CPR and First Aid
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
how to recognize an emergency
look for unusual noises, sights, odors, appearances and behaviors
example: screams, breaking glass, crashing metal

safety
do not risk your own _________________ in orer to rescue or provide first aid to another person

Good Samaritan Laws
state laws that help protect healthcare professionals and ordinary citizens from liability while giving emergency care to accident victims. You are protected if you are certified and obtain consent, act in good faith, are not paid, use reasonable skill and care, are not negligent (careless), and do not abandon the person

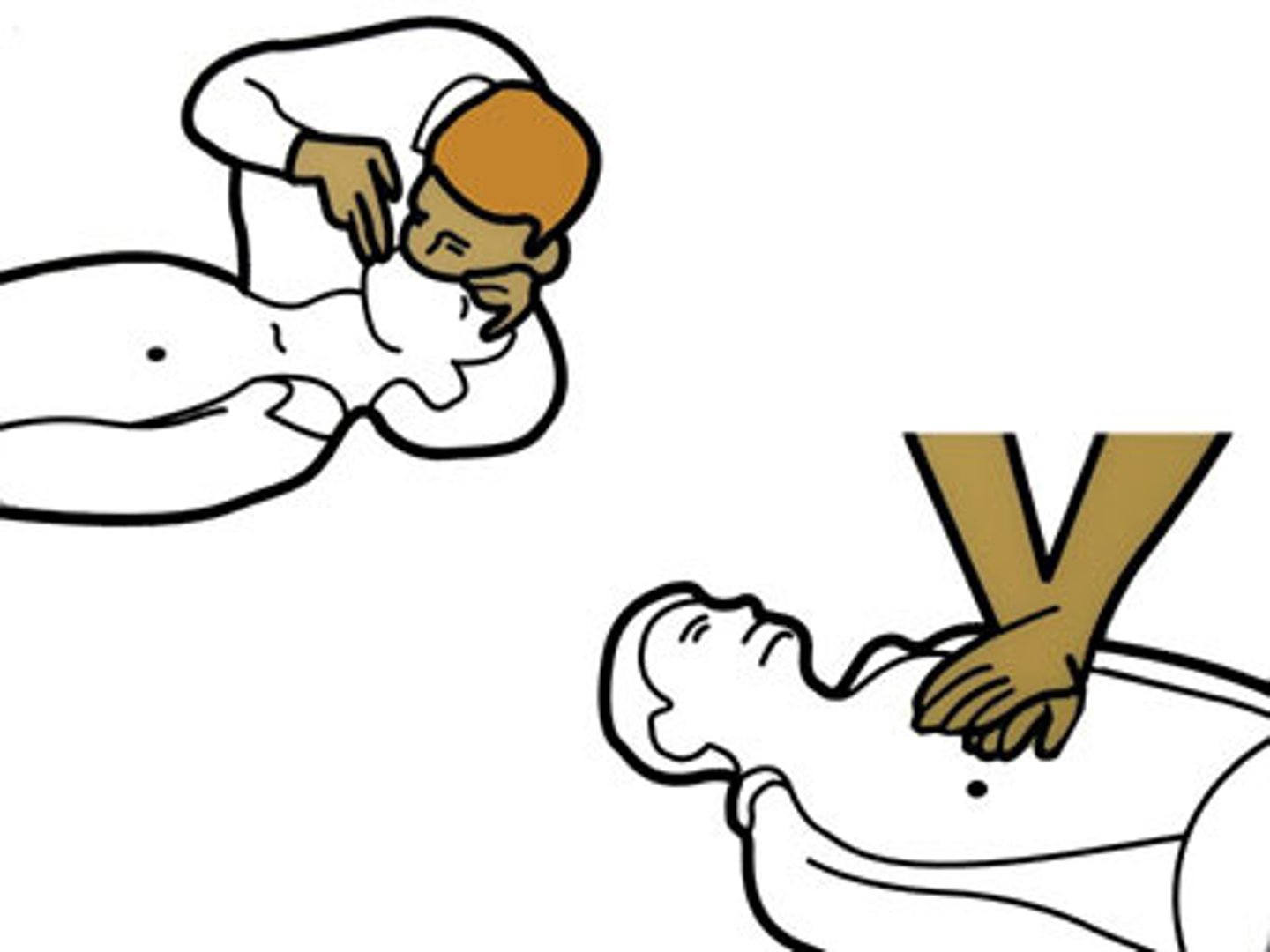
how to open an Airway
tilt head, lift chin

signs of life
movement or breathing
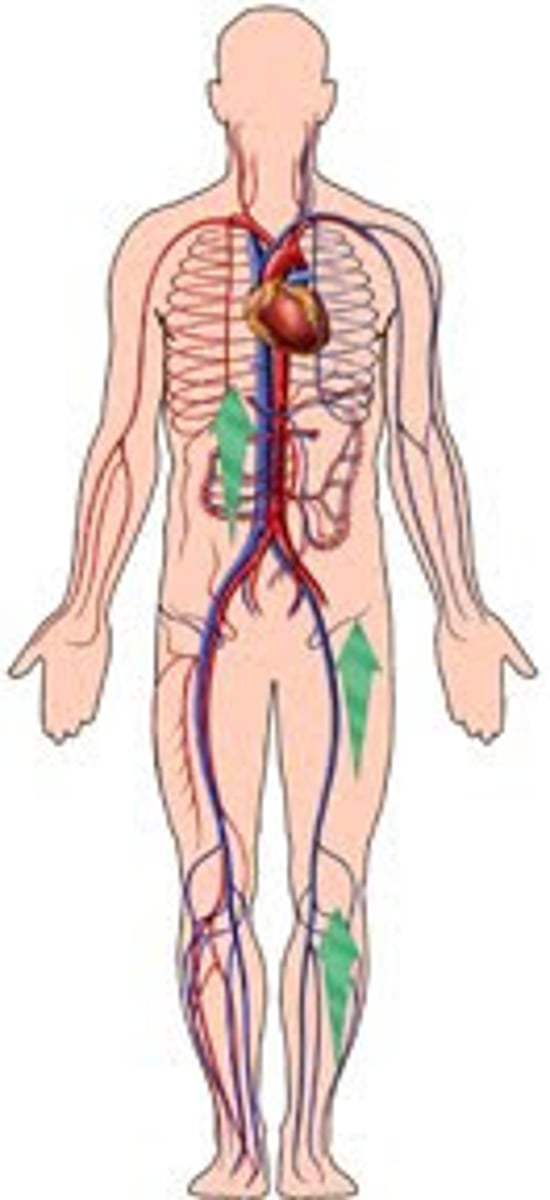
ABCs
Airway, Breathing, and Circulation (blood flowing through the body)

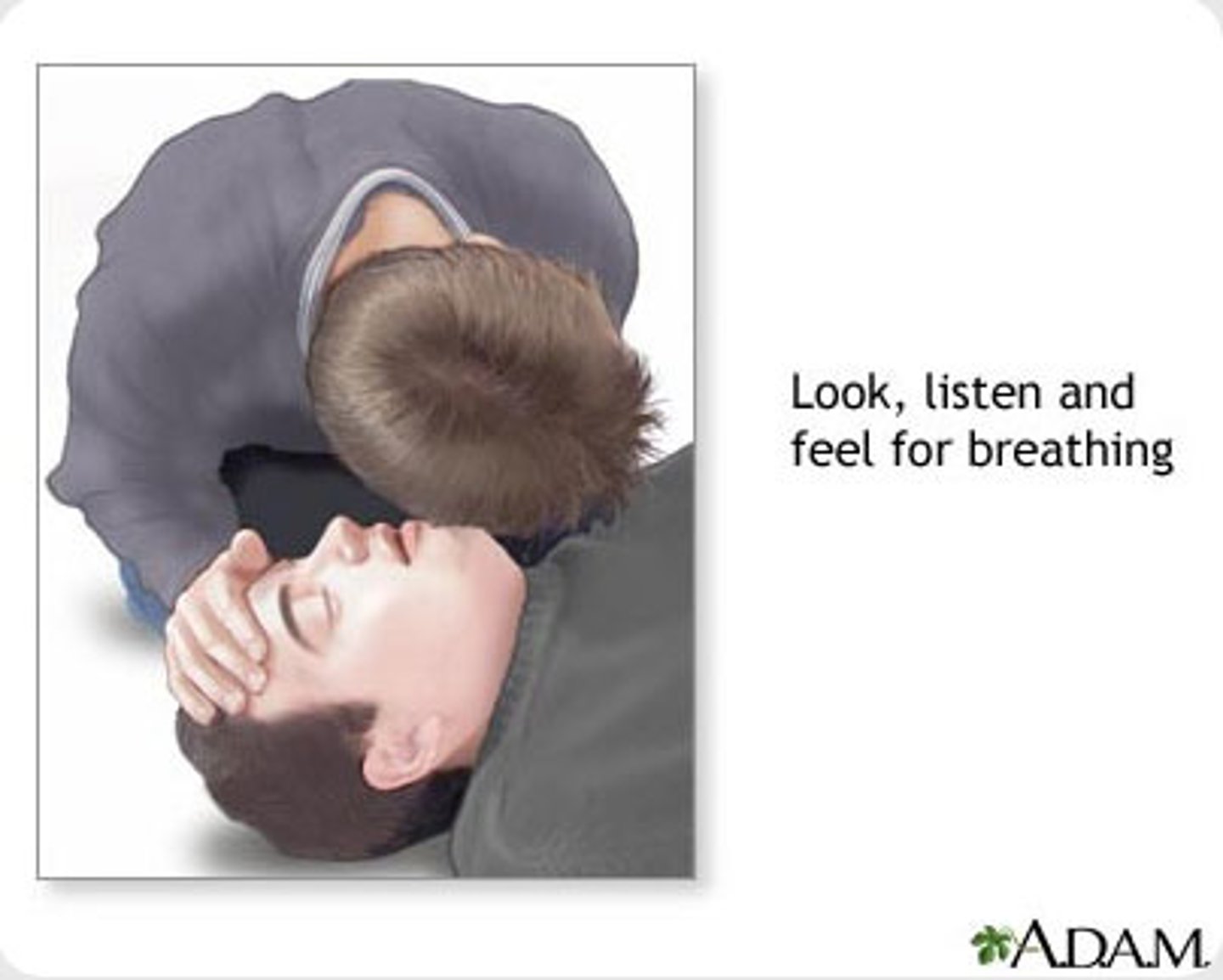
How to check Breathing
look for movement of the chest, listen and feel for air movement by placing your ear and then your cheek at the mouth and nose of the victim
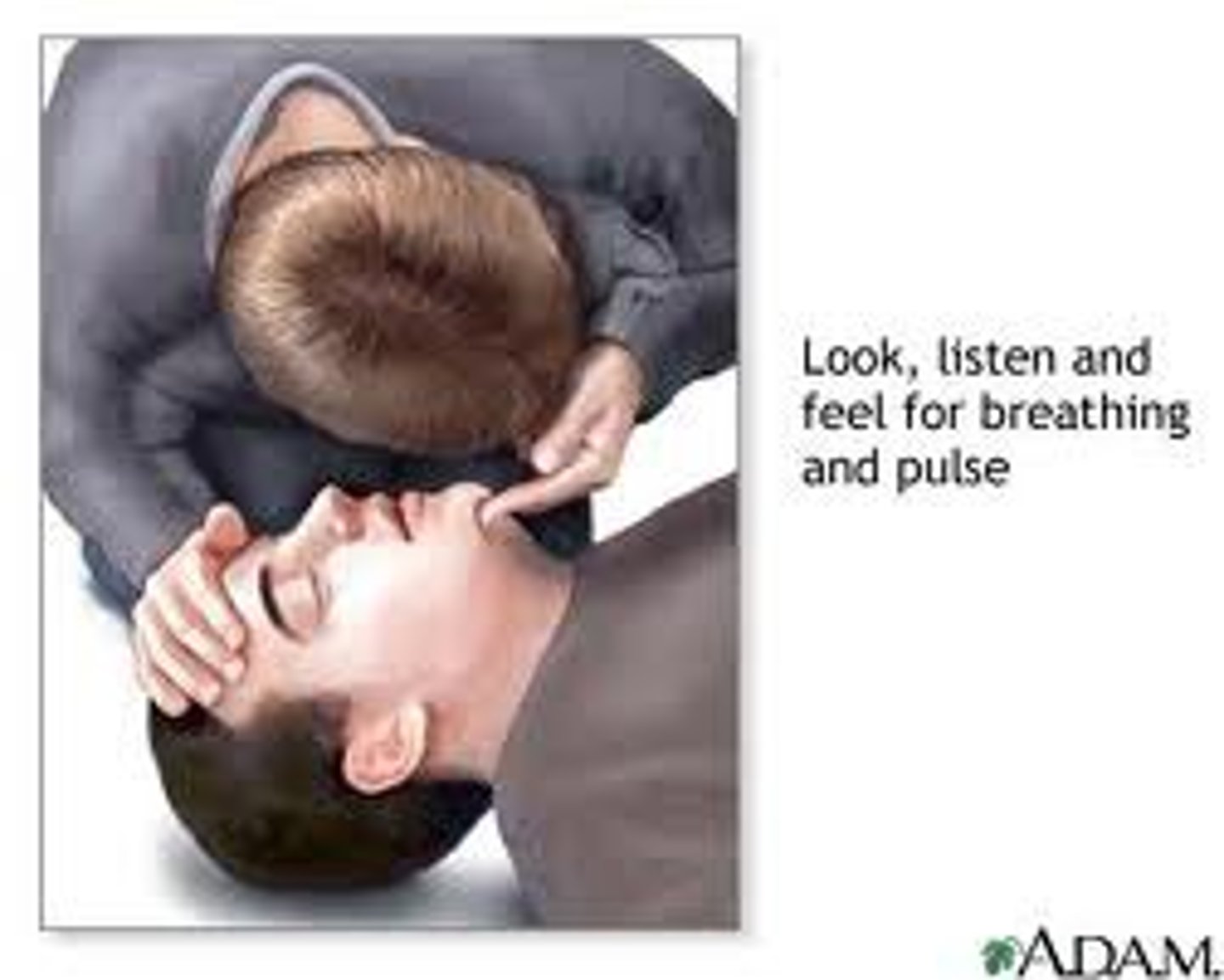
how to check Circulation
place your index and middle fingers into the groove of the neck next to the voice box to feel the carotid artery pulse
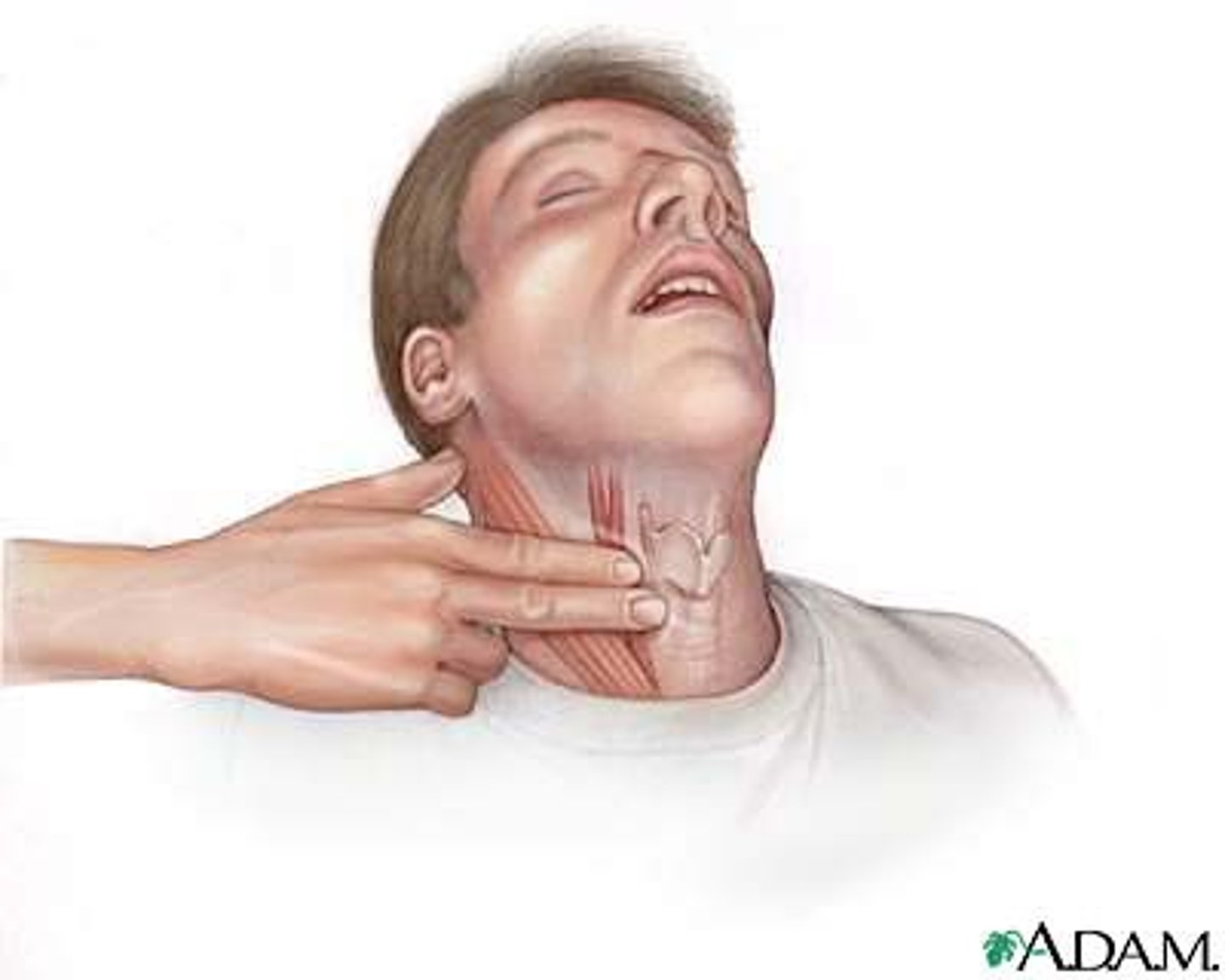
index finger
the finger next to the thumb; also called pointer finger

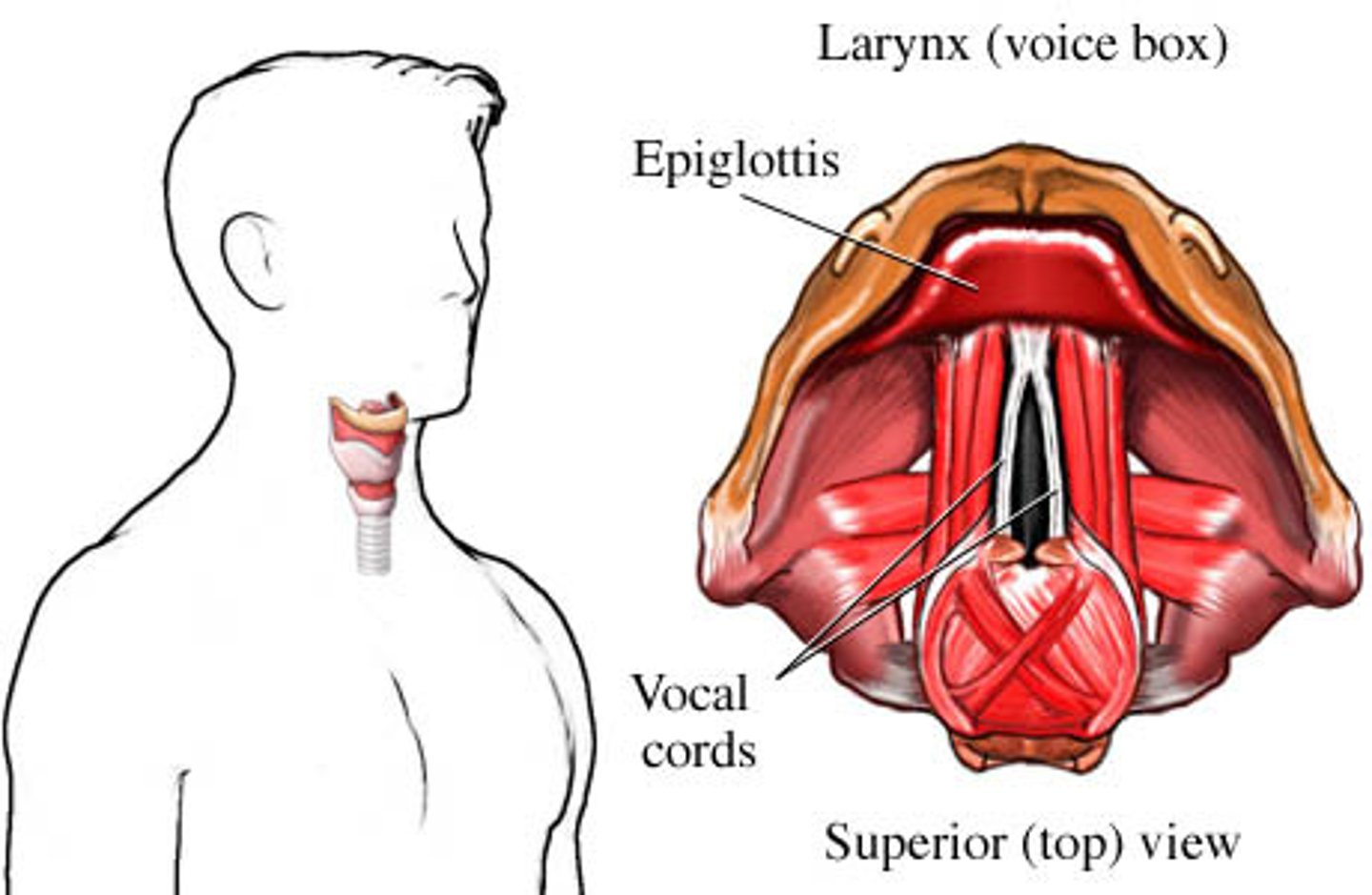
voice box
larynx
Rescue Breathing
an emergency technique in which a rescuer gives air to someone who is not breathing. To perform this, a person blows air into a victim's lungs to give him/her oxygen

how to give rescue breaths to an adult
1. tilt head, lift chin, pinch the nose shut
2. take a breath and make a complete seal over the person's mouth
3. blow in to make chest clearly rise (1 second)
4. Begin CPR/administer AED if breaths go in OR assume unconscious choking if breaths do NOT go in
Steps to check an injured child or infant
1. check scene, then check child
2. obtain consent from parent/guardian if present
3. Tap on shoulder and shout, "Are you okay?"
4. No response, call 911 or if alone, give 2 minutes of care then call 911
5. Open airway, check for signs of life for no more than 10 seconds
6. give 2 rescue breaths if not breathing
7. If breaths go in, check for pulse and severe bleeding. If breaths do NOT go in, begin rescue breathing. No pulse, begin CPR/AED
8. If breathing, place in recovery position and monitor ABCs

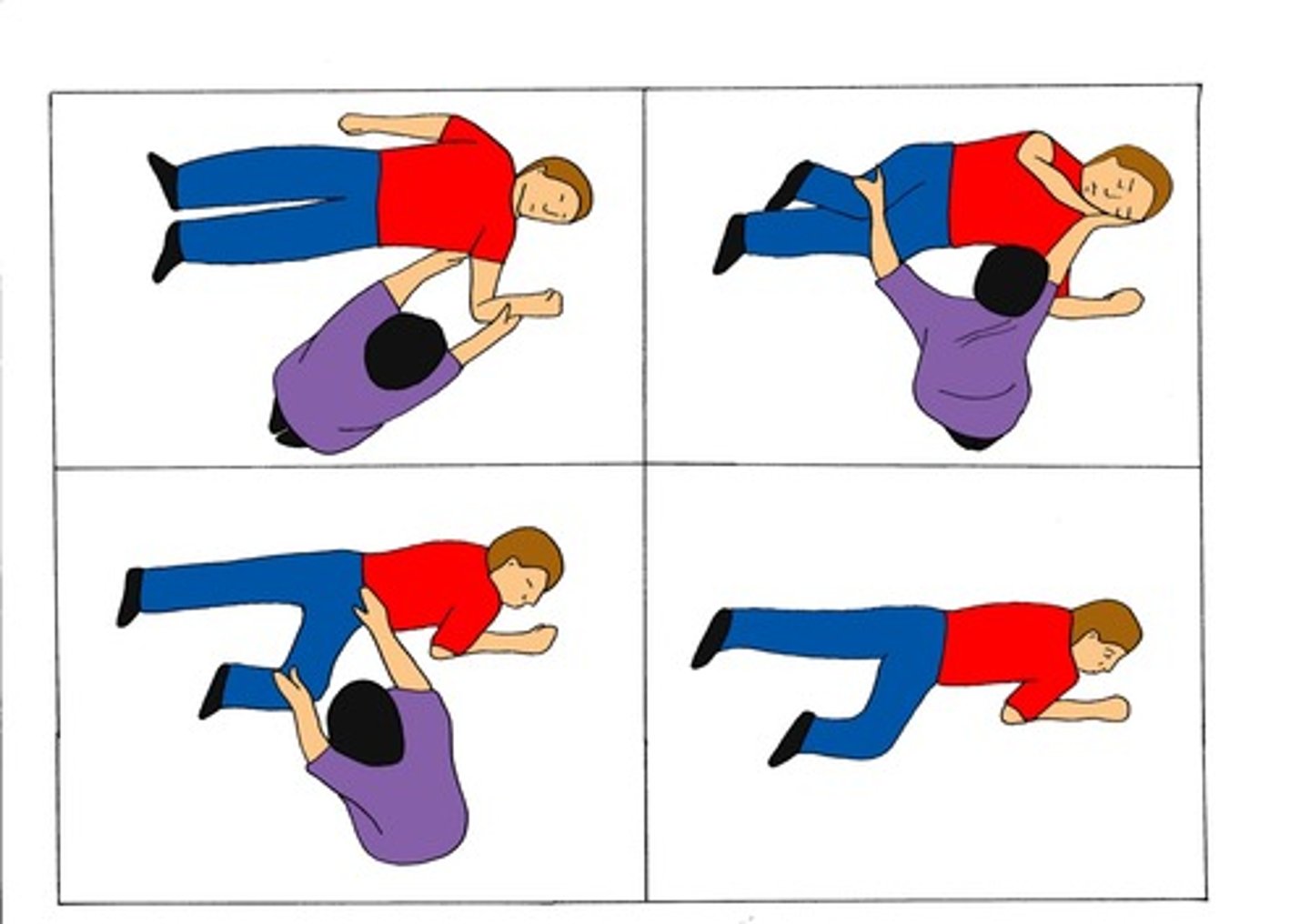
recovery position
a side-lying position used to maintain a clear airway in unconscious patients without injuries who are breathing adequately
Rescue Breathing for Child/Infant (Age 1-12)
1. give 1 rescue breath (for about 1 second) every 3 seconds, pinch nose shut, make seal over child's mouth and nose (infant), blow in to make chest clearly rise
2. After 2 minutes, recheck signs of life and pulse for no more than 10 signs
3. If pulse, but no breathing, continue. If NO pulse, begin CPR/Administer AED

unconscious choking/ no breaths go in
tilt head farther back, give 2 rescue breaths, if chest does not rise, give 30 chest compressions; look for an object and remove it if seen; try 2 rescue breaths; continue these steps if breath does NOT go in. If breaths DO go in, check for signs of life and give care.

conscious choking
victim can't cough, speak, cry or breath
1. check scene, check person
2. Have someone call 911
3. obtain consent
4. lean person forward, give 5 back blows with heel of your hand
5. give 5 quick, upward abdominal thrusts (or chest thrusts for infants, pregnant or obese people)
6. continue back blows and abdominal thrusts until object is forced out, the person can breathe or cough forcefully, OR the person becomes unconscious

two
number of fingers used in chest compressions for infant

abdominal thrusts
the act of applying pressure to a choking person's stomach to force an object out of the throat

choking when you are alone
1. self-administer abdominal thrusts
2. place your fist above your navel (belly button)
3. cover your fist with your hand and thrust upward and inward
4. lean over the back of a chair, table or other firm object and quickly press your abdomen upward and inward

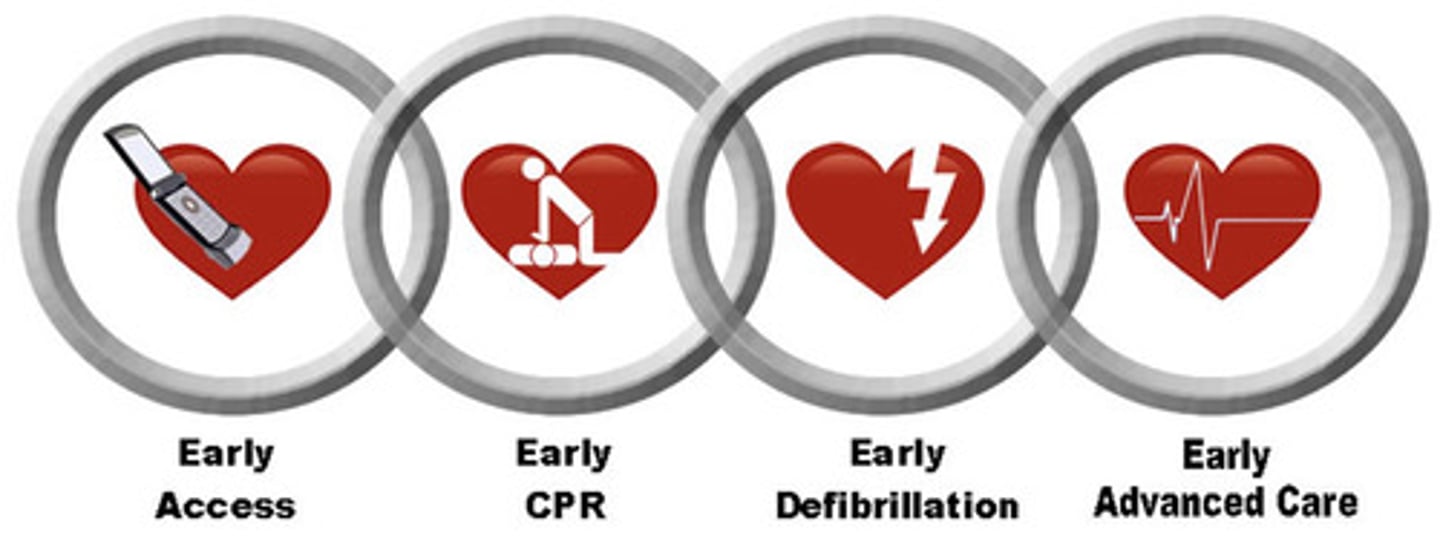
Cardiopulmonary Resuscitation (CPR)
life saving technique that combines rescue breathing and chest compressions

compressions
techniques that allow the rescuer to artificially pump the heart, delivering blood to the body and bringing oxygen to the lungs

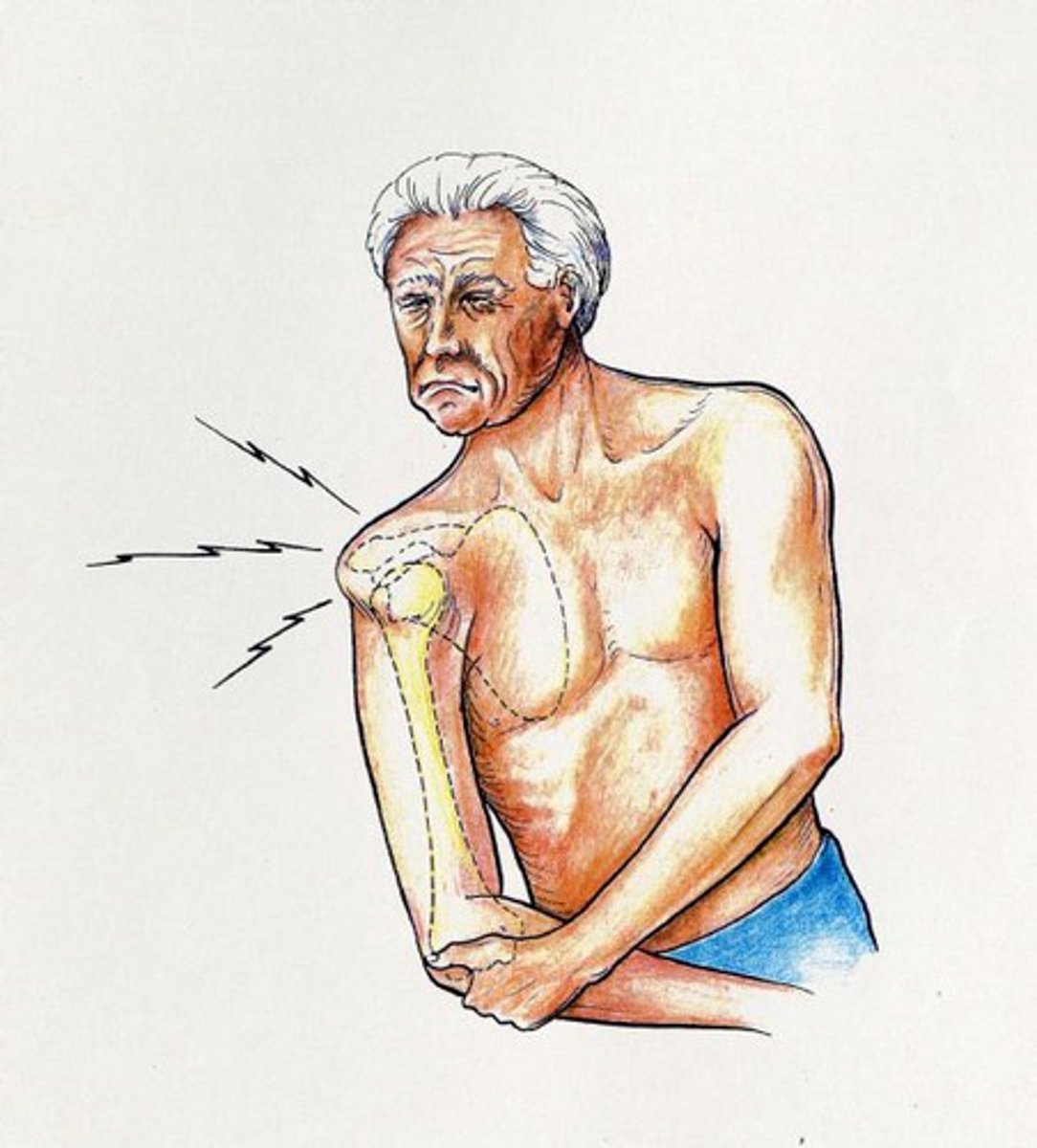
heart attack
when an area of the heart muscle suffers damage and loses function due to lack of oxygen. The heart stops beating
cardiac arrest
when the heart stops beating due to stroke, severe injuries, electrical shock, drug overdose, chest trauma, drowning or suffocation. Leads to unconsciousness, no pulse, no signs of circulation
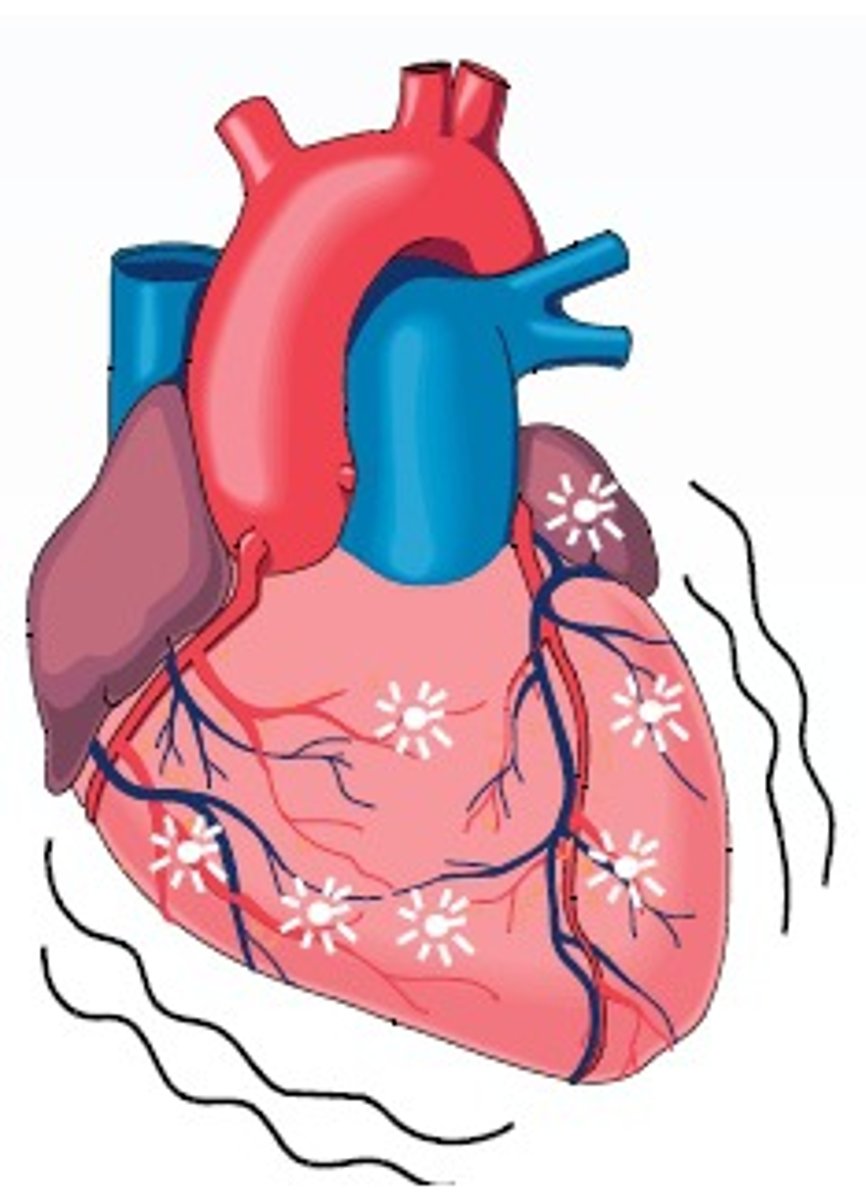
signs of circulation
consciousness, a pulse, pink nail beds, warm skin
If a person does not have these, they are in cardiac arrest
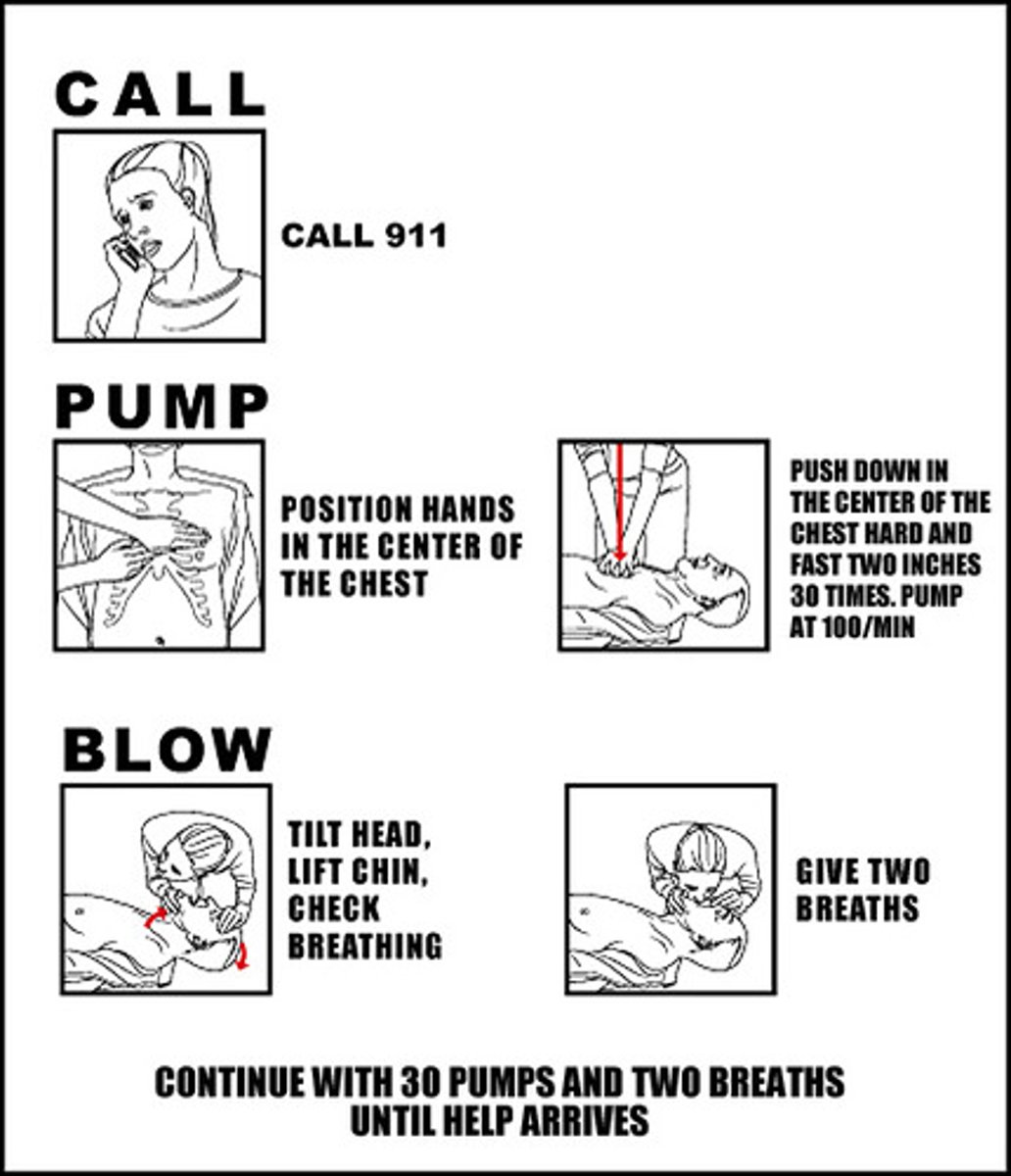
Adult CPR
1. give 30 chest compressions and 2 rescue breaths
2. continue until scene becomes unsafe, you see a sign of life, AED is ready to use, you are too exhausted, or another trained responder arrives and takes over

Adult CPR skills >12 years old
hand position: 2 hands in center of chest
compression depth: 1 1/2 - 2 inches
cycle: 30 compressions, 2 breaths
rate: 30 compressions in 18 seconds or 100 per minute
Child CPR skills (1-12 years old)
hand position: 1 or 2 hands in center of chest
compression: 1-1 1/2 inches
cycle: 30 compressions, 2 breaths
rate: 30 compressions in 18 seconds

Infant CPR skills <1 year old
hand position: 2 or 3 fingers on lower half of chest, one finger width below nipple line
compression depth: 1/2 - 1 inch
cycle: 30 compressions, 2 breaths
rate: 30 compressions in 18 seconds

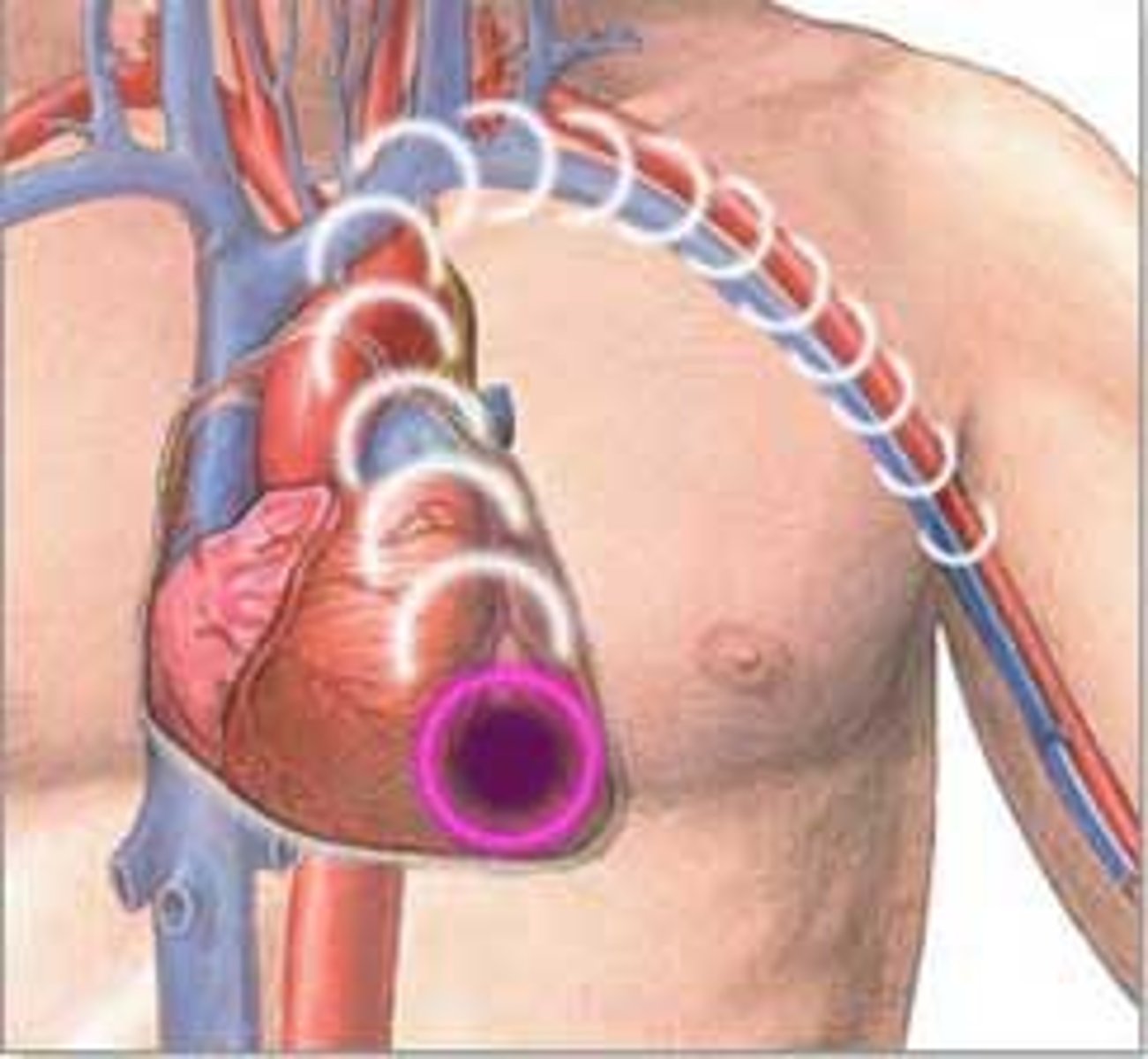
Automatic External Defibrillators (AEDs)
portable defibrillators that are available in many public areas. The machine first determines if the victim needs a shock. If shock is needed, the machine talks the rescuer through administering the procedure

defibrillation
shocking the heart back into beating again by delivering an electric current to the heart which will, in turn, return the heart to a regular rhythm
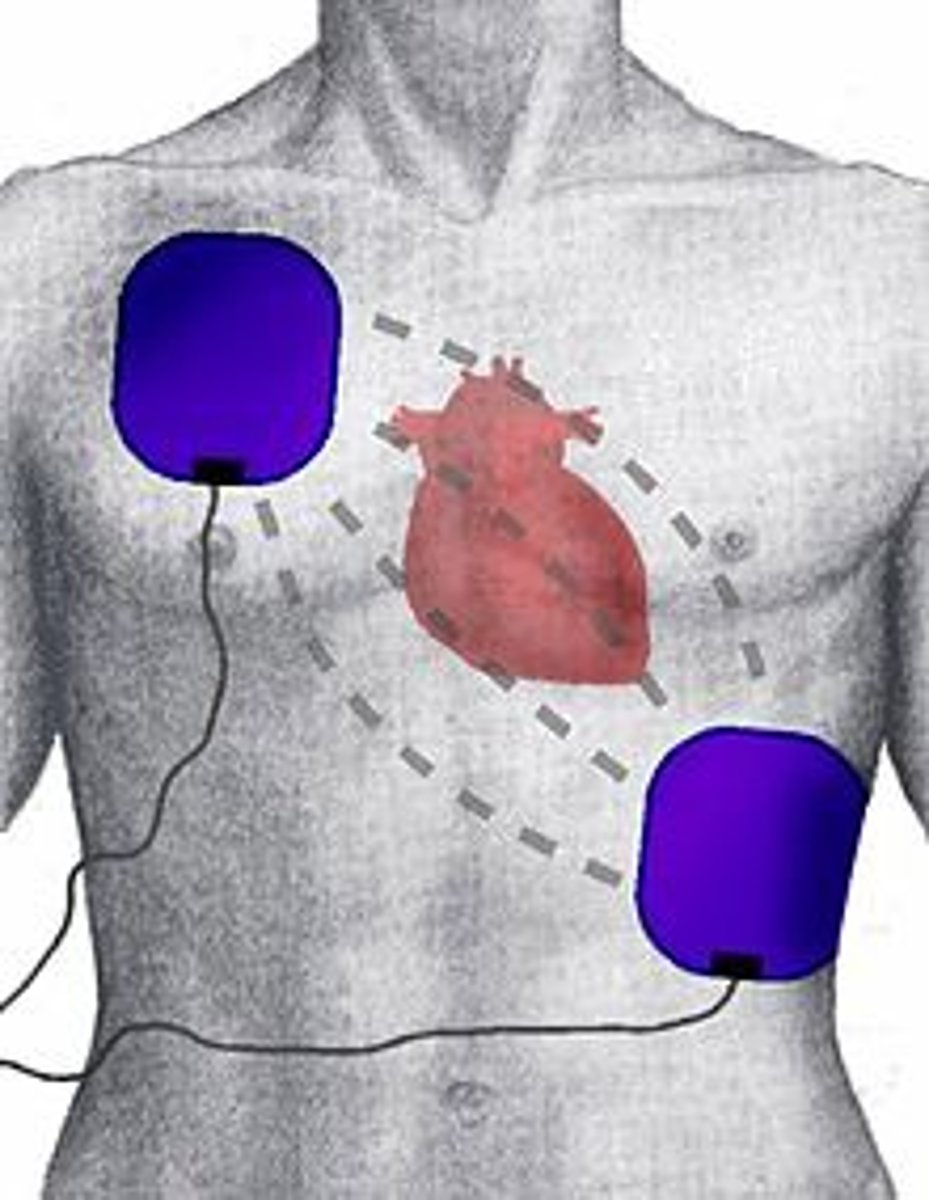
survival rate with AED
30% or higher, according to the American Red Cross, if used within minutes after cardiac arrest
wound
a break or tear in the soft tissue of the body

puncture
when skin is pierced with a pointed object

caring for minor wounds
1. wash hands, put on disposable gloves if available
2. place sterile or clean cloth on wound and apply direct pressure
3. Rinse wound with water and gently wash
4. Seek medical help if you can't remove dirt or debris from the wound. Apply antibacterial ointment
5. Cover wound with sterile dressing and bandage. Change dressing at least once a day, keeping wound clean and dry. Seek medical help if wound becomes infected--tender, swollen and red

caring for serious wounds with severe bleeding
1. seek medical help immediately, protect yourself from blood by wearing disposable gloves
2. lay victim down, elevate feet and legs. Place in half-seated position if a head wound
3. find the wound by following the blood. Uncover wound if under clothing
4 place dressing over wound and apply direct pressure
5. raise wound above level of heart and continue to apply direct pressure if arm or leg is wounded
6. apply pressure at pressure point if bleeding continues
7. release pressure point and secure with bandage when bleeding stops. Do not remove dressings

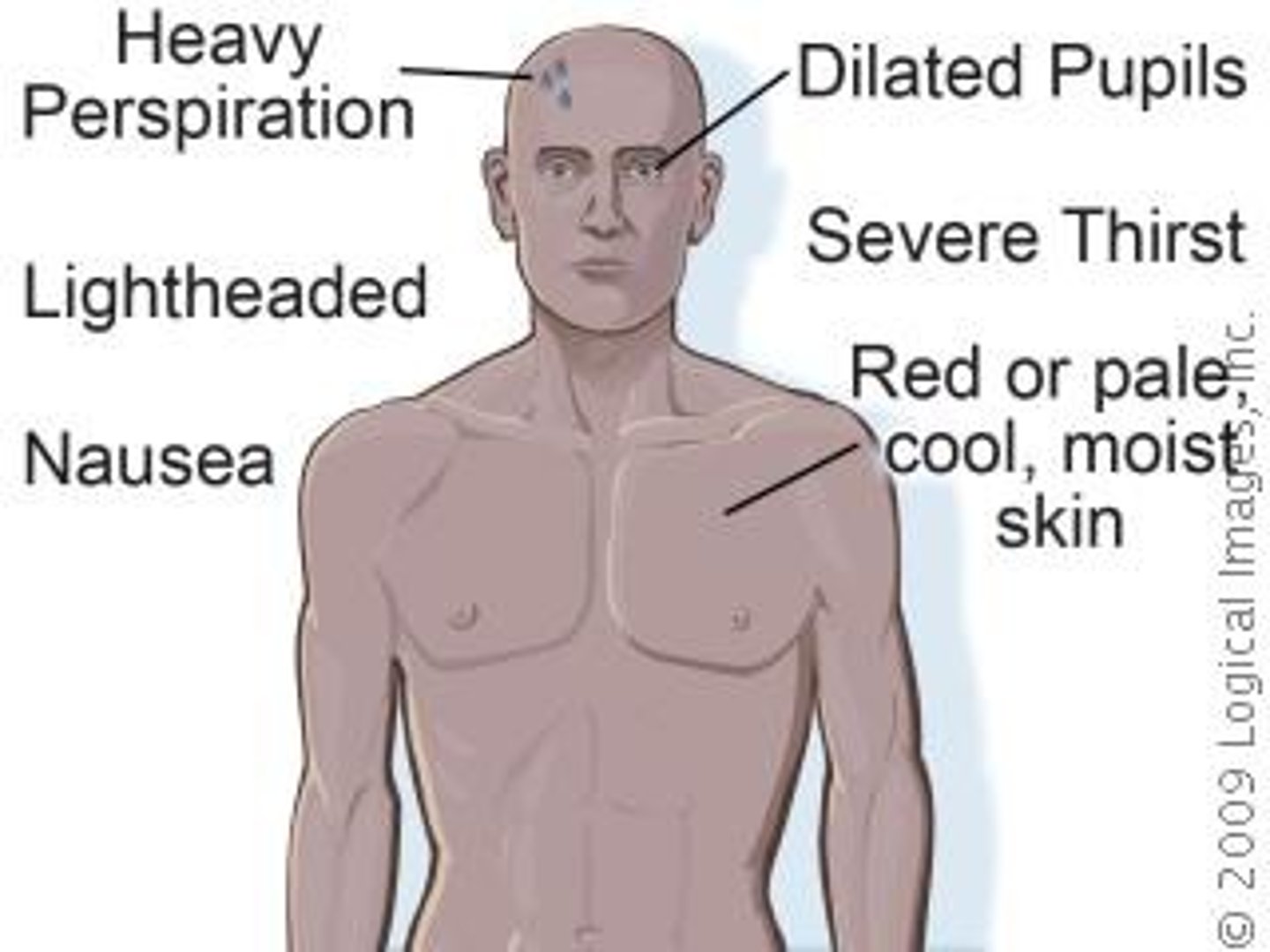
shock
a condition in which some body organs are not getting enough oxygenated blood. It may occur when heart is not pumping properly, a considerable amount of blood is lost from the body hemorrhaging, dehydration or a systemic infection, or when the nervous system is damaged by injury or drugs

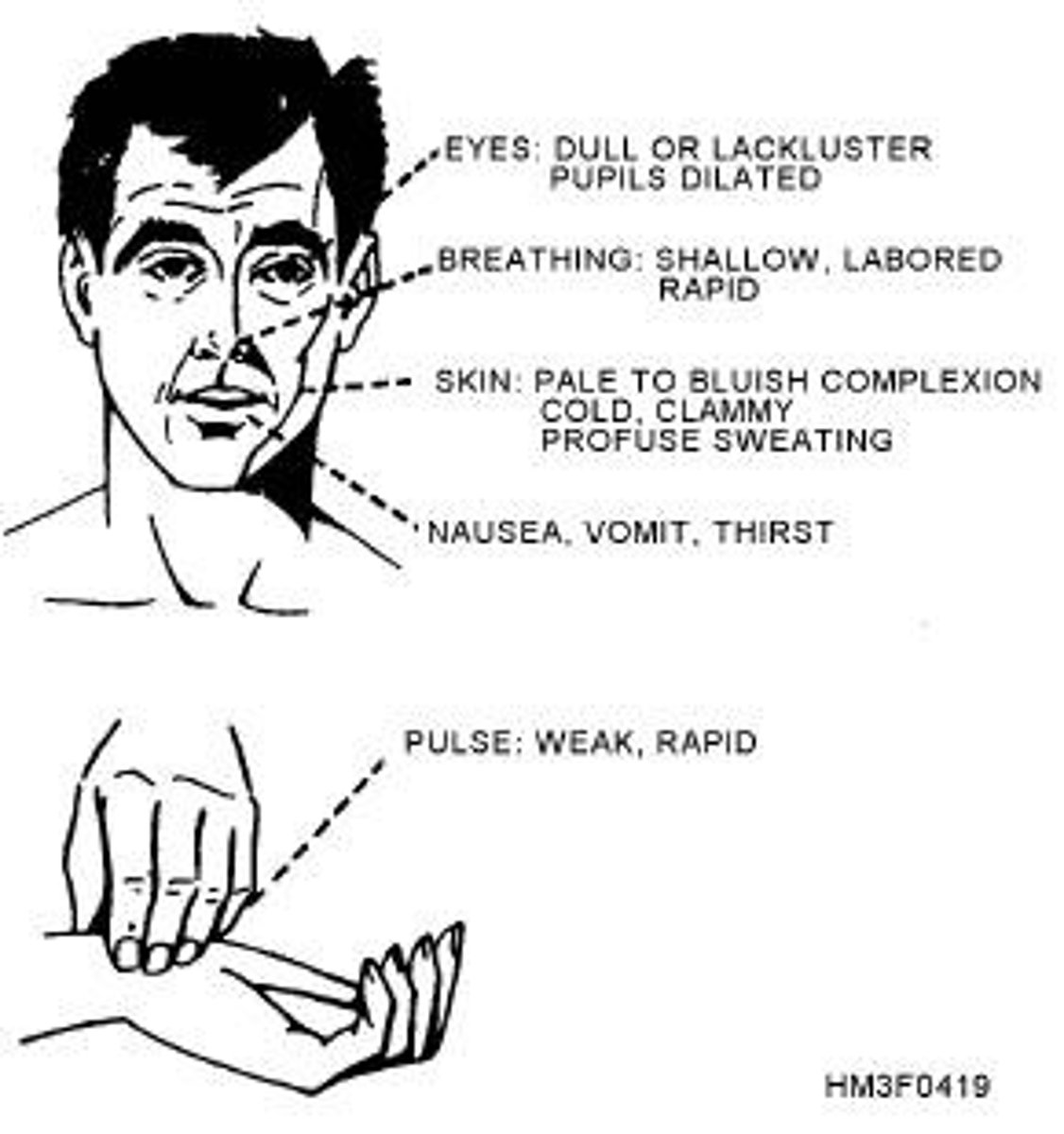
symptoms of shock
anxious, restless, lethargic (slow-moving), unconscious, pale and cold skin, nauseous or vomiting, increased pulse and respiration rates, bluish tinge to skin, thirsty, dilated (enlarged) pupils
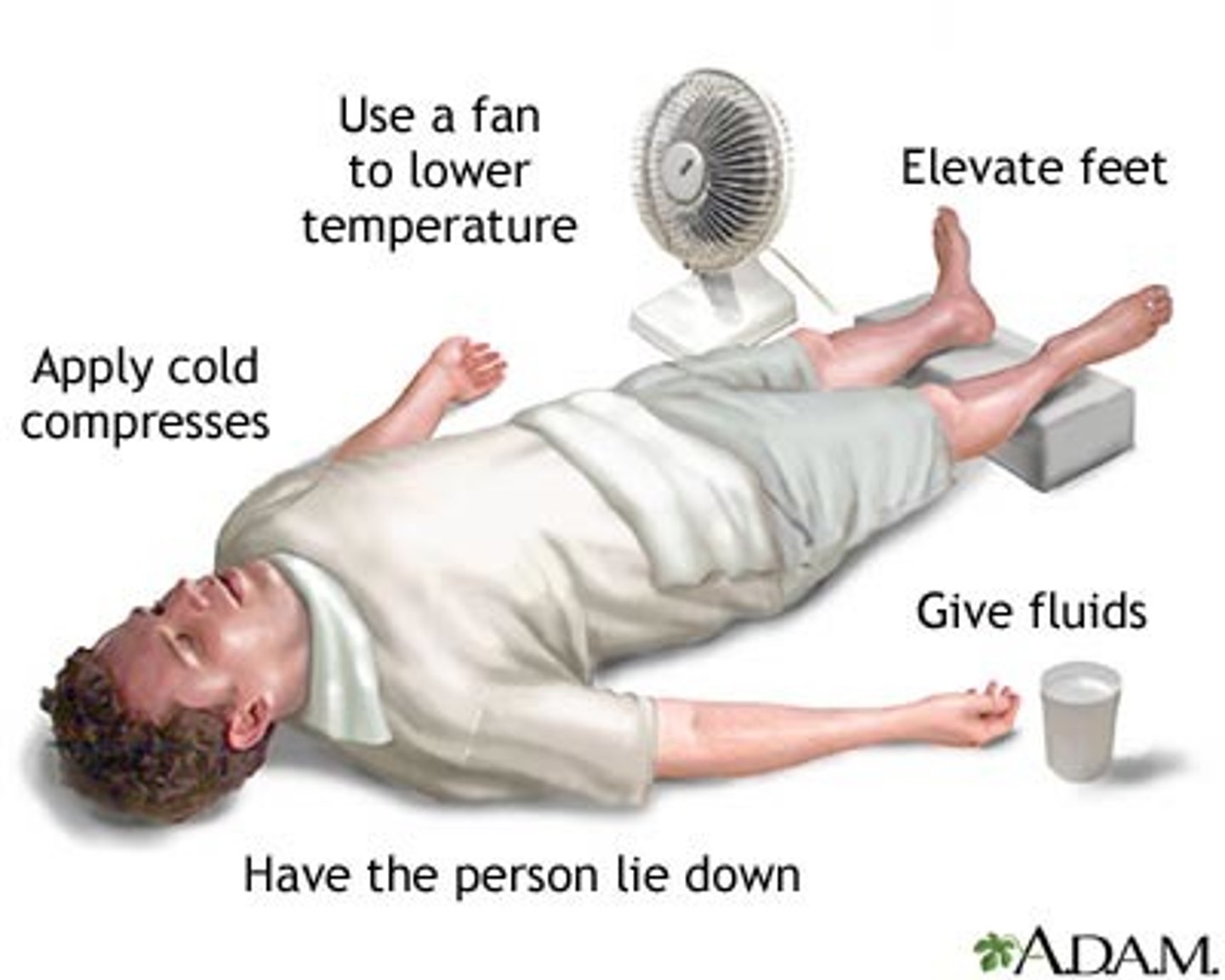
treating shock
1. check ABCs and treat for injuries
2. lay victim on back
3. raise legs 8-12 inches
4. cover with blankets, coats
5. call for medical assistance
6. do not give victim anything to eat or drink

burn
an injury to the skin and other tissues caused by heat, chemicals, electricity, or radiation. The degree refers to the depth of tissue damage

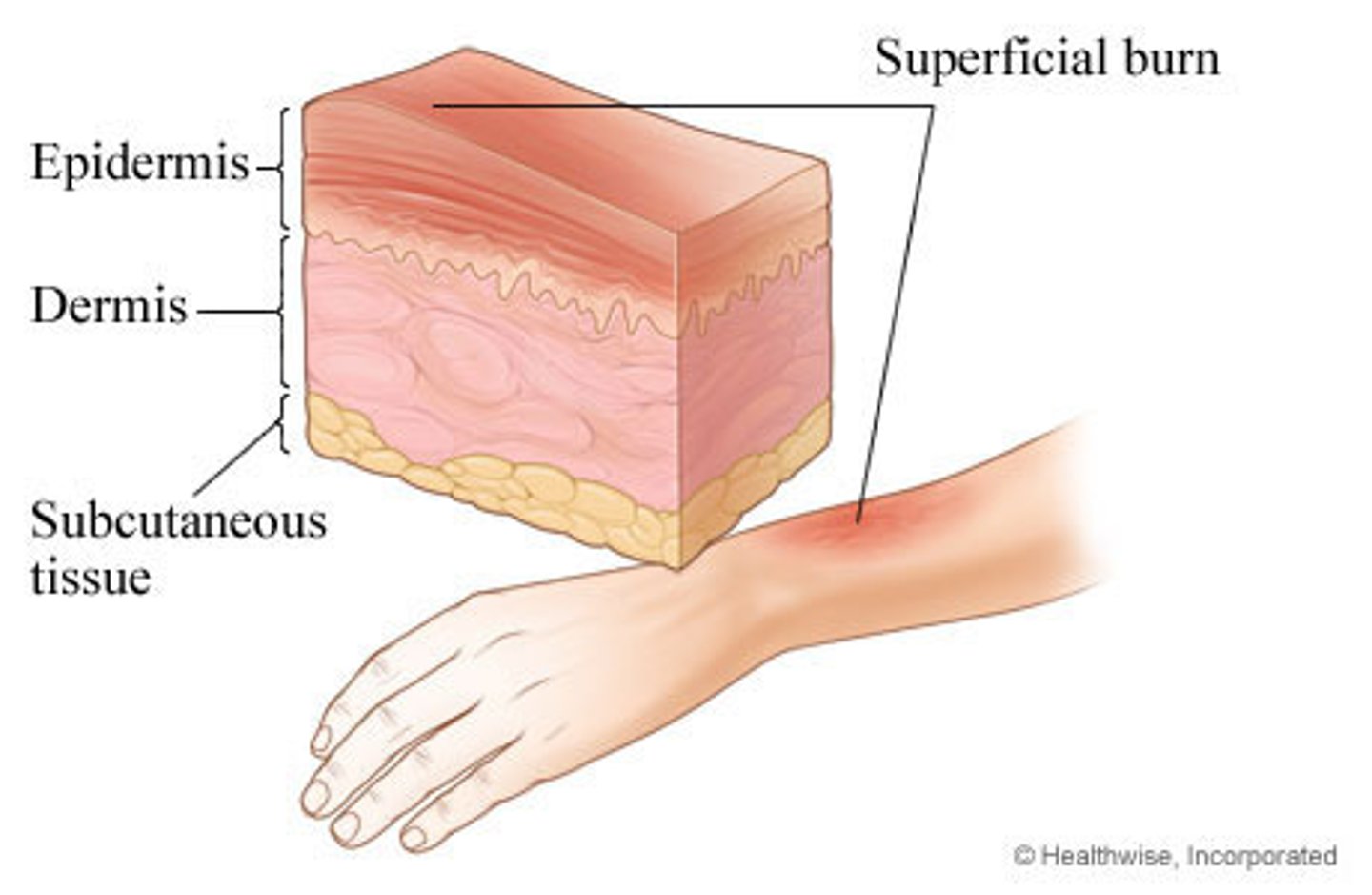
first degree burns
burns that affect only the outer layer of the skin and look pink. Take 3-6 days to heal. No scars.
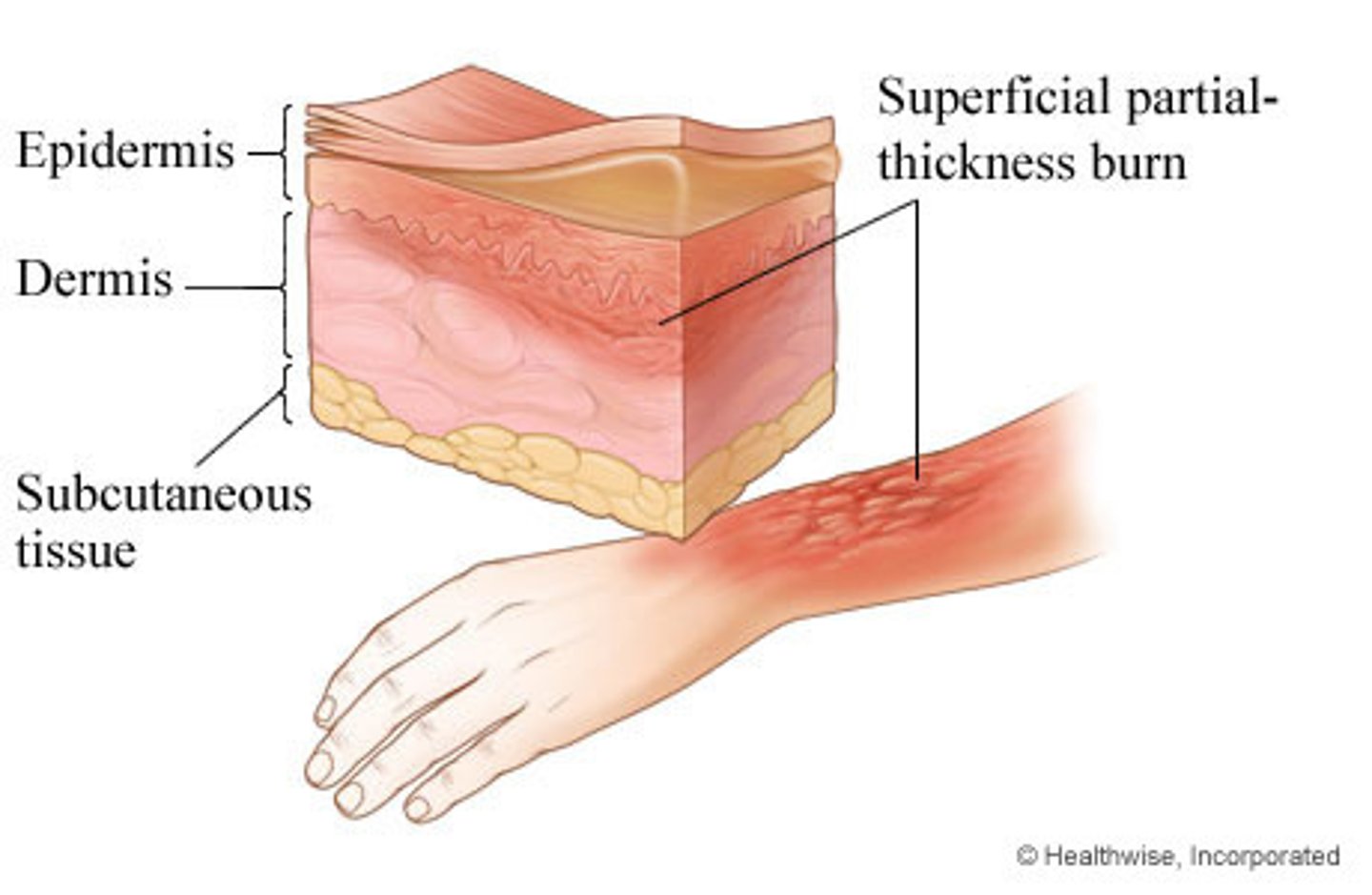
second degree burns
burns that go into the inner skin layer and are red, swollen, and blistered. Take less than 3 weeks to heal. Scars possible.
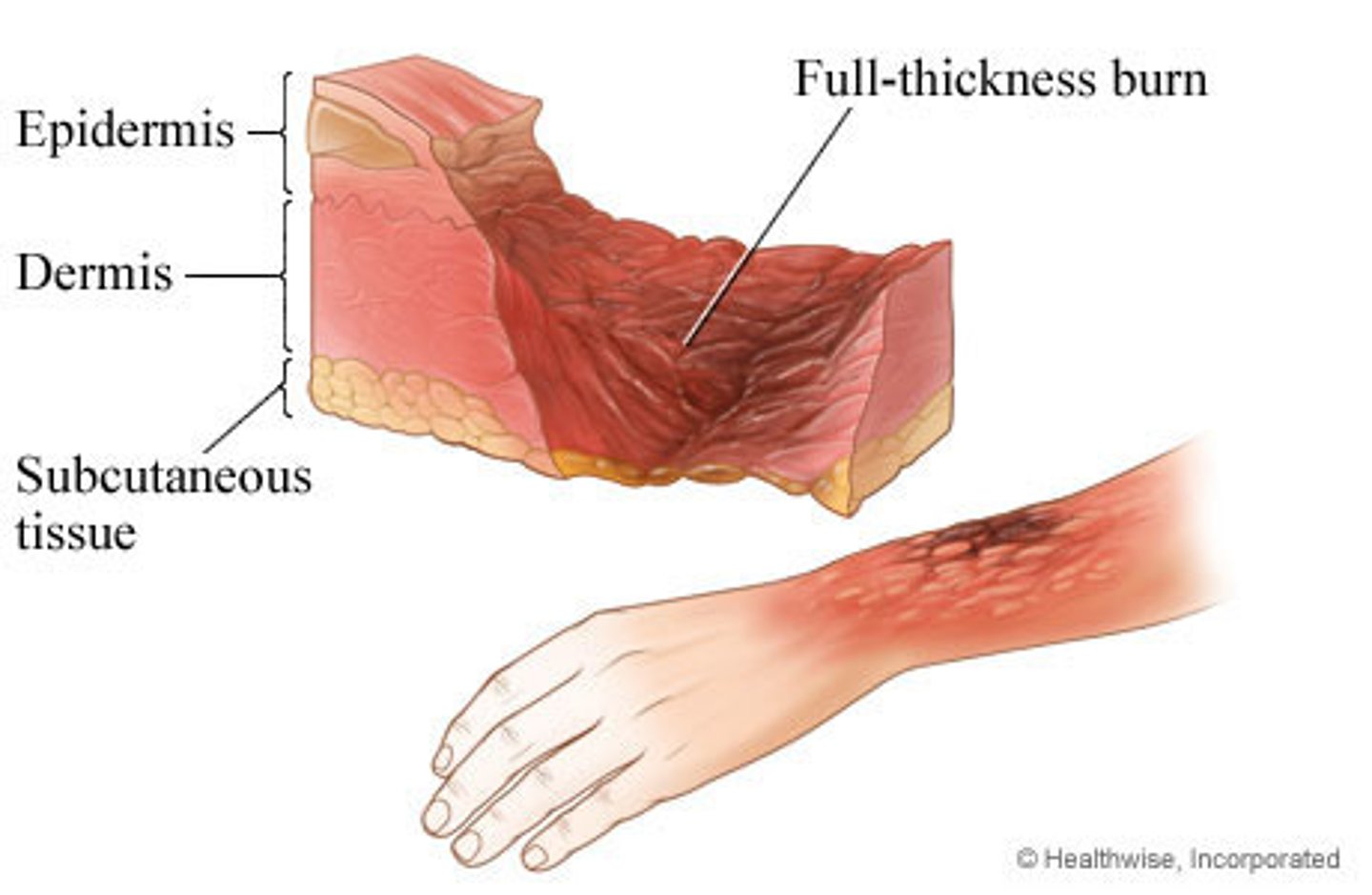
third degree burns
burns that go through all skin layers as well as tissue beneath the skin. Burns appear white, tan or charred black. Skin graft must be performed to heal. Some scarring. Take months to heal.
treating first degree burns
apply cool water until pain stops, apply moisturizing lotion

treating second degree burns
apply cool water until pain stops, apply antibacterial ointment, seek medical attention if severe

treating third degree burns
cover with clean, dry cloth; treat for shock; seek medical attention immediately

thermal burns
caused by contact with open flames, hot liquids or surfaces, or other sources of high heat
Treat by removing victim from source, cool burn with water, check for bleeding and shock, seek medical attention

chemical burns
caused by contact with chemicals that can burn the skin
Treat by flushing burn with lots of cool water to remove chemical, or brush powdered chemical off skin with clean cloth
electrical burns
direct exposure to electricity
Treat by shutting off current, approach only if safe, cool burn with water, check breathing and for signs of bleeding, treat for shock, seek medical attention
special consideration for burns
Seek medical help if severe 2nd degree, 3rd degree, chemical or electrical burns
Never apply ointment or cream to severe burn
Never remove clothing stuck to burn wound
Always treat burns to face, hands and feet as severe.

fracture
crack or break in a bone

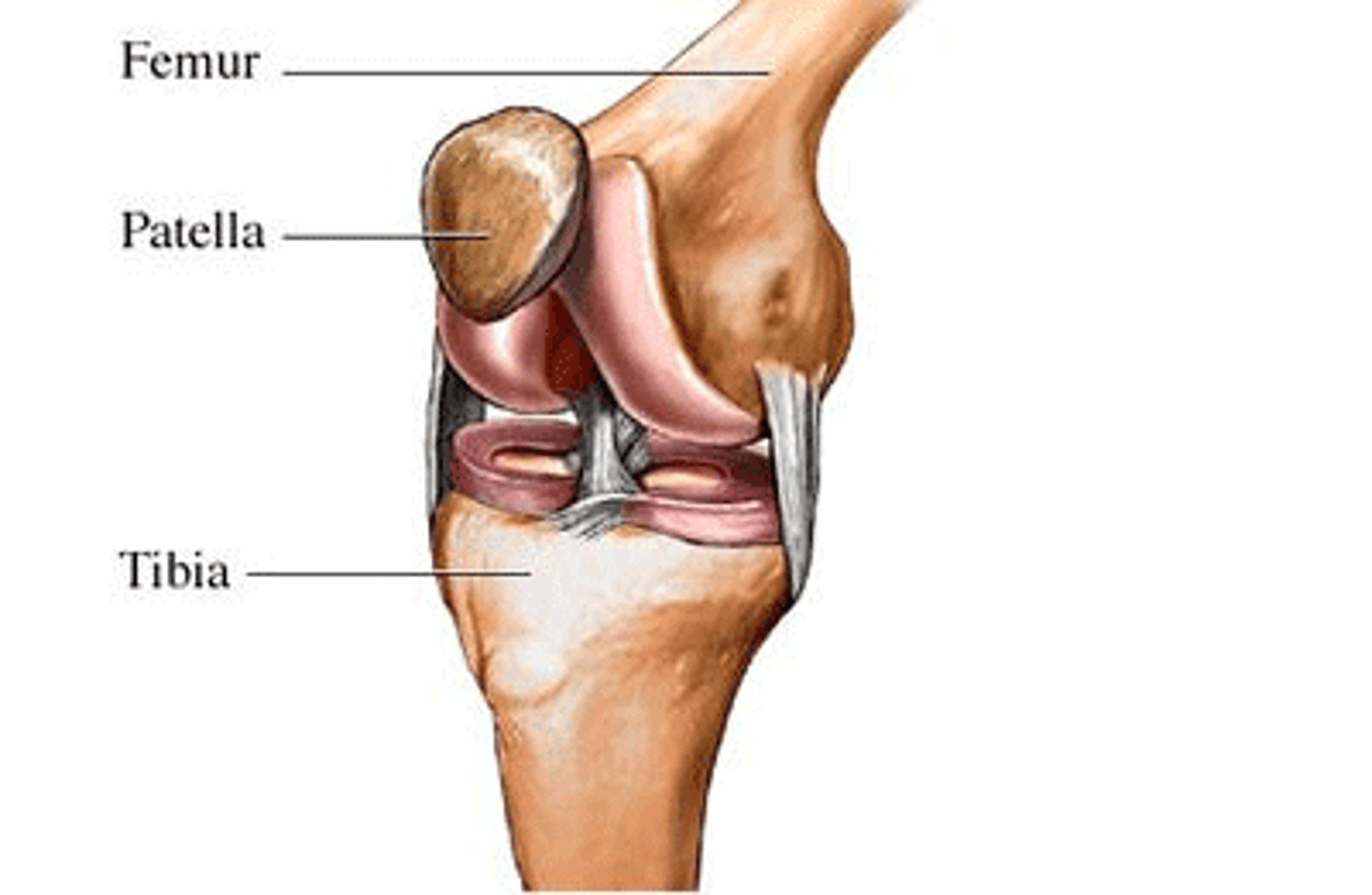
dislocation
injury in which a bone has been forced out of its normal position in a joint
open fracture
skin is broken and bone ends may stick out of skin; obvious wound
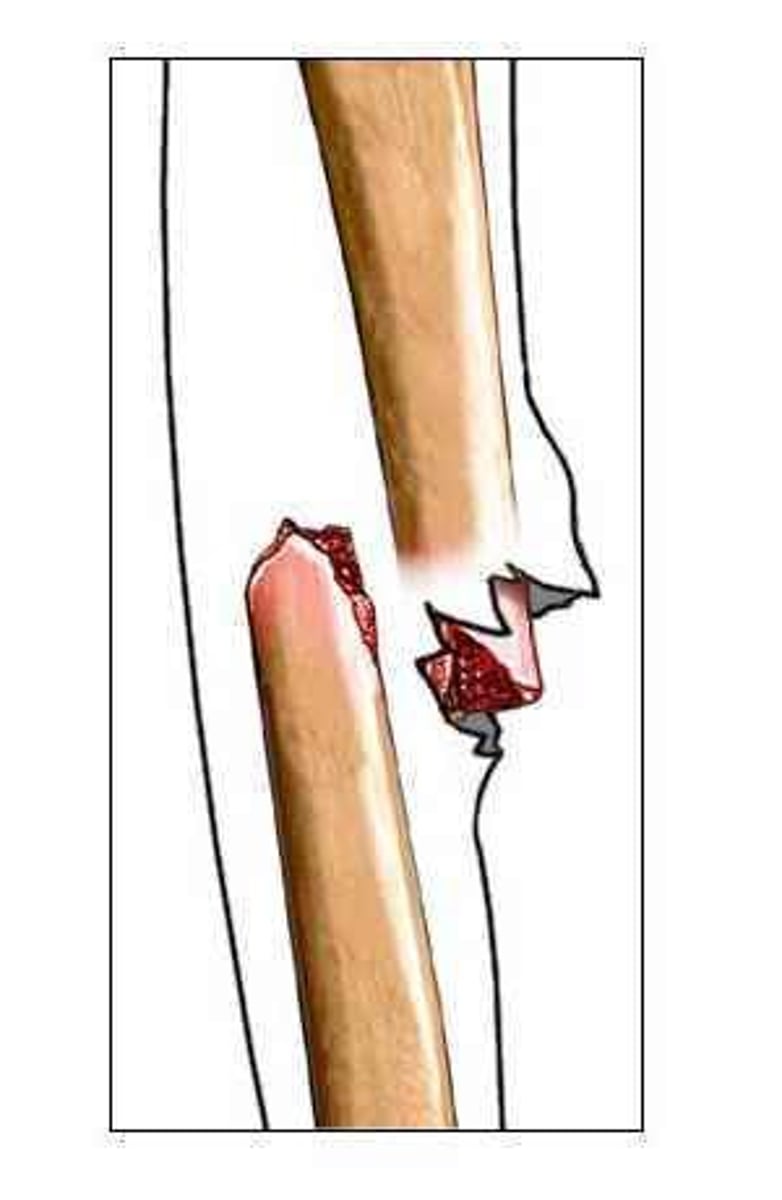
closed fracture
skin is unbroken. Injured bone causes pain and tenderness, loss of function, deformity, unnatural movement, swelling, bruising, grating sensation
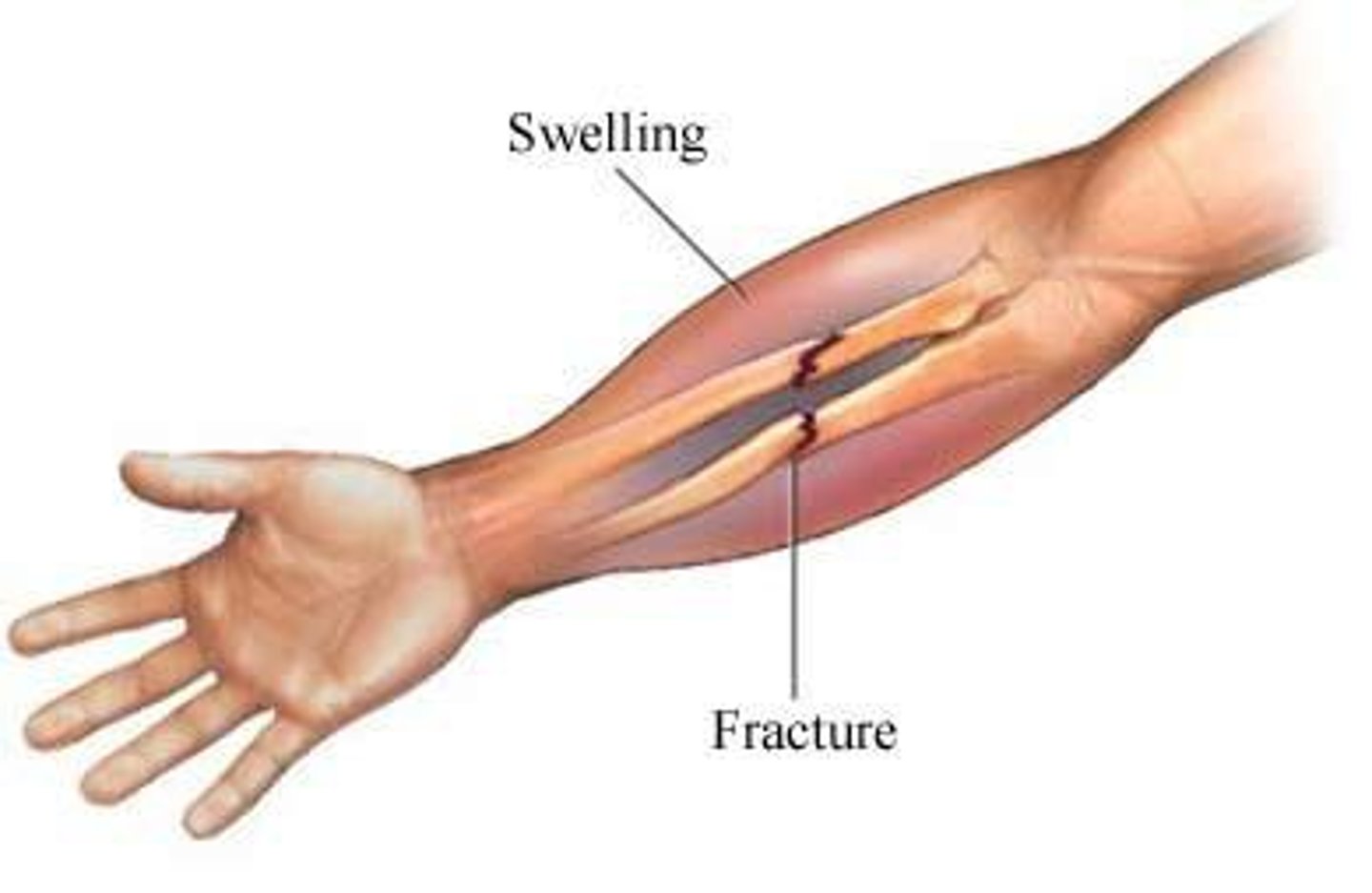
treating a fracture
check for bleeding, call for medical help, splint the area in position it was found, placing padding between splint and body, cover wounds with clean, dry dressing

splint
device used to stabilize a body part
Used to reduce pain, prevent further damage of tissues surrounding fracture, reduce bleeding and swelling

ligament
tissue that connects bone to bone
compression of bone, joint or muscle injury
wrap injured area with elastic bandage to prevent movement or swelling

heat exhaustion
condition in which the body becomes heated to a higher temperature than normal
causes: exercising or working in hot, humid place when heavy sweating causes loss of body fluids

symptoms of heat exhaustion
cold, moist skin; normal or above skin temperature; headache; nausea; extreme fatigue (tiredness)
treatment of heat exhaustion
move to shady place; remove clothes; apply cool, wet towels; use fan; give victim half a glass of cool (not cold) water every 15 minutes
heat stroke
condition in which the body loses its ability to cool itself by sweating because the victim has become dehydrated

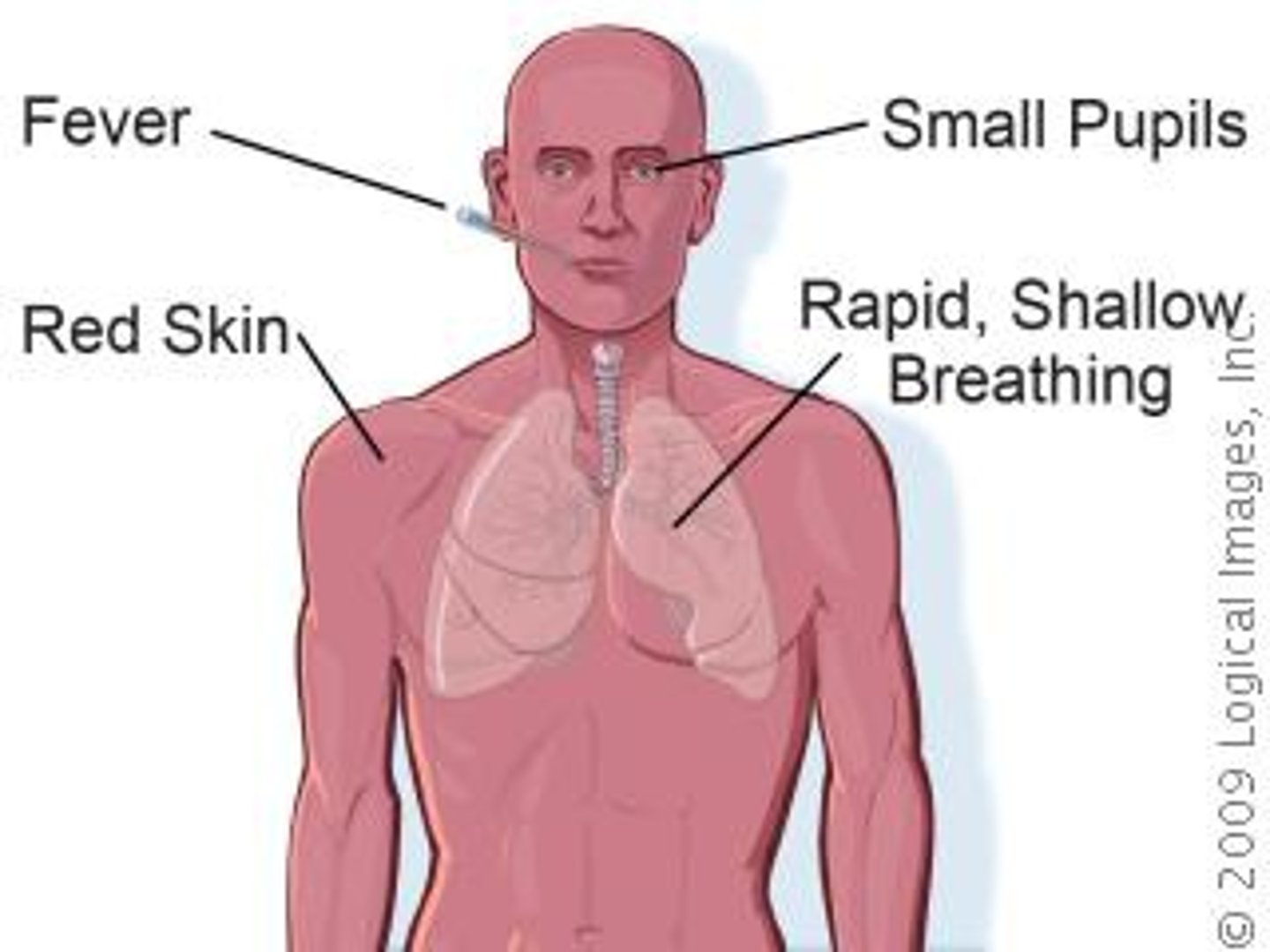
symptoms of heat stroke
hot, dry skin; higher than normal body temperature; rapid pulse; rapid, shallow breathing; could lose consciousness
treatment of heat stroke
seek medical help, move to cool place, cool body rapidly by immersing victim in cool (not cold) water or placing icepacks where large blood vessels are; only give food/water if not vomiting

steps to checking an injured person
1. Check the scene, remove hazards (dangers), determine how many victims
2. tap shoulder and shout, "Are you okay?"
3. Call 911 if no response
4. open airway, check for signs of life for no more than 10 seconds
5. No breaths go in, then look for severe bleeding and begin CPR/AED
6. If breathing, put in recovery position, check ABCs
