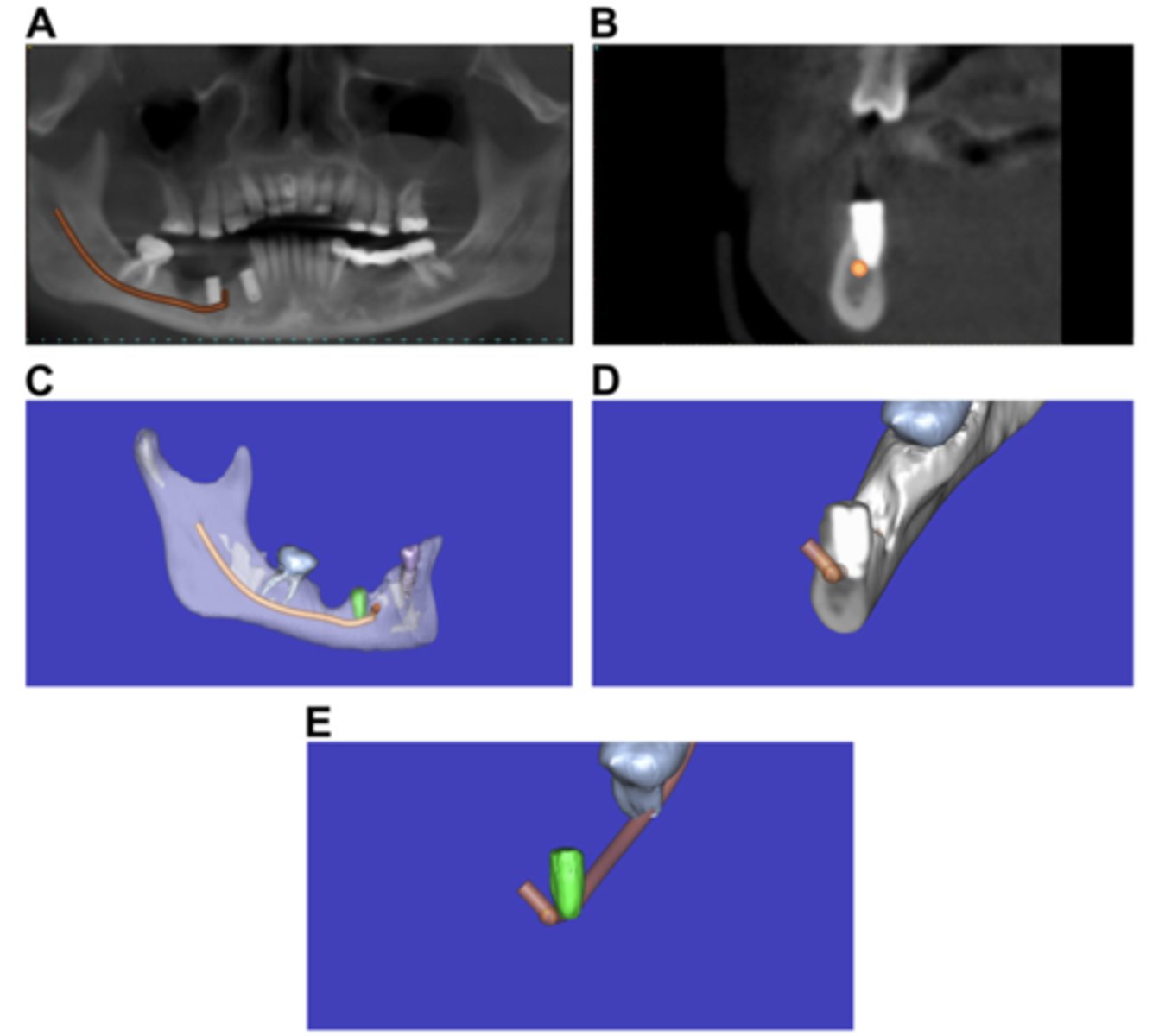
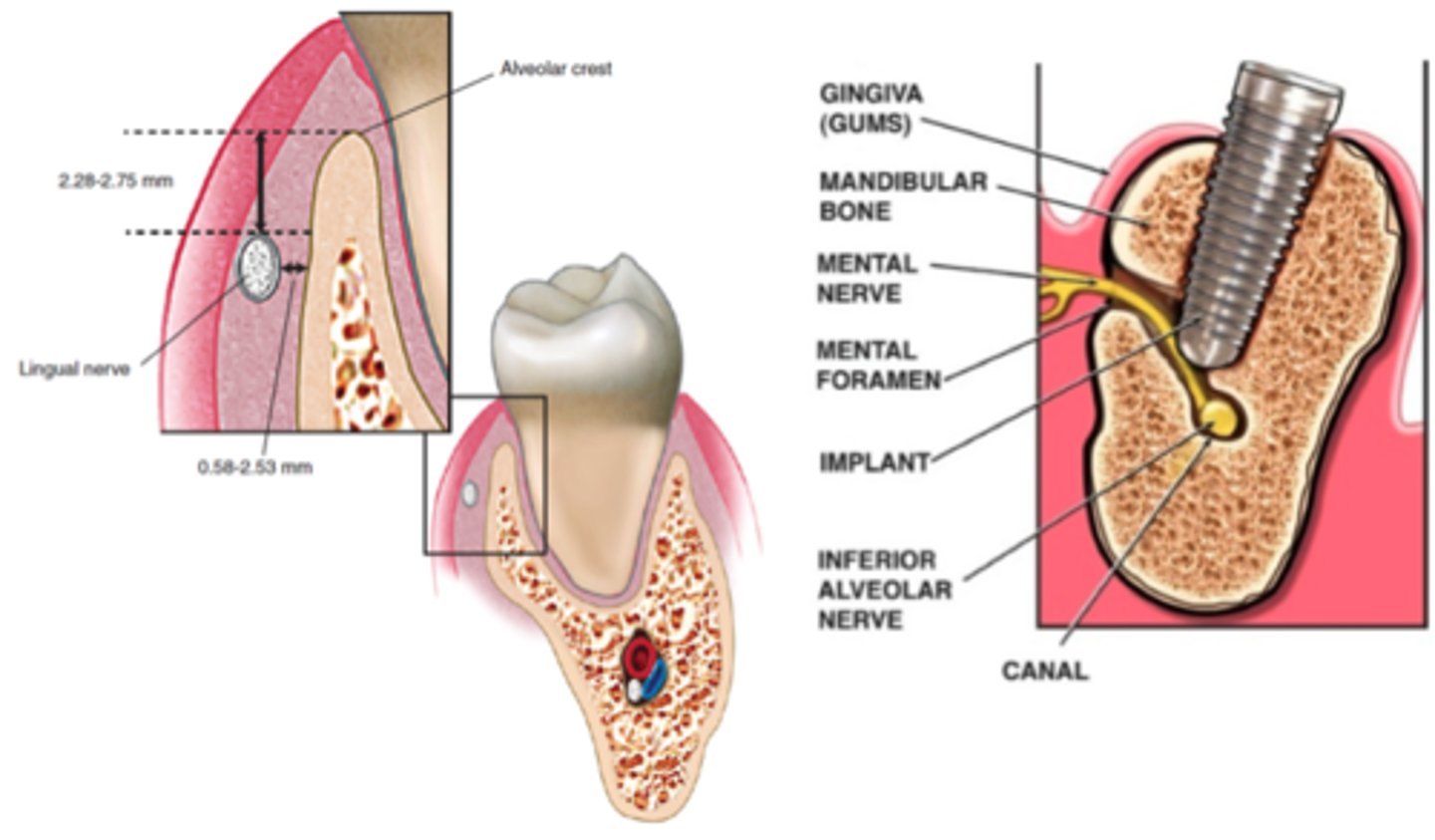
If a CT confirms implant contact with the IAC, what should be done?
Reposition or remove the implant immediately before osseointegration to create at least a 2 mm separation from the canal.
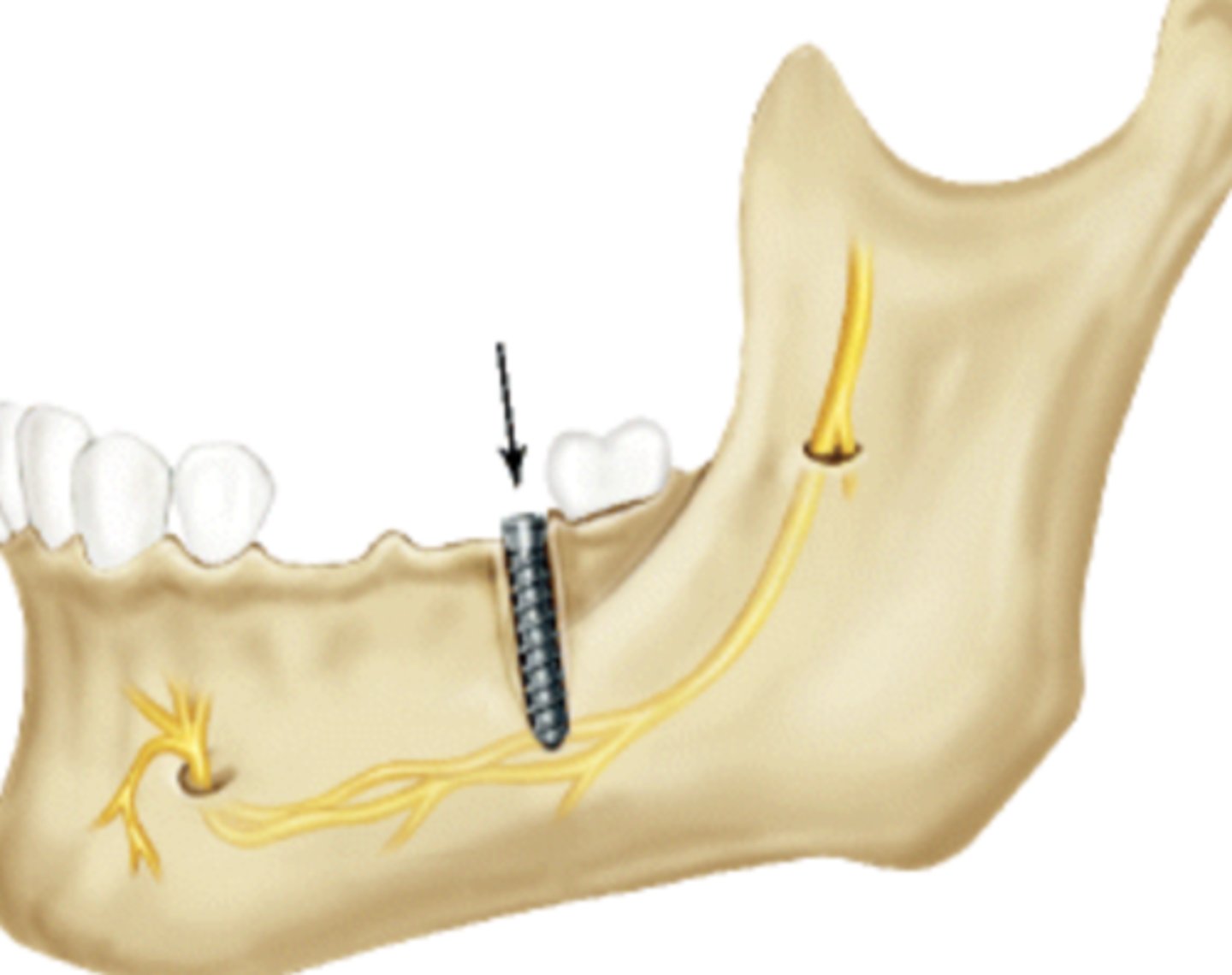
What is the minimum distance recommended between implant and IAC?
At least 2 mm of separation.
When should microsurgical consultation be considered for nerve injury?
No improvement in 3 months (anesthesia) or 4 months (hypoesthesia w/ or w/out pain)
What is the difference between anesthesia and hypoesthesia?
Anesthesia is the complete loss of sensation.
Hypoesthesia is a partial loss or reduction in sensation (numbness but not total).
What is the "12-week rule" in nerve injury management?
If total anesthesia persists beyond 3 months, surgical evaluation is indicated.
What warrants early microsurgical consult?
nerve transection i.e. direct visualization of nerve severance during surgery
What anatomical feature may allow for spontaneous recovery of the IAN after injury?
The IAN lies within a bony canal, which can guide nerve regeneration and support spontaneous recovery.
How long can patients with partial sensory recovery be monitored before making treatment decisions?
Monthly, as long as they show consistent improvement. Once progress stops, a decision must be made.
What is the typical timeline for evaluating and managing nerve injuries after implant surgery?
-Within 24 hours: Evaluate if patient reports pain or altered sensation
-0–3 months: Monitor with serial neurosensory testing (NST); many cases recover spontaneously.
-At 3 months: If anesthesia persists → refer for microsurgical consult.
-At 4 months: If hypoesthesia or pain persists → consider surgical referral.
-After 3–4 months: If there’s some improvement, continue monthly follow-up
-Stop follow-up: If no further improvement over time, spontaneous recovery is unlikely and treatment decisions should be made
What is paresthesia?
neuropathy that manifests as persistent anesthesia or an altered sensation ranging from complete numbness to burning, tingling, or continual pain

What are most oral paresthesias caused by?
direct trauma associated w/ a surgical procedure such as dental extraction or orthognathic surgery

What are possible factors that may contribute to paresthesia after nonsurgical dentistry?
-traumatic injury to the nerve via direct contact w/ the needle
-hemorrhage into the nerve sheath
-hydrostatic pressure from injection
-neurotoxicity from local anesthetic itself
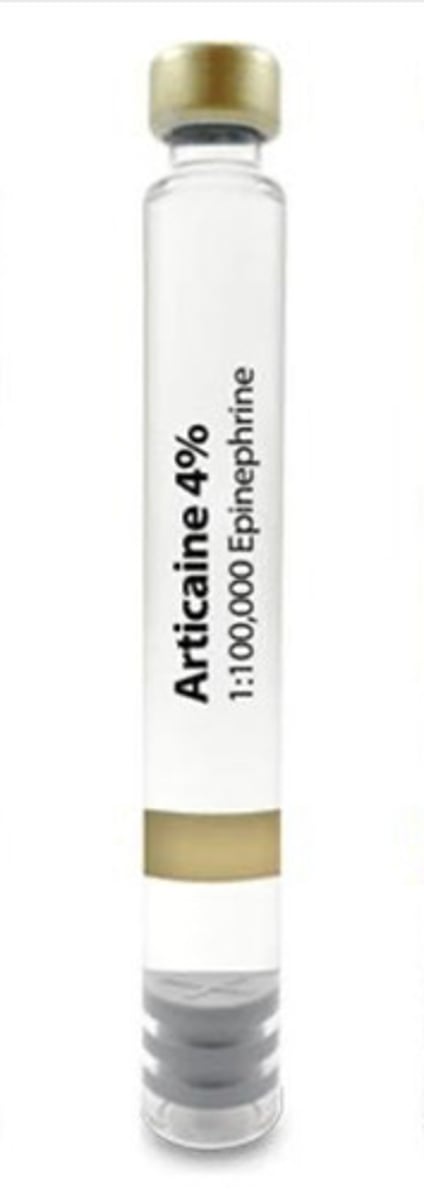
What did investigators in Canada find regarding nonsurgical paresthesia statistics across three studies spanned from 1973 to 2008?
-overall incidence of paresthesia was 1:785,000 with two drugs most often implicated being 4% prilocaine and 4% articaine
-# of annual cases of paresthesia increased beginning in 1985 shortly after the intro of articaine into the canadian market
-lingual nerve was affected in ~70% of all cases

Which local anesthetic was most frequently associated with permanent paresthesia in a northern California study before articaine's release in the U.S.?
4% prilocaine

How did paresthesia reports of 4% articaine and 2% lidocaine compare to 4% prilocaine in northern California studies?
on the basis of their estimated use:
-Articaine and lidocaine: proportional/lower to usage
-prilocaine had more reports than expected

What local anesthetic involved 88% of nerve injury reports in Denmark?
articaine - with lingual nerve involved in 78% of cases
What was the purpose of U.S. study regarding occurrence of paresthesia after dental local anesthetic administration?
As studies had been done in Ontario, Denmark and northern California, they wanted to determine if the type of local anesthetic affected reports of paresthesia in the U.S.
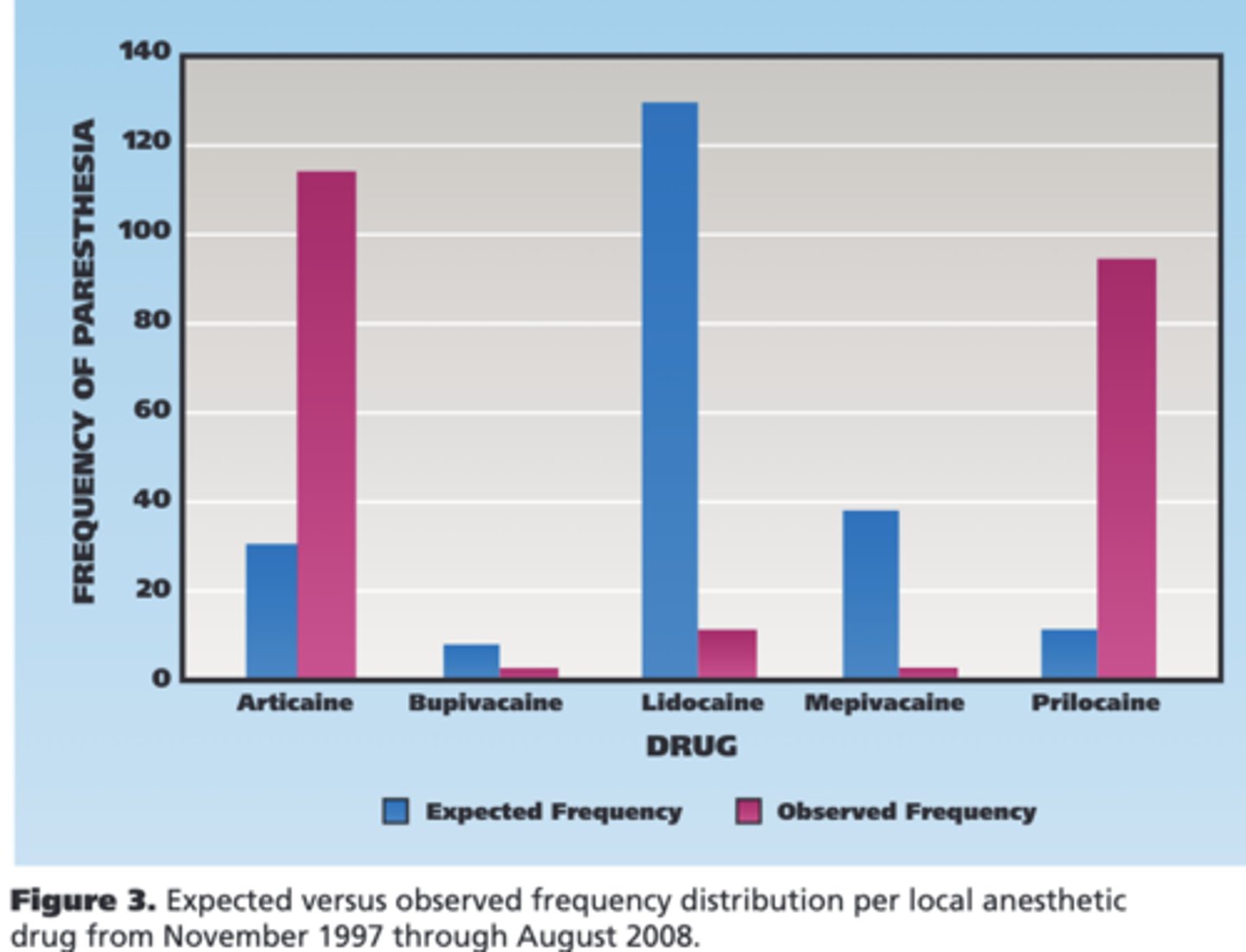
How was the U.S. study regarding occurrence of paresthesia after dental local anesthetic administration conducted?
By retrospectively analyzing nonsurgical paresthesia cases reported to the FDA from November 1997 to August 2008
How was the U.S. study on local anesthetic-related paresthesia conducted?
-analyzed FDA Adverse Event Reporting System data from 1997-2008
-Included non-surgical U.S. cases involving oral paresthesia from articaine, bupivacaine, lidocaine, mepivacaine, or prilocaine
-Excluded surgical procedures and outdated drugs
-Data analyzed included nerve involved, symptoms, anesthetic used, and resolution
-χ² and binomial tests were used to compare reported vs. expected cases based on anesthetic sales.
Which local anesthetic had the most frequently reported paresthesia before 2000?
4% prilocaine
Which local anesthetic became most frequently reported for paresthesia after 2000?
Articaine
What did χ² analysis show about articaine and prilocaine in relation to reported paresthesia cases?
Both were associated with significantly more cases than expected based on market share
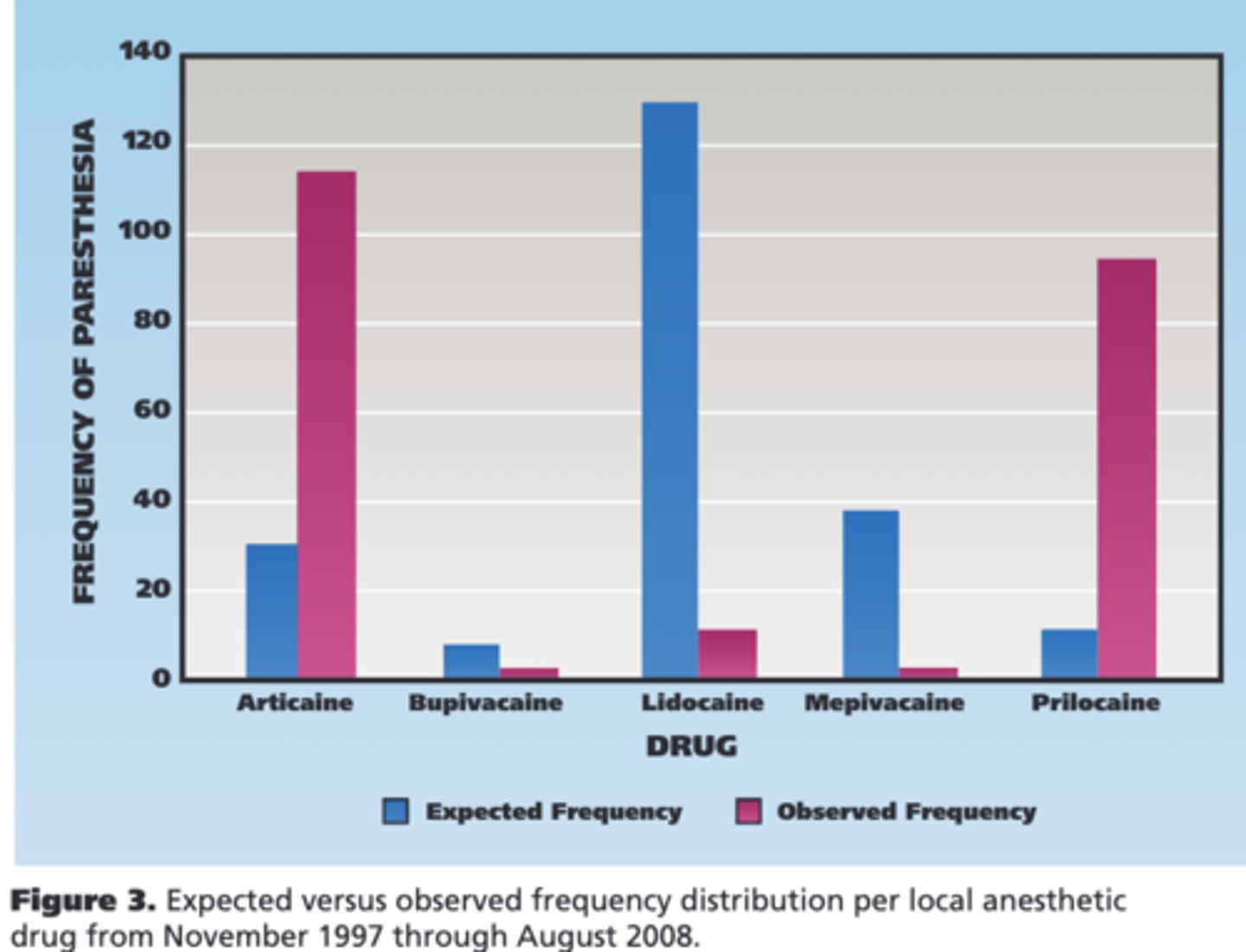
How many times more than expected were paresthesia cases reported for prilocaine and articaine?
-Prilocaine: 7.3× more
-Articaine: 3.6× more
What was the overall reported incidence of paresthesia across all drugs in the US study?
1 in 13,800,970
What was the mean age and age range of patients with paresthesia?
Mean age: 41.9 years; range: 15–78 years -> with Patients in their 30s, 40s, and 50s most affected by paresthesia
What was the sex distribution among reported paresthesia cases?
61% female, 39% male
What injection technique was used in most paresthesia cases?
Mandibular nerve block (94.5%).
Which dental arch was most affected by paresthesia?
Mandibular arch (95.1%)
Which nerve was most commonly affected in paresthesia reports?
Lingual nerve (tongue affected in 170 of 191 cases).
What symptoms were commonly reported along with paresthesia?
Taste disturbance: 17.7% (44 cases)
Dysesthesia: 21.8% (54 cases)

What event during injection may indicate direct nerve contact?
Positive aspiration of blood or electric shock sensation.
What was the most common type of nonsurgical dental procedure associated with paresthesia?
Restorative dentistry (74.2% of known procedures).
What was the range of duration for reported oral paresthesia?
From 1 day to 736 days
How many paresthesia cases were confirmed to fully resolve?
34 out of 108 cases - Of these resolved paresthesia cases, 25 cases resolved within 2 months
What key finding does this study confirm about articaine and prilocaine?
It confirms that 4% articaine and 4% prilocaine are associated with a higher risk of paresthesia, consistent with studies from Canada and Denmark.
What is unique about articaine and prilocaine compared to other dental anesthetics in the U.S.?
They are the only anesthetics formulated as 4% solutions, while others are lower concentration (e.g., lidocaine 2%, bupivacaine 0.5%).
Why might the lingual nerve be more prone to injury than the inferior alveolar nerve?
It is often unifascicular, making it more vulnerable to damage, whereas the IAN is multifascicular.
What is a possible cause of nerve damage after anesthetic injection, according to the study?
A combination of minor needle trauma and dose-dependent neurotoxicity of the anesthetic.