Later life/neurocognitive disorders
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
Effects to consider when measuring elderly:
age effects, cohort effects, time-of-measurement effects
>65 psychopathology rates
methodology issues
lower; more positive emotion and focus on intimacy (social selectivity), but also methodology issues! These are: response bias/disclosure, selective mortality, and cohort effects
Treatment with medicine:
more severe side effects, usually tested on young people, polypharmacy risks
Dementia umbrella term percentages:
Alzheimer’s 50-75%, vascular 20-30%, Lewy body 10-25%, FTD 10-15%
Psychiatric symptoms secondary to dementia:
50% depression, also sleep disturbances, loss of impulse control, delusions or hallucinations
[Study slides for neuropsychological assessment]
Stages for dementia
Pre- —> asymptomatic —> subjective complaint —> MCI —> dementia
Mild neurocognitive disorder (MCI) criteria
based on 1) concerns of patient/close other/clinician and 2) modest neurocognitive decline in 1+ cognitive domains; *does not interfere with independence in everyday activity!! Although may need more effort or support
Major neurocognitive disorder criteria:
SAME CRITERIA but SUBSTANTIAL decline (on formal testing) and DOES interfere with independence in everyday activity
Dementia prevalence 2010:
>35 million
Alzheimer’s disease:
mainly memory loss, disorientation.
Amyloid cascade hypothesis: Neurons have plaques (protein deposits) outside and neurofibrillary tangles (tau proteins inside neuron) —> causing immune response, inflammation, neurons die, frontal and temporal and parietal lobes shrink
Protective factors for Alzheimer’s:
exercise, cognitive engagement
Frontotemporal dementia:
most common=behavioral variant!!; prevalence <1%, loss of neurons in frontal (PFC) and temporal (anterior) regions, memory not impacted, starts in 50s!!!! Death in 5yrs
Vascular dementia:
usually stroke -> blood clot -> neuron death; symptoms vary
Dementia with lewy bodies:
1% (rare), Lewy bodies are proteins; vivid hallucination and dreams, etc
Treatment:
meds slow the decline but don’t restore memory (e.g. cholinesterase inhibitors)
Delirium:
extreme trouble focusing attention. Criteria: disturbance in attention/awareness; change in cognition that isn’t dementia; rapid onset and fluctuation throughout day; symptoms ARE caused by a medical condition or toxin or substance
Delirium etiology and treatment:
etiology is drug use or withdrawal or metabolic/nutritional deficiencies; treatment for underlying condition can have complete recovery, without treatment there’s risk of death in 6mo, uses atypical antipsychotics
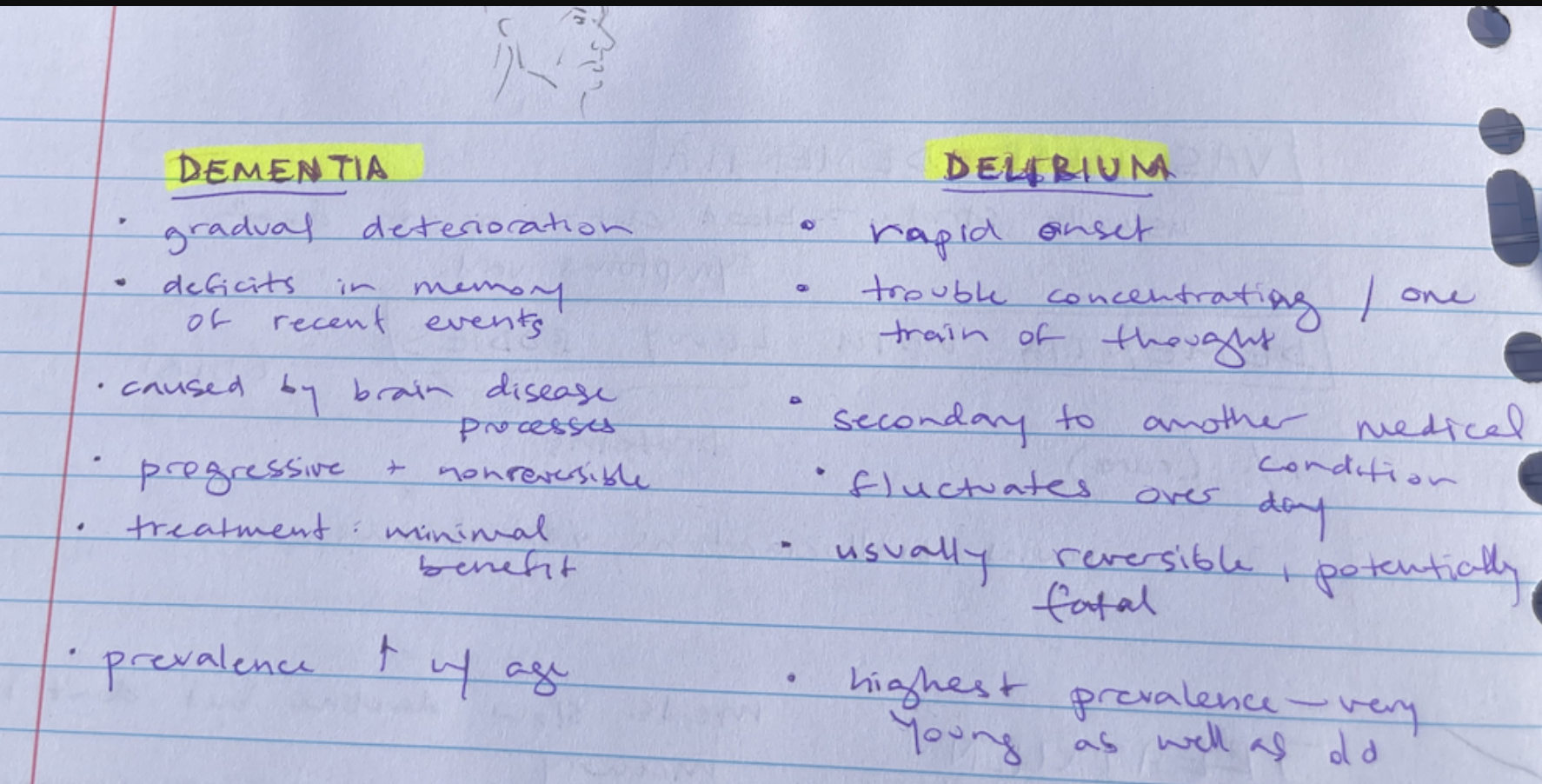
Dementia vs delirium: