(22.6) Gas Exchange
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
38 Terms
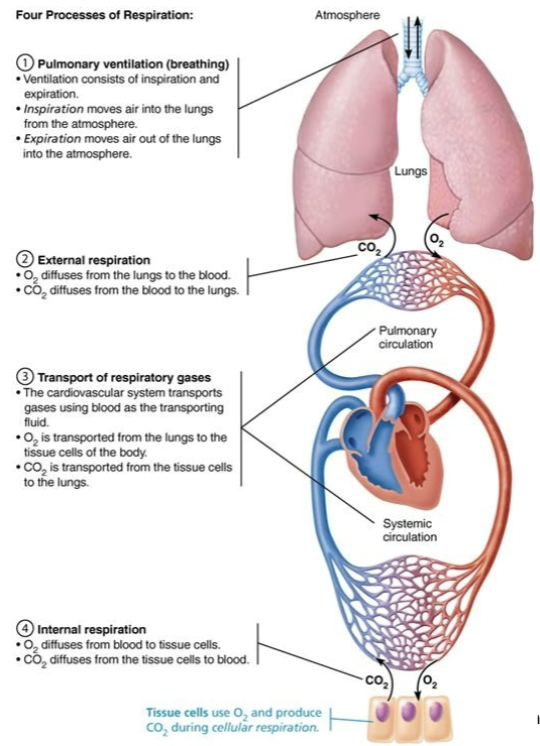
Explain Gas Exchange
Occurs between lungs and blood as well as blood and tissues
Both process are subjected to
Basic properties of gases
Composition of alveolar gas
Define Dalton’s Law of Partial Pressures
Total pressure exerted by a mixture of gases is the SUM of pressures exerted by each gas in the mixture
TELLS US WHICH DIRECTION GASES GO (FROM HIGH TO LOWER PRESSURE)
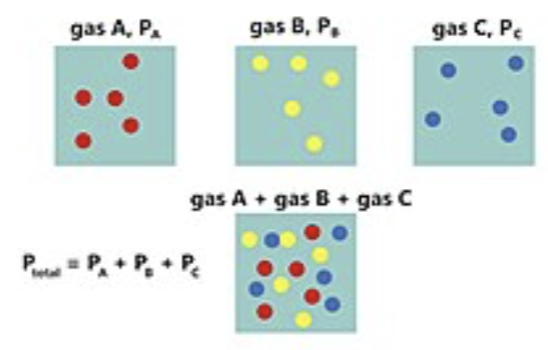
Define Partial Pressure
The pressure exerted by a single component of a mixture of gases
Directly proportional to its percentage in mixture
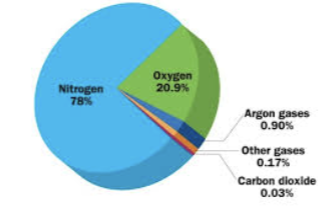
Total Patm = ?
760 mmHg
How much is Nitrogen in the air?
78.6%
Calculate Partial Pressure of Nitrogen (PN2)
0.786 × 760 mmHg = 597 mmHg N2
How much is Oxygen in the air?
20.9%
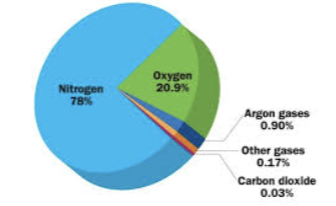
Calculate Partial Pressure of Oxygen (PO2)
0.209 × 760 mmHg = 159 mmHg
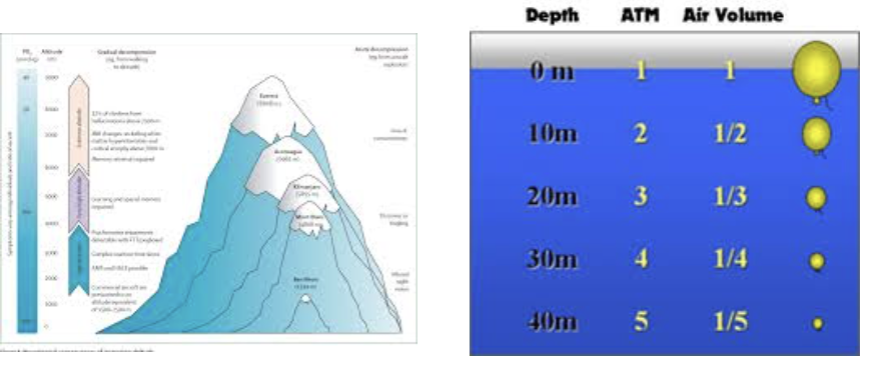
Compare High & Lower Altitudes influence on Partial Pressure
HIGH altitudes → Partial pressure DECLINES
LOWER altitudes (under water)→ Partial pressure INCREASES significantly
Define Henry’s Law
For gas mixtures in contact with liquids: Each gas will dissolve in the liquid in proportion to its partial pressure of that gas
At equilibrium → partial pressures in the two phases will be equal
HOW MUCH OF GAS DISSOLVES INTO BLOOD
Amount of each gas that will dissolve depends on =?
Solubility
CO2 is 20x more soluble in water than O2, and little N2 will dissolve
Temperature
As temperature of liquid rises, solubility decreases
Compare Approx % Gas Partial Pressure in the Atmosphere & in the Alveoli (for O2 and CO2)
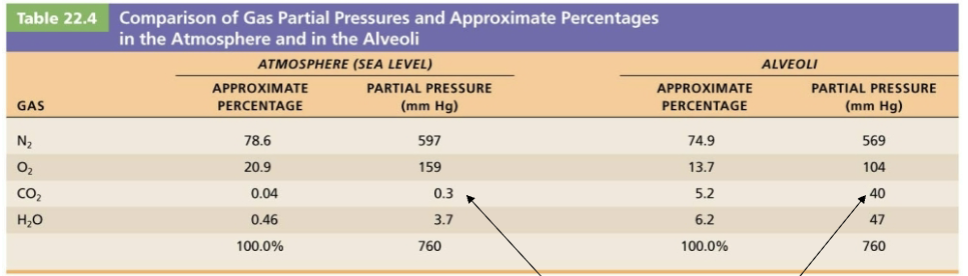
Describe how atmospheric and alveolar air differ in composition
Alveoli contain more CO2 and water vapor than atmospheric air
Explain why does Alveoli contain more CO2 and water vapor than Atmospheric air
Gas exchanges occurring in the lungs (O2 diffuses from the alveoli into the pulmonary blood and CO2 diffuses in the opposite direction)
Humidification of air by conducting passages
The mixing of alveolar gas that occurs with each breath
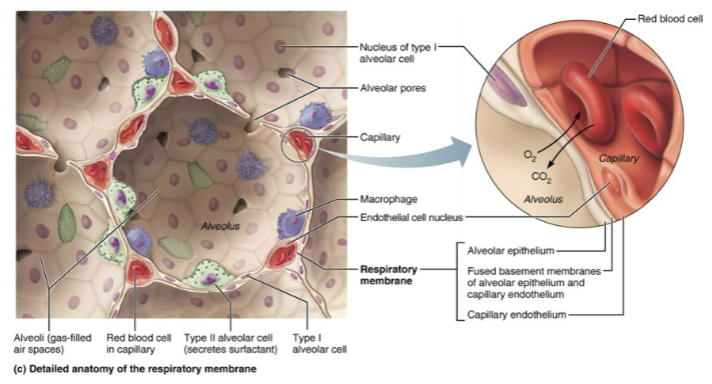
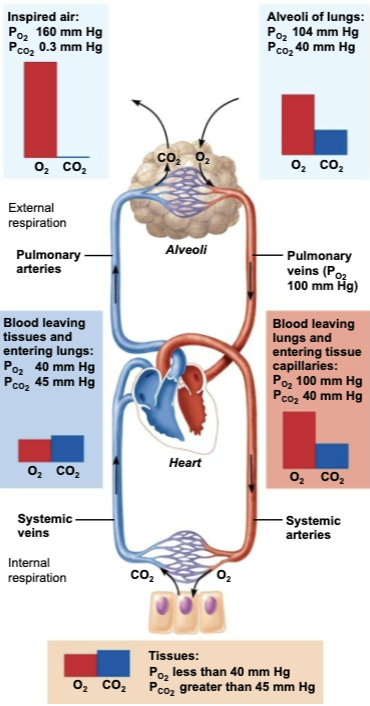
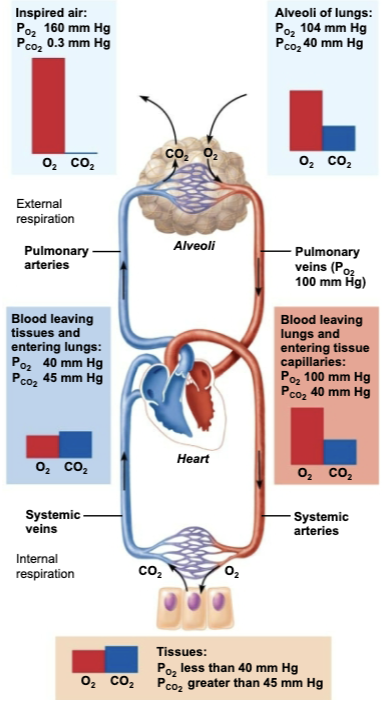
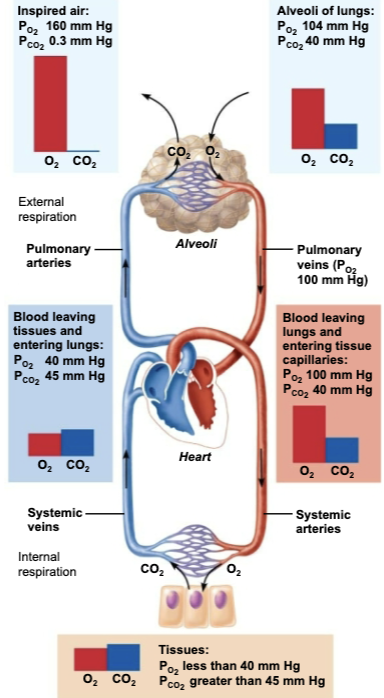
Define External Respiration
Pulmonary Gas Exchange
Involves the exchange of O2 (uptake) CO2 (unloading) across respiratory membranes
List Factors that Influence on External Respiration
Partial pressure gradients and gas solubilities
Thickness and surface area of the respiratory membrane
Ventilation-perfusion coupling (matching alveolar ventilation with pulmonary blood perfusion)
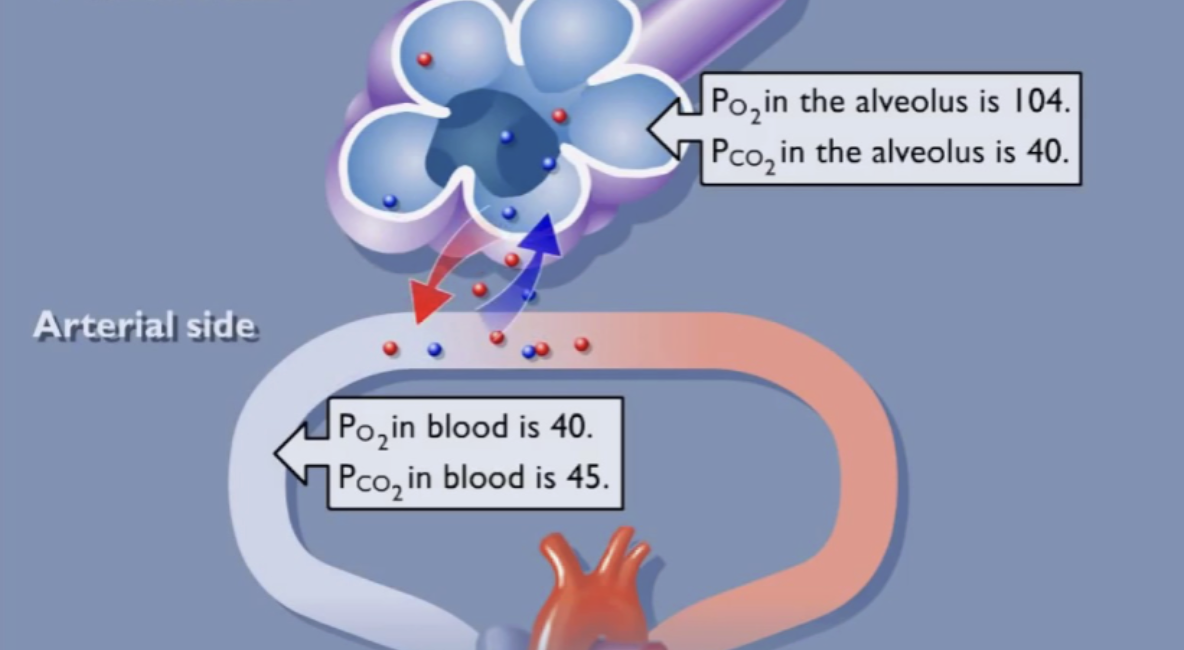
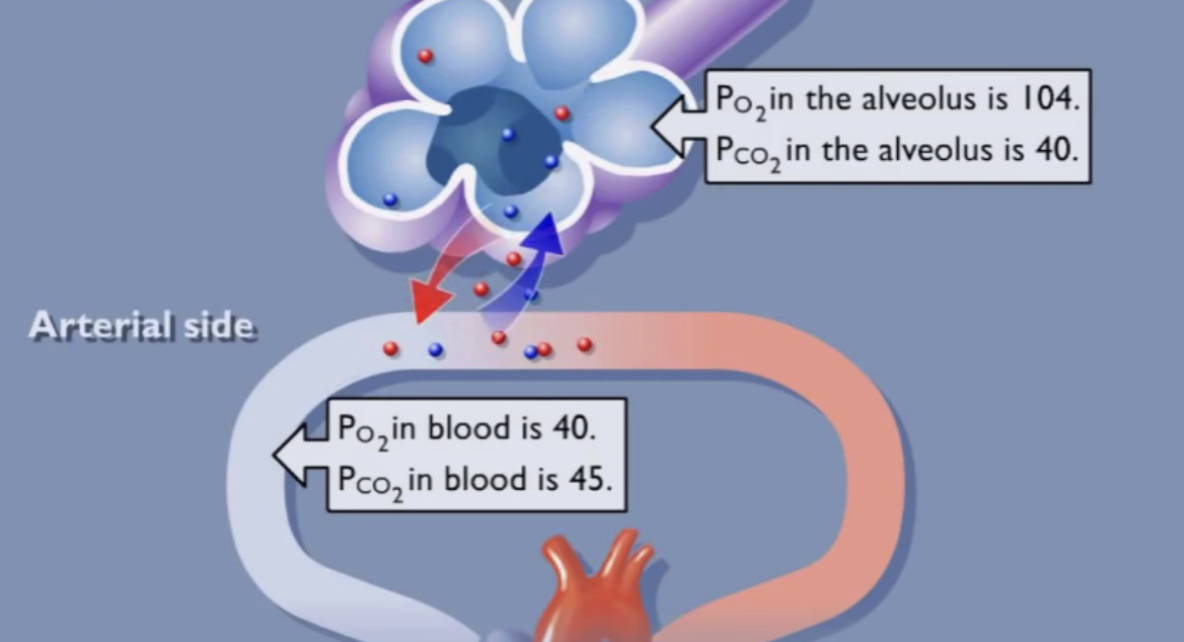
Explain Partial pressure gradients and gas solubilities
Influences on External Respiration (1/3)
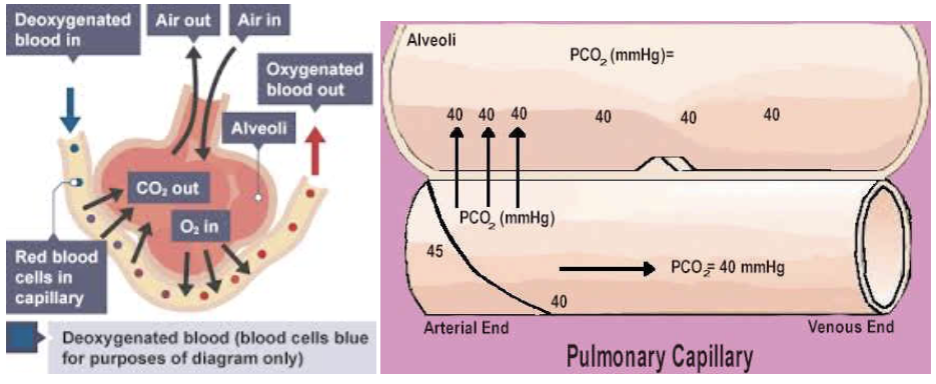
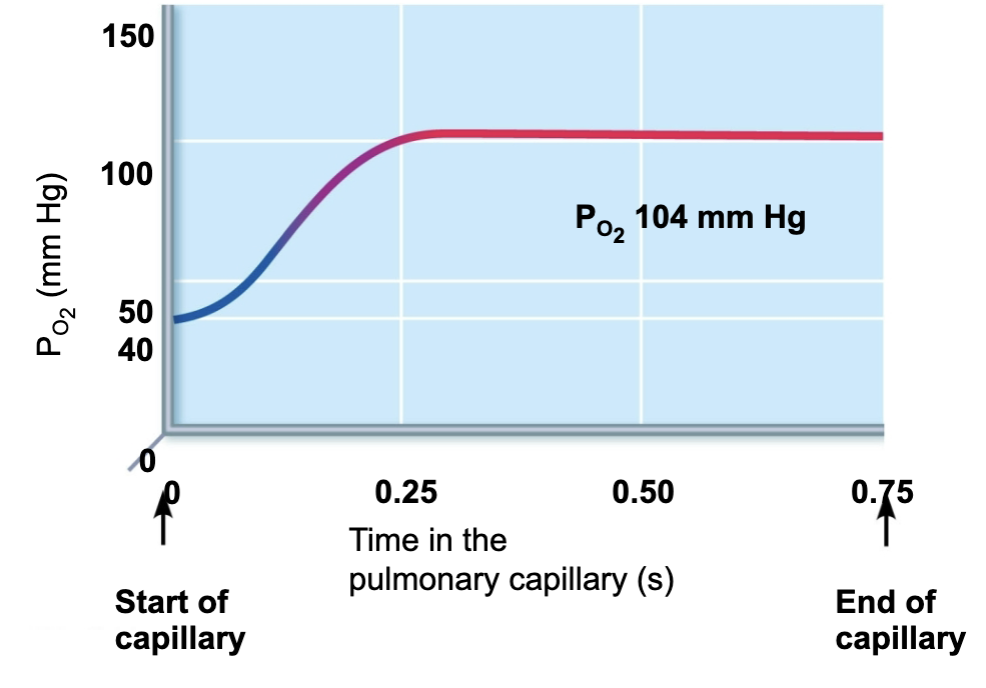
A STEEP partial pressure gradient exist between blood in the pulmonary arteries and alveoli and O2 diffuses rapidly until it reaches equilibrium at PO2 of 104 mmHg
Alveoli → Blood
CO2 moves in the opposite direction ALONG a partial pressure that is much LESS steep → reaching equilibrium at 40 mmHg
Blood → alveoli
Through gradient is not as steep → CO2 still diffuses in equal amounts with oxygen
REASON is that CO2 is 20x MORE soluble in plasma and alveolar fluid than oxygen
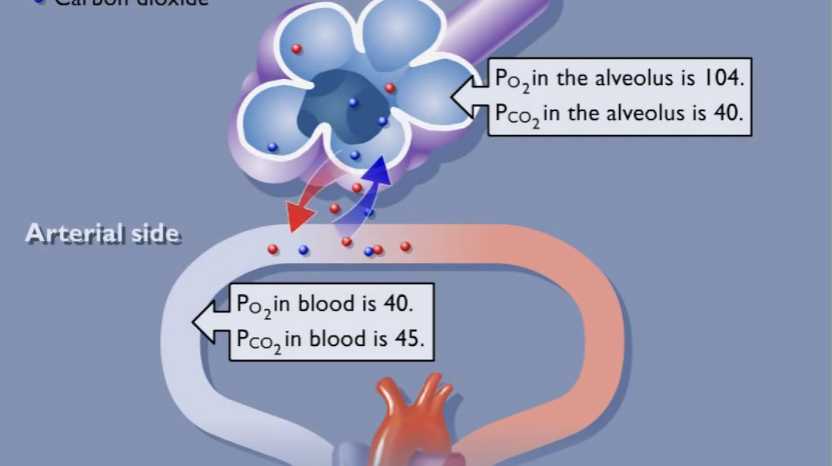
T/F: PO2 is greater in the alveolus than the blood, so oxygen diffuses into the blood.
→ TRUE
During pulmonary gas exchange, oxygen will diffuse down its partial pressure gradient from the alveolus into the blood until the partial pressure is equal in both locations.
_______ has a greater partial pressure in the pulmonary capillaries than in the alveoli, so it diffuses into the _______.
CO2 has a greater partial pressure in the pulmonary capillaries than in the alveoli, so it diffuses into the alveoli
Despite the fact that the partial pressure difference is so much smaller for CO2, why is there as much CO2 exchanged between the alveoli and blood as there is O2?
→ CO2 is much more soluble in blood than O2
How would the partial pressures of O2 and CO2 change in an exercising muscle?
→ The partial pressure of O2 would decrease, and the partial pressure of CO2would increase
Cells use O2 and produce CO2 during cellular respiration to produce ATP. Exercising muscles need more ATP.
Oxygenation of Blood in the Pulmonary Capillaries @ Rest
A STEEP partial pressure gradient exist between blood in the pulmonary arteries and alveoli and O2 diffuses rapidly until it reaches equilibrium at PO2 of 104 mmHg
Alveoli → Blood
CO2 moves in the opposite direction ALONG a partial pressure that is much LESS steep → reaching equilibrium at 40 mmHg
Blood → alveoli
Partial pressure gradients promoting gas movements in the body
O2
Air enters through the nose or mouth
Air travels down the trachea and then enters the bronchi
Air travels down smaller and smaller bronchioles
Air reaches small sacs (alveoli)
CO2
CO₂ is released from the mitochondria
CO₂ diffuses into a capillary
CO₂ is carried to the lungs
CO₂ diffuses into an alveolus
Air exits through nose or mouth
Explain Thickness and surface area of the respiratory membrane
Influences on External Respiration (2/3)
Respiratory membranes are very thin → 0.5-1 um thick
Large total surface area of the alveoli is 40x the surface area of the skin

Explain Ventilation-perfusion coupling
Influences on External Respiration (3/3)
Ventilation (amount of gas reaching alveoli) and perfusion (amount of blood flowing through pulmonary capillaries) must be coupled for optimal, efficient gas exchange
VENTILATION = how much air reaches the alveoli
PERFUSION = how much blood reaches the alveoli
How is Ventilation-perfusion coupling controlled?
Both controlled by local auto regulatory mechanisms
Alveolar PO2 → controls perfusion by changing arteriolar diameter
Alveolar PCO2 → controls ventilation by changing bronchiolar diameter
Explain Influence of local PO2 on Perfusion
Changes in local alveolar PO2 cause changes in diameters of local arterioles
If PO2 is low (from poor ventilation) → arterioles constrict to decrease perfusion
Directs blood to go to well ventilated alveoli → where O2 is high (and CO2 is low), so blood can pick up more oxygen (and remove more CO2)
If PO2 is high (from good ventilation) → arterioles dilates to increase perfusion
Opposite mechanism, seen in systemic arterioles that dilate when oxygen is low and constrict with high
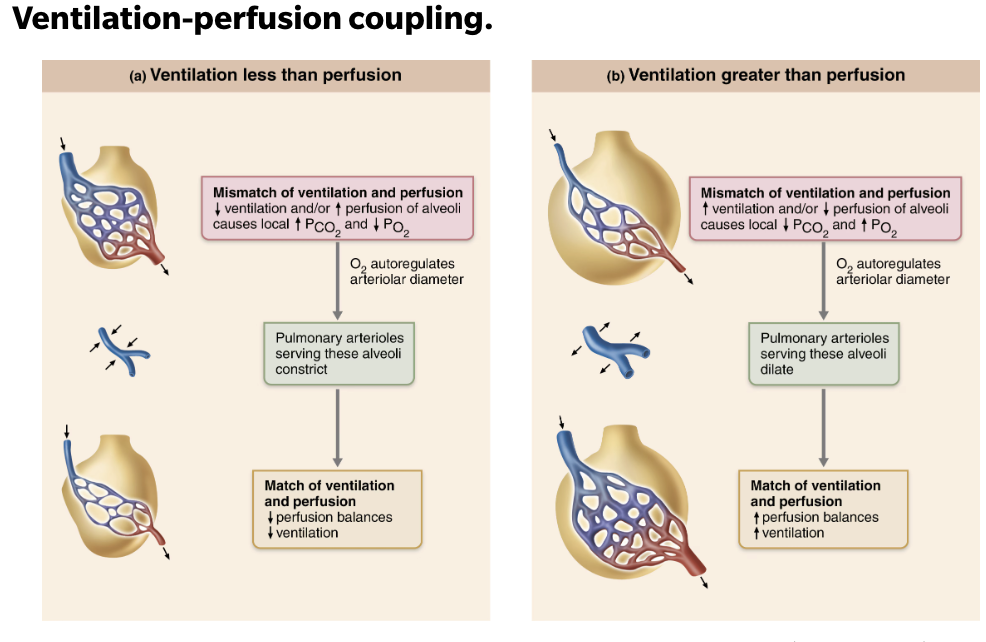
Explain Influence of local PCO2 on Ventilation
Poor alveolar ventilation results in low alveolar PO2 (high PCO2) →
Pulmonary arterioles constrict → less blood goes to this poorly ventilated alveolus
Bronchioles dilate→ to bring more air in and wash out the extra CO₂
To improve the match by sending less blood and more air.
Good alveolar ventilation results in high alveolar PO2 (low PCO2)
Pulmonary arterioles dilate → more blood is sent to this well-ventilated alveolus
Bronchioles constrict→ because not as much extra airflow is needed
To match plenty of air with plenty of blood.
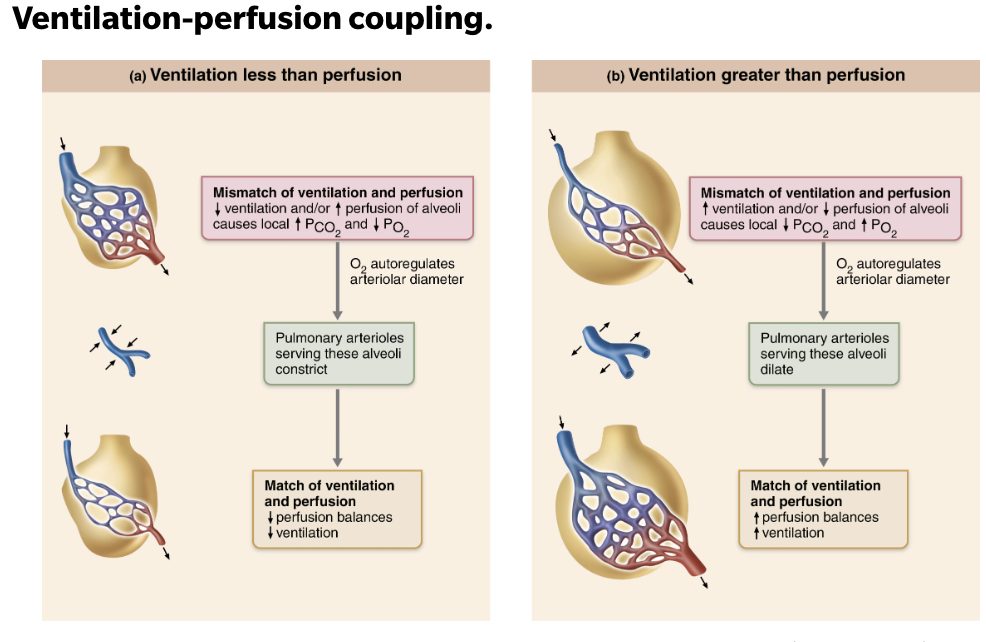
What would occur if lung cancer restricts the airflow to a group of alveoli?
→ PO2 in the affected alveoli would decrease, and their arterioles would vasoconstrict
If PO2 is low (from poor ventilation) → arterioles constrict to decrease perfusion
Directs blood to go to well ventilated alveoli → where O2 is high (and CO2 is low), so blood can pick up more oxygen (and remove more CO2)
SUMMARY of Factors that Influence on External Respiration
Partial pressure gradients and gas solubilities
A STEEP partial pressure gradient exist between blood in the pulmonary arteries and alveoli and O2 diffuses rapidly until it reaches equilibrium at PO2 of 104 mmHg
Alveoli → Blood
CO2 moves in the opposite direction ALONG a partial pressure that is much LESS steep → reaching equilibrium at 40 mmHg
Blood → alveoli
Thickness and surface area of the respiratory membrane
Very thin
Huge surface area for efficient gas exchange
Ventilation-perfusion coupling
Ensures a close match between the amount of gas reaching that alveoli and the blood flow in the pulmonary capillaries
VENTILATION = how much air reaches the alveoli
PERFUSION = how much blood reaches the alveoli
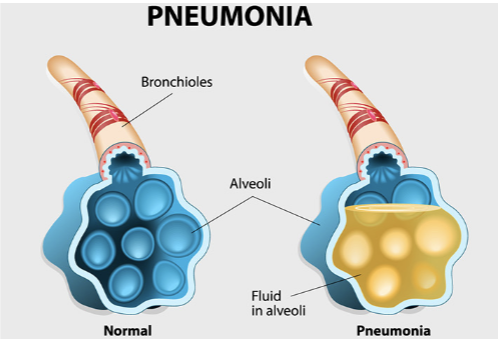
Explain Cause and Effect of Pneumonia
CAUSE
Effective thickness of respiratory membrane INCREASES dramatically if the lungs become waterlogged and edematous
EFFECT
Pneumonia
Explain Cause, Effect, and Treament of Emphysema
CAUSE
Reduce the alveolar surface area
EFFECT
Walls of adjacent alveoli break down and the alveolar chambers enlarge
TREATMENT
Administering supplemental oxygen → Increase the PO2 in the alveoli to increase the diffusion of oxygen across the respiratory membrane
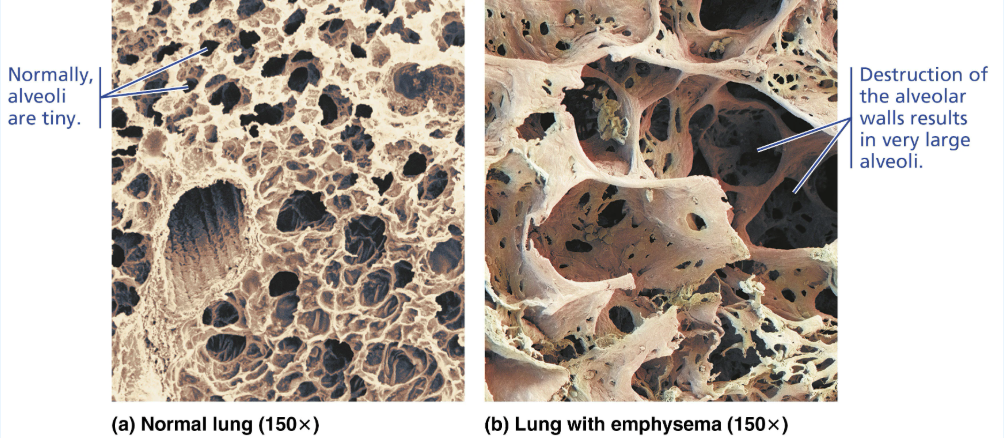
Name other examples of Pulmonary Diseases that REDUCE Alveolar Surface Area
Tumors
Mucus
Inflammatory material
Reduce surface area by blocking gas flow into alveoli
Define Internal Respiration
Involves capillary gas exchange in body tissues
T/F: Diffusion gradients for O2 and CO2 are reversed from those from external respiration and pulmonary gas exchange, the factors promoting has are identical
→ TRUE
Compare Partial pressure and diffusion gradients between Internal Respiration vs External Respiration
Partial pressures and diffusion gradients in Internal Respiration are REVERSED compared to External Respiration
Tissue PO2 is ALWAYS LOWER than in arterial blood PO2 (40 vs 100 mmHg) → so O2 moves from blood to tissues
Tissue PCO2 is ALWAYS HIGHER than arterial blood PCO2 (45 vs 40 mmHg) → so CO2 moves from tissues into blood
Venous blood returning to heart has PO2 of 40mmHg and PCO2 of 45 mmHg
Which way would O2 and CO2 diffuse during internal respiration?
O2 would diffuse into the cells, and CO2 would diffuse into the systemic capillaries.
Relate Dalton’s and Henry’s laws to events of pulmonary and tissue gas exchange.
Dalton’s Law → Total pressure exerted by a mixture of gases is the SUM of pressures exerted by EACH gas in the mixture
How gas behaves in a mixture of gasses (from higher pressure to lower pressure)
Henry’s Law → For gas mixtures in contact with liquids: Each gas will dissolve in the liquid in proportion to its partial pressure of that gas
How gases move into and out of solution